Occupational Health Clinic Oversight Committee: Final Report to the Governor and Legislature
December 2012
- The Final Report to the Governor and Legislature is available in Portable Document Format, (PDF, 816KB, 45pg.)
Oversight Committee Members
- Ellen Lee Clarke, District Council 37
- Roger A. Cook,Western NY Council on Occupational Safety and Health
- Marsha M. Fitzgerald, RN COHN-S/CM, First Niagara Risk Management
- Kitty H. Gelberg, PhD, MPH, NYS Department of Health (Commissioner's Designee)
- Wesley L. Hicks, MD, FACS (December 2010 – August 2011), Roswell Park Cancer Institute
- Gregory J. Kash, PhD, Northrop Grumman (Business Council Designee)
- Steven Markowitz, MD, Queens College
- James M. Melius, MD, Laborers Health & Safety Trust Fund (AFL-CIO Designee)
- Kenneth J. Munnelly, NYS Workers' Compensation Board (Chair's Designee)
- Mary O'Reilly, PhD, CIH, CPE, ARLS Consultants, Inc.
- Melvin Rivers, Albany Youth Construction Initiative Program
- Ambrish Shenoy (February 2010 – November 2012), NYS Insurance Fund
- Barbara M. Stanley, NYS Department of Labor (Commissioner's Designee)
- Daniel Vogrin, PhD, Melillo Center for Mental Health
- Heather Hynick, RN, MSN, FNP-BC, ANP, RNFA, Saratoga Hospital
Table of Contents
- Executive Summary
- Introduction
- Sustaining Access to Occupational Medicine Expert Care: Continued Need for Occupational Health Clinic Network
- Statewide Needs to be Met by the Network
- Coordination of Clinic Activities with Not-For-Profit, Private Sector Concerns and State Agencies, Including but not Limited to an Evaluation of Current Jurisdictional and Oversight Responsibilities
- Coordination and Sharing of Clinic Resources and Services
- Dissemination of Research Results and Educational Information
- Identification of Funding Sources for the Network
- Activities of the Clinics and Their Effectiveness in Meeting the Objectives as Set Forth in Statute and in Clinic-Specific Contracts with the State
- Local, Regional, Occupation or Business Sector Specific Needs that May be Met by One or More Clinic
- Other Issues as Determined by the Oversight Committee
- Incorporation of Provisions to Implement Its Recommendations in Requests for Applications of State Funding for Occupational Health Clinics
- References
- Appendix A. Partial List of Educational Materials Developed by the NYS Occupational Health Clinic Network
- Appendix B. Peer Reviewed Literature Published By The New York State Occupational Health Clinic Network, 2004-2011
- Appendix C. Comments Received During Public Comment Period
Executive Summary
The New York State Occupational Health Clinic Network (NYS OHCN) was the first partially publicly funded, statewide, public health-based network offering clinical and preventive occupational disease services in the United States. It was established to address the need for specialized regional occupational health centers open to all state residents for the diagnosis and treatment of occupational disease. The Network was established in 1987 with six regionally based clinics; it has since increased to ten regionally based clinics, with one additional specialty clinic for agriculture. The clinics reside in a variety of institutional settings, including state and private medical schools, a healthcare insurer, and a local consortium of unions.
The Oversight Committee was created by Section 2490 of the Public Health Law (PHL). The Committee was charged with making recommendations to the governor and legislature regarding the NYS OHCN. This report represents the findings of the Oversight Committee. Specific comments and recommendations (in bold) from the Committee are provided below.
-
Evaluation of current jurisdictional and oversight responsibilities
Overall, the New York State Department of Health (NYS DOH) has done a very good job in developing and managing the network of occupational health clinics. The structure for communication and information flow among the clinics and NYS DOH is very useful. The requirement for local advisory boards has been very helpful in ensuring that the clinics are responsive to their core mission and to local needs. The NYS DOH has faced difficulties due to funding limitations and the diversity of institutions that operate these clinics.
Coordination with other agencies
In order to fulfill the mission of the NYS OHCN, coordination between NYS DOH and other state agencies such as the Department of Labor (DOL) and the Workers' Compensation Board (WCB) could be helpful. The Committee recommends that NYS DOH and other state agencies take steps to work more closely with each other on the occupational health clinic program.
-
Coordination and sharing of clinic resources and services
The clinics have worked together on numerous projects including but not limited to hazardous waste training; pesticide specialist training; and education on the Health Show, a nationally syndicated weekly public radio program. The clinics also provide technical and administrative assistance to each other.
Consistency of services
The Committee notes the sharp differences in distribution of frequencies of patient diagnoses by clinic. This spectrum of patients evaluated and the services emphasized by each of the clinics reflects in part the interests and history of the clinic and may not necessarily reflect the broad set of needs of the local communities. Needs assessments should be completed at least once during the five year contract cycle by each clinic.
-
Dissemination of research results and educational information
Network staff collaborated to develop nine clinical practice reviews, which were published in the American Journal of Industrial Medicine. These were designed to assist clinicians in the diagnosis, treatment and prevention of occupational conditions. The clinics have developed a breadth of educational materials to meet their particular needs and have also published numerous articles in peer-reviewed journals.
Sharing of materials
The clinics should exercise leadership in professional education and clinical research. To aid in this process, there should be a more efficient method of sharing educational materials between the clinics that will allow them to develop and print materials, as needed, in a more cost-efficient manner.
-
Identification of funding sources for the Network
Workers' Compensation Law (WCL) § 151 provides for the administrative expenses of the Workers' Compensation Board (WCB). Included in the WCL § 151 assessment is an "additional sum as may be certified to the chair and the department of audit and control… for the New York state occupational health clinics network". Each year, the NYS DOH makes a budget request for the clinics and when the final amount is approved and certified, the WCB includes it in its § 151 assessment bills. All assessment money collected is transferred to the NYS DOH for distribution to the clinics.
Increased funding
The occupational health clinics continue to address a significant need for occupational health services in New York State that is not being otherwise addressed. The NYS DOH has done a very good job of developing and managing the clinic network. Unfortunately, the current funding is not adequate to the overall mission and objectives for the occupational health clinics. Therefore, the Committee recommends that funding for the clinic network should receive an annual inflationary increase to stay current with the medical care services inflation and the increase in the number of patient visits requiring ongoing treatment (see Section F). This represents less than a 1 percent increase from the total §151 assessment, which should not be reflected as any increase in workers' compensation costs for employers. This should include an increase to the NYS DOH to facilitate greater oversight of the fund. The impact of this increase, including costs to employers, should then be evaluated.
Outside services
In order to increase revenue coming into the clinics, the clinics should continue to develop appropriate outside services that are compatible with their basic state-supported mission. These may include contracts with employers for some occupational health services. These services should be consistent with assessed needs and should, in most cases, be self supporting.
New opportunities for the clinic network
Recent changes in federal and state programs also provide opportunities for the clinic network. The recent health reform legislation passed by Congress expands the requirements for preventive services. These new requirements provide an opportunity for the clinic network to expand the type of services offered by the clinic. The Committee recommends that the clinic network explore expanding their services to address these changes.
-
The effectiveness of the clinics in meeting the objectives
The network of occupational health clinics has done a very good job of addressing their original mission of providing high quality occupational medicine services, specializing in the diagnosis, treatment and prevention of occupational diseases. The NYS DOH has established a network of clinics providing occupational health services in all regions of the state, and these clinics are providing a high volume of occupational medicine services to people with occupational diseases. The public health approach has allowed the clinics to be in a unique position to respond to exposure episodes and disease clusters. Overall, this has been a very successful effort.
During its review, the Committee found some issues with the occupational health clinics that need to be addressed. Some of these are due to restraints on available funding; however, others could be overcome with administrative changes in the manner in which the clinics are managed.
Balance of services
In many of the clinics, a high proportion of the available clinical resources are being applied to the ongoing treatment of patients (particularly those with musculoskeletal problems). This reflects the low reimbursement rate from the WCB for medical services and the reluctance of other providers to provide these services. This makes referrals from the clinics to appropriate community providers after diagnosing work-related illnesses difficult. There also is a sense among some occupational health clinics that they provide better treatment for such patients than the patients might receive in the general community. This increase in the proportion of resources devoted to treatment has resulted in fewer resources being devoted to occupational disease diagnostic and preventive services and thus fewer new patients being seen by the clinics. The WCB has recently increased its reimbursement rates, though whether this will revive the interest of many physicians to provide treatment for occupational conditions is unclear. The NYS DOH should develop broad targets for the ratio of diagnostic visits to treatment visits and otherwise work with the WCB and the occupational health clinics to address this issue.
Limited preventive and educational services
The network is mandated to provide preventive services to help address occupational health problems in workplaces in their regions. Although the primary purpose of the occupational health clinics is to provide diagnostic services for occupational diseases, the clinics should also play a key role in other areas including prevention of occupational illnesses; education of health care providers, workers, and employers about occupational health; and research on occupational diseases and their prevention. These essential functions present enormous opportunities to amplify the impact of the NYS OHCN. However, provision of these services has been constrained by the lack of funding provided to the clinics. Concomitant with the increased funding, the Committee recommends an increased emphasis of the clinic network and the individual clinics on these areas including more coordination with the state and federal occupational health agencies.
Disparities in meeting needs and providing services
The Committee observed that there were significant differences in the clinical services and populations served by the different clinics. While some of this can be explained by regional differences, there are large differences even within similar regions. These differences are also reflected in the outreach efforts by the different clinics. Services and outreach focused mainly on selected groups or illnesses limit the access of people from other industries or with other illnesses to the clinics. While some of these differences may be justified, the observed disparities support the notion that there are continued unmet needs and limits the ability of the clinics to function as a network. Each clinic should use its needs assessments to determine if the clinic is providing necessary services to the identified high-risk populations.
Failure to meet basic objectives of the network
One of the clinics appears to only be providing general medical exams and has diagnosed very few occupational diseases in its regional population, which is likely to have the highest burden of occupational illnesses in the state based on the industries within their catchment area. This situation has gone on for many years with little change on the part of the clinic. The NYS DOH has met with the clinic and has identified specific steps the clinic needs to take. These will be included in the 2011-2012 contract to focus the clinic on taking immediate steps to address this problem. This process should be continued until the clinic refocuses its medical services and outreach to work-related illnesses.
-
Needs that may be met by one or more clinic
New York's economy is changing and these employment changes are reflected in the profile of the patients being seen in the clinics. In general, the occupational health clinics have adjusted their outreach to address regional needs for services and to address major groups in the work force needing services.
Representativeness of advisory boards
The clinic advisory boards should be representative of the local community with a mix of business, union, public health and community groups represented. The composition of these boards should be periodically reviewed and there should be consideration of new members to reflect the needs identified within the community.
Development of Return to Work programs
It has been well established that those who return to work as soon as medically possible after occupational injuries (e.g., being offered a modified duty or redesigning the work station), often have a better chance of staying in the workforce over the long term. Employers with effective Return to Work Programs typically see lower workers' compensation rates, higher morale, higher productivity and may be eligible to apply for one of the Workplace Safety and Incentive Programs offered under NYS Department of Labor Industrial Code Rule 60. The clinics supported under the NYS OHCN should consider developing return to work programs under explicit guidelines that they develop in consultation with their advisory boards. By having the capability of developing effective return to work programs and establishing competency in this area, the clinics could likely increase the number of on-site assessments. With greater awareness of the NYS OHCN and their ability to provide these services, injured workers could be evaluated sooner than later increasing their chances of accurate diagnoses and assessments thereby improving their chances of successfully re-entering the workforce.
-
Other issues as determined by the Oversight Committee
Problems with support from the parent institution
One of the clinics has had problems due to an antagonistic relationship with the medical school through which it receives its funding. This has been an ongoing problem for many years and has resulted in many administrative problems. The advisory board for this clinic expressed serious concerns about these problems. NYS DOH has worked with the school to improve the situation. This work needs to continue to assure appropriate steps are taken to address this issue.
Improved management of clinic network
The Committee believes that the NYS DOH has done a very good job of developing and managing the NYS OHCN. The Committee is recommending some improvements including addressing problems at two of the clinics as previously outlined. The Committee also recommends a more active management process. The current clinic contracts do not necessarily match the applications submitted by the clinics in response to the NYS DOH request for applications (RFA). The applications usually requested more funding than was awarded and hence usually promised more services than can be supported through the actual contact award. The Committee recommends that NYS DOH implement a procedure where the annual contracts include requirements for specific services in the major areas of clinic activity (i.e., clinical services, outreach, etc.) that is realistic given the amount of funding awarded to each clinic.
-
Implementation of recommendations in requests for applications
The Oversight Committee plans to use the recommendations from this report to provide advice to the NYS DOH in the writing of the next Request for Applications (RFA). This activity will occur in 2011 with a planned release of the RFA to occur in 2012 for the next five year funding cycle beginning in 2013.
Introduction
-
History of the Formation of the New York State Occupational Health Clinic Network
The New York State Occupational Health Clinic Network (NYS OHCN) is unique in the United States as a partially publicly funded, statewide, public health-based network offering clinical and preventive occupational disease services. It was established to address the need for specialized regional occupational health centers open to all state residents for the diagnosis and treatment of occupational diseases (Mount Sinai School of Medicine, 1987). An evaluation of the problem of occupational disease in New York State conducted by the Mount Sinai School of Medicine focused upon assessing the nature, magnitude and costs of occupational disease in New York State and developed recommendations for improving the recognition, prevention and treatment of occupational disease. The study estimated that occupational exposures were responsible for more than 35,000 new cases of disease and 5,000 to 7,000 deaths each year in New York State. The annual cost, in 1985 dollars, was estimated to be over $600 million for five disease categories - cancer, chronic respiratory disease, pneumoconioses , strokes and coronary heart disease, and fatal kidney disease. The majority of these costs were borne directly by the ill workers and/or their families.
The evaluation concluded that the state's resources, both in clinical facilities and professionals trained in occupational health, were inadequate to meet the public health need and recommended that the State of New York establish a statewide network of occupational health clinics. As a result, the New York State Legislature appropriated $1,000,000 from the general fund for six regional clinics in 1987. Funding for the clinics was transferred in 1989 to the Workers Compensation Board through an amendment of subdivision 2 of section 151 of the workers' compensation law.
-
Implementation of the New York State Occupational Health Clinic Network
The Network was established in 1987 with six regionally based clinics; it has since increased to ten regionally based clinics, with one additional specialty clinic. The clinics reside in a variety of institutional settings, including state and private medical schools, a healthcare insurer, and a local consortium of unions.
The NYS OHCN was established to achieve five main goals:
- to contribute to the quantification and description of the occupational disease burden in the state;
- to increase the accuracy of the diagnosis of occupational disease;
- to improve the treatment and management of occupational disease;
- to contribute to the prevention of occupational disease; and
- to strengthen and expand training programs in occupational health for professionals at all levels.
The clinics employ multidisciplinary teams of physicians, nurses, industrial hygienists, health educators and social workers trained in occupational health, to perform a variety of prevention activities as well as to provide clinical services. Staff is able to provide diagnosis and basic treatment for the full range of occupational diseases, along with evaluating the work conditions of the patients to determine whether co-workers are at risk and to improve the workplace environment. The clinics are open to anyone in New York State with a potential work-related illness. A sliding fee scale assures access for those without health insurance. Receiving funding from New York State allows clinic staff to spend more time with each of their patients than typical health care facilities.
Figure 1. Location and Catchment Areas of the New York State Occupational Health Clinics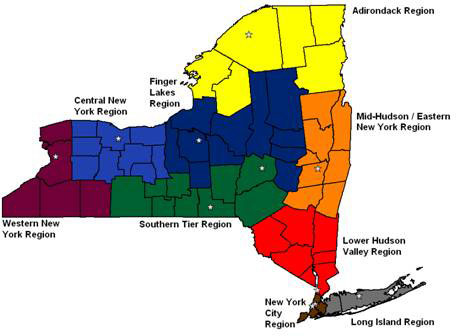
The clinics are located throughout the state in order to meet specific regional needs with two clinics located in the New York City region (Figure 1). In addition, legislation was enacted (Article 39 of the Public Health Law, PHL) that established a clinic to provide services in the area of agricultural safety and health (the New York Center for Agricultural Medicine and Health, NYCAMH). While occupational medicine practice is generally similar through all regions of the United States, integration of practice with specific local needs is desirable. Therefore, each clinic maintains a local advisory committee consisting of local businesses, organized labor, the medical community, local elected officials, community and/or health organizations, environmental groups and government representatives from federal, state and local health and labor offices. These boards reach into their own communities to raise awareness of clinic services and learn more about local needs. Each clinic also focuses on the high-risk industries and occupations within their area. When overlap of these services are identified, the Network works together to meet the general needs of New York workers.
Administrative and scientific oversight of the NYS OHCN is provided by the New York State Department of Health (NYS DOH). Quarterly meetings are held that include the medical directors and other professional staff from each clinic, as well as NYS DOH representatives. The day-long meetings are used to discuss a variety of administrative, medical and public health issues, and to enhance collaboration and help identify emerging occupational health risks. The clinics submit quarterly status reports to the Department that summarize their activities for the preceding three months; and each clinic submits an annual report that provides a more comprehensive summary of their activities for the previous year. Information on each patient visit, stripped of patient identifiers to ensure confidentiality, is provided to the NYS DOH. Each clinic enters data on all visits that occur at their clinics and satellite offices and this information is automatically uploaded to a NYS DOH secure server. The NYS DOH conducts quality control of the data and, when necessary, the clinics are responsible for making appropriate corrections to their data. These data are used to identify hazards, risk factors and trends; direct resources on emerging problems; create prevention strategies; and evaluate the success of various interventions.
Requests for Applications for clinic funding are issued every five years, and after a competitive process with review from both NYS DOH reviewers and external individuals, contracts are awarded for five-year periods. In 1992, contracts were awarded to eight clinics; then in 2008, the number of contracts awarded was expanded to 10 clinics plus the agricultural specialty clinic.
-
Occupational Health Clinics Oversight Committee
The Oversight Committee was created by Section 2490 of the PHL. The PHL indicates that the Oversight Committee is to be comprised of 15 appointees. Thirteen positions are currently filled. These include representatives from the NYS DOH, the Department of Labor (DOL), the Workers Compensation Board (WCB), nominees from the American Federation of Labor - Congress of Industrial Organization (AFL-CIO) and from the Business Council.
The Committee was specifically charged with making recommendations to the Governor and the legislature regarding:
- statewide needs to be met by the network;
- coordination of clinic activities with not-for-profit, private sector concerns and state agencies, including but not limited to an evaluation of current jurisdictional and oversight responsibilities;
- coordination and sharing of clinic resources and services;
- dissemination of research results and educational information;
- identification of funding sources for the network;
- the activities of the clinics and their effectiveness in meeting the objectives as set forth in statute and in clinic-specific contracts with the state;
- local, regional, occupation or business-sector specific needs that may be met by one or more clinic;
- other issues as determined by the Oversight Committee; and
- incorporation of provisions to implement its recommendations in requests for applications for state funding for occupational health clinics.
The Oversight Committee was originally authorized in 1989 through PHL 2490. In 2008, simultaneous with an increase in funding appropriated to the NYS OHCN, the Committee was established. Appointments were initiated in 2009 and a quorum existed by September 2009. The first meeting was held in January 2010 and the Committee has subsequently met in person quarterly, with two additional meetings by conference call. In order to learn more about the network, the Committee heard from the medical directors of each clinic and from a representative of each clinic's advisory board. The Committee also heard from the Acting Medical Director for the NYS Workers' Compensation Board (WCB), and from the director of the public employee division of the NYS AFL-CIO. All meetings were open to the public. A time period devoted to take testimony was provided in two of the meetings. All meeting announcements were posted on the NYS DOH public website prior to the meetings.
NYS DOH responded to requests for information from Committee members through a private website that allowed communication, file storage, and discussion. Background information in the form of the original Mount Sinai report (Mount Sinai School of Medicine, 1987), the summary of the clinic data from 1988 through 2003, and the most recent Request for Application was provided. Clinic-specific information including copies of the clinics' quarterly and annual reports; advisory board membership lists, meeting agendas and minutes; listings of peer-reviewed publications from the clinics, educational materials developed by the clinics, success stories, and examples of collaborations between the clinics were posted on the website. The successful applications from the last funding cycle in 2008 were also provided.
Sustaining Access to Occupational Medicine Expert Care: Continued Need for Occupational Health Clinic Network
-
Statewide Needs to be Met by the Network
There are over nine million workers in New York State, of whom six percent are self-employed; 53 percent are male and 15 percent are of Hispanic origin (US Department of Labor, 2011). Figure 2 displays the distribution of civilian employment in New York State by industry of employment.
According to the Bureau of Labor Statistics, there were an estimated 181,100 work-related injuries and illnesses in New York State in 2007, but this number is known to be severely underestimated (US General Accounting Office, 2009). The rate of work-related injuries and illnesses, by industry, is also displayed in Figure 2. Workers employed in the public sector, including police, corrections, nursing home and health care workers, experience the highest rate of work-related injuries, and also represent the second highest employment in New York State. Other high-risk industries include transportation, construction, and education and health services – all of which employ a large number of New Yorkers. Over 14,000 work-related hospitalizations occur annually, but again, research suggests that this represents less than one-half of the true number of work-related hospitalizations (unpublished data, NYS DOH). Over 200 traumatic occupational fatalities occur every year. In 2007, there were 3.537 billion dollars spent on Workers' Compensation benefits in New York State (National Academy of Social Insurance, 2010).
Figure 2. Number of Employees and Incidence Rate Per 100 Full-Time Workers of Non-Fatal Occupational Injuries and Illnesses, by Industry in New York State, 2009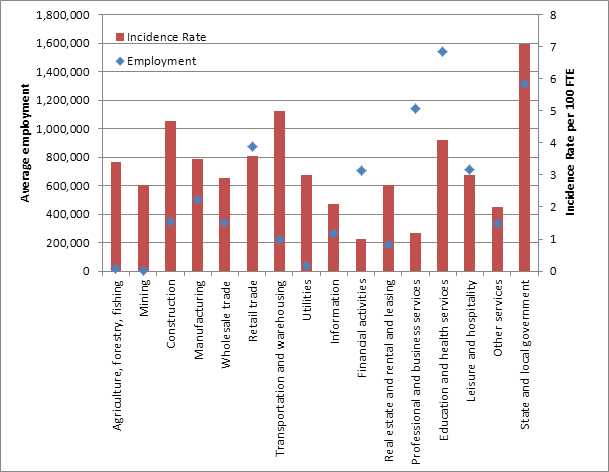
At the time that the clinic network was established, there was a shortage of occupational medicine specialists in the state. Most were employed by private industry (either directly or under contract), and people with occupational diseases (or suspected of having work-related illnesses) had very few clinical resources available to them for the diagnosis of occupational diseases. Without the availability of these services, these patients had difficulty learning whether their health problems might be related to work and establishing workers' compensation claims for these illnesses. Health insurance companies would often deny such claims (personal or group health insurance does not cover work-related illnesses or injuries) leaving the ill person with little recourse other than paying for the diagnostic and treatment services themselves.
The 1987 Mt. Sinai report also documented (to the extent possible with the available surveillance data) the high burden of occupational illnesses among New York State residents. Occupational diseases such as asbestosis, silicosis, lead poisoning, carpal tunnel syndrome, occupational cancers, and other chronic occupational illnesses were prevalent among New York State residents, and many of the hazards contributing to these illnesses were still common in New York State work sites. Prevention of these hazards was hampered by the failure to diagnose or conduct surveillance for these occupational diseases due to the dearth of occupational medicine resources throughout New York State.
These fundamental problems continue in New York. There is still not an adequate number of occupational medicine physicians in the state. In 2007, there were 116 board-certified occupational medicine physicians, of whom some are retired. Occupational safety and health professionals are increasingly working for consulting firms that provide safety and health services on a contractual basis, and most continue to work directly for employers or under contract with employers to provide occupational health services (Institute of Medicine, 2000). The sole occupational medicine physician training program in the state, administered at Mount Sinai School of Medicine, graduates fewer occupational medicine physicians annually at present than in 1987 (Mount Sinai School of Medicine, 1987). Without the NYS OHCN, many people with occupational illnesses would have difficulty finding a well-trained physician to diagnose and treat their illness and to help them navigate the still difficult workers' compensation system. There has also been a steady decline in New York State in the number of other occupational safety and health professionals including board-certified occupational health nurses, industrial hygienists, safety engineers and other safety health professionals (Council of State and Territorial Epidemiologists, 2011). There is no recent information about teaching of occupational health in medical schools in the United States; however, the last survey in 1992 found that only 60 percent of medical schools required occupational health as part of the curriculum with an average of six hours of teaching (Burstein, 1994), suggesting that the majority of physicians may not be able to successfully recognize, treat or prevent work-related illnesses and injuries.
Although there have been significant shifts in employment patterns in New York State since 1987, a significant number of New York State residents continue to work in jobs with occupational health hazards that put them at risk of developing occupational related illnesses. Due to the characteristic long latency between exposure and subsequent onset of chronic occupational disease, many people who worked in "older" industries are still at risk of developing serious occupational illnesses even though they may not have been exposed for many years. The contribution that the clinic network makes for occupational disease diagnosis, treatment, and prevention continues to fill a unique and vital need in New York State.
-
Coordination of Clinic Activities with Not-For-Profit, Private Sector Concerns and State Agencies, Including but not Limited to an Evaluation of Current Jurisdictional and Oversight Responsibilities
The NYS DOH has done a very good job in developing and managing the network of occupational health clinics. The data portrait of the clinics assembled by NYS DOH is excellent. The structure for communication and information flow among the clinics and NYS DOH is very useful. The requirement for local advisory boards has been very helpful in ensuring that the clinics are responsive to their core mission and to local needs. The NYS DOH has faced difficulties due to funding limitations, and the diversity of institutions that operate these clinics.
The NYS DOH has funded the clinics through contracts that are awarded through a competitive Request for Applications (RFA) process every five years. Given the paucity of occupational medicine specialists and services and the diverse nature of the mission of these clinics, there has been relatively little competition for the contracts. While this might be expected, the lack of competition can stifle innovation and lead to poor performance on the part of some individual clinics. There are concerns about whether the contracts with some clinics should be renewed or maintained. These challenges place a greater onus on the NYS DOH to use the RFA and contract management process to ensure that the clinics receiving the awards fulfill the mission of the clinics.
Recommendation
Coordination with other agencies. In order to fulfill the mission of the NYS OHCN, coordination between NYS DOH and other state agencies could be helpful. In particular, NYS DOL and the WCB could benefit from more involvement with the clinic network and, at the same time, be helpful to the clinics. The Committee recommends that NYS DOH and other state agencies take steps to work more closely with each other on the occupational health clinic program. Examples of activities that would be mutually beneficial would be training administrative law judges in the use of the WCB Medical Treatment Guidelines; designing and providing medical management for return-to-work programs for employers; and providing information about the clinics to prospective patients and employers.
-
Coordination and Sharing of Clinic Resources and Services
As described earlier, NYS DOH meets with the members (i.e., medical personnel and administrators) of the clinics every quarter. In general, at each meeting the clinics rotate in presenting a case report that is used to educate the other clinics about unique issues being encountered. In addition, there is often a discussion of sentinel events where the clinics can share information about interesting cases and request input from the other clinics about appropriate follow-up for their patients. Prior to each meeting, the required quarterly reports are shared with the other clinics, and there is time during lunch to allow the clinic members to discuss issues with each other.
A groupsite has been created on the internet that allows for sharing of documents between the clinics. The site is available only to the clinics, and each member of the site is allowed to post information they believe is relevant to the other clinics. Minutes of meetings, quarterly reports, and discussion groups are all available on this site.
The clinics have worked together on numerous projects. A partial list of these is provided below:
- Hazardous Waste Training: For the past seven years, three clinics have collaborated to provide over 20 classes of eight-hour update trainings annually to approximately 450 unionized operating engineers.
- Pesticide Specialist Training: Three clinics presented lectures at a statewide joint labor-management conference regarding health effects associated with pesticide exposure. Over 200 people attended these lectures.
- Education on the Health Show: The Health Show ran a series of 11 shows on occupational health with interviews conducted with occupational health experts. This series showcased the clinic network. The Health Show is a nationally syndicated weekly public radio program produced by the National Productions unit at Northeast Public Radio. It can be heard on nearly 200 public radio and ABC radio stations around the country reaching approximately 400,000 people. The program is also heard in 138 countries on U.S. Armed Forces Radio. The Health Show covers all aspects of modern health: prevention, treatment, research, administration and more.
- Collaboration with the New York Center for Agricultural Medicine and Health: Various clinics have utilized the services of the specialty agricultural clinic, including training fishermen on health and safety, and conducting education and outreach and running clinics with farmworkers and migrants. These activities reached approximately 360 people.
- Staff Assistance: The clinics have assisted each other when there are staff shortages and have sent new staff to other clinics for training purposes. Medical directors have both gained experience and have assisted in providing direction to other clinics with new directors; and staff has received training from other clinics for activities such as firefighter programs.
Recommendation
Consistency of services. The Committee notes the sharp differences in distribution of frequencies of patient diagnoses by clinic. This spectrum of patients evaluated and the services emphasized by each of the clinics reflects in part the interests and history of the clinic and may not necessarily reflect the broad set of needs of the local community. Needs assessments should be completed at least once during the five year contract cycle by each clinic. Each clinic should include one project annually focused upon reaching a high risk population in their catchment area.
-
Dissemination of Research Results and Educational Information
One of the goals of the clinic network is to improve the treatment and management of occupational disease in New York State. Network staff collaborated to develop nine clinical practice reviews, which were published in the January 2000 issue of the American Journal of Industrial Medicine. These were designed to assist clinicians in the diagnosis, treatment and prevention of the following occupational conditions:
- Medical examination for asbestos-related disease
- Clinic evaluation and management of lead-exposed construction workers
- The diagnosis and management of solvent-related disorders
- Clinical evaluation and management of work-related carpal tunnel syndrome
- Evaluation and management of chronic work-related musculoskeletal disorders of the distal upper extremity
- Evaluation and management of occupational low back disorders
- Occupational hearing loss
- Clinic evaluation, management and prevention of work-related asthma
- Medical evaluation for respirator use
These reviews integrated primary, secondary and tertiary disease prevention approaches into the clinical model by emphasizing a team approach to the diagnosis and treatment of occupational diseases.
Each clinic is required to have an advisory board that assists in setting policy for that clinic. This has allowed for a network of partners to be developed that are useful for disseminating information into the working community. These partnerships, along with other outreach endeavors, have allowed the clinics to enlist communities in prioritizing occupational health problems, determining and evaluating potential interventions, and then actually testing these interventions with the goal of widespread dissemination.
The clinics develop educational materials to meet their particular needs. A partial list of these materials has been collated and is available in Appendix A. These materials show the breadth of work with which the clinics are involved. The clinics also publish numerous articles in peer-reviewed journals. A list of the articles published from 2004 is provided in Appendix B.
Recommendation
Sharing of materials. The clinics should exercise leadership in professional education and clinical research. To aid in this process, there should be a more efficient method of sharing educational materials between the clinics that will allow them to develop and print materials, as needed, in a more cost-efficient manner.
-
Identification of Funding Sources for the Network
Workers' Compensation Law (WCL) § 151 provides for the administrative expenses of the WCB. This statutory provision requires the WCB to annually prepare an itemized statement of its expenses and authorizes the Chair to assess upon and collect a proportion of such expenses from each insurance carrier, the state insurance fund and each self-insurer, including group self-insurers, writing workers' compensation insurance in New York State. Included in the WCL §151 assessment is an "additional sum as may be certified to the chair and the department of audit and control… for the New York state occupational health clinics network…" [WCL §151 (2) (a)].
Table 1. Administrative Assessments for New York State
Occupational Health Clinic NetworkYear Appropriation YTD Transfers 2007 – 2008 $6,108,000.00 $6,275,372.65 2008 – 2009 $6,141,200.00 $5,954,326.82 2009 – 2010 $10,188,000.00 $10,961,760.62 2010 – 2011 $10,135,900.00 $9,861,421.27 Each year, the NYS DOH makes a budget request for the clinics and when the final amount is approved and certified, the WCB includes it in its §151 assessment bills. The WCB does not set the budget amount and has no authority to increase or decrease the funds. All assessment money collected is transferred to the NYS DOH. In essence, the WCB acts as an assessment and collection agent for the NYS DOH. Table 1 represents monies appropriated and collected by the WCB for the Occupational Health Clinics Network during the past four years.
The appropriation for the clinics has been approximately $10 million for the past two fiscal years. The differences in the appropriated amounts and the transferred amounts are due to payment variances by the insurers and are adjusted from year to year.
The budget for the occupational health clinics has not kept up with the demands and needs for services from the clinic. The budget for the network was flat for many years, and the increased funding provided in the 2009 state budget is not adequate to fully support the efforts of the network. Other sources of funding could be helpful, but these sources also have limitations. For example, potential sources (payments from the WCB for treating patients in the clinics) are often inadequate to cover costs. The clinics currently receive additional reimbursement from the WCB, health insurance, and other private sources (e.g., employers). This ranges from minimal to approximately one-third of their overall budget for clinical services. There are large differences among the clinics in how much additional reimbursement they seek and receive. There are outside sources of income for the clinics that could be pursued without diminishing the overall mission of the clinics. These include contracts with employers for some occupational health services. The WCB may also provide opportunities including assisting in return to work evaluations and helping the employer establish a return to work program. These additional services need to be compatible with the basic mission of the clinics and in a manner that does not impact their mission. The Committee also recommends that in most cases such additional services should be self supporting (i.e., the state funding for the clinics should not support these services). Figure 3 displays the annual funding of the NYS OHCN since 1991 compared to what the funding should have been if it kept up with the cost of medical care services inflation according to the Bureau of Labor Statistics (US Department of Labor (a), 2011).
Figure 3. Annual Occupational Health Clinic Network Funding vs. Inflation Adjusted Funding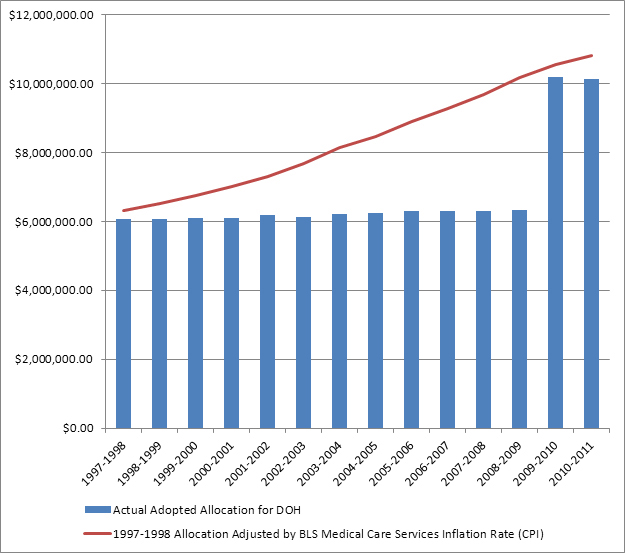
Recommendations
Increased funding. The occupational health clinics continue to address a significant need for occupational health services in New York State that is not being otherwise addressed. The NYS DOH has done a very good job of developing and managing the clinic network. Unfortunately, the current funding is not adequate to the overall mission and objectives for the occupational health clinics. With additional funding, the clinics could provide more clinical services and better educational, outreach, and preventive services. Therefore, the Committee recommends that funding for the clinic network should receive an annual inflationary increase to stay current with the medical care services inflation and the increase in the number of patient visits requiring ongoing treatment (see Section F). This represents less than a 1 percent increase from the total § 151 assessment, which should not be reflected as any increase in workers' compensation costs for employers. This should include an increase to the NYS DOH to facilitate greater oversight of the fund. The impact of this increase, including costs to employers, should then be evaluated.
Outside services. In order to increase revenue coming into the clinics, the clinics should continue to develop appropriate outside services that are compatible with their basic state-supported mission. These services should be consistent with the needs assessment (described above) and should, in most cases, be self supporting . The recent changes to the NYS Workers' Compensation Law provide an opportunity to develop new services that will also assist in the implementation of that law.
New opportunities for the clinic network. Recent changes in federal and state programs also provide opportunities for the clinic network. The WCB is currently implementing medical guidelines and other changes required by legislation passed in 2007. There are opportunities for the clinic network to assist in this implementation and possibly to provide new services such as return to work evaluations. The recent health reform legislation passed by Congress expands the requirements for preventive services. These new requirements provide an opportunity for the clinic network to expand the type of services offered by the clinic. The Committee recommends that the clinic network explore expanding their services to address these changes.
-
Activities of the Clinics and Their Effectiveness in Meeting the Objectives as Set Forth in Statute and in Clinic-Specific Contracts with the State
The network of occupational health clinics has done a very good job of addressing their original mandate. The NYS DOH has established a network of clinics providing occupational health services in all regions of the state, and these clinics are providing a high volume of occupational medicine services to people with occupational diseases. Occupational medicine resources have been established in major medical centers that previously did not have such comprehensive services. Within the constraints of their present resources, they are also providing outreach and preventive services within their regions. In 2010, the clinic network provided medical services to 6,355 patients of which 6,096 were occupationally related. Overall, this has been a very successful effort. The centers have all established advisory boards that represent their regions and help to ensure that regional needs are being addressed.
There are numerous stories detailing the success of the clinics in identifying, treating and assisting patients with occupational disease. Below are a few of these stories.
- A worker/patient had been employed for 13 years climbing communications towers. Due to many serious injuries related to this physically demanding and dangerous work, the patient could no longer safely work in that occupation. While completing a bachelor's degree in political science, the patient's interest in worker health and safety policies led to an internship with one of the clinics and the development of a project for which he has received one of the nation's highest awards for occupational health and safety, the Tony Mazzochi Award by the Occupational Health Section of the American Public Health Association. The Tall Towers Health and Safety Project has brought together workers from this growing industry to develop a safety and health agenda and strategy for the industry.
- A tip regarding massive wage violations led two clinic outreach workers to uncover a labor trafficking operation of 19 H-2B (non-agricultural temporary worker program) food service workers (lawfully present in the United States). The clinic conducted physical examinations on about half the workers, and found they suffered from dehydration, hunger, insect bites, burns, musculoskeletal problems, and health problems worsened by their working conditions. The clinic was able to marshal state and federal agencies to address the situation, which resulted in the arrest of the trafficker, who had been conducting his activities in New York for about a dozen years.
- Workers at a large industrial laundry reported routinely finding and getting stuck with needles hidden in sheets and other laundry originating in area hospitals. In addition, there were worker concerns over excessive noise from a row of large dryers. The clinic conducted a site visit, measured noise levels, interviewed workers, observed the work process, and talked with management. While recommendations were made to the employer to bring them into compliance, the employer chose not to implement any of the recommendations. Therefore, an OSHA complaint was filed. OSHA's inspection revealed numerous violations resulting in significant fines, and workplace changes to make this dangerous work safer.
- A woman who was a long time Department of Motor Vehicles employee presented to a clinic with chronic neck, shoulder and arm problems. Almost all of her work day was spent on a computer. The clinic industrial hygienist was able to perform a workplace evaluation and identified a number of problems with the ergonomic set up of the patient's work setting. These were corrected and the patient was able to continue working with reduced symptoms. Over a period of years, this process was repeated several times. The patient's symptoms were exacerbated when changes in her workstation were instituted by the employer. They were re-evaluated by the industrial hygienist and further modifications were made. As a result of this long-term relationship and process, this particular worker was able to stay on the job for at least 10 years longer than she would have been able to if no workplace changes had been made.
- A dental hygienist at a community health center had been diagnosed with asthma, but still needed to use her rescue bronchodilator inhaler several times a day. Evaluation at the clinic showed her asthma to be work-related, associated with latex exposure. Because she could not work and had become destitute, the clinic negotiated with the union to get her placed on short-term disability until her Workers' Compensation case was established. The clinic was then able to work with her employer to thoroughly clean the health facility and replace all powdered latex gloves with vinyl or nitrile gloves. This allowed the patient to return to work, and after three years, she had no further asthma symptoms.
- One clinic medical director provides occupational safety and health education to the local, state and national firefighting communities. Educational workshops and presentations have been provided at the following conferences: NYS Professional Firefighters Association; NYS Association of Fire Chiefs; Fire Department Instructors on preventing occupational illness and injury.
- Various clinic medical directors have assisted the WCB in writing the medical treatment guidelines that were released in December 2010. In addition, two of the clinic medical directors have also been acting medical directors for the WCB.
- The clinical practice reviews written by the network (American Journal of Industrial Medicine, 2000) were used by the clinic network to guide clinical practice and as a tool to foster quality of care and consistent practice. A quality assurance/quality improvement (QA/QI) program was developed and implemented to enable the clinics to evaluate the level and consistency of care provided in the diagnosis of each of those conditions chosen for the clinic practice reviews. The QA/QI process also enabled the network to evaluate the quality and consistency of case management and the degree to which prevention is integrated in to the clinics' practices.
- Various clinics have been involved in working with migrant farmworkers. They provide general and preventive health services for conditions such as back, neck or arm strain, skin rashes, eye injuries and respiratory problems. The specialty agricultural health clinic developed a manual to assist health care professionals in the examining room. This manual provides information ranging from cultural differences of various migrant groups to descriptions of specific commodity work and the patterns of injury documented for each commodity. Treatment guidelines for common problems are included, as are photocopy-ready patient information sheets in Spanish and Creole.
Disaster Response. The public health approach has allowed the clinics to be in a unique position to respond to exposure episodes and disease clusters. In the past decade, a few situations, as described below, have occurred where the clinics have made substantial contributions.
- World Trade Center Response
One illustration of the importance of the NYS OHCN was its rapid and multifaceted response to the World Trade Center terrorist attack. Occupational medicine physicians from the network recognized the potential respiratory illnesses that might result from exposure to the dust and smoke during the rescue and recovery work at the site. Within days after September 11, they began to treat patients who became ill as a result of exposure to the dust released during the collapse of the towers. They initiated medical studies to evaluate possible health problems among these workers. Once they started to document serious health problems, they expanded their efforts and (with federal and philanthropic funding) established a medical screening program for the thousands of workers who were exposed at the site. This effort was then expanded to include the other regional clinics who were able to provide services to rescue and recovery workers who had responded from their regions. This provided the basis for documenting serious occupational illnesses in thousands of these workers, and the effort has been expanded to include medical treatment for these workers funded by the federal government. The NYS OHCN provided a major expert resource for the needed diagnosis and treatment for these many workers. Without such a readily available resource, the health problems being experienced by the rescue and recovery workers might not have been so rapidly recognized, and the overall effort to establish the medical program needed for these workers would have been much more difficult. In addition, the prior coordination of the occupational health clinics as a network facilitated a collaborative and efficient clinical occupational health response to the demand for care from affected persons.
- Anthrax Response
Also in 2001, letters containing anthrax were mailed to a variety of locations in New York City along with other places in the United States. At least 22 people developed anthrax infections and five died from the exposure. The NYS OHCN assisted in developing training programs for postal workers. Thousands of workers were trained by the clinic staff.
- Respirator Training of Long-Term Care Facilities During the 2009 H1N1 Flu Pandemic
During the 2009 H1N1 influenza pandemic, the NYS DOH identified that the 639 long term care facilities in New York State needed training on respiratory protection issues. The clinic network was recruited to conduct needs assessments for those long term care facilities in their designated geographic regions and to provide any necessary training, medical assessments and fit testing associated with the appropriate use of respiratory protection and other personal protective equipment.
Recommendations
During its review, the Committee found some issues with the occupational health clinics that need to be addressed. Some of these are due to restraints on available funding; however, others could be overcome with administrative changes in the manner in which the clinics are managed.
Balance of services. In many of the clinics, a high proportion of the available clinical resources is being applied to the ongoing treatment of patients (particularly those with musculoskeletal problems). This reflects the low reimbursement rate from the WCB for medical services and the reluctance of other providers to provide these services. This makes referrals from the clinics to appropriate community providers after diagnosing work-related illnesses difficult. There also is a sense among some occupational health clinics that they provide better treatment for such patients than the patients might receive in the general community. This increase in the proportion of resources devoted to treatment has resulted in fewer resources being devoted to occupational disease diagnostic and preventive services and thus fewer new patients being seen by the clinics. The WCB has recently increased its reimbursement rates, though whether this will revive the interest of many physicians to provide treatment for occupational conditions is unclear. The NYS DOH should develop broad targets for the ratio of diagnostic treatment visits for the clinics and otherwise work with the WCB and the occupational health clinics to address this issue.
Limited preventive and educational services. The network is mandated to provide preventive services to help address occupational health problems in workplaces in their regions. Although the primary purpose of the occupational health clinics is to provide diagnostic services for occupational diseases, the clinics should also play a key role in other areas including prevention of occupational illnesses, education of health care providers, workers, and employers about occupational health, and research on occupational diseases and their prevention. These essential functions present enormous opportunities to amplify the impact of the NYS OHCN. However, provision of these services has been constrained by the lack of funding provided to the clinics. Concomitant with the increased funding, the Committee recommends an increased emphasis of the clinic network and the individual clinics on prevention and education including more coordination with the state and federal occupational health agencies.
Disparities in meeting needs and providing services. The Committee observed that there were significant differences in the clinical services and populations served by the different clinics. While some of this can be explained by regional differences, there are large differences even within similar regions. For example, two clinics focus much of their outreach and clinic services on firefighters while the other clinics see very few firefighters. A few clinics see mostly patients with musculoskeletal diseases while another clinic diagnoses and treats mostly patients with occupational pulmonary disease. These differences are also reflected in the outreach efforts by the different clinics. Services and outreach focused mainly on selected groups or illnesses limit the access of people from other industries or with other illnesses to the clinics. While some of these differences may be justified, the observed disparities support the notion that there are continued unmet needs and also limit the ability of the clinics to function as a network. Each clinic should use its needs assessments to determine if the clinic is providing necessary services to the identified high-risk populations.
Failure to meet basic objectives of the network. One of the clinics appears to only be providing general medical exams and has diagnosed very few occupational diseases in its regional population, which is likely to have the highest burden of occupational illnesses in the state based on the industries within their catchment area. Between 2005 and 2009, this clinic reported diagnosing only 14 patients with occupationally related illnesses. This clinic has also lacked an onsite fully trained director of occupational medicine. The current arrangement of oversight provided by a distant occupational medicine physician is not adequate. This situation has gone on for many years with little change on the part of the clinic. NYS DOH has met with the clinic and has identified specific steps the clinic needs to take. These will be included in the 2011-2012 contract to focus the clinic on taking immediate steps to address this problem. This process should be continued until the clinic refocuses its medical services and outreach to work-related illnesses.
-
Local, Regional, Occupation or Business Sector Specific Needs that May be Met by One or More Clinic
As mentioned above, New York's economy is changing. In the past decade, New York State has lost more than 250,000 jobs in manufacturing (County Business Patterns, 2008). Major industries such as steel manufacturing and leather tanning, which used to be major sources of employment in some regions of the state have downsized or virtually disappeared. To a lesser extent, new industries such as semiconductor manufacturing, with their own health hazards are replacing the older industries. These employment changes are reflected in the profile of the patients being seen in the clinics with a lower proportion derived from industrial and construction occupations and more coming from the firefighting, health care and other public administrative and service industries over the last few years. Table 2 displays the industries of employment for the clinic network patients during the first and last five years.
Table 2. Industries of Employment of New York State
Occupational Health Clinic Network Patients,
1988-1992 and 2006-2010Total Number of Patients 1988-1992 2006-2010 10,448 100% 20,127 100% Agriculture 140 1.3% 427 2.1% Mining 109 1.0% 48 0.2% Construction 1,969 18.8% 2,098 10.3% Manufacturing 1,747 16.7% 2,276 11.2% Transportation 921 8.8% 1,699 8.4% Wholesale 94 0.9% 272 1.3% Retail 226 2.2% 670 3.3% Finance, Insurance, Real Estate 292 2.8% 292 1.4% Services 2,900 27.8% 5,670 28.0% Public Administration 2,050 19.6% 6,502 32.1% The occupational health clinics have also adjusted their outreach to address regional needs for services and to address major groups in the work force needing services. For example, the clinic located in the mid-Hudson region has been assisting local fire departments with their required medical examinations. The Central New York Clinic has expanded its outreach in nearby areas. A major success of the NYS OHCN has been the development of the New York Center for Agricultural Medicine and Health in Cooperstown. In collaboration with other groups working on agricultural safety and health issues, this clinic has integrated clinical, research and education activities to develop outstanding occupational safety and health programs for agricultural workers throughout the state.
In recent years, occupational health disparities among groups based on race, ethnicity, and gender have received increasing attention (American Journal of Industrial Medicine, 2010). The population of New York is among the most diverse in the country and likely expresses similar disparity challenges that have been documented elsewhere. The NYS OHCN should make this a priority in the coming five years.
Recommendations
Representativeness of advisory boards. The clinic advisory boards should be representative of the local community with a mix of business, union, public health agencies and community groups represented. The composition of these boards should be periodically reviewed and there should be consideration of new members to reflect the needs identified within the community.
Development of Return to Work programs. It has been well established that those who return to work as soon as medically possible after occupational injuries (e.g., being offered a modified duty or redesigning the work station), often have a better chance of staying in the workforce over the long term. Employers with effective Return to Work Programs typically see lower workers' compensation rates, higher morale, higher productivity and may be eligible to apply for one of the Workplace Safety and Incentive Programs offered under NYS Department of Labor Industrial Code Rule 60. The clinics supported under the NYS OHCN should consider developing return to work programs under explicit guidelines that they develop in consultation with their advisory boards. By having the capability of developing effective return to work programs and establishing competency in this area, the clinics could likely increase the number of on-site assessments. With greater awareness of the NYS OHCN and their ability to provide these services, injured workers could be evaluated sooner than later increasing their chances of accurate diagnoses and assessments thereby improving their chances of successfully re-entering the workforce.
-
Other Issues as Determined by the Oversight Committee
Recommendations
Problems with support from the parent institution. One of the clinics has had problems due to having an antagonistic relationship with the medical school through which it receives funding. This has been an ongoing problem for many years and has resulted in many administrative problems. The advisory board for this clinic expressed serious concerns about these problems. The problems with lack of support from the medical school were evident to the Oversight Committee who heard from the clinic director, the advisory committee and the Chair of the Department of Preventive Medicine at the medical school. Despite strong letters of support from the medical school for the funding application, the medical school does not appear to be providing the level of support needed for the clinic to fully meet its mandate. NYS DOH has worked with the school to improve the situation. This work needs to continue to assure appropriate steps are taken to address this issue.
Improved management of clinic network. The Committee believes that the NYS DOH has done a very good job of developing and managing the NYS OHCN. The Committee is recommending some improvements including addressing problems at two of the clinics (outlined above). The Committee also recommends a more active management process. The current clinic contracts do not necessarily match the applications submitted by the clinics in response to the NYS DOH RFA (the applications usually requested more funding than was awarded and hence usually promised more services than can be supported through the actual contact award). The Committee recommends that NYS DOH implement a procedure where the annual contracts include requirements for specific services in the major areas of clinic activity (i.e., clinical services, outreach, etc.) that is realistic given the amount of funding awarded to each clinic. Although this will require more work on the part of the NYS DOH and clinic staff, it will provide better accountability.
-
Incorporation of Provisions to Implement Its Recommendations in Requests for Applications of State Funding for Occupational Health Clinics
The Oversight Committee plans to use the recommendations from this report to provide advice to the NYS DOH in the writing of the next Request for Applications (RFA). This activity will occur in 2011 with a planned release of the RFA to occur in 2012 for the next five year funding cycle in 2013.
References
American Journal of Industrial Medicine. The Diagnosis and Treatment of Occupational Diseases: Integrating Clinical Practice with Prevention. 2000. 37(1):1-157.
American Journal of Industrial Medicine. Special Issue: Occupational Health Disparities. 2010. 53(2):81-215.
Burstein JM, Levy BS. The Teaching of Occupational Health in US Medical Schools: Little Improvement in 9 Years. American Journal of Public Health. 1994. 84(4):846-849.
Council of State and Territorial Epidemiologists. Occupational Health Indicators. Available: https://www.cste.org/group/OHIndicators . [accessed 24 January 2011].
County Business Patterns 2008. Available: https://www.census.gov/data/datasets/2008/econ/cbp/2008-cbp.html . [accessed 24 January 2011].
Institute of Medicine. Safe Work in the 21st Century: Education and Training Needs for the Next Decade's Occupational Safety and Health Personnel. 2000.
Mount Sinai School of Medicine. Occupational Disease in New York State. Proposal for a Statewide Network of Occupational Disease Diagnosis and Prevention Centers. Report to the New York State Legislature. February 1987.
National Academy of Social Insurance. Workers' Compensation: Benefits, Coverage, and Costs, 2008. September 2010.
United States Department of Labor, Bureau of Labor Statistics. Geographic Profile of Employment and Unemployment, 2009. Available: https://www.bls.gov/opub/geographic-profile/home.htm . [accessed 24 January 2011].
United States Department of Labor(a), Bureau of Labor Statistics. Consumer Price Index, All Urban Consumers (Current Series). Available: https://www.bls.gov/news.release/cpi.toc.htm . [accessed 24 January 2011].
United States Government Accountability Office. Workplace Safety and Health. Enhancing OSHA's Records Audit Process Could Improve the Accuracy of Worker Injury and Illness Data. GAO-10-10. October 2009.
Appendix A. Partial List of Educational Materials Developed by the NYS Occupational Health Clinic Network
Lectures
- Asbestosis - Master of Public Health
- Assessing Causation and Disability - Family Medicine Residency 3rd Year
- Beryllium, Welding and Hard Metal Disease - Master of Public Health
- Cardiovascular Occupational Disease - Master of Public Health
- Clinical Epidemiology and Preventive Medicine - Medical students
- Coal Workers Pneumoconiosis - Master of Public Health
- Cost Analysis/Legal Responsibility - Master of Public Health
- Environmental Detectives - Master of Public Health
- Environmental and Occupational Toxicology – Medical students
- Ergonomics and Industrial Hygiene - Master of Public Health
- Ergonomics Program Elements - Master of Public Health
- Hazard Identification and Interpreting Injury and Illness Data - Master of Public Health
- Hazard Identification/Lifting - Master of Public Health
- Heavy Metals - Master of Public Health
- History of Occupational Medicine and the Role of Labor - Master of Public Health
- Identifying Occupational Disease - Medical School
- Incident/Accident Investigation - Master of Public Health
- Introduction to Construction - Master of Public Health
- Introduction to Environmental and Occupational Health - Master of Public Health
- Introduction to Occupational Medicine – Toxicology class lecture
- Introduction to Occupational Pulmonary Diseases - Master of Public Health
- Low Back Pain Outcomes After Pain Management Referral - Grand Rounds
- Making a Case for Safety - Master of Public Health
- Medico Legal Aspects of Asbestos and Pulmonary Occupational Disease – Master of Public Health
- Migrant and Seasonal Farmworkers – Anthropology class lecture
- Nuts and Bolts of Workers' Compensation - Grand Rounds
- Occupational and Environmental Lung Disease - Master of Public Health
- Occupational Gastrointestinal Disease - Master of Public Health
- Occupational Hematology - Master of Public Health
- Occupational Infectious Disease - Master of Public Health
- Occupational Kidney Disease - Master of Public Health
- Public Health Response to Disaster: WTC Medical Program – Master of Public Health
- Qualitative Epidemiology as a tool in Occupational Epidemiology – Master of Public Health
- Respiratory Hazards in Agriculture – Animal Science Class
- Safety History and Scope of Current Problem - Master of Public Health
- Safety in Various Trades - Master of Public Health
- Silicosis - Master of Public Health
- Solvents - Master of Public Health
- Stress in the Workplace - Grand Rounds
- Supporting the Safety Process: Labor Unions/Management Committees - Master of Public Health
- Taking an Occupational History - Master of Public Health
- Work-Related Musculoskeletal Disorders - Master of Public Health
- Workers' Compensation Reform: Implications for Physicians - Grand Rounds
Presentations
- 30 Year Old Mason with Dyspnea
- A Case of Parkinson's Disease
- Acute, Subacute and Chronic Effects of Smoke Inhalation
- Advocating for Injured Workers in Workers' Compensation
- The Aging Workforce and Chemical Exposures
- Agricultural Hazards Awareness Training for Firefighter and EMS Personnel
- Agricultural Safety Hazard Awareness
- Anhydrous Ammonia Safety
- The ANSI Standard on Use of Respiratory Protective Equipment
- Asbestos Abatement Training
- ATV Safety
- Asbestos Awareness Training
- Asbestos, Silica and Lead
- Avian Influenza
- Back Injury Prevention
- Barriers to Occupational Health for Low Wage Workers
- Basic First Aid
- Bloodborne Pathogens
- BP Oil Spill: Potential Health Hazards for Workers and Volunteers Involved in the Clean Up Effort
- Cardiovascular Disease
- Careers in Occupational Medicine
- Cattle Treatment Safety
- Chainsaw Safety
- Characteristics of Work-related Asthma Patients Seen by the Occupational Health Clinical Center
- Clinical Guidelines for Adults Exposed to the World Trade Center Disaster
- Cold Weather Safety
- Computer Vision Syndrome
- Confined Spaces in Agriculture
- CPR/AED for Adults, Children, and Infants
- Dealing with Pre-ROPS Tractors: Exploring the Viability of a Tractor Trade-in Program
- Diesel Exhaust Exposure for Operating Engineers
- Demystifying Indoor Environmental Quality
- Electronic Medical Records Suited for Occupational and Environmental Health
- Environmental and Physical Hazards in Agriculture
- The Experience of Occupational Injury
- Exposure Assessment Methods
- Fatigue at Work
- Food Borne Pathogens in the Dairy Industry
- Forklift Safety
- Framing the Future in Light of the Past: Living in a Chemical World
- Fungus and Bioaerosols Training
- Good Nutrition
- Green Cleaning Products
- H1N1 Swine Flu Prevention
- Hay and Forage Equipment Safety
- Hazard Communication
- Hazard Communication Standard for Dairy Farms
- Hazards in the Restaurant Industry
- HazMat Toxicology and Industrial Hygiene
- The Health Effects of Asbestos
- The Health Effects of Lead
- Health Effects of Solvent Exposure
- Health Hazards for Farmworkers
- Health Hazards from Incomplete Decontamination and Not Using Respiratory Protection
- Health Hazards in Hospitals
- Heat and Cold Stress
- Heat-Related Illness
- How Important are My Medicines?
- Hydrogen Cyanide
- Hypertension and the Firefighter
- Impairment Assessments and AMA Guides
- Impairment and Disability Assessment
- Indoor Environmental Quality: Prevention, Response and Remediation
- Industrial Hygiene in the Workplace
- Industrial Hygiene Training for NYC Transit Workers
- Is Your Boss Treating You Like a Slave?
- Know Your Health and Safety Rights
- Ladder Safety
- Lead Awareness
- Lower Back Pain Prevention & Safe Lifting
- Marking and Lighting of Agricultural Machinery
- Measuring Toxins in the Workplace
- Mechanical Hazards in Agricultural Machinery
- Medical Management of Blood Borne Pathogens
- Medical Surveillance for Lead Exposure
- Medical Surveillance for Operating Engineers
- More Than Meets the Eye: Aspects of the Impact of an Occupational Illness on Injured Workers
- MRSA
- Musculoskeletal Disease in Women Carpenters
- Musculoskeletal Injury Prevention of Low Back Pain
- Noise Induced Hearing Loss
- Noise Measurement and Engineering and Administrative Controls
- Occupational Asthma
- Occupational Disease and Medical Surveillance
- Occupational Disease Determining Causation: Case Studies
- Occupational Lung Disease
- Occupational Medicine for the Internist
- Office Ergonomics
- On-Farm Safety Surveys
- Orchard Ladder Safety
- OSHA's Guidelines for Nursing Homes
- The OSHA Lead Standard
- Packinghouse and Processing Line Safety for Vegetable Farms and Orchards
- Pandemic Awareness: A business perspective
- Patient Care Ergonomics for Health Care Workers
- PCB's and the Operator
- Performing Arts Music: Ergonomics and Musculoskeletal Disorders
- Personal Hygiene for Migrant Farmworkers
- Personal Protective Equipment for Farmworkers
- Pesticide Applicators: Cornell Cooperative Extension
- Pesticides and Parkinson's Disease
- Preparing Yourself for Surgery
- Preventing Back Injury in the Fire Service
- Preventing Tuberculosis in the Fire Service
- Prevention of Line of Duty Cardiac Deaths in the Fire Service
- Promoting Awareness, Identification and Prevention of Work-related Symptoms in a Mobile Migrant
- Workers' Clinic in Central New York
- Promoting Health and Safety through Ergonomic Design
- Recognizing Occupational Disease
- Reducing Take Home Pesticide Exposures
- Respiratory Disease in Agriculture
- Respiratory Protection in Construction
- Respiratory Protection Plan for Long-term Care Facilities on Long Island
- Rochester Automobile Dealers Association Safe*T Program
- Safe Handling of Dairy Cattle
- Safe Lifting and Carrying
- Safe Operation of Agricultural Machinery on Public Roadways
- Safe Operation of Farm Trucks on Public Roadways
- Safe Patient Handling
- Safe Use of Agricultural Tractors in Woodlots
- Sarcoidosis
- Screening Exams in Occupational Medicine
- Selecting and Using PPE for Pesticide Applications
- Sharps Safety for Healthcare Workers
- The Silica Toolbox Talks, Tools to Help You Prevent Overexposure to Silica
- Skidsteer Safety
- Slips, Trips, and Falls
- Slogging Through and Opting Out: Workers' Compensation in New York State
- Social Marketing of Tractor Rollbars
- Socioeconomic Disparities, Extended Work Hours and Musculoskeletal Disorders among Health Care Workers
- Strategies for a Safe School
- Stress Management
- Stress Reduction and Meditation
- Superpave – Safe Work Practices
- TB Awareness
- Topics in Workplace Safety and Health
- Tower Climbers Health and Safety Issues: New York Perspectives on 'The Most Dangerous Job in America'
- Tractor and Power-Take-Off Safety
- Train the Trainer - Respirator Use and Fit Testing
- Using Occupational Health Clinical Resources
- Worker Protection Standard – Worker
- Worker Protection Standard - Handler
- Workers' Compensation in New York State
- Workers' Compensation Issues
- Workers' Compensation Reform 2007
- Workers' Compensation Update and the New York State Medical Treatment Guidelines 2010
- Workplace Education
- Workplace Violence
- Workplace Walkaround Safety and Health Inspections
- Work-Related Musculoskeletal Disorders, Ergonomics, and Safe Lifting Techniques
- Worksite Wellness
Flyers/Brochures
- Clinic Specific Brochures
- A Guide for Healthy Work: Office Ergonomics
- Air Quality
- Allergies
- Animal Handling (English & Spanish)
- Ankle Sprains
- Bunker Silo Safety
- Carpal Tunnel Syndrome (English & Chinese)
- Children's Farm Safety Workshops
- Cholesterol
- Clinician's Guide to Irritative and Respiratory Problems in Relation to Environmental Exposures from the World Trade Center Disaster
- Cold Weather (English & Spanish)
- Construction Hazards: Dust
- Construction Hazards: Other Chemicals
- Construction Hazards: Solvents
- Depression Flyer
- Diabetes & Your Glucose Level
- Disposable Dust Masks
- Disposable Dust Masks - tip sheet
- Dust Masks (English & Spanish)
- EAP Program (Health Workers)
- Ergonomics Exposures, Problems, and Solutions
- Ergonomic Tips for Computer Users
- Eye Safety - tip sheet
- Farm Emergency Response Program
- Farmer's Occupational Health Clinic
- Farmstead Safety
- Fire Safety / Extinguishers (English & Spanish)
- Footwear Safety (English & Spanish)
- Gastroesophageal Reflux Disease
- Guides for Managing Lead Control Programs in Construction (workbook and factsheets)
- Guides for Managing Crystalline Silica Control Programs in Construction (workbook and factsheets)
- H1N1 (Swine Flu) Safety (English & Spanish)
- Health Issues Fact Sheet
- Healthy Exercise
- Healthy Workplace for Employers & Businesses
- Healthy Workplace for Workers, Retirees, & Residents
- Hearing (English & Spanish)
- Hearing Loss
- Hearing Loss in Farmers
- Hearing Protection (English & Spanish)
- Heat and Sun Safety (English, Spanish & Creole)
- Hypertension
- Indoor Air Quality: Facts about Mold and Dampness
- Insomnia
- Ladder Safety (English & Spanish)
- Lead in the Workplace
- Lead (Chinese)
- Low Back Pain and Lumbar Stabilization Exercises
- Lower Back Pain
- Lyme Disease (English & Spanish)
- Manganese Information for Pipefitters
- Manganese Information for Welders
- MDF Safety for Carpenters
- Mechanical Hazards (English & Spanish)
- Mercury (Chinese)
- MRSA Facts for Hospital Workers
- Needle Sticks (English & Spanish)
- Noise and Hearing Loss
- Office Ergonomics: A Survival Guide
- On Farm Safety Program
- Patellofemoral Pain Syndrome
- Peak Flow Monitoring
- Personal Hygiene (English & Spanish)
- Personal Protective Equipment (English & Spanish)
- Poison Ivy (English, Spanish & Creole)
- Processing Line (English & Spanish)
- Promoting Healthy Work through Occupational Ergonomics
- Protecting Your Back
- PTO Safety
- Respiratory Hazards
- Respiratory Hazards - tip sheet
- Safe Lifting & Carrying (English, Spanish & Creole)
- Safe Tractor Operating (English & Spanish)
- Safe Tractor Starting (English & Spanish)
- Safety Glasses (English & Spanish)
- Sharing the Road
- Sharp Tool Safety (English & Spanish)
- Silo Filler's Disease
- Silo Fillers - tip sheet
- Skid Steer Loaders
- SMV Marking & Lighting
- Stress Reduction & Your Breath
- Survival Guide for Choosing an Adjustable and Padded Office Chair
- Tractor Safety
- Tractor Safety Lifesavers (English & Spanish)
- Upright Silo Safety
- Using PPE
- West Nile Virus (English & Spanish)
- Whole Body and Segmental Vibration for WTC Laborers
- Work Safely with Spray-on Fireproofing
- Workers' Compensation: Benefits for WTC Rescue, Recovery, and Clean-up Workers
- Worker Health & Safety Rights
- You're Somebody at Work
Newsletter Articles
- Asbestosis
- Burned, High Risks and Low Benefits for Workers in the New York City Restaurant Industry
- Cancer Clusters
- Chemicals in the Workplace
- Ergonomics Information for All
- LIOEHC Helps Long Island's Fishermen Safely Navigate Dangerous Waters
- New Long Island Occupational & Environmental Health Center Program to Offer Free Health
- Exams For LI Migrant Agricultural Workers
- Occupational Asthma
- Occupational Disease
- Organic Solvent Toxicity
- Problems with the Indoor Air Environment at Workplaces
- Social Work
- Toxic Mold
- Trends in the Occupational Medicine Profession and Services: What the Long Island
- Occupational & Environmental Health Center (LIOEHC) Can Offer
- What is an Occupational Medicine Doctor?
Appendix B. Peer Reviewed Literature Published By The New York State Occupational Health Clinic Network, 2004-2011
- Auerbach K; Auerbach A. "Climate of New York State". Encyclopedia of Global Warming and Climate Change. S. George Philander. Thousand Oaks, CA: Sage Publications, 2008.
- Auerbach K. "Drug Testing Methodologies". Drug Courts. Lessenger, JE and Roper, GF. New York: Springer-Verlag, 2007. 215-233.
- Auerbach K. "Cell Phones and Cancer". Encyclopedia of Cancer and Society. Graham Colditz. Thousand Oaks, CA: Sage Publications, 2007.
- Barron BA, Beckett WS, Utell MJ. Clinical activities in an academic hospital-based occupational medicine program. J Occup Environ Med 2005; 47:587-593.
- Barron BA, Utell MJ. Occupational malaria. In: Occupational and Environmental Infectious Diseases, W.E. Wright, ed. OEM Press, 2nd edition. Beverly Farms, MA, 2009, pp. 457-490.
- Barron BA, Beckett WS, Utell MJ: Clinical activities in an academic hospital-based occupational medicine program. J Occup Environ Med 2005; 47:587-593.
- Beckett W, Kallay M, Sood A, Zuo Z, Milton D. Hypersensitivity pneumonitis associated with environmental mycobacteria. Environ Health Perspect 2005;47:587-593.
- Beckett W, Chalupa D, Pauly-Brown A, Speers D, Stewart J, Frampton M, Utell M, Huang L, Cox C, Zareba W, Oberdorster G. Comparing inhaled ultrafine versus fine zinc oxide particles in healthy adults: a human inhalation study. Am J Respir Crit Care Med 2005; 15:1129-1135.
- Beckett WS, Chalupa DF, Pauly-Brown A, Speers DM, Stewart JC, Frampton MW, Utell MJ, Huang LS, Cox C, Zareba W, Oberdörster G. Comparison of inhaled ultrafine vs. fine zinc oxide particles in healthy adults: a human inhalation study. Am J Respir Crit Care Med, 2005; 171:1129-1135.
- Berger Z, Rom WN, Reibman J, Kim M, Zhang S, Luo L, et al. Prevalence of workplace exacerbation of asthma symptoms in an urban working population of asthmatics. J Occ Env Med 2006; 48(8):833-839.
- Bills CB, Dodson N, Stellman JM, Southwick S, Sharma V, Herbert R, Moline JM, Katz CL. Stories behind the symptoms: a qualitative analysis of the narratives of 9/11 rescue and recovery workers. Psychiatr Q, 2009; 80:173-189.
- Bills CB, Levy NA, Sharma V, Charney DS, Herbert R, Moline JM, Katz CL. Mental health of workers and volunteers responding to events of 9/11: review of the literature. Mt Sinai J Med, 2008; 75:115-127.
- Brower MA, Earle-Richardson G, May JJ, Jenkins P. Occupational injury and treatment of migrant and seasonal farmworkers. J Agromed, 2009; 14(2):172-178.
- Caddell M, Doney B, Bang K, Petsonk E. Respiratory protection in US industry – an evaluation of program quality indicators and occupational heatlh outcomes. Journal of the International Society for Respiratory Protection, 2007; 24:63-73.
- Carrabba J, Scofield SM, May JJ. On-farm safety program. J Agromed, 2008; 13(3):139-148.
- Chalupa D, Morrow PE, Oberdorster G, Utell MJ, Frampton MW. Ultrafine particle deposition in subjects with asthma. Environ Hlth Perspect, 2004; 112:879-882.
- Cocchiarella L. Disability assessment and determination in the United States, Part I: In: UpToDate, Sokol HN MD (Ed) UpToDate, Waltham Ma. 2010, pending
- Cocchiarella L. Disability assessment and determination in the United States, Part II: In: UpToDate, Sokol HN, MD (Ed). UpToDate, Waltham Ma. 2010, pending
- Collins S, Warren N, Landsbergis PA, LaMontagne AD. Stopping stress at its origins addressing working conditions (letter). Hypertension, 2007; 49:e33.
- Dave SK, Beckett WS. Occupational asbestos exposure and predictable asbestos related diseases in India. Am J Indust Med, 2005;48:137-143.
- De la Hoz RE, Aurora RN, Landsbergis P, Bienenfeld LA, Afilaka AA, Herbert R. Snoring and obstructive sleep apnea among former World Trade Center rescue workers and volunteers. J Occup Environ Med, 2010;52:29-32.
- De la Hoz RE, Shohet MR, Wisnivesky JP, Bienenfeld LA, Afilaka AA, Herbert R. Atopy and upper and lower airway disease among former World Trade Center workers and volunteers. J Occup Environ Med, 2009; 51:992-995.
- De la Hoz RE, Christie J, Teamer JA, Bienenfeld LA, Afilaka AA, Crane M, Levin SM, Herbert R. Reflux symptoms and disorders and pulmonary disease in former World Trade Center rescue and recovery workers and volunteers. J Occup Environ Med, 2008; 50:1351-1354.
- De la Hoz RE, Hill S, Chasan R, Bienenfeld LA, Afilaka AA, Wilk-Rivard E, Herbert R. Health care and social issues of immigrant rescue and recovery workers at the World Trade Center site. J Occup Environ Med, 2008; 50:1329-1324.
- De la Hoz RE, Shohet MR, Bienenfeld LA, Afilaka AA, Levin SM, Herbert R. Vocal cord dysfunction in former World Trade Center (WTC) rescue and recovery workers and volunteers. Am J Ind Med, 2008; 51:161-165.
- De la Hoz RE, Shohet MR, Chasan R, Bienenfeld LA, Afilaka AA, Levin SM, Herbert R. Occupational toxicant inhalation injury: the World Trade Center (WTC) experience. Int Arch Occup Environ Health, 2008; 81:479-485.
- Earle-Richardson G, Jenkins P, Scott EE, May JJ. Improving Agricultural Injury Surveillance: a comparison of incidence rates among three data sources. American Journal Industrial Medicine Accepted Dec 7, 2010.
- Earle-Richardson G, Sorensen J, Brower M, Hawkes L, May JJ. Community Collaborations for Farmworker Health in New York and Maine: Process Analysis of Two Successful Interventions. AJPH 2009; 99(S3):S584-S587.
- Earle-Richardson G, Jenkins P, Strogatz D, Bell E, Freivalds A, Sorensen J, May JJ. Electromyographic Assessment of Apple Bucket Intervention Designed to Reduce Back Strain. Ergonomics 2008; 51(6):902-919.
- Earle-Richardson G, Brower M.A, Jones A.M, May J.J., & Jenkins P. Estimating the Occupational Morbidity for Migrant and Seasonal Farmworkers in New York State: A Comparison of Two Methods. Annals of Epidemiology, 2008; 18(1):1-7.
- Earle-Richardson G, Jenkins P, Strogatz D, Bell E, Sorensen J, May J.Orchard Evaluation of Ergonomically Modified Apple Bucket. J Agromed 2007; 11(3/4):95-105.
- Earle-Richardson G, Jenkins P, Freivalds A, Burdick P, Park S, Lee C, Mason C, May JJ. Laboratory Evaluation of Belt Usage with Apple Buckets. Am J Ind Med 2006; 49(1):23-29.
- Earle-Richardson G, Jenkins P, Strogatz D, Bell EM, May JJ. Development and initial assessment of objective fatigue measures for apple harvest work. Applied Ergonomics 2006; 37(6):719-727.
- Earle-Richardson G, Jenkins P, Fulmer S, Mason C, Burdick P, May J.An Ergonomic Intervention to Reduce Back Strain Among Apple Harvest Workers in New York State. Applied Ergonomics 2005; 36(3):327-334.
- Earle-Richardson G, Jenkins P, Stack S, Sorensen J, Larson A, May JJ. Estimating Farmworker Population Size in New York State Using a Minimum Labor Demand Method. J Ag Safety and Health 2005; 11(3):335-345.
- Elder ACP, Gelein R, Finkelstein J, Frampton M, Utell M, Carter J, Driscoll K, Kittelson D, Watts W, Hopke P, Vincent R, Premkumari K, Oberdorster G. Effects of Inhaled Fine/Ultrafine Particles Combined with Other Air Pollutants. In 9th International Inhalation Symposium, Heinrich, U., Ed.; 2004; pp 53-68.
- Elder A, Gelein R, Finkelstein J, Phipps R, Frampton M, Utell M, Topham D, Kittelson D, Watts W, Hopke P, Jeong C-H, Kim E, Liu W, Zhao W, Zhou L, Vincent R, Kumarathasan P, Oberdörster G. On-Road Exposure to Highway Aerosols. 2. Exposures of Aged, Compromised Rats. Inhal Toxicol, 2004; 16(Suppl.1): 41-53.
- Elder A, Couderec J-P, Gelein R, Eberly S, Cox C, Xia X, Zareba W, Hopke P, Watts W, Kittelson D, Frampton M, Utell M, Oberdorster G. Effects of on-road highway aerosol exposures on autonomic responses in aged, spontaneously hypertensive rats. Inhalation Toxicol, 2007; 19:1-12.
- Enright P, Skloot G, Herbert R. Standardization of spirometry in assessment of responders following manmade disasters: The World Trade Center Worker and Volunteer Medical Screening Program. Mt Sinai J Med, 2008; 75:109-114.
- Fang S, Herbert R, Dropkin J, Triola D, Landsbergis PA. Workers' Compensation experience of computer users with musculoskeletal disorders. Am J Ind Med, 2007; 50:512-518.
- Fanning EW, Froines JR, Utell MJ, Lippmann M, Oberdorster G, Frampton M, Godleski J, Larson TV. Particulate matter (PM) research centers (1999-2005) and the role of interdisciplinary center-based research. Environ Health Persp, 2009; 117(7):167-174.
- Fischer FM, Borges FN, Rotenberg L, Latorre Mdo R, Soares NS, Rosa PL, Texeira LR, Nagai R, Steluti J, Landsbergis P. Work ability of health care shift workers: what matters? Chronobiol Int, 2006; 23: 1165-1179
- Frampton MW, Samet JM, Utell MJ.Cardiopulmonary consequences of particle inhalation. In: Particle-Lung Interactions. P. Gehr and J. Heyder, eds., Lung Biology and Disease, Marcel Dekker, New York, in press.
- Frampton MW, Samet JM, Utell MJ. Exposures in outdoor air. In: Textbook of Clinical Occupational and Environmental Medicine. L. Rosenstock and M. Cullen, eds., 2nd edition, W.B. Saunders, Philadelphia, PA, 2008, pp. 1143-1150.
- Frampton MW, Utell MJ. Sulfur dioxide. In: Environmental and Occupational Medicine, 3rd edition. W.N. Rom and S.B. Markowitz, eds., Lippincott Williams&Wilkins, Philadelphia, PA, pp. 1480-1486, 2007.
- Frampton MW, Utell MJ (eds). Exposure to Airborne Particles: Health Effects and Mechanisms. Clinics in Occupational and Environmental Medicine. 2006; 5(4): Saunders, Philadelphia.
- Frampton MW, Utell MJ, Zareba W,Oberdörster G, Cox C, Huan L-S, Morrow PE, Lee FE-H, Chalupa D, Frasier DM, Speers DM, Stewart J. Health effects of exposure to ultrafine carbon particles in healthy subjects and subjects with asthma. Health Effects Institute Research Report No. 126, Boston, MA, pp. 1-47, 2005.
- Frampton MW, Stewart J, Oberdörster G, Morrow GE, Chalupa D, Frasier DM, Speers DM, Cox C, Huang L-S, Utell MJ. Inhalation of carbon ultrafine particles alters blood leukocyte expression profile in humans. Environ Health Persp, 2006; 114:51-58.
- Frampton MW, Samet JM, Utell MJ. Exposures in outdoor air. In: Textbook of Clinical Occupational and Environmental Medicine. L. Rosenstock and M. Cullen, eds., W.B. Saunders, Philadelphia, PA, 2005, pp. 1143-1150.
- Freivalds A, Park S, Lee C, Earle-Richardson G, Mason C, May JJ. Effect of belt/bucket interface in apple harvesting. International Journal of Industrial Ergonomics 2006; 36(11):1005-1010.
- Friedman S, Cone J, Eros-Sarnyai M, Prezant D, Szeinuk J, Clark N, Milek D, Levin S, Guillio R. Clinical guidelines for adults exposed to the World Trade Center Disaster. City Health Info, 2006; 25: 47-58.
- Friedman-Jiménez , G, Claudio L. Disparities in Environmental and Occupational Health, Environmental and Occupational Medicine, 4th ed., eds: William N. Rom, MD, MPH and Steven Markowitz, MD, Philadephia: Lipponcott Williams & Wilkins, 2007. Chap 113.
- Gadomski A, Ackerman S, Burdick P, Jenkins P. Efficacy of the North American guidelines for children's agricultural injuries. Am J Public Health 2006; 96(4):722-727.
- Gadomski A, de Long R, Burdick P, Jenkins P. Do Economic Stresses Influence Child Work Hours on Family Farms? J Agromed 2005; 10(2):39-48.
- Gaetano DE, Hodge B, Clark A, Ackerman S, Burdic P, Cook MW. Preventing Skin Cancer Among a Farming Population: Implementing Evidence-Based Interventions. AAOHN Journal 2009; 57(1):24-33.
- Gaetano D, Ackerman S, Clark A, Hodge B, Hohensee T, May J, Whiteman W. Health surveillance for rural firefighters and emergency medical services personnel. AAOHN 2007; 55(2):57-63.
- Gehring U, Triche E, van Strien R, Belanger K, Holford T, Gold D, Jankun T, Ren P, McSharry J, Beckett W, Platts-Mills T, Chapman M, Bracken M, Leaderer B. Prediction of residential pet and cockroach allergen levels using questionnaire information. Environ Health Perspect 2004;112:834-839.
- Harrison D . International Byssinosis, Environmental and Occupational Medicine, 4th ed., eds: William N. Rom, MD, MPH and Steven Markowitz, MD, Philadephia: Lipponcott Williams & Wilkins, 2007. Chap 29. p.490.
- Hawkes L, May J, Paap K, Santiago B, Ginley B.Identifying the Occupational Health Needs of Migrant Workers. J Comm Practice. 2007; 15(3):57-76.
- Herbert R, Moline J, Skloot G, Metzger K, Baron S, Luft B, Markowitz SB, Udasin I, Harrison D, Stein D, Todd A, Enright P, Stellman JM, Landrigan PJ, Levin SM. The World Trade Center Disaster and the health of workers: five-year assessment of a unique medical screening program. Environ Health Perspect, 2006; 114:1853-1858.
- Herbert R. A mental health program for ground zero rescue and recovery workers: cases and observations. Psychiatr Serv, 2006; 57:1335-1338.
- Herbert R, Szeinuk J. Integrating clinical care with prevention of occupational illness and injury. In: Rosenstock L, Cullen MR, Brodkin CA, Redlich CA. Textbook of Clinical Occupational and Environmental Medicine. Philadelphia: Elsevier Saunders, 2nd edition, 2005; pp: 1263-1274.
- Jenkins P, Stack S, May JJ, Earle-Richardson G. Growth of the Spanish-Speaking Workforce in the Northeast Dairy Industry. J Agromed, 2009; 14(1):58-65.
- Jenkins P, Earle-Richardson G, Burdick P, May J. Handling nonresponse in surveys: analytic corrections compared with converting nonresponders. Am J Epidemiol; 2008; 167(3):369-374.
- Jenkins PL, Stack SG, Earle-Ricahardson G, Scofield SM, May JJ. Using Screening events to reduce hazardous exposures to farmers. J Ag Saf Health 2007; 13(1):57-64.
- Jenkins P, Earle-Richardson G, Burdick P, May J. Handling Nonresponse in Surveys: Analytic Corrections Compared with Converting Nonresponders. Am J Epidemiol 2007; 167(3): 369-374.
- Jenkins P, Earle-Richardson G, Bell E, May JJ, Green A. Chronic Disease Risk in Central New York Dairy Farmers: Results from a Large Health Survey 1989-1999. Am J Ind Med 2005; 47(1):20-26.
- Jeong CH, Hopke PK, Chalupa D, Utell M. Characteristics of nucleation and growth events of ultrafine particles measured in Rochester, NY. Environ Sci Technol, 2004; 38:1933-1940.
- Jeong C-H, Evans GJ, Hopke PK, Chalupa D, Utell MJ. Influence of atmospheric dispersion and new particle formation Events on ambient particle number in Rochester, USA and Toronto, Canada. J. Air Waste Management Assoc., 2006; 56:431-443.
- Johanning E, Landsbergis PA, Fisher S, Christ E, Gores B, Luhrman R. Whole-body vibration and ergonomic study of U.S. railroad locomotives. J Sound Vibr, 2006; 298:594-600.
- Katz CL, Levin S, Herbert R, Munro S, Pandya A, Smith R. Psychiatric symptoms in Ground Zero ironworkers in the aftermath of 9/11: prevalence and predictors. Psychiatr Bull, 2009; 33:49-52.
- Katz CL, Smith R, Silverton M, Holmes A, Bravo C, Jones K, Kiliman M, Lopez N, Malkoff L, Marrone K, Neuman A, Stephens T, Tavarez W, Yarowsky A, Levin S, Herbert R. A mental health program for ground zero rescue and recovery workers: cases and observations. Psychiatr Serv, 2006; 57:1335-1338.
- Kirkhorn SR, Earle-Richardson G, Banks RJ. Ergonomic risks and musculoskeletal disorders in production agriculture: recommendations for effective research to practice. J Agromed 2010; 15(3):281-299.
- Kirkhorn SR, Earle-Richardson G. Repetitive Motion Injuries. In: Lessenger JE, editor. Agricultural Medicine: A Practical Guide. New York: Springer, 2006: 324-338.
- LaMontagne AD, Keegel T, Louie AM, Ostry A, Landsbergis PA. A systematic review of the job stress intervention evaluation literature, 1990-2005. Int J Occup Environ Health, 2007; 13:268-280.
- Landsbergis PA, Schnall P, Schwartz J, Baker D, Belkic K, Pickering T. Working conditions and masked (hidden) hypertension: Insights into the global epidemic of hypertension. Scand J Work Environ Health Suppl, 2008; 6:41–51.
- Lax MB. Workers' Compensation Reform Needs an agenda…and a Strategy. New Solutions In Press
- Lax MB,Klein R. More Than Meets the Eye: Social, Economic, and Emotional Impacts of Work Related Injury and Illness. New Solutions, 2008; 18(3):343-360.
- Lax MB Guidotti Fails to Convince on Two Issues. New Solutions, 2008; 18(3):325-328.
- Lax MB, Inspiration for a Movement: Re-Reading Death on the Job. New Solutions, 2006; 16:299-332.
- Looney RJ, Beckett WS, Utell MJ. Occupational airways disease. In: Baum's Textbook of Pulmonary Diseases, 7th edition. J.D. Crapo, J. Glassroth, J. Karlinsky,T.E. King, Jr. eds., Lippincott Williams & Wilkins, Philadelphia, 2004, pp. 975-988.
- Mangahas CR, dela Cruz GV, Friedman-Jiménez G, Jamal S. Endothelin-1 induces CXCL1 and CXCL8 secretion in human melanoma cells. J Investigative Dermatology 2005; 125(2):307-312.
- Maxim LD, Galvin JB, Nebo R, Seagraves AM, Kappa OA, Utell MJ. Occupational Exposure to Carbon/coke Fibers in Plants That Produce Green or Calcined Petroleum Coke and Potential Health Effects: 1. Fiber Characteristics. Inhalation Toxicol, 2006, 18:1-16.
- Maxim LD, Galvin JB, Niebo R, Segrave AM, Kampa OA, Utell MJ. Occupational Exposure to Carbon/coke Fibers in Plants That Produce Green or Calcined Petroleum Coke and Potential Health Effects: 2. Fiber Concentrations. Inhalation Toxicol, 2006, 18:17-32.
- May JJ. Occupational Health Problems in Migrant Farmworkers, in Latino Farmworkers in the Eastern United States. Health, Safety and Justice. Arcury T and Quandt S (eds) Springer, 2009.
- May JJ., Hawkes L, Jones A, Burdick P, Ginley B, Santiago B, Rowland M. Evaluation of a Community-Based Effort to Reduce Blueberry Harvesting Injury. Am J Ind Med 2008; 51(4):307-315.
- May JJ, Sorensen J, Burdick P, Earle-Richardson G, Jenkins P. Rollover Protection on New York Tractors and Farmers' Readiness for Change. J Ag Safety and Health 2006; 12(3):199-213.
- May JJ, Scofield SM. "Safety for agricultural educators". J Agromed 2005; 10(4):65-70.
- Mendelson DS, Roggeveen M, Levin SM, Herbert R, de la Hoz RE. Air trapping detected on end-expiratory high-resolution computed tomography in symptomatic World Trade Center rescue and recovery workers. J Occup Environ Med, 2007; 49:840-845.
- Mitchell C, Gochfeld M, Shubert J, Kipen H, Moline J, Langlieb A, Everly G, Udasin I, Wartenburg D, Paulson G. Surveillance of workers responding under the National Response Plan. J Occup Environ Med, 2007; 49:922-927.
- Moline J, Herbert R, Crowley L, Troy K, Hodgman E, Shukla G, Udasin I, Luft B, WallensteinS, Landrigan P, Savitz D. Multiple myeloma in World Trade Center responders: A case series. J Occup Environ Med, 2009; 51:896-902.
- Moline JM, Herbert R, Levin S, Stein D, Luft B, Udasin IG, Landrigan PJ. The WTC Medical Monitoring and Treatment Program: comprehensive health care response in the aftermath of disaster. Mt Sinai J Med, 2008; 75:67-75.
- Moline JM, Herbert R, Levin S, Stein D, Luft BJ, Udasin IG, Landrigan PJ.WTC Medical Monitoring and Treatment program: Comprehensive health care response in aftermath of disaster. Mt Sinai J Med, 2008; 75:67-75.
- Moline JM, Herbert R, Nguyen N. Health consequences of the September 11th World Trade Center attacks: a review. Cancer Invest, 2006; 24:294-301.
- Murphy DJ, Myers J, McKenzie EA, Cavaletto R, May J, Sorensen J. Tractors and Rollover Protection in the United States. J Agromedicine 2010; 15(3):249-263.
- Ogulei D, Hopke PK, Chalupa DC, Utell MJ. Modeling sources contributions to ultrafine particle number concentrations measured in Rochester, NY. Aerosol Science and Technol, 2007, 41:179-201.
- Perry MJ, May JJ. Noise and Chemical Induced Hearing Loss: Special Considerations for Farm Youth. J Agromed 2005; 10(2):49-55.
- Phipps R, Beckett WS, Kaufman J, Martey C, Sime PJ, Thatcher TH. Anti-inflammatory therapies for lung injury. In Lung Injury. Mechanisms, Pathophysiology and Therapy. Notter RF, Finkelstein JA, Holm BA, eds. Lung Biology in Health and Disease series; 2005. Boca Raton, Taylor and Francis Group.
- Pietropaoli AP, Frampton MW, Hyde RW, Morrow PE, Oberdörster G, Cox C, Speers DM, Frasier LM, Chalupa DC, Huang LS, Utell MJ. Pulmonary function, diffusing capacity and inflammation in healthy and asthmatic subjects exposed to ultrafine particles. Inhalation Toxicol, 2004; 16(Suppl. 1):59-72.
- Pietropaoli AP; Perillo IB, Perkins PT, Frasier LM, Speers DM, Frampton MW, Utell MJ, and Hyde RW: Smokers have reduced nitric oxide production by conducting airways but normal levels in the alveoli. Inhalation Toxicol, 2007; 19(6-7):533-4.
- Pietropaoli AP, Frampton MW, Oberdorster G, Cox C, Huang L, Marder V, Utell MJ. Blood markers of coagulation and inflammation in healthy subjects exposed to carbon ultrafine particles. In: Effects of Air Contaminants on the Respiratory Tract -Interpretations from Molecular to Meta Analysis. INIS Monographs, Fraunhofer IRB Verlag, Stuttgart, Germany, 2004, pp.181-194.
- Piligian G, Szeinuk J, Levin S, Moline J, Milek D, Afilaka A, Wilk-Rivard E. Non-specific triggers also provoke occupational asthma. Am J Respir Crit Care Med, 2006; 173:357.
- Prezant DJ, Levin S, Kelly KJ, Aldrich TK. Upper and lower respiratory diseases after occupational and environmental disasters. Mt Sinai J Med, 2008; 75:89-100.
- Reddy MB, Dobrev ID, McNett DA, Tobin JM, Utell MJ, Morrow PE, Domoradzki JY, Plotzke KP, Andersen ME. Inhalation dosimetry modeling with decamethylcyclopentasiloxane in rats and humans. Toxicol. Sci, 2008; 105: 275 – 285.
- Reddy MB, Looney RJ, Utell MJ, Plotzke KP, Andersen ME. Modeling of Human Dermal Absorption of Octamethylcyclotetrasiloxane (D4) and Decamethylcyclopentasiloxane (D5). Toxicol. Sci, 2007; 99:422-431.
- Robertson SM, Murphy DJ, Davis LA. Social and Emotional Impacts of Farmwork Injuries: An Exploratory Study. The Journal of Rural Health 2006; 22(1):26-35.
- Rondinelli R. Senior advisor: Cocchiarella L, G. AMA Guides to the Evaluation of Permanent Impairment, American Medical Association, 6th Edition, December, 2007
- Rotenberg L, Portela LF, Banks B, Griep RH, Fischer FM, Landsbergis P. A gender approach to work ability and its relationship to professional and domestic work hours among nursing personnel. Appl Ergon, 2008; 39:646-652.
- Samet JM, Utell MJ. Indoor and Outdoor Air Pollution. In: Fishman's Pulmonary Diseases and Disorders, 4th edition. A.P. Fishman, J.A. Elias, J. A. Fishman, M.A. Grippi, R.M. Senior, and A.I. Pack, eds., McGraw-Hill, 2008, pp. 1009-1036.
- Samet JM, Geyh A, Utell MJ. The legacy of the world trade center dust. N Engl J Med, 2007; 356(22):2233-2236.
- Santa Rosa PLF, Fischer FM, da Silva Borges FN, da Silva Soares N, Rothenberg L, Landsbergis P. Perceived sleep duration and fatigue among nursing personnel (Portugese). Revista Enfermagem UERJ, 2007; 15:100-106.
- Savitz D, Oxman R, Metzger K, Wallenstein S, Stein D, Moline J, Herbert R. Epidemiologic research on manmade disasters: strategies and implications of cohort definition for the World Trade Center Worker and Volunteer Surveillance Programs. Mt Sinai J Med, 2008; 75:77-87.
- Shah AP, Pietropaoli AP, Frasier L, Speers DM, Chalupa D, Delahanty J, Utell MJ, Frampton MW. Effect of inhaled ultrafine particles on reactive hyperemia in healthy human subjects. Environ Health Persp, 2008; 116:375-380.
- Skloot GS, Schechter CB, Herbert R, Moline JM, Levin SM, Crowley LE, Luft BJ, Udasin IG, Enright PL.Longitudinal assessment of spirometry in the World Trade Center medical monitoring program. Chest, 2009; 135:492-498.
- Smith DA, Ness EM, Herbert R, Schechter CB, Phillips RA, Diamond JA, Landrigan, PJ. Abdominal diameter index: a more powerful anthropometric measure for prevalent coronary heart disease risk in adult males. Diabetes Obes Metab, 2005; 7:370-80.
- Sood A, Beckett W, Cullen M. Variable response to long-term corticosteroid therapy in chronic beryllium disease. Chest, 2004;126:2000-2007.
- Sorensen JA, McKenzie, Jr., EA, Purschwitz M, Fiske, T, Jenkins, PL, O'Hara P, May JJ. Complications with farmer installation of rollover protective structures: Results from a random inspection of New York ROPS rebate self-installers. J Agromedicine. 2011; 16(1):19-29.
- Sorensen JA, Conway G, DeSpain M, Wyckoff S, Bayes B, JJ May. Dealing with tractors that can't be retrofitted: Exploring the viability of a tractor trade-in program. Journal of Agromedicine 2011;16(1):30-39.
- Sorensen JA, Jenkins PL, Bayes B, Clark S, May JJ. Cost-effectiveness of a ROPS social marketing campaign. Journal of Agricultural Safety and Health. 2010; 16(1):31-40.
- Sorensen JA, McKenzieEA , Purschwitz M, Fiske, T, Jenkins PL, O'Hara P, May JJ. Results from inspections of farmer-installed rollover protective structures. J Agromed 2010 in press
- Sorensen JA, Jenkins PL, Emmelin M, Stenlund H, Weinehall L, Earle-Richardson G, May J. The Social Marketing of Safety Behaviors: A Quasi-Randomized Controlled Trial of Tractor Retrofitting Incentives. Am J Public Health 2010 in press
- Sorensen JA. Social Marketing for Injury Prevention: Changing Risk Perceptions and Safety-related Behaviors Among New York farmers. PhD diss. Umea Universitet Print and Media, 2009.
- Sorensen J, Emmelin M, Papp K, Purschwitz, M, & May JJ. Encouraging Farmers to Retrofit Tractors: A Qualitative Analysis of RIsk Perception Amongst A Group of High Risk Farmers in New York. J Ag Safety and Health 2008; 14(1):105-117.
- Sorensen JA, May JJ, Purschwitz, M Emmelin M. Encouraging farmers to retrofit tractors: qualitative analysis of risk perceptions among a group of high-risk farmers in New York. J Ag Safety Health 2008; 14(1):105-117.
- Sorensen JA., May JJ, Ostby-Malling R, Lehmen T, Stand J, StenlundH, Weinehall L, Emmelin M. Encouraging the Installation of Rollover Protective Structures in New York State: The Design of a Social Marketing Intervention. Scand J Pub Health, 2008; 36(8):859-869.
- Sorensen JA, May J, O;Hara P, Ostby R, Lehman T, Viebrocks S, Emmelin M. Evaluating Tractor Safety Messages: A Concept Development Project. Soc Mar Q 2008; 14(4):22-44.
- Sorensen J, May JJ, Jenkins P, Jones AM, Earle-Richardson G. Risk Perceptions, Barriers, and Motivators to Tractor ROPS Retrofitting in the New York State Farm Community. J Ag Safety and Health 2006; 12(3):215-226.
- Stack S, Jenkins P, Earle-Richardson G, Ackerman S, May JJ.Spanish-speaking Dairy Workers in New York, Pennsylvania and Vermont: Results from a Survey of Farm Owners. J Agromed 2006;11(2):37-44.
- Stellman J, Smith R, Katz CL, Sharma V, Charney D, Herbert R, Moline JM, Luft B, Markowitz S, Udasin I, Harrison D, Baron S, Landrigan PJ, Levin S, Southwick S. Enduring mental health morbidity and social function impairment in World Trade Center rescue, recovery, and cleanup workers: The psychological dimension of an environmental health disaster. Environ Health Perspect, 2008; 116:1248-1253.
- Stellman J, Smith R, Katz C, Sharma V, Charney D, Herbert R, et al. Mental Health Morbidity and Social Function Impairment in Rescue, Recovery and Cleanup Workers at the World Trade Center Disaster. Environmental Health Perspectives, 2008; 116(9):1248-1253.
- Stewart JC, Hyde RW, Boscia J, Chow MY, O'Mara RE, Perillo I, Pietropaoli A, Smith CJ, Torres A, Utell MJ, Frampton MW. Changes in markers of epithelial permeability and inflammation in chronic smokers switching to a nonburning tobacco device (Eclipse). Nicotine Tob Res, 2006; 8:773-783.
- Su Y, Sipin MF, Spencer MT, Qin X, Moffet RC, Shields LG, Prather KA, Venkatachari P, Jeong C-H, Kim E, Hopke PK, Gelein RM, Utell MJ, Oberdorster G, Bernsten J, Devlin RB, Chen LC. Real-time characterization of the composition of individual particles emitted from ultrafine particle concentrators. Aerosol Science and Technol, 2006; 40:437-455.
- Szeinuk J, Padilla M, de la Hoz RE. Potential for diffuse parenchymal lung disease after exposures at World Trade Center Disaster site. Mt Sinai J Med, 2008; 75:101-107.
- Szeinuk J, Wilk-Rivard EJ. Silicatosis in a Carpet Installer. A case presentation. Environ Health Perspect, 2007; 115:932-935.
- Thurston GD, Bekkedal MYB, Roberts E, Ito K, Pope CA, Glenn B, özkaynak, Utell MJ. Use of health information in air pollution health research: Past successes and emerging needs. Journal of Exposure Science and Environmental Epidemiology, 2009; 19:45-58.
- Triche E, Belanger K, Bracken M, Beckett W, Holford T, Gent J, McSharry J-E, Leaderer BP. Indoor heating sources and respiratory symptoms in nonsmoking women. Epidemiology 2005;16:377-384.
- Utell MJ, Samet JM. Clinical perspectives on cardiorespiratory toxicology. In: Environmental Toxicants: Human Exposures and Their Health Effects. 2nd Edition. M. Lippmann, ed., Wiley, Interscience, New York, 2008, in press.
- Utell, M.J., S. Mehta and M.W. Frampton: Determinants of susceptibility. In: Air Quality Guidelines: Global Update 2005. World Health Organization. Copenhagen, Denmark. pp. 111-133, 2006.
- Utell MJ, Beckett WS. Implications for occupational exposure to particulate matter. Clin Occup Environ Med, 2006; 5(4):883-93.
- Marier M, VanRaalte J. Exploring sampling of asbestos in residences near Thetford Mines: the public health threat in Quebec. Int Journal of Occ and Env Health 2007; 13:386-397.
- Van Vegchel N, deJonge J, Landsbergis PA. Occupational stress in (inter)action: the interplay between job demands and job resources. J Organiz Behav, 2005; 26:535-560.
- Vora R, Frampton MW, et al: Cardiovascular changes after exposure to ultrafine carbon particles (manuscript in preparation).
- Wagner NL, Beckett WS, Steinberg R. Using spirometry results in occupational medicine and research. Common errors and good practice in statistical analysis and reporting. Indian Journal of Occupational Medicine 2006; 10:5-10.
- Zareba W, Couderc JP, Oberdörster G, Chalupa D, Speers DM, Cox C, Huang LS, Peters A, Utell MJ, Frampton MW. ECG parameters and exposure to carbon ultrafine particles in young healthy subjects. Inhalation Toxicol, 2009; 30(4):603-610.
- Zuckerman N, Szeinuk J. ACOEM evidence-based statement: medical surveillance of workers exposed to crystalline silica – some comments and suggestions (let). J Occup Environ Med, 2006; 48: 659-660.
Appendix C. Comments Received During Public Comment Period
A draft version of this report was made available on the New York State Department of Health website from August 7, 2012 through September 30, 2012 for public comment. The pages that follow are the responses received.