MRT Plan Current STCs - April 1, 2022
- Plan is also available in Portable Document Format (PDF)
CENTERS FOR MEDICARE & MEDICAID SERVICES
WAIVER AUTHORITIES
NUMBER: 11-W-00114/2
TITLE: Medicaid Redesign Team AWARDEE: New York State Department of Health
AWARDEE: New York State Department of Health
All requirements of the Medicaid program expressed in law, regulation, and policy statement, not expressly waived in this list, shall apply to the demonstration.
The following waivers shall enable New York to implement the approved Special Terms and Conditions (STC) for the New York Medicaid Redesign Team (MRT) section 1115 demonstration (formerly the New York Partnership Plan) beginning April 1, 2022, and ending March 31, 2027.
1. Statewideness Section 1902(a)(1)
To permit New York to geographically phase in the Managed Long Term Care (MLTC) program and the Health and Recovery Plans (HARP) and to phase in Behavioral Health (BH) Home and Community Based Services (HCBS) into HIV Special Needs Plans (HIV SNP).
2. Comparability Section 1902(a)(10), section 1902(a)(17)
- To enable New York to apply a more liberal income standard for individuals who are deinstitutionalized and receive HCBS through the managed long-term care program than for other individuals receiving community-based long-term care.
- To the extent necessary to permit New York to waive cost sharing for non-drug benefit cost sharing imposed under the Medicaid state plan for beneficiaries enrolled in the Mainstream Medicaid Managed Care Plan (MMMC) - including HARP and HIV SNPs - and who are not otherwise exempt from cost sharing in 447.56(a)(1).
- Family of One Non-1915 Children, or "Fo1 Children" - To allow the state to target eligibility to, and impose a participation capacity limit on, medically needy children under age 21 who are otherwise described in 42 Code of Federal Regulations (CFR) § 435.308 of the regulations who: 1) receive Health Home Comprehensive Care Management under the state plan in replacement of the case management services such individuals formerly received through participation in New York's NY #.4125 1915(c) waiver and who no longer participate in such waiver due to the elimination of the case management services, but who continue to meet the targeting criteria, risk factors and clinical eligibility standard for such waiver; and 2) receive HCBS 1915(c) services who meet the risk factors, targeting criteria, and clinical eligibility standard for the above-identified 1915(c) waiver. Individuals who meet either targeting classification will have excluded from their financial eligibility determination the income and resources of third parties whose income and resources could otherwise be deemed available under 42 CFR §435.602(a)(2)(i). Such individuals will also have their income and resources compared to the medically needy income level (MNIL) and resource standard for a single individual, as described in New York's state Medicaid plan.
3. Amount, Duration & Scope Section 1902(a)(10)(B)
To enable New York to provide BH HCBS services and the Adult Rehabilitation Services named Community Oriented Recovery and Empowerment (CORE) Services, whether furnished as a state plan benefit or as a demonstration benefit to targeted populations that may not be consistent with the targeting authorized under the approved state plan, in amount, duration and scope that exceeds those available to eligible individuals not in those targeted populations.
4. Freedom of Choice Section 1902(a)(23)(A)
To the extent necessary to enable New York to require beneficiaries to enroll in managed care plans, including the MMMC, and MLTC (excluding individuals designated as "Long-Term Nursing Home Stays") and HARPs programs in order to obtain benefits offered by those plans. Beneficiaries shall retain freedom of choice of family planning providers.
5. Reasonable Promptness Section 1902(a)(8)
To enable the state to limit the number of medically needy Fo1 Children not otherwise enrolled in the Children's 1915(c) waiver.
Title XIX Requirements Not Applicable to Self-Direction Pilot Program
(see Expenditure Authority 8, "Self-Direction Pilot")
6. Direct Payment to Providers Section 1902(a)(32)
To the extent necessary to permit the state to make payments to beneficiaries enrolled in the Self Direction Pilot Program to the extent that such funds are used to obtain self-directed HCBS long term care (LTC) services and supports.
EXPENDITURE AUTHORITIES
NUMBER: 11-W-00114/2
TITLE: Medicaid Redesign Team
AWARDEE: New York State Department of Health
Under the authority of section 1115(a)(2) of the Social Security Act ("the Act"), expenditures made by New York for the items identified below, which are not otherwise included as expenditures under section 1903 of the Act shall, until the ending date specified for each authority as listed below, be regarded as expenditures under the state's title XIX plan. These expenditure authorities shall be effective from April 1, 2022, through March 31, 2027, except as otherwise noted.
The following expenditure authorities shall enable New York to implement the approved Special Terms and Conditions (STC) for the New York Medicaid Redesign Team Medicaid Section 1115 demonstration.
- Demonstration-Eligible Populations. Expenditures for healthcare related costs for the following populations that are not otherwise eligible under the Medicaid state plan.
- Demonstration Population 2 (Temporary Assistance for Needy Families (TANF) Adult). TANF Recipients. Expenditures for health care related costs for low-income adults enrolled in TANF. These individuals are exempt from receiving a Modified Adjusted Gross Income (MAGI) determination in accordance with 1902(e)(14)(D)(i)(I) of the Act.
- Demonstration Population 9 (HCBS Expansion). Individuals who are not otherwise eligible, are receiving HCBS, and who are determined to be medically needy based on New York's medically needy income level, after application of community spouse and spousal impoverishment eligibility and post-eligibility rules consistent with section 1924 of the Act.
- Demonstration Population 10 (Institution to Community). Expenditures for health care related costs for individuals moved from institutional nursing facility settings to community settings for long term services and supports who would not otherwise be eligible based on income, but whose income does not exceed the income standard described in STC 4.4(c), and who receive services through the managed long-term care program under the demonstration.
- Included in Demonstration Population 12 [Family of One (Fo1) Children]. Medically needy children Fo1 Demonstration children under age 21 with a waiver of 1902(a)(10)(C)(i)(III) who meet the targeting criteria, risk factors, and clinical eligibility standard for #NY.4125 waiver including intermediate care facilities (ICF), nursing facilities (NF), or Hospital Level of Care (LOC) who are not otherwise enrolled in the Children's 1915(c).
- Twelve-Month Continuous Eligibility Period. Expenditures for health care related costs for individuals who have been determined eligible under groups specified in Table 6 of STC 4.4(e) for continued benefits during any periods within a twelve-month eligibility period when these individuals would be found ineligible if subject to redetermination. This authority includes providing continuous coverage for the Adult Group determined financially eligible using MAGI based eligibility methods. For expenditures related to the Adult Group, specifically, the state shall make a downward adjustment of 2.6 percent in claimed expenditures for federal matching at the enhanced federal matching rate and will instead claim those expenditures at the regular matching rate.
- Facilitated Enrollment Services. Expenditures for enrollment assistance services provided by managed care organizations (MCO), the costs for which are included in the claimed MCO capitation rates.
- Demonstration Services for Behavioral Health Provided under Mainstream Medicaid Managed Care. Expenditures for provision of residential addiction services, crisis intervention and licensed behavioral health practitioner services to MMMC enrollees only and are not provided under the state plan [Demonstration Services 9].
- Targeted Behavioral Health HCBS and CORE Services. Expenditures for the provision of BH HCBS and CORE Services under HARP and HIV SNP that are not otherwise available under the approved state plan [Demonstration Services 8].
- Self-Direction Pilot. Expenditures to allow the state to make self-direction services available to HARP and HIV/SNP enrollees receiving BH HCBS or children meeting targeting criteria for the Children's 1915(c) Waiver and in MMMC receiving HCBS under the Children's Waiver. The program will be in effect from January 1, 2017, through March 31, 2027 [Demonstration Services 8].
- Residential and Inpatient Treatment for Individuals with Substance Use Disorder (SUD). Expenditures for Medicaid state plan services furnished to otherwise eligible individuals who are primarily receiving treatment and/or withdrawal management services for substance use disorder (SUD) who are short-term residents in facilities that meet the definition of an institution for mental diseases (IMD).
- Health-Related Social Needs (HRSN) Services. Expenditures for health-related social needs services not otherwise covered that are furnished to individuals who meet the qualifying criteria as described in Section 6. This expenditure authority is contingent on compliance with Section 7, as well as all other applicable STCs.
- Expenditures for HRSN Services Infrastructure. Expenditures for payments for allowable administrative costs and infrastructure not otherwise eligible for Medicaid payment, to the extent such activities are authorized in Section 6 of the STCs. This expenditure authority is contingent on compliance with Section 7 of the STCs, as well as all other applicable STCs.
- Medicaid Hospital Global Budget Initiative. Expenditures for incentive payments to eligible private not-for-profit hospitals with a 0 percent or less operating margin for meeting data collection requirements, reporting expectations, meeting milestones for transitioning to alternative payment models, and demonstrating improvement in health care quality and equity, as specified in the STCs.
- Designated State Health Programs (DSHP). Expenditures for designated programs, described in these STCs (Section 11), which are otherwise state-funded, and not otherwise eligible for Medicaid payment. These expenditures are subject to the terms and limitations and not to exceed specified amounts as set forth in these STCs. These expenditures are specifically contingent on compliance with Section 7, as well as all other applicable STCs.
- Health Equity Regional Organization (HERO). Expenditures for an independent contracted statewide entity designed to develop regionally focused approaches to reduce health disparities, advance health equity, and support the delivery of health-related social needs as described in Section 13.
- Workforce Initiatives. Expenditures for provider student loan repayment and Career Pathway Training programs that meet the criteria as specified in Section 12 of the STCs.
- Time limited expenditure authority is granted until four years following the demonstration, in order for the state to pay close-out administrative and monitoring service commitments.
Title XIX Requirements Not Applicable to the HRSN Expenditure Authorities
Comparability; Amount, Duration, and Scope Section 1902(a)(10)(B), Section 1902(a)(17)
To the extent necessary to enable the state to provide a varying amount, duration, and scope of HRSN services to a subset of beneficiaries, depending on beneficiary needs.
Comparability; Provision of Medical Assistance and Reasonable Promptness 1902(a)(17), 1902(a)(8) Sections 1902(a)(10)(B),
To the extent necessary to allow the state to offer HRSN services to an individual who meets the qualifying criteria for HRSN services, including delivery system enrollment, as described in Section 6 of the STCs.
To the extent necessary to allow the state to delay the application review process for HRSN services in the event the state does not have sufficient funding to support providing these services to eligible beneficiaries.
SPECIAL TERMS AND CONDITIONS
NUMBER: 11-W-00114/2
TITLE: Medicaid Redesign Team
AWARDEE: New York State Department of Health
I. PREFACE
The following are the STCs for the New York Medicaid Redesign Team section 1115(a) Medicaid demonstration (hereinafter "demonstration" or "MRT") to enable the New York State Department of Health (hereinafter "state" or "DOH") to operate this demonstration. The Centers for Medicare & Medicaid Services (CMS) has granted the state waivers of requirements under section 1902(a) of the Social Security Act (hereinafter "the Act") and expenditure authorities authorizing federal matching of demonstration costs that are not otherwise matchable and which are separately enumerated.
These STCs set forth in detail the nature, character, and extent of federal involvement in the Demonstration and New York's obligations to CMS related to this demonstration. The MRT demonstration will be statewide and is approved from April 1, 2022, through March 31, 2027.
The STCs have been arranged into the following sections:
- Preface
- Program Description and Objectives
- General Program Requirements
- Populations Affected by and Eligible Under the Demonstration
- Demonstration Benefits and Enrollment
- Delivery Systems
- General Reporting Requirements
- General Financial Requirements
- Monitoring Budget Neutrality
- Evaluation of the Demonstration
- Schedule of Deliverables for the Demonstration
Additional attachments have been included to provide supplementary information and for specific STCs.
- Home and Community-Based Services (HCBS) Expansion Program Benefits
- Behavioral Health (BH) HCBS and Community Oriented Recovery and Empowerment (CORE) Services in Health and Recovery Plans (HARP)
- Mandatory Managed Long-Term Care/Care Coordination Model (CCM)
- List of Eligible Goods and Services Under BH HCBS Individual Directed Goods and Services
- Developing the Evaluation Design
- Preparing the Interim and Summative Evaluation Reports
- Evaluation Design [Reserved]
II. PROGRAM DESCRIPTION AND OBJECTIVES
The state's goal in implementing the Medicaid Redesign Team Section 1115(a) demonstration is to improve access to health services and outcomes for low-income New Yorkers by:
- Improving access to health care for the Medicaid population;
- Improving the quality of health services delivered; and
- Expanding coverage with resources generated through managed care efficiencies to additional low-income New Yorkers;
The demonstration is designed to permit New York to use a managed care delivery system to deliver benefits to Medicaid recipients, create efficiencies in the Medicaid program, and enable the extension of coverage to certain individuals who need long term care and supports. It was originally approved in 1997 to enroll most Medicaid recipients into MCOs (Medicaid managed care program). As part of the demonstration's renewal in 2006, authority to require some disabled and aged populations to enroll in mandatory managed care was transferred to a new demonstration, the Federal-State Health Reform Partnership (F-SHRP). Effective April 1, 2014, this authority was restored to this demonstration as F-SHRP was phased out.
In 2001, the Family Health Plus (FHPlus) program was implemented as an amendment to the demonstration, providing comprehensive health coverage to low-income uninsured adults, with and without dependent children, who have income greater than Medicaid state plan eligibility standards. FHPlus was further amended in 2007 to implement an employer sponsored health insurance (ESHI) component. Individuals eligible for FHPlus who have access to cost-effective ESHI are required to enroll in that coverage, with FHPlus providing any wrap-around services necessary to ensure that enrollees get all FHPlus benefits. FHPlus expired on December 31, 2013, and became a state-only program, but federal matching funding for state expenditures for FHPlus will continue to be available as a designated state health program through December 31, 2014.
In 2002, the demonstration was expanded to incorporate a family planning benefit under which family planning and family planning related services were provided to women losing Medicaid eligibility and to certain other adults of childbearing age (family planning expansion program). The family planning expansion program expired on December 31, 2013, and became a state plan benefit.
In 2010, the Home and Community Based Services Expansion program (HCBS Expansion program) was added to the demonstration. It covers cost-effective home and community-based services to certain adults with significant medical needs as an alternative to institutional care in a nursing facility. The benefits and program structure mirrors those of existing section 1915(c) waiver programs and aims to cover quality services for individuals in the community, ensure the well-being and safety of the participants and increase opportunities for self-advocacy and self-reliance.
As part of the 2011 extension, the state was authorized to develop and implement two new initiatives designed to improve the quality of care rendered to Partnership Plan recipients. The first, the Hospital-Medical Home (H-MH) project, provided funding and performance incentives to hospital teaching programs in order to improve the coordination, continuity and quality of care for individuals receiving primary care in outpatient hospital settings and facilitate certification of such programs by the National Committee for Quality Assurance as patient-centered medical homes. This demonstration initiative ended on December 31, 2014.
Under the second 2011 initiative, the state would have provided funding, on a competitive basis, to hospitals and/or collaborations or hospitals and other providers for the purpose of developing and implementing strategies to reduce the rate of Potentially Preventable Readmissions for the Medicaid population. The demonstration initiative was never implemented.
Finally, in 2011 CMS began providing matching funding for the state's program to address clinic uncompensated care through its Indigent Care Pool (ICP). This pool expired on December 31, 2014.
In 2012, New York added to the demonstration an initiative to improve service delivery and coordination of long-term care services and supports for individuals through a managed care model. Under the MLTC program, eligible individuals in need of more than 120 days of community-based long-term care are enrolled with managed care providers to receive long term services and supports as well as other ancillary services. Other covered services are available on a fee-for-service basis to the extent that New York has not exercised its option to include the individual in the MMMC program. Enrollment in MLTC was phased in geographically and by group.
The state's goals specific to MLTC are listed below:
- Expanding access to managed long-term care for Medicaid enrollees who are in need of long-term services and supports (LTSS)
- Improving patient safety and quality of care for enrollees in MLTC plans
- Reducing preventable inpatient and nursing home admissions
- Improving satisfaction, safety and quality of life
In April 2013, New York had three amendments approved. The first amendment was a continuation of the state's goal for transitioning more Medicaid beneficiaries into managed care. Under this amendment, the Long-Term Home Health Care Program (LTHHCP) participants began transitioning, on a geographic basis, from New York's 1915(c) waiver into the 1115 demonstration and into managed care. Second, this amendment eliminated the exclusion from MMMC of both foster care children placed by local social service agencies and individuals participating in the Medicaid buy-in program for the working disabled.
Additionally, the April 2013 amendment approved expenditure authority for New York to claim federal financial participation (FFP) for expenditures made for certain DSHP beginning April 1, 2013, through March 31, 2014. These DSHPs were aimed to improve health outcomes for Medicaid and other low-income individuals, and the federal funding was linked to requirements for the state to submit deliverables to demonstrate successful efforts to transform its health system for individuals with developmental disabilities.
A December 2013 amendment was approved to ensure that the demonstration made changes that were necessary in order to coordinate its programs with the Medicaid expansion and other changes made under the Affordable Care Act (ACA) implementation beginning January 1, 2014.
Effective April 1, 2014, CMS approved an amendment to extend several authorities that expired in calendar year 2014. As part of the amendment CMS extended authorities related to the transitioning of parents into state plan coverage and other authorities that provide administrative ease to the state's programs and continuing to provide services to vulnerable populations, i.e. HCBS Expansion program and individuals moved from institutional settings into community-based settings.
Also, effective April 1, 2014, populations receiving managed care or managed long-term care in the 14 counties that encompassed the Federal-State Health Reform Partnership (F-SHRP) demonstration were moved into this demonstration.
An amendment approved on April 14, 2014, allowed New York to take the first steps toward a major delivery system reform through a Delivery System Reform Incentive Payment (DSRIP) program. This amendment to the Partnership Plan demonstration provided for an Interim Access Assurance Fund (IAAF) to ensure that sufficient numbers and types of providers were available in the community to participate in the transformation activities contemplated by the DSRIP Program. The DSRIP program incentivized providers through additional payments beginning in 2015. The amendment also included expenditure authority for DSHPs to allow the state to concentrate resources on the investments necessary to implement its DSRIP program. Savings from the DSRIP program were anticipated to exceed the cost of the DSHP program.
On December 31, 2014, CMS amended the demonstration to enable New York to extend long term nursing facility services to enrollees of New York's MMMC and MLTC populations. Enrollment in MMMC and MLTC was extended to individuals entering residential health care facilities (RHCF) for stays that are classified as permanent. As part of the agreement, the state also instituted an independent LTSS assessment process via an enrollment broker and implemented its Independent Consumer Support Program in areas of the state where services and enrollment were being instituted.
In August 2015, CMS approved New York's request to implement HARP to integrate physical, behavioral health and BH HCBS for Medicaid enrollees with Serious Mental Illness (SMI) and/or SUD to receive services in their own homes and communities. Under the demonstration, HARPs are a separate coverage product that is targeted to Medicaid enrollees that meet need-based criteria for SMI and/or SUD established by the state. HIV SNP under MMMC will also offer BH HCBS services to eligible individuals meeting targeting, risk, and functional needs criteria. All MMMC plans will offer BH benefits in integrated plans including four new demonstration services.
The demonstration was also amended to effectuate eligibility flexibilities for the Adult Group, including allowing adults enrolled in TANF to be enrolled as a demonstration population, without a MAGI determination, extension of continuous eligibility for members of the Adult Group who turn 65 during their continuous eligibility period and temporary coverage for members of the Adult Group who are determined eligible to receive coverage through the Marketplace.
On November 30, 2016, CMS approved an extension of the demonstration, but in response to comments by the state, that extension was rescinded and superseded by a modified approval effective December 7, 2016. In December 2016, the Partnership Plan was renamed New York MRT. The extension included time-limited authorization to extend the DSRIP program first authorized in 2014, through March 31, 2020. The extension also included a new time-limited DSHP authority to the extent that the state increases its Medicaid expenditures through its DSRIP program and achieves metrics that will result in anticipated cost savings that offset the DSHP expenditures. DSHP funding will be phased down over the demonstration period. The DSRIP and DSHP authorities are intended to be a one-time investment in system transformation that can be sustained through ongoing payment mechanisms and/or state and local initiatives.
The Behavioral Health Self-Direction Pilot was included as part of the renewal. This pilot made self-direction services available to HARP and HIV SNP enrollees receiving BH HCBS. The program is authorized to be in effect from January 1, 2017, through March 31, 2027
On April 19, 2019, CMS approved an amendment to allow a waiver of comparability which permits managed care enrollees to only be assessed a drug copay. The state will not assess the non-drug benefit cost sharing described in the Medicaid state plan.
On August 2, 2019, CMS approved an amendment containing the following changes:
- Allow children with HCBS under the state's 1915(c) Children's Waiver and children placed in foster care through a Voluntary Foster Care Agency (VFCA) to enroll in Mainstream Managed Care or an HIV SNP.
- Continues Medicaid eligibility for Non-1915 children who would have been eligible under the Children's Waiver had case management not been moved under the State Plan as a Health Home service or who were in a non-SSI category and receive HCBS or Health Home (HH) comprehensive case management.
- Include Children's Waiver HCBS and State Plan behavioral health services in the Medicaid managed care benefit package.
- Include children receiving HCBS under the Children's waiver in the Self Direction Pilot for Individual Directed Goods and Services.
On December 19, 2019, CMS approved an amendment with the following changes for Partially Capitated MLTC plans:
- Implement a lock-in policy for partially capitated MLTC plans, pursuant to which enrollees of partially capitated MLTC plans are able to transfer to another partially capitated plan without cause during the first 90 days of a 12-month period and with good cause during the remainder of the period. A member of a partially capitated MLTC plan may transfer to another type of MLTC plan at any time.
- Limit the nursing home benefit in the partially capitated MLTC plan to three months for those enrollees who have been designated as Long-Term Nursing Home Stays (LTNHS) in a skilled nursing or residential health care facility, at which time the individual will be involuntarily disenrolled from the partially capitated MLTC plan and payment for nursing home services will be covered by Medicaid fee for service for individuals that qualify for institutional Medicaid coverage. Consistent with this partially capitated MLTC benefit change, individuals age 21 years of age or older who are dually eligible for Medicare and Medicaid and LTNHS in a nursing home will be excluded from enrollment in a partially capitated MLTC plan.
On October 5, 2021, CMS approved an amendment that added a set of rehabilitative services (as such term is defined in Section 1905(a)(13) of the Social Security Act) called CORE, substitutes for and improves upon four BH HCBS within the HARP and HIV SNP. CORE Services can be found in Attachment D and are available to HARP members and HIV SNP members meeting HARP eligibility criteria for whom such services are recommended by a physician or Licensed Practitioner of the Healing Arts as defined by New York State. Through the transition to CORE Services, the State will improve access to rehabilitation and recovery services for HARP beneficiaries. New York State will ensure continuity of care for individuals for BH HCBS including the four services transitioning to CORE. Individuals receiving or eligible for remaining BH HCBS and the BH HCBS, which directly transition to CORE Services will not receive a reduction in services and/or eligibility based on this Waiver amendment. An updated list of BH HCBS can also be found in Attachment D.
On March 23, 2022, CMS approved a 5-year extension of the New York Medicaid Redesign Team demonstration. As part of the extension, CMS approved the state's second component of its managed long-term care (MLTC) amendment request to allow dual eligibles to stay in Mainstream Managed Care Plans that offer D-SNPs once they become eligible for Medicare.
III. GENERAL PROGRAM REQUIREMENTS
- Compliance with Federal Non-Discrimination Statutes. The state must comply with all applicable federal statutes relating to non-discrimination. These include, but are not limited to, the Americans with Disabilities Act of 1990 (ADA), Title VI of the Civil Rights Act of 1964, section 504 of the Rehabilitation Act of 1973 (Section 504), the Age Discrimination Act of 1975, and section 1557 of the Patient Protection and Affordable Care Act (Section 1557).
- Compliance with Medicaid and Children's Health Insurance Program (CHIP) Law, Regulation, and Policy. All requirements of the Medicaid and CHIP programs expressed in federal law, regulation, and policy statement, not expressly waived or identified as not applicable in the waiver and expenditure authority documents (of which these terms and conditions are part), apply to the demonstration.
- Changes in Medicaid and CHIP Law, Regulation, and Policy. The state must, within the timeframes specified in federal law, regulation, or written policy, come into compliance with any changes in law, regulation, or policy affecting the Medicaid or CHIP programs that occur during this demonstration approval period, unless the provision being changed is expressly waived or identified as not applicable. In addition, CMS reserves the right to amend the STCs to reflect such changes and/or changes as needed without requiring the state to submit an amendment to the demonstration under STC 7 section III. CMS will notify the state 30 business days in advance of the expected approval date of the amended STCs to allow the state to provide comment. Changes will be considered in force upon issuance of the approval letter by CMS. The state must accept the changes in writing.
- Impact on Demonstration of Changes in Federal Law, Regulation, and Policy.
- To the extent that a change in federal law, regulation, or policy requires either a reduction or an increase in federal financial participation (FFP) for expenditures made under this demonstration, the state must adopt, subject to CMS approval, a modified budget neutrality agreement for the demonstration as necessary to comply with such change, as well as a modified allotment neutrality worksheet as necessary to comply with such change. The trend rates for the budget neutrality agreement are not subject to change under this subparagraph. Further, the state may seek an amendment to the demonstration (as per STC 7 of this section) as a result of the change in FFP.
- If mandated changes in the federal law require state legislation, unless otherwise prescribed by the terms of the federal law, the changes must take effect on the earlier of the day such state legislation becomes effective, or on the last day such legislation was required to be in effect under the law, whichever is sooner.
- State Plan Amendments. The state will not be required to submit title XIX or XXI state plan amendments (SPA) for changes affecting any populations made eligible solely through the demonstration. If a population eligible through the Medicaid or CHIP state plan is affected by
- change to the demonstration, a conforming amendment to the appropriate state plan is required, except as otherwise noted in these STCs. In all such cases, the Medicaid and CHIP state plans govern.
- Changes Subject to the Amendment Process. Changes related to eligibility, enrollment, benefits, beneficiary rights, delivery systems, cost sharing, sources of non-federal share of funding, budget neutrality, and other comparable program elements must be submitted to CMS as amendments to the demonstration. All amendment requests are subject to approval at the discretion of the Secretary in accordance with section 1115 of the Act. The state must not implement changes to these elements without prior approval by CMS either through an approved amendment to the Medicaid or CHIP state plan or amendment to the demonstration. Amendments to the demonstration are not retroactive and no FFP of any kind, including for administrative or medical assistance expenditures, will be available under changes to the demonstration that have not been approved through the amendment process set forth in STC 7 below, except as provided in STC 3.
- Amendment Process. Requests to amend the demonstration must be submitted to CMS for approval no later than 120 calendar days prior to the planned date of implementation of the change and may not be implemented until approved. CMS reserves the right to deny or delay approval of a demonstration amendment based on non-compliance with these STCs, including but not limited to the failure by the state to submit required elements of a complete amendment request as described in this STC, and failure by the state to submit required reports and other deliverables according to the deadlines specified therein. Amendment requests must include, but are not limited to, the following:
- An explanation of the public process used by the state, consistent with the requirements of STC 12 of this section. Such explanation must include a summary of any public feedback received and identification of how this feedback was addressed by the state in the final amendment request submitted to CMS;
- A detailed description of the amendment, including impact on beneficiaries, with sufficient supporting documentation;
- A data analysis which identifies the specific "with waiver" impact of the proposed amendment on the current budget neutrality agreement. Such analysis must include current total computable "with waiver" and "without waiver" status on both a summary and detailed level through the current approval period using the most recent actual expenditures, as well as summary and detailed projections of the change in the "with waiver" expenditure total as a result of the proposed amendment, which isolates (by Eligibility Group) the impact of the amendment;
- An up-to-date CHIP allotment worksheet, if necessary;
- The state must provide updates to existing demonstration reporting and quality and evaluation plans. This includes a description of how the evaluation design and annual progress reports will be modified to incorporate the amendment provisions, as well as the oversight, monitoring and measurement of the provisions.
- Extension of the Demonstration. States that intend to request an extension of the demonstration must submit an application to CMS from the Governor or Chief Executive Officer of the state in accordance with the requirements of 42 CFR §431.412(c). States that do not intend to request an extension of the demonstration beyond the period authorized in these STCs must submit phase-out plan consistent with the requirements of STC 9.
- Demonstration Phase-Out. The state may only suspend or terminate this demonstration in whole, or in part, consistent with the following requirements.
- Notification of Suspension or Termination: The state must promptly notify CMS in writing of the reason(s) for the suspension or termination, together with the effective date and a transition and phase-out plan. The state must submit a notification letter and a draft transition and phase-out plan to CMS no less than six months before the effective date of the demonstration's suspension or termination. Prior to submitting the draft transition and phase-out plan to CMS, the state must publish on its website the draft transition and phase-out plan for a 30-day public comment period. In addition, the state must conduct tribal consultation in accordance with STC 12, if applicable. Once the 30-day public comment period has ended, the state must provide a summary of the issues raised by the public during the comment period and how the state considered the comments received when developing the revised transition and phase-out plan.
- Transition and Phase-out Plan Requirements: The state must include, at a minimum, in its phase-out plan the process by which it will notify affected beneficiaries, the content of said notices (including information on the beneficiary's appeal rights), the process by which the state will conduct administrative reviews of Medicaid or CHIP eligibility prior to the termination of the demonstration for the affected beneficiaries, and ensure ongoing coverage for eligible beneficiaries, as well as any community outreach activities the state will undertake to notify affected beneficiaries, including community resources that are available.
- Transition and Phase-out Plan Approval. The state must obtain CMS approval of the transition and phase-out plan prior to the implementation of transition and phase-out activities. Implementation of transition and phase-out activities must be no sooner than 14 calendar days after CMS approval of the transition and phase-out plan.
- Transition and Phase-out Procedures: The state must comply with all applicable notice requirements found in 42 CFR, part 431 subpart E, including sections 431.206, 431.210 and 431.213. In addition, the state must assure all applicable appeal and hearing rights are afforded to beneficiaries in the demonstration as outlined in 42 CFR, part 431 subpart E, including sections 431.220 and 431.221. If a beneficiary in the demonstration requests a hearing before the date of action, the state must maintain benefits as required in 42 CFR §431.230. In addition, the state must conduct administrative renewals for all affected beneficiaries in order to determine if they qualify for Medicaid or CHIP eligibility under a different eligibility category prior to termination, as discussed in October 1, 2010, State Health Official Letter #10-008 and as required under 42 CFR 435.916(f)(1). For individuals determined ineligible for Medicaid, the state must determine potential eligibility for other insurance affordability programs and comply with the procedures set forth in 42 CFR 435.1200(e).
- Exemption from Public Notice Procedures 42 CFR Section 431.416(g). CMS may expedite the federal and state public notice requirements under circumstances described in 42 CFR 431.416(g).
- Enrollment Limitation during Demonstration Phase-Out. If the state elects to suspend, terminate, or not extend this demonstration, during the last six months of the demonstration, enrollment of new individuals into the demonstration must be suspended. The limitation of enrollment into the demonstration does not impact the state's obligation to determine Medicaid eligibility in accordance with the approved Medicaid state plan.
- FFP. If the project is terminated or any relevant waivers are suspended by the state, FFP must be limited to normal closeout costs associated with the termination or expiration of the demonstration including services, continued benefits as a result of beneficiaries' appeals, and administrative costs of disenrolling beneficiaries.
- Withdrawal of Waiver or Expenditure Authority. CMS reserves the right to withdraw waivers and/or expenditure authorities at any time it determines that continuing the waiver or expenditure authorities would no longer be in the public interest or promote the objectives of title XIX and title XXI. CMS will promptly notify the state in writing of the determination and the reasons for the withdrawal, together with the effective date, and afford the state an opportunity to request a hearing to challenge CMS' determination prior to the effective date. If a waiver or expenditure authority is withdrawn, FFP is limited to normal closeout costs associated with terminating the waiver or expenditure authority, including services, continued benefits as a result of beneficiary appeals, and administrative costs of disenrolling beneficiaries.
- Adequacy of Infrastructure. The state will ensure the availability of adequate resources for implementation and monitoring of the demonstration, including education, outreach, and enrollment; maintaining eligibility systems; compliance with cost sharing requirements; and reporting on financial and other demonstration components.
- Public Notice, Tribal Consultation, and Consultation with Interested Parties. The state must comply with the state notice procedures as required in 42 CFR 431.408 prior to submitting an application to extend the demonstration. For applications to amend the demonstration, the state must comply with the state notice procedures set forth in 59 Fed. Reg. 49249 (September 27, 1994) prior to submitting such request. The state must also comply with the Public Notice Procedures set forth in 42 CFR 447.205 for changes in statewide methods and standards for setting payment rates.
- The state must also comply with tribal and Indian Health Program/Urban Indian Organization consultation requirements at section 1902(a)(73) of the Act, 42 CFR 431.408(b), State Medicaid Director Letter #01-024, or as contained in the state's approved Medicaid State Plan, when any program changes to the demonstration, either through amendment as set out in STC 7 of this section or extension, are proposed by the state.
- Federal Financial Participation (FFP). No federal matching funds for expenditures for this demonstration, including for administrative and medical assistance expenditures, will be available until the effective date identified in the demonstration approval letter, or if later, as expressly stated within these STCs.
- Administrative Authority. When there are multiple entities involved in the administration of the demonstration, the Single State Medicaid Agency must maintain authority, accountability, and oversight of the program. The State Medicaid Agency must exercise oversight of all delegated functions to operating agencies, MCOs, and any other contracted entities. The Single State Medicaid Agency is responsible for the content and oversight of the quality strategies for the demonstration.
- Common Rule Exemption. The state must ensure that the only involvement of human subjects in research activities that may be authorized and/or required by this demonstration is for projects which are conducted by or subject to the approval of CMS, and that are designed to study, evaluate, or otherwise examine the Medicaid or CHIP program - including public benefit or service programs, procedures for obtaining Medicaid or CHIP benefits or services, possible changes in or alternatives to Medicaid or CHIP programs and procedures, or possible changes in methods or levels of payment for Medicaid benefits or services. CMS has determined that this demonstration as represented in these approved STCs meets the requirements for exemption from the human subject research provisions of the Common Rule set forth in 45 CFR 46.104(d)(5).
IV. POPULATIONS AFFECTED BY AND ELIGIBILITY UNDER THE DEMONSTRATION
- Eligible under the Medicaid State Plan (State Plan Eligibles). Mandatory and optional Medicaid state plan populations derive their eligibility through the Medicaid state plan and are subject to all applicable Medicaid laws and regulations in accordance with the Medicaid state plan, except as expressly waived and as further described in these STCs. Should the state amend the state plan to make any changes to eligibility for Medicaid mandatory populations, upon submission of the state plan amendment, the state must notify CMS in writing of the pending state plan amendment. The Medicaid Eligibility Groups (MEGs) listed in the Reporting and the Budget Neutrality sections of the STCs will be updated upon approval of changes to State plan eligibility and will be considered a technical change to the STCs.
- Individuals Not Otherwise Eligible under the Medicaid State Plan. Beneficiary eligibility groups who are made eligible for the demonstration by virtue of the expenditure authorities expressly granted in this demonstration are subject to Medicaid laws or regulations, except for those identified as non-applicable in the expenditure authorities for this document. Eligibility criteria are described elsewhere in this section. Individuals made eligible under this demonstration by virtue of the expenditure authorities expressly granted include:
- Individuals in the HCBS Expansion program;
- Individuals moved from Institutional Settings to Community Settings and receiving MLTC but who would have excess income or resources under the state plan;
- Adults who are receiving TANF benefits and have not been determined eligible using MAGI-based methods;
- Individuals previously eligible in the adult group who are no longer eligible in that group but are still within a 12-month continuous eligibility period;
- Children under age 21 who are medically needy (both Supplemental Security Income (SSI)-related and non-SSI related) and have parental income and resources (if applicable) waived and otherwise meet eligibility criteria for 1915(c) waiver #.4125 as Fo1 Demonstration children;
- People who are not eligible under the Children's waiver. Note: Unlike the Fo1 Children's (Demonstration Population 12) expenditures authorized under section 1115(a)(2) in these STCs, additional Family of One Children (SSI-related) that receive their HCBS under the state's Children's 1915(c) Waiver do not require this demonstration's expenditure authority.
- Program Components. The Medicaid Redesign demonstration includes two distinct components–MMMC and MLTC –each of which affects different populations, some of which are eligible under the state plan and some of which are eligible only as an expansion population under the demonstration. In addition, subsets of MMMC and MLTC are eligible for additional benefits. Table 1 summarizes the Medicaid state plan populations that are affected by the demonstration. In addition, the following expansion populations must participate in MLTC: Demonstration Population 9 (HCBS Expansion) and Demonstration Population 10 (Institution to Community). More detailed descriptions follow.
Table 1: State Plan Populations Affected by the Demonstration
State Plan Mandatory and Optional Groups MMMC: Medicaid-eligible; not otherwise excluded from MMMC enrollment (includes HARP and SNP for eligible individuals) MLTC: Need more than 120 days of community-based long-term care services Pregnant Women Pregnant women (42 CFR §435.116) Income up to 218% of FPL Pregnant minors under age 21 (42 CFR §435.222) No income test Demonstration Population 2 [TANF Adult] Without Medicare: Demonstration Population 5 [Non-Duals 18-64] With Medicare: Demonstration Population 7 [MLTC Adult Age 18-64 Duals] Children Infants (218% FPL) and children under age 19 (149% FPL) (42 CFR §435.117 and §435.118) Demonstration Population 1 [TANF Child] N/A Children age 19 and 20 (42 CFR §435.222) Income up to 133% of FPL if living alone and 150% if living with parents Demonstration Population 1 TANF CHILD Without Medicare: Demonstration Population 5 [Non-Duals 18-64] With Medicare: Demonstration Population 7 [MLTC Adult Age 18-64 Duals] Medically needy children age 19 and 20 (42 CFR §435.308) Income at or below the monthly income standard or with spenddown N/A Without Medicare: Demonstration Population 5 [Non-Duals 18-64] With Medicare: Demonstration Population 7 [MLTC Adult Age 18-64 Duals] Adults Adult group (42 CFR §435.119) Over age 18, under age 65, non-disabled, non-pregnant with income up to 133% of FPL, not eligible for Medicare Part A or B benefits, not eligible under the parents and other caretaker relative group, the foster care child group, or the former foster care child group. Demonstration Population 11 [New Adult Group] New Adult Group: Demonstration Population 11 Parents and Caretakers Parents and other caretaker relatives (42 CFR §435.110 and §435.220) Income up to 133% of FPL Includes low-income adults enrolled in TANF who are exempt from receiving a MAGI determination in accordance with §1902(e)(14)(D)(i)(I) of the Act.
Includes Transitional Medical Assistance under sections 1902(a)(52) and (e)(1); 1925; and 1931(c)(2) of the Social Security ActDemonstration Population 2 [TANF Adult] Without Medicare: Demonstration Population 5 [Non-Duals 18-64] With Medicare: Demonstration Population 7 [MLTC Adult Age 18-64 Duals] Medically needy parents and other caretaker relatives (42 CFR §435.310) Income at or below the monthly income standard or with spenddown N/A Without Medicare, Demonstration population 5 [Non-Duals 18-64] With Medicare, Demonstration population 7 [MLTC Adult Age 18-64 Duals] Disabled Blind and disabled individuals age 64 and under receiving SSI (42 CFR §435.120) Voluntarily enrolled or required to enroll in managed care in those counties participating in the MRT (formerly Partnership Plan) as of October 1, 2006, Demonstration Population 3 [SSI 0 through-64] Without Medicare, Demonstration Population 5 [Non-Duals 18-64] With Medicare, Demonstration Population 7 [MLTC Adults 18-64 Duals] Medically needy adults/children aged 18 through 64 blind and disabled (42 CFR §435.322 and §324) Income at or below the monthly income standard, or with spend down to monthly income standard N/A Without Medicare, Demonstration Population 5 [Non-Duals 18-64] With Medicare, Demonstration Population 7 [MLTC Adults 18-64 Duals] Aged 18 through 64 Medicaid Buy In for Working People with Disabilities Income up to 250% of FPL Demonstration Population 2 [TANF Adult] Without Medicare, Demonstration Population 5 [Non-Duals 18-64] With Medicare, Demonstration Population 7 [MLTC Adults 18-64 Duals] Aged Aged Individuals Age 65 and Over Receiving SSI (42 CFR §435.120) Optional Adults aged 65 or older (42 CFR §435.210) Voluntarily enrolled or required to enroll in managed care in those counties participating in the MRT (formerly Partnership Plan) as of October 1, 2006, Demonstration Population 4, [SSI 65 and above] Without Medicare, Demonstration Population 6 [Non-Duals 65+] With Medicare, Demonstration Population 8 [MLTC age 65+ Duals] Medically needy age 65 and over (42 CFR §435.320) Income at or below the monthly income standard, or with spend down to monthly income standard N/A Without Medicare, Demonstration Population 6 [Non-Duals 65+] With Medicare, Demonstration Population 8 [MLTC age 65+ Duals] Foster Care Children with adoption assistance, foster care or guardianship under title IV-E (42 CFR §435.145)
No income testDemonstration Population 1 [TANF Child] N/A Children in state foster care Children receiving non IV-E guardianship assistance (42 CFR §435.222)
No income testDemonstration Population 1 [TANF Child] N/A Former foster care children up to age 26 (42 CFR §435.150)
No income testDemonstration Population 1 [TANF Child] N/A Independent Foster Care Adolescents 18 through 20 (In foster care on the date of 18th birthday) (42 CFR §435.226
No income testDemonstration Population 1 [TANF Child] Without Medicare, Demonstration Population 5 [Non-Duals 18-64] With Medicare, Demonstration Population 7 [MLTC Adults 18-64 Duals] Children receiving state adoption assistance (42 CFR 435.227) No income test Demonstration Population 1 [TANF Child] N/A
- Mainstream Medicaid Managed Care Program (MMMC). This component provides Medicaid state plan and demonstration benefits through a managed care delivery system comprised of MCOs and primary care case management (PCCM) arrangements to most recipients eligible under the state plan. All state plan eligibility determination rules apply to these individuals.
Table 2: Individuals Excluded from MMMC (including HARP and HIV SNP)
- Eligibility. Table 1 above lists the groups of individuals who receive Medicaid benefits through the mainstream Medicaid managed care component of the demonstration, as well as the relevant expenditure reporting category (demonstration population) for each.
- Exclusions and Exemptions from MMMC. Notwithstanding the eligibility criteria in STC 4.3, certain individuals cannot receive benefits through the MMMC program (i.e., excluded), while others may opt out from receiving benefits through the MMMC program (i.e., exempted). Excluded individuals are outside the demonstration and are not included in Demonstration Populations. Exempt individuals are included in the demonstration and in Demonstration Populations regardless of whether they enroll in managed care. Tables 2 and 3 list those individuals either excluded or exempted from MMMC.
* Aliessa Aliens are NOT excluded from Managed Care but are excluded from FFP.
Individuals who become eligible for Medicaid only after spending down a portion of their income Residents of state psychiatric facilities and residents of Residential Treatment Facilities for Children and Youth Individuals under age 21 who are permanent residents of Residential Health Care Facilities or temporary residents of Residential Health Care Facilities at time of enrollment Medicaid eligible infants living with incarcerated mothers Youth in Office of Children and Family Services (OCFS) facilities and in the care and custody of the Office of Family & Children Services Individuals with access to comprehensive private health insurance Certified blind or disabled children living or expected to live separate and apart from their parents for 30 days or more Individuals expected to be Medicaid eligible for less than 6 months (except for pregnant women) Individuals receiving hospice services (at time of enrollment) Individuals with a "county of fiscal responsibility" code of 97, except for individuals in the New York Office of Mental Health family care program who other than their residence in district 97 would be eligible to enroll in MMMC Individuals with a "county of fiscal responsibility" code of 98 including Individuals in an Office for People with Developmental Disabilities (OPWDD) facility or treatment center Individuals who are under 65 years of age (screened and require treatment) in the Centers for Disease Control and Prevention breast, cervical, colorectal or prostate cancer, and who are not otherwise covered under creditable health coverage (Individuals with a "county of responsibility" code of 99) Individuals who are eligible for Emergency Medicaid Aliessa Court Ordered Individuals* Residents of Assisted Living Programs
Table 3: Individuals who may be exempted from MMMC (including HARP and HIV SNP)
Individuals with chronic medical conditions who have been under active treatment for at least 6 months with a sub-specialist who is not a network provider for any Medicaid MCO in the service area or whose request has been approved by the New York State Department of Health Medical Director because of unusually severe chronic care needs. Exemption is limited to six months. Child and Youth residents of Residential Rehabilitation Services for Youth (RRSY). Note: as the RRSY services are phased into managed care through contract amendments, the children in RRSYs will mandatorily phase into the demonstration. Individuals designated as participating in Office for People with Developmental Disabilities (OPWDD)-sponsored programs Medicare recipients who enroll and remain enrolled in the MMMC plan's aligned Medicare D-SNP Native Americans Individuals in the following Section 1915(c) waiver programs: Traumatic Brain Injury (TBI) and Nursing Home Transition & Diversion (NHTD) Individuals in the Office for People with Developmental Disabilities Home and Community Based Services (OPWDD HCBS) Section 1915(c) waiver program - Managed Long Term Care (MLTC).. This component provides a limited set of Medicaid state plan benefits including long-term services and supports through a managed care delivery system to individuals eligible through the state plan who require more than 120 days of community-based long-term care services as indicated on the uniform assessment tool. See Attachment B for a listing of MLTC services. Services not provided through the MLTC program are provided on a fee-for-service basis. The state has authority to expand mandatory enrollment into MLTC to all individuals identified in under the MLTC column in Table 1 (except those otherwise excluded or exempted as outlined in 3(a)(ii) of this section).
Table 4: Individuals excluded from MLTC
- Eligibility for MLTC. Table 1 above lists the groups of individuals who may be enrolled in the Managed Long Term Care component of the demonstration as well as the relevant expenditure reporting category (demonstration population) for each. To be eligible, all individuals in this program must need more than 120 days of community-based long-term care services and for MAP and PACE also have a nursing home level of care.
- Exclusions and Exemptions from MLTC. Notwithstanding the eligibility criteria in STC 3 of this section, certain individuals cannot receive benefits through the MLTC program (i.e., excluded) while others may request an exemption from receiving benefits through the MLTC program (i.e. exempted). Excluded individuals are outside the demonstration and are not included in Demonstration Populations. Exempt individuals are included in the demonstration and in Demonstration Populations regardless of whether they enroll in managed care. Tables 4 and 5 list those individuals either excluded or exempted from MLTC.
- Non-duplication of Payment. MLTC Programs will not duplicate services included in an enrollee´s Individualized Education Program under the Individuals with Disabilities Education Act, or services provided under the Rehabilitation Act of 1973.
* Aliessa Aliens are NOT excluded from Managed Care but are excluded from FFP.
Residents of psychiatric facilities (stays exceeding 30 days) Residents of skilled nursing or residential health care facilities who have been designated as Long Term Nursing Home Stays (LTNHS) in such facility are excluded from enrollment in a partially capitated MLTC plan. Residents of skilled nursing or residential health care facilities who are enrolled in a partially capitated MLTC plan are ineligible to continue their MLTC plan enrollment if they are LTNHS for more than three months. Individuals expected to be Medicaid eligible for less than six months Individuals eligible for Medicaid benefits only with respect to tuberculosis-related services Individuals with a "county of fiscal responsibility" code 99 in Medicaid Management Information System (MMIS) (Individuals eligible only for breast and cervical cancer services) Individuals receiving hospice services (at time of enrollment) Individuals with a "county of fiscal responsibility" code of 97 (Individuals residing in a state Office of Mental Health facility) Individuals with a "county of fiscal responsibility" code of 98 including Individuals in an Office for People with Developmental Disabilities (OPWDD) facility or treatment center Individuals who are under 65 years of age (screened and require treatment) in the Centers for Disease Control and Prevention (CDC) breast, cervical, colorectal and/or prostate early detection program and need treatment for breast, cervical, colorectal or prostate cancer and who are not otherwise covered under creditable health coverage Residents of intermediate care facilities for individuals with intellectual disabilities (ICF/IID) Individuals who could otherwise reside in an ICF/IID, but choose not to Residents of alcohol/substance abuse long term residential treatment programs Individuals eligible for Emergency Medicaid Individuals in the Office for People with Developmental Disabilities Home and Community Based Services (OPWDD HCBS) section 1915(c) waiver program Individuals in the following section 1915(c) waiver programs: Traumatic Brain Injury (TBI), Nursing Home Transition & Diversion (NHTD) (see Attachment C) Residents of Assisted Living Programs Individuals in receipt of Limited Licensed Home Care Services Individuals in the Foster Family Care Demonstration Aliessa Court Ordered Individuals*
Table 5: Individuals who may be exempted from MLTC
Individuals aged 18 through 20 who are nursing home certifiable and require more than 120 days of community based long term care services Native Americans Individuals who are eligible for the Medicaid buy in for the working disabled and are nursing home certifiable - Home and Community Based Services Expansion Program (HCBS Expansion). This component provides home and community-based services similar to those provided under the state´s section 1915(c) HCBS waivers (Nursing Home Transition and Diversion Program/NHTD, and Traumatic Brain Injury Program/TBI) to certain medically needy individuals. These services enable these individuals to live at home with appropriate supports rather than in a nursing facility. See Attachment C for HCBS Expansion services. All HCBS Expansion individuals will be transitioned as appropriate to MLTC.
- Eligibility for the HCBS Expansion. This group, identified as Demonstration Population 9/HCBS Expansion, includes married medically needy individuals1:
- who meet a nursing home level of care;
- whose spouse lives in the community; and
- who would be income-eligible for Medicaid services in the community but for the application of the spousal impoverishment eligibility and post-eligibility rules of section 1924 of the Act.
- Health and Recovery Plans (HARP): This component provides integrated Medicaid covered services and services specifically to address the needs of individuals with a SMI and SUD conditions under the demonstration. Members enrolled in the Health and Recovery Plans described below may elect to remain enrolled in mainstream MCOs. Within the HARPs, a benefit package of BH HCBS and Community Oriented Recovery and Empowerment (CORE) Services are provided, in addition to the existing MMMC benefit package (excluding long term nursing facility services). See Attachment B for a listing of BH HCBS and CORE Services.
- Eligibility for HARP. Eligible individuals include Medicaid adult beneficiaries age 21 or over eligible for Medicaid furnished in MMMC under the demonstration with a specified SMI and/or serious SUD diagnosis and who meet categorical criteria or risk factors specified by New York's Office of Mental Health (OMH) or New York's Office of Addiction Services and Supports (OASAS) identified by a:
- review of behavioral health service utilization, or
- receipt of a qualifying score on a state-approved assessment tool.
- Population-Specific Program Requirements
- MMMC Enrollment of Individuals Living with HIV. The state is authorized to require individuals living with HIV to receive benefits through MMMC. Individuals living with HIV will have 30 days in which to select a health plan. If no selection is made, the individual will be auto-assigned to an MCO. Individuals living with HIV who are enrolled in an MCO (voluntarily or by default) may request transfer to an HIV SNP at any time if one or more HIV SNPs are in operation in the individual's district. Further, transfers between HIV SNPs will be permitted at any time. Individuals in HIV SNPs will be eligible for BH HCBS if meeting the targeting, risk and functional needs requirements for BH HCBS. Individuals in HIV SNPs will be eligible for CORE if they otherwise would meet HARP eligibility criteria. HIV SNPs will meet all requirements of MMMC plans providing LTSS as well as HARP plans relating to delivery of BH HCBS and CORE.
- Restricted Recipient Programs. The state may require individuals participating in a restricted recipient program administered under 42 CFR 431.54(e) to enroll in MMMC or MLTC. Furthermore, MCOs may establish and administer restricted recipient programs, through which they identify individuals that have utilized Medicaid services at a frequency or amount that is not medically necessary, as determined in accordance with utilization guidelines established by the state and restrict them for a reasonable period of time to obtain Medicaid services from designated providers only. The state must adhere to the following terms and conditions in this regard.
- Restricted recipient programs operated by MCOs must adhere to the requirements in 42 CFR 431.54(e) (1) through (3), including the right to a hearing conducted by the state.
- The state must require MCOs to report to the state whenever they want to place a new person in a restricted recipient program. The state must maintain summary statistics on the numbers of individuals placed in restricted recipient programs, and the reasons for those placements, and must provide the information to CMS upon request.
- Individuals Moved from Institutional Settings to Community Settings for Long Term Services and Supports. Individuals discharged from a nursing facility who enroll into or remain enrolled in the MLTC program in order to receive community based long term services and supports or who move from an adult home as defined in subdivision 25 of section 2 of the social services law, to the community and, if applicable, enroll into the MLTC program, are eligible based on a special income standard. The special income standard is also available to MLTC members who were enrolled in the program as a result of the mandatory Nursing Facility transition, and subsequently able to be discharged to the community from the nursing facility, with the services of MLTC program in place. For married individuals who meet the criteria to be considered an "institutionalized spouse," spousal impoverishment rules shall apply. Eligibility is not based on the special income standard for individuals subject to spousal impoverishment rules. The special income standard will be determined by utilizing the average Department of Housing and Urban Development (HUD) Fair Market Rent (FMR) dollar amounts for each of the seven regions in the state, and subtracting from that average, 30 percent of the Medicaid income level (as calculated for a household of one) that is considered available for housing. The seven regions of the state include: Central, Northeastern, Western, Northern Metropolitan, New York City, Long Island and Rochester.
The state shall work with Nursing Home Administrators, nursing home discharge planning staff, family members and the MLTC health plans to identify individuals who may qualify for the housing disregard as they are able to be discharged from a nursing facility back into the community and remain enrolled in or newly enrolled into the MLTC program.
Enrollees receiving community based long term services and supports must be provided with nursing facility coverage through managed care, if nursing facility care is needed for 120 days or less and there is an expectation that the enrollee will return to community-based settings. During the short-term nursing facility stay, the state must retain the enrollees' community maintenance needs allowance. In addition, the state will ensure that the MLTC MCOs work with individuals, their families, nursing home administrators, and discharge planners to help plan for the individual's move back into the community, as well as to help plan for the individual's medical care once he/she has successfully moved into his/her home. For dually eligible enrollees, the MCO is responsible for implementing and monitoring the plan of care between Medicare and Medicaid. The MCO must assure the services are available to the enrollee.- Continuous Eligibility Period
- Duration. The state is authorized to provide a 12-month continuous eligibility period to the groups of individuals specified in Table 6, regardless of the delivery system through which they receive Medicaid benefits. Each newly eligible individual's 12-month period shall begin at the initial determination of eligibility; for those individuals who are re-determined eligible consistent with Medicaid state plan rules, the 12-month period begins at that point. At each annual eligibility redetermination thereafter, if an individual is re-determined eligible under the Medicaid state plan the individual is guaranteed a subsequent 12-month continuous eligibility period. 12-month continuous eligibility is also authorized for the Adult Group under section 1902(a)(10)(A)(i)(VIII) of the Act.
- Exceptions. Notwithstanding subparagraph (a), if any of the following circumstances occur during an individual's 12-month continuous eligibility period, the individual's Medicaid eligibility shall be terminated, suspended or re-determined:
- The individual cannot be located
- The individual is no longer a New York State resident
- The individual requests termination of eligibility
- The individual dies
- The individual fails to provide, or cooperate in obtaining a Social Security Number, if otherwise required
- The individual provided an incorrect or fraudulent Social Security Number
- The individual was determined eligible for Medicaid in error
- The individual is receiving treatment in a setting where Medicaid eligibility is not available (e.g. institution for mental disease)
- The individual is receiving care, services or other supplies under a section 1915 waiver
- The individual was previously otherwise qualified for emergency medical assistance benefits only, based on immigration status, but is no longer qualified because the emergency has been resolved
- The individual fails to provide the documentation of citizenship or immigration status required under federal law
- The individual is incarcerated
- The individual turns 65 years of age and is no longer eligible for the Adult Group
- The individual policy holder fails to provide documentation of third-party health insurance
Table 6: Groups Eligible for a 12 Month Continuous Eligibility Period
State Plan Mandatory and Optional Groups Statutory or Regulatory Reference Individuals determined eligible as pregnant women 42 CFR § 435.116 Individuals determined eligible as the Adult Group 42 CFR § 435.119 Individuals determined eligible as parents or other caretaker relatives 42 CFR § 435.110 Low-income families, except for children § 1931 of the SSA V. DEMONSTRATION BENEFITS AND ENROLLMENT
- Alternative Benefit Plan. The Affordable Care Act Adult Group will receive benefits provided through the state's approved Alternative Benefit Plan (ABP) SPA.
- Demonstration Benefits. The following benefits are provided through the indicated delivery system to individuals eligible for the Medicaid managed care components of the demonstration:
- Mainstream Medicaid Managed Care (MMMC). State plan and demonstration benefits are delivered through MCOs with the exception of certain services carved out of the MMMC contract and delivered directly by the state on a fee-for-service basis. All MMMC benefits (regardless of delivery method), as well as the co-payments charged to MMMC recipients. In addition to state plan benefits, there are three demonstration services provided only to all enrollees in MMMC under the demonstration.
- Cost Sharing for MMMC. MMMC beneficiaries including HARPs and HIV-SNPs, who are not otherwise exempt from cost sharing consistent with 447.56(a)(1), will be charged drug copays that are approved in the Medicaid state plan. MMMC beneficiaries will not be subject to any non-drug copays that are described in the Medicaid state plan.
- Children's HCBS. MMMC plans will provide HCBS for children not otherwise excluded or exempted from MMMC under the concurrent authority of the 1915(c) Children's waiver and this 1115 demonstration. Independent assessments and person-centered services planning for HCBS under the Children's waiver will be conducted by a State Plan Health Home provider or the state's Independent Entity as described and included in the approved Children's waiver. All HCBS benefits are listed in the approved Children's waiver or the approved State Plan for Community First Choice Option (CFCO). All reimbursement for Children's Waiver HCBS will be non-risk for the first 24 months subject to the non-risk UPL at 42 CFR 447.362. The MCO must pay the FFS fee schedule for non-risk services as long as the HCBS are non-risk (i.e., 24 months). There are no co-payments for Children's waiver services.
- Managed Long Term Care. State plan benefits are delivered through MCOs or, in certain districts, prepaid inpatient health plans, with the exception of certain services carved out of the MLTC contract and delivered directly by the state on a fee-for-service basis.
- For those individuals receiving a nursing home benefit in the partially capitated MLTC plan they will be limited to three months for those enrollees who have been designated as LTNHS in a skilled nursing or residential health care facility as of the effective date of this amendment. After three months the individual will be involuntarily disenrolled from the partially capitated MLTC plan and payment for nursing home services will be covered by Medicaid fee for service for individuals who qualify for institutional Medicaid coverage.
- Should an individual prefer discharge–and an assessment of the individual's medical needs indicates they may be safely discharged to the community–they may remain enrolled in their MLTC plan, while residing in the nursing home on a temporary basis for more than three months, until their discharge plans are resolved, and the individual is transitioned out of the nursing home.
- Health and Recovery Plans (HARP). State plan and demonstration benefits that are identical to MMMC with an additional component that provides BH HCBS and CORE for SMI and SUD needs will be provided by the HARPs. Long term care services (in excess of 120 days) or permanent placement in a Nursing facility, however, are not provided by HARPs. There are no co-payments for HARP services. All BH HCBS and CORE benefits are listed in Attachment B. CORE Services for HARP enrollees and BH HCBS for HARP enrollees meeting targeting, risk, and need-based functional criteria are only provided under the demonstration. The state must update the Medicaid state plan for rehabilitation and other mental health and substance use disorder services as identified through a companion letter to TN 10-38 as well as substance use disorder demonstration services not described in the current state plan. HIV SNPs also provide CORE to enrollees meeting HARP eligibility criteria and BH HCBS to enrollees meeting targeting, risk, and need-based criteria. The state will adhere to all state plan requirements pertaining to comparability. Below is a table showing how the state defines its services under CORE, and how this compares to services under BH HCBS.
Table 7 - BH HCBS and CORE
Existing BH HCBS before CORE Service Crosswalk after CORE Transition BH HCBS Community Psychiatric Support & Treatment (CPST) CORE Community Psychiatric Support & Treatment (CPST) BH HCBS Family Support and Training (FST) CORE Family Support and Training (FST) BH HCBS Empowerment Services - Peer Support CORE Empowerment Services - Peer Support BH HCBS Psychosocial Rehabilitation (PSR) CORE Psychosocial Rehabilitation (PSR) BH HCBS Short-Term Crisis Respite Crisis Intervention, including Short-Term Crisis Respite - already available to all Medicaid managed care recipients BH HCBS Intensive Crisis Respite Crisis Intervention, including Intensive Crisis Respite - already available to all Medicaid managed care recipients BH HCBS Education Support Services No change BH HCBS Pre-Vocational Services No change BH HCBS Transitional Employment No change BH HCBS Intensive Supported Employment No change BH HCBS Ongoing Supported Employment No change BH HCBS Habilitation No change BH HCBS Non-Medical Transportation No change
- HARPs Services Tiers. HARP enrollees receive BH HCBS services under the following tier structure in accordance with their person-centered plan of care. HARP enrollees are permitted to appeal any service denial decisions.
- Tier 1 BH HCBS services include:
- Employment supports
- Education supports
- Tier 2 includes all Tier 1 BH HCBS services plus additional services as specified in Attachment J to individuals whose medical need surpasses the need for Tier 1 services.
- HARPs Services Utilization Thresholds. The following thresholds will limit coverage of HARPs-specific services for individual HARPs enrollees. These limits will not affect state plan or other demonstration benefits. The state will track and report overall utilization, including any utilization threshold exceeded for clinical reasons, to ensure cost containment as well as compile sufficient fee for service data to submit HARPs capitation rates to CMS for approval.
- Tier 1 -- Threshold of $8,000 per person, per 12-month period. Up to $10,000 in services are permitted. For ROS, the thresholds will be adjusted to reflect the HCBS rate differentials.
- Tier 2 -- Threshold of $16,000 per person, per 12-month period. Up to $20,000 in services are permitted. For ROS, the thresholds will be adjusted to reflect the HCBS rate differentials.
- Self-Direction Pilot. The Self-direction Demonstration will be available to HARP and HIV/SNP enrollees eligible for receiving BH HCBS services or children meeting the target criteria of the Children's waiver and receiving HCBS under the Children's waiver through MMMC. The program will be in effect from January 1, 2017, through March 31, 2027. It will include 8 pilot sites phased in over the demonstration.
- Voluntary Enrollment and Disenrollment from Self-Direction Pilot. Participation in the Self-Direction pilot is voluntary, and participants may opt out at any time.
- Enrollee Notification. The state must notify eligible enrollees about the option to self-direct services. The state must develop a waiting list for enrollees who wish to participate in the pilot should the demand exceed capacity.
- Choice of Providers. Self-direction pilot participants will have a choice of support broker within the service center. Each participant should have the choice of provider and location for self-directed services, except as noted in 5.2(c)(iii)(5) below.
- Services Eligible for Self-Direction: This pilot includes all behavioral health HCBS services offered by HARPs and HIV SNPs and Individual Directed Goods and Services (IDGS) detailed in Attachment D. Children meeting targeting criteria of the 1915(c) Children's waiver and receiving HCBS through MMMC are eligible to self-direct up to $2,000 in IDGS only using a Fiscal Management Services provider within the service center. Each participant will have the choice of provider and location for IDGS. Children's IDGS should be used as the funding source of last resort - only for those costs that cannot be covered by any other source and that are vital to the implementation of the POC. Individual Directed Goods and Services are services, equipment, or supplies not otherwise provided through this waiver, the 1915(c) Children's Waiver, or through the Medicaid State Plan that address an identified need in the service plan. The item or service must be identified in the service plan and either:
- decrease the need for other Medicaid services;
- promote inclusion in the community; or
- increase the participant's safety in the home environment.
- To be an eligible service:
- the participant must lack funds to purchase the item or service; and
- the service is not available through another source.
- Services Ineligible for Self-Direction: Individual goods and services that are not eligible are listed below.
- Experimental or prohibited treatments;
- Purchases for or from third parties who are family members, friends, or significant others aside from family or social functions that promote social inclusion and are incorporated in the service plan;
- Room and Board in a residential facility, including assisted living facilities;
- Tobacco products, alcohol products, firearms, contraband or illegal items;
- Pornographic materials, prostitution services, escort services;
- Payment of court-ordered costs, attorney fees, fines, restitution, or similar debts;
- Credit card payments of any kind, or similar debts;
- Items purchased for the purpose of resale;
- Gift cards or prepaid debit cards;
- Services or goods that are recreational in nature;
- Goods and services not in the service plan or related to a recovery goal, or that is solely for recreation that a household does not include a person with a disability would be expected to pay for as a household expense (e.g. subscription to a cable television service).
- Evaluation. The state shall follow the evaluation requirements specified in Section 17 below.
- Reporting. Information from the pilot must be incorporated into the quarterly and annual reports detailed in STC 14.7.
- Protocols. Payment and operational protocols must be submitted by New York to CMS within 120 days of award.
Home and Community Settings Qualities. Enrollees receiving Medicaid HCBS and LTSS services furnished through the 1115 demonstration, including individuals who receive services under the demonstration´s HCBS Expansion program, MMMC and HARP, including HIV SNP, must receive services in residential and non-residential settings located in the community, which meet CMS standards for HCBS settings as articulated in current 1915(c) policy, including regulations at 42 CFR §441.301. The Statewide Transition Plan must include HARPs BH HCBS settings and meet CMS approval for required settings to be funded beyond November 30, 2015. A full list of home and community-based qualities are provided in Attachment C. Individuals Provided with LTSS under the Demonstration. The state is authorized to require certain individuals using long-term services and supports to enroll in either Mainstream Medicaid Managed Care, or Managed Long-Term Care as identified in Section I. Once these individuals are enrolled in managed care, the state is required to provide the following protections for the population.2
- Person Centered Service Planning. All individuals utilizing long-term services and supports will have a person-centered individual service plan maintained at the MCO. Person-centered planning includes consideration of the current and unique psycho-social and medical needs and history of the enrollee, as well as the person´s functional level, and support systems. The person-centered plan is developed by the enrollee with the assistance of the MCO and individuals the enrollee chooses to include.
When a service provider is an approved State Plan Health Home3 provider and also a HCBS provider, this entity may conduct person-centered service planning, care coordination, and provision of HCBS provision as long as firewalls are constructed between the service planning, care coordination, and service provision. A home and community-based service provider who is not also an approved State Plan Health Home provider may not conduct person-centered service planning with individuals who they also provide HCBS, unless that service provider is the only qualified and willing entity available to conduct the service planning. If a service provider is the only willing and qualified entity to conduct service planning, the state must require such provider to establish firewalls between the service provision and planning functions. The person-centered plan is developed in accordance with 42 CFR §441.301(c)(4)(F)(1) through (8).- Health home program will have administrative safeguards in place when providing person-centered planning and care coordination and services that have transitioned from 1915(c) waivers to eligible health home individuals. In addition, the state agrees to meet all health home requirements including reporting annually on quality and utilization measures.
- Verification of MLTC Plan Enrollment. The state shall implement a process for MLTC plans, network and non-network providers for the state to confirm enrollment of enrollees who do not have an enrollee identification card or seek services from a provider before developing a person-centered service plan.
- Health and Welfare of Enrollees. The state shall ensure a system is in place to identify, address, and seek to prevent instances of abuse, neglect, and exploitation of its enrollees on a continuous basis. This should include provisions such as critical incident monitoring and reporting to the state, investigations of any incident including, but not limited to, wrongful death, restraints, or medication errors that resulted in an injury. In each quarterly report, the state will provide information regarding any such incidents by plan. The state will also ensure that children and adults receiving MLTC or LTSS are afforded linkages to child and/or adult protective services through all service entities, including the MCOs.
- Maintaining Accurate Beneficiary Address. New York will complete return mail tracking for enrollment notification mailings. The state will use information gained from returned mail to make additional outreach attempt through other methods (phone, email, analysis of prior claims, etc.).
- Network of Qualified Providers. The provider credentialing criteria described at 42 CFR §438.214 must apply to all providers participating in the state´s Medicaid managed care and managed long-term care programs. To the extent possible, the MCO shall incorporate criminal background checks, reviewing abuse registries as well as any other mechanism the state includes within the MCO contract.
- MMMC or MLTC Enrollment and Transition of Care Period. For initial transitions into MLTC or MMMC from fee-for-service, each enrollee receiving community-based LTSS must continue to receive services under the enrollee´s pre-existing service plan for at least 90 days after enrollment or until a care assessment has been completed. Any reduction, suspension, denial or termination of previously authorized services shall trigger the required notice under 42 CFR § 438.404 and applicable appeal rights.
Option for Consumer Directed Personal Assistance Program (CDPAP). Enrollees shall have the option to elect self-direction of Personal Assistance under the MMMC program. The state shall ensure through its contracts with the MCOs that enrollees are afforded the option to select self-direction and enrollees are informed of CDPAP as a voluntary option. Individuals who select self-direction must have the opportunity to have choice and control over how services are provided and who provides the service, except as noted in STC 2(E) of this section.
- Information and Assistance in Support of Participant Direction. The state/MCO shall have a support system that provides participants with information, training, counseling, and assistance, as needed or desired by each participant, to assist the participant to effectively direct and manage their self-directed services. Participants shall be informed about self-directed care, including feasible alternatives, before electing the self-direction option.
- Participant Direction by Representative. The participant who self-directs the personal care service may appoint a volunteer designated representative to assist with or perform employer responsibilities to the extent approved by the participant. Services may be directed by a legal representative of the participant. Consumer-directed services may be directed by a non-legal representative freely chosen by the participant. A person who serves as a representative of a participant for the purpose of directing services cannot serve as a provider of personal attendant services for that participant.
- Participant Employer Authority. The participant (or the participant´s representative) must have decision making authority over workers who provide personal care services.
- Participant. The participant (or the participant´s representative) provides training, supervision and oversight to the worker who provides services. A Fiscal/Employer Agent that follows IRS and local tax code laws functions as the participant´s agent in performing payroll and other employer responsibilities that are required by federal and state law.
- Decision-Making Authorities. The participants exercise the following decision-making authorities: recruit staff, hire staff, verify staff´s ability to perform identified tasks, schedule staff, evaluate staff performance, verify time worked by staff and approve time sheets, and discharge staff.
- Disenrollment from Self-Direction. A participant may voluntarily disenroll from the self-directed option at any time and return to a traditional service delivery system through the MMMC, or MLTC program. To the extent possible, the member shall provide his/her intent to withdraw from participant direction. A participant may also be involuntarily disenrolled from the self-directed option if continued participation in the consumer-directed services option would not permit the participant´s health, safety, or welfare needs to be met, or the participant demonstrates the inability to self-direct by consistently demonstrating a lack of ability to carry out the tasks needed to self-direct services, or if there is fraudulent use of funds such as substantial evidence that a participant has falsified documents related to participant-directed services. If a participant is terminated voluntarily or involuntarily from the self-directed service delivery option, the MCO must transition the participant to the traditional agency direction option and must have safeguards in place to ensure continuity of services.
- Payment for Services Will be Made Following the Service Being Rendered and only upon receipt of an acceptable receipt, invoice or signed and approved timesheet, as applicable.
- Appeals. The following actions shall be considered adverse action under both 42 CFR §431 subpart E and 42 CFR §438 subpart F:
- a reduction, suspension or termination of authorized CDPAP services;
- A denial of a request to change Consumer Directed Personal Assistance Program services.
Adding Services to the MMMC, and/or MLTC Plan Benefit Package. At any point in time the state intends to add to either the MMMC, or MLTC plan benefit package currently authorized state plan or demonstration services that have been provided on a fee-for-service basis, the state must provide CMCS, Disabled and Elderly Health Programs Group, Division of Managed Care Plans (DMCP) the following information, with at least 30 days´ notice prior to the inclusion of the benefit, in writing:
- A description of the benefit being added to the benefit package;
- A detailed description of the state´s oversight of the MCO´s readiness to administer the benefit including:
- readiness and implementation of activities, including onsite reviews, phone meetings and desk audits that review policies and procedures for new services;
- data sharing to allow plans to create services plans as appropriate;
- process to communicate the change to enrollees;
- MCO network development to include providers of that service; and
- any other activity performed by the state to ensure plan readiness.
- Information concerning the changes being made to the MMMC and/or MLTC contract provisions and capitation payment rates in accordance with STC 2 in Section VI.
DMCP reserves the right to delay implementation of the benefit transition until such time as appropriate documentation is provided showing evidence of MCO readiness. In addition, new services that are not currently authorized under the state plan or demonstration may be added only through approved amendments to the state plan or demonstration.
DMCP will notify the state of concerns within 10 days of receiving the state´s written notice of the change. If no comments are received, the state may proceed with the scheduled benefit transition.Adding Populations to MMMC and/or MLTC Enrollment. Any time the state is ready to expand mandatory MMMC and /or MLTC plan enrollment into a new Medicaid population, the state must submit an 1115 amendment in accordance with STC 7 in Section III. The amendment request must include the following:
- a description of the population and the list of the counties that will have populations moving to mandatory enrollment;
- a list of MCO with an approved state certificate of authority to operate in those counties demonstrating that enrollees will be afforded choice of plan that will be providing services;
- confirmation that the MCO have met the network requirements in STC 10 in Section VI for each MCO; and
- an analysis of why the most appropriate authority to implement mandatory MMMC and/or MLTC for the new population, i.e. what the state is demonstrating by implementing the change to the demonstration.
Assurances During LTSS Expansion for MMMC, HIV SNP, and HARP Enrollees. To provide and demonstrate seamless transitions for enrollees, the state must (where applicable):
- Send sample notification letters. Existing Medicaid providers must receive sample beneficiary notification letters via widely distributed methods (mail, email, provider website, etc.) so that providers are informed of the information received by enrollees regarding their managed care transition.
- Provide continued comprehensive outreach, including educational tours for enrollees and providers. The educational tour should educate enrollees and providers regarding plan enrollment options, rights and responsibilities and other important program elements. The state must provide webinars, meeting plans, and send notices through outreach and other social media (e.g. state´s website). The enrollment broker, choice counseling entities, ombudsman and any group providing enrollment support must participate.
- Operate a call center independent of the MLTC, and MMMC, HIV SNP, and HARP plans. This entity must be able to help enrollees in making independent decisions about plan choice and be able to document complaints about the plans. During the first 60 days of implementation the state must review all call center response statistics to ensure all contracted plans are meeting requirements in their contracts. After the first 60 days, if all entities are consistently meeting contractual requirements the state can decrease the frequency of the review of call center statistics, but no more than 120 days should elapse between reviews.
- Review the outcomes of the auto-assignment algorithm to ensure that MLTC and MMMC plans with more limited networks do not receive the same or larger number of enrollees as plans with larger networks.
- Require MCO to maintain the current worker/recipient relationship for no less than 90 days.
Assessment of LTSS needs for MLTC, and MMMC and Behavioral Health Assessments for HARPs and HIV SNPs. LT SS needs assessments must be conflict free plans will not complete any LTSS needs assessments for individuals requesting such services prior to enrollment in a plan. Non-dually eligible individuals requesting LT SS will be assessed for criteria necessitating enrollment in MLTC or an alternate waiver program. An independent LT SS assessment must be in place in any geographic location where MLTC or, LT SS in MMMC will be mandated. An independent BH HCBS assessment system must be in place in any geographic location where HARP enrollment is an option for eligible individuals. LT SS assessments for skilled nursing facility services in MMMC, and BH HCBS assessments of enrollees aged 21 and over for HARPs and HIV SNPs will be conflict free prior to implementation and geographic phase in. Post Assessment Education. New Medicaid applicants must be provided the results of their assessment and educated on the steps in the Medicaid eligibility determination, including denial and fair hearing procedures. Individuals who are currently Medicaid eligible must be provided information regarding choice of plan. Operation of the HCBS Expansion Program. The individuals eligible for this component of the demonstration will receive the same HCBS as those individuals determined eligible for and enrolled in the state´s Nursing Home Transition and Diversion Program (NHTDP) and Traumatic Brain Injury Program (TBIP) authorized under section 1915(c) of the Act. The specific benefits provided to participants in this program are listed in Attachment C. The state will operate the HCBS Expansion program in a manner consistent with approved NHTDP and TBIP 1915(c) waiver programs and must comply with all administrative, operational, quality improvement and reporting requirements contained therein. The state shall provide enrollment and financial information about the individuals enrolled in the HCBS Expansion program. Facilitated Enrollment. Facilitated enrollers, which may include MCOs, health care providers, community-based organizations, and other entities under state contract, will engage in those activities described in 42 CFR §435.904(d)(2), as permitted by 42 CFR §435.904(e)(3)(ii), within the following parameters:
- Facilitated enrollers will provide program information to applicants and interested individuals as described in 42 CFR §435.905(a).
- Facilitated enrollers must afford any interested individual the opportunity to apply for Medicaid without delay as required by 42 CFR §435.906.
- If an interested individual applies for Medicaid by completing the information required under 42 CFR §435.907(a) and (b) and 42 CFR §435.910(a) and signing a Medicaid application, that application must be transmitted to New York State Department of Health for determination of eligibility.
- The protocols for facilitated enrollment practices between the state and the facilitated enrollers must:
- ensure that choice counseling activities are closely monitored to minimize adverse risk selection; and
- Specify that determinations of Medicaid eligibility are made solely by the Medicaid agency or its designee.
Passive Enrollment. For any component that requires passive enrollment of potential enrollees, individuals must have the ability to "opt out" Where the notice is sent 30 days in advance of the passive enrollment. The individual may opt out at any time after receipt of the notice and within the first 90 days following the passive enrollment. The individual may also change after the 12-month lock-in period at any time. Enrollees who enrolled through the health exchange or the local social services district in an MMMC plan whose MCO also operates a HARP line of business will be passively enrolled with the ability to opt-out within the first 90 days following passive enrollment and return to their original MMMC plan. Following the 90-day opt out period, HARP enrollees may not change plans again until the remainder of the twelve-month lock-in period has lapsed. HARP eligible enrollees in an MMMC plan who´s MCO does not operate a HARP line of business will be allowed to voluntarily enroll in a HARP. The enrollee must be given the choice of HARPs available for enrollment and the current plan must assist the enrollee in transferring to the HARP. The state will notify CMS and the public at least 60 days before exercising the option to modify needs-based eligibility criteria. When a HARP enrollee leaves the HARP and transfers into another plan, care must be coordinated for physical and behavioral health during the transition to best meet the needs of the enrollee. The current and new plans must work together when an enrollee transfers to another plan. HCBS Electronic Visit Verification System. The state will demonstrate compliance with the Electronic Visit Verification System (EVV) requirements for personal care services (PCS) by January 1, 2020, and home health services by January 1, 2023 in accordance with section 12006 of the 21st Century CURES Act. HCBS Quality Systems and Strategy. The state is expected to implement systems that measure and improve its performance to meet the waiver assurances set forth in 42 CFR and 441.302. The Quality Review provides a comprehensive assessment of the state´s capacity to ensure adequate program oversight, detect and remediate compliance issues and evaluate the effectiveness of implemented quality improvement activities. For 1915(c)-Approvable HCBS, for services that could have been authorized to individuals served under a 1915(c) waiver, the state must have an approved Quality Improvement Strategy and is required to develop and measure performance indicators for the following waiver assurances: The state will submit a report to CMS which includes evidence on the status of the HCBS quality assurances and measures that adheres to the requirements outlined in the March 12, 2014, CMS Informational Bulletin, Modifications to Quality Measures and Reporting in §1915(c) Home and Community-Based Waivers. (1915(c) and 1915(i) HCBS). NOTE: This information could be captured in the 1115 Summary report detailed in section VIII.
- Administrative Authority: A performance measure should be developed and tracked any authority that the State Medicaid Agency (SMA) delegates to another agency, unless already captured in another performance measure.
- Level of Care: Performance measures are required for the following two sub-assurances: applicants with reasonable likelihood of needing services receive a level of care determination and the processes for determining level of care are followed as documented. While a performance measure for annual levels of care is not required to be reported, the state is expected to be sure that annual levels of care are determined.
- Qualified Providers: The state must have performance measures that track that providers meet licensure/certification standards, that non-certified providers are monitored to assure adherence to waiver requirements, and that the state verifies that training is given to providers in accordance with the waiver.
- Service Plan: The state must demonstrate it has designed and implemented an effective system for reviewing the adequacy of service plans for HCBS participants. Performance measures are required for choice of waiver services and providers, service plans address all assessed needs and personal goals, and services are delivered in accordance with the service plan including the type, scope, amount, duration, and frequency specified in the service plan.
- Health and Welfare: The state must demonstrate it has designed and implemented an effective system for assuring HCBS participants health and welfare. The state must have performance measures that track that on an ongoing basis it identifies, addresses and seeks to prevent instances of abuse, neglect, exploitation and unexplained death; that an incident management system is in place that effectively resolves incidents and prevents further singular incidents to the extent possible; that state policies and procedures for the use or prohibition of restrictive interventions are followed; and, that the state establishes overall health care standards and monitors those standards based on the responsibility of the service provider as stated in the approved waiver.
- Financial Accountability: The state must demonstrate that it has designed and implemented an adequate system for insuring financial accountability of the HCBS program. The state must have performance measures that track that it provides evidence that claims are coded and paid for in accordance for services rendered, and that it provides evidence that rates remain consistent with the approved rate methodology throughout the five-year waiver cycle.
The state must report annually the deficiencies found during the monitoring and evaluation of the HCBS waiver assurances, an explanation of how these deficiencies have been or are being corrected, as well as the steps that have been taken to ensure that these deficiencies do not reoccur. The state must also report on the number of substantiated instances of abuse, neglect, exploitation and/or death, the actions taken regarding the incidents and how they were resolved. Submission is due no later than 6 months following the end of the demonstration year. NOTE: This information could be included in the annual reports submitted for 1115 waivers detailed in section VIII. For 1915(i)-Approvable HCBS, for services that could have been authorized to individuals served under a 1915(i) waiver, the state must have an approved Quality Improvement Strategy and is required to develop performance measures to address the following requirements:
- Service plans that:
- address assessed needs of 1915(i) participants;
- are updated annually; and
- document choice of services and providers.
- Eligibility Requirements: The state will ensure that:
- an evaluation for 1915(i) State plan HCBS eligibility is provided to all applicants for whom there is reasonable indication that 1915(i) services may be needed in the future;
- the processes and instruments described in the approved program for determining 1915(i) eligibility are applied appropriately; and
- the 1915(i) benefit eligibility of enrolled individuals is reevaluated at least annually (end of demonstration year) or if more frequent, as specified in the approved program.
- Providers meet required qualifications.
- Settings meet the home and community-based setting requirements as specified in the benefit and in accordance with 42 CFR 441.710(a)(1) and (2).
- The SMA retains authority and responsibility for program operations and oversight.
- The SMA maintains financial accountability through payment of claims for services that are authorized and furnished to 1915(i) participants by qualified providers.
- The state identifies, addresses, and seeks to prevent incidents of abuse, neglect, and exploitation.
- The state must also describe the process for systems improvement as a result of aggregated discovery and remediation activities.
Person-centered planning. The state assures there is a person-centered service plan for each individual determined to be eligible for HCBS. The person-centered service plan is developed using a person-centered service planning process in accordance with 42 CFR 441.301(c)(1) (1915(c)) or 42 CFR 441.725(c) (1915(i)), and the written person-centered service plan meets federal requirements at 42 CFR 441.301(c)(2) (1915(c)) or 42 CFR 441.725(b) (1915(i)). The person-centered service plan is reviewed and revised upon reassessment of functional need as required by 42 CFR 441.365(e), at least every 12-months, when the individual´s circumstances or needs change significantly, or at the request of the individual. Conflict of Interest: The state agrees that the entity that authorizes the services is external to the agency or agencies that provide the HCB services. The state also agrees that appropriate separation of assessment, treatment planning and service provision functions are incorporated into the state´s conflict of interest policies except for as stated in section V, STC 4(a). Each beneficiary eligible for long-term services and supports will have informed choice on their option to self-direct LTSS, have a designated representative direct LTSS on their behalf, or select traditional agency-based service delivery. Both level of care and person-centered service planning personnel will receive training on these options. (MLTSS with self-direction) The state, either directly or through its MCO contracts must ensure that participants´ engagement and community participation is supported to the fullest extent desired by each participant. (MLTSS) The state will assure compliance with the characteristics of HCBS settings as described in 1915(c) and 1915(i) regulations in accordance with implementation/effective dates as published in the Federal Register. Beneficiaries may change managed care plans if their residential or employment support provider is no longer available through their current plan. (MLTSS) VI. DELIVERY SYSTEMS
- Contracts. Procurement and the subsequent final contracts developed to implement selective contracting by the state with any provider group shall be subject to CMS approval prior to implementation. Payments under contracts with public agencies, that are not competitively bid in a process involving multiple bidders, shall not exceed the documented costs incurred in furnishing covered services to eligible individuals (or a reasonable estimate with an adjustment factor no greater than the annual change in the consumer price index that shall be rebased based on actual documented costs no less than every two years).
- Managed Care Contracts. No FFP is available for activities covered under contracts and/or modifications to existing contracts that are subject to 42 CFR §438 requirements prior to CMS approval of model contract language. The state shall submit any supporting documentation deemed necessary by CMS. The state must provide CMS with a minimum of 45 days to review and approve changes. CMS reserves the right, as a corrective action, to withhold FFP (either partial or full) for the demonstration, until the contract compliance requirement is met.
- Managed Care Data Requirements. All managed care organizations shall maintain an information system that collects, analyzes, integrates and reports data as set forth at 42 CFR §438.242. This system shall include encounter data that can be reported in a standardized format. Encounter data requirements shall include the following:
- Encounter Data (Health Plan Responsibilities). The health plan must collect, maintain, validate and submit data for services furnished to enrollees as stipulated by the state in its contracts with the health plans.
- Encounter Data (State Responsibilities). The state shall, in addition, develop mechanisms for the collection, reporting, and analysis of these, as well as a process to validate that each plan's encounter data are timely, complete and accurate. The state will take appropriate actions to identify and correct deficiencies identified in the collection of encounter data. The state shall have contractual provisions in place to impose financial penalties if accurate data are not submitted in a timely fashion. Additionally, the state shall contract with its EQRO to validate encounter data through medical record review.
- Encounter Data Validation Study for New Capitated Managed Care Plans. If the state contracts with new managed care organizations, the state shall conduct a validation study 18 months after the effective date of the contract to determine completeness and accuracy of encounter data. The initial study shall include validation through a sample of medical records of demonstration enrollees.
- Submission of Encounter Data to CMS. The state shall submit encounter data to the Medicaid Statistical Information System (MSIS) and when required T-MSIS (Transformed MSIS) as is consistent with federal law and per STC 13 in Section III. The state must assure that encounter data maintained at managed care organizations can be linked with eligibility files maintained at the state.
- Interpretation Services and Culturally Competent Care. The MCOs and other entities acting on behalf of the state Medicaid agency, including, but not limited to enrollment brokers, must have interpretation services and provide care that is consistent with the individual's culture. MCOs must conduct analyses to determine any gaps in access to these services and will expand its workforce accordingly. The MCOs may also require the use of remote video and voice technology when necessary.
- Marketing Oversight.
- The state shall require each MCO to meet 42 CFR §438.104 and state marketing guidelines regarding prohibition of cold calls, use of government logos, and other standards.
- All materials used to market the MCO shall receive prior approval from the state.
- The state shall require through its contracts that each MCO provide all individuals who were not referred to the plan by the enrollment broker with information (in a format determined by the state) describing managed long-term care, a list of available plans and contact information to reach the enrollment broker for questions or other assistance.
- Managed Care Benefit Packages. Individuals enrolled in managed care plans under the demonstration must receive from the managed care program the benefits as identified in Attachments A through F, respectively. As noted in plan readiness and contract requirements, the state must require that, for enrollees in receipt of LTSS, each MCO/PIHP coordinate, as appropriate, needs state plan services that are excluded from the managed care delivery system but available through a fee-for-service delivery system, and must also assure coordination with services not included in the established benefit package. Plans will be at risk for any Medicaid covered service that is currently delivered. BH HCBS in HARPs and HIV SNPs will be non-risk for the initial years in accordance with STC 2 of section V. If the MCO network is unable to provide necessary medical services covered under the contract to a particular enrollee, the MCO will be required to cover these services out of network for the enrollee. The costs of room and board may not be covered and cannot be included when determining the MCO payment rates.
- Managed Care Rates Transition for HARPs. While working towards a managed care capitated rate for HARPs, the state may not proceed with implementation in a region until it has approved HCBS fee for service rates for such region. The state must submit HARP capitation rates to CMS for approval no later than December 31, 2017. Should the state not have the ability to submit proposed rates, it must request a temporary extension to continue using the most recently approved rates.
- Managed Care Rate Transition for Nursing Facilities (NF). As of February 1, 2015, plans are required to pay contracted nursing homes either the existing FFS rate or a negotiated rate which allows the nursing home and the plan to engage in other financing arrangements. MLTC and MMMC plans will be reimbursed with an actuarial sound rate in compliance with 42 CFR §438.6. MLTC will develop a blended rate structure to promote community integration of institutional/Home and Community Based Services (HCBS). MMMC will develop a separate rate cell for the nursing home population and will include an HCBS "rate cohort" in its non-nursing home rate cells. The state shall submit an actuarial certification to CMS for approval of the April 1, 2015, rates that contains the following modifications:
- MLTC transition rates must be phased out
- Documentation must be submitted identifying the unique and cumulative impact of the various capitation rate withholds
- Documentation must be submitted assessing gaps in rate setting for MLTC plans that necessitate funds to mitigate risks
- Behavioral Health Services Furnished by MMMC, HIV SNPs, and HARPs. To the extent that an MCO is not able to meet the requirements for the management of the expanded behavioral health services, the MCO must contract with a managed care behavioral health organization to manage those services for enrollees. If the MCO network is unable to provide necessary medical services covered under the contract to a particular enrollee, the MCO will be required to cover these services out of network for the enrollee. This includes up to at least 2023 during which time the MCO will reimburse OMH ambulatory licensed and OASAS certified providers the FFS fee schedule to ensure continuity of care. MCOs must pay at least the FFS fee schedule for 24 months for the following services: Other Licensed Practitioner (OLP), Crisis Intervention, Community Psychiatric Support and Treatment (CPST), Psychosocial Rehabilitation (PSR), and Family and Youth Peer Support. After 90 days, the MCO may apply utilization review criteria to individuals under the care of non-participating providers. Plans will be required to authorize services and reimburse providers whether the behavioral health provider is contracted with the health plans or is an out of network provider. New York will reimburse MCOs for VFCA per diem/Preventive Residential Treatment Services on a non- risk basis subject to the non-risk UPL at 42 CFR 447.362. The MCO must pay the FFS fee schedule as long as the Preventive Residential Treatment Services are non-risk.
For SUD services and the delivery system changes associated with the new demonstration services and resulting state plan amendments including changes under the CMS IAP and with CMS approval, the state may require the MCOs through their contracts to adopt system- wide changes and rates to ensure that the innovations are adopted in a consistent manner statewide.- Independent Consumer Support Program. To support the beneficiary's experience receiving and applying to receive long term services and supports in a managed care environment, the state shall create and maintain a permanent independent consumer support program to assist beneficiaries in understanding the coverage model and in the resolution of problems regarding services, coverage, access and rights.
- Organizational Structure. The Independent Consumer Support Program shall operate independently from any MRT MCO. Additionally, to the extent possible, the program shall also operate independently of the state Medicaid agency.
- Accessibility. The services of the Independent Consumer Support Program shall be available to all Medicaid beneficiaries enrolled in MRT who are in need of LTSS (institutional, residential and community based) and must be accessible through multiple entryways (e.g., phone, internet, office) and also provide outreach in the same manner as appropriate.
- Functions. The Independent Consumer Support Program shall assist beneficiaries to navigate and access covered LTSS, including the following activities:
- offer beneficiaries support in the pre-enrollment state, such as unbiased health plan choice counseling and general program-related information;
- serve as an access point for complaints and concerns about health plan enrollment, access to services and other related matters;
- help enrollees understand the fair hearing, grievance and appeal rights and processes within the health plan and at the state level, and assist them through the process if needed/requested; and
- conduct trainings with MRT MCO and providers on community-based resources and supports that can be linked with covered plan benefits.
- Staffing. The Independent Consumer Support Program must employ individuals who are knowledgeable about the state's Medicaid programs; beneficiary protections and rights under Medicaid managed care arrangements; and the health and service needs of persons with complex needs, including those with a chronic condition, disability, and cognitive or behavioral needs.
- Data Collection and Reporting. The Independent Consumer Support Program shall track the volume and nature of beneficiary contacts and the resolution of such contacts on a schedule and manner determined by the state, but no less frequently than quarterly.
- Geographic expansion of MLTC and LTSS in MMMC. In any geographic location where the state is mandating MLTC or LTSS in MMMC, the state must have the Independent Consumer Support Program in place at least 30 days prior to enrollment procedures for that geographic location.
- Required Monitoring Activities by the State and/or EQRO. The state's EQR process for the MMMC and MLTC plans shall meet all the requirements of 42 CFR §438 Subpart E. In addition, the state, or its EQRO shall monitor and annually evaluate the MCO/PIHPs performance on specific new requirements under mandatory enrollment of individuals utilizing long term services and supports. The state shall provide an update of the processes used to monitor the following activities as well as the outcomes of the monitoring activities within the annual report in STC 8 in Section VII. The new requirements include, but are not limited to the following:
- MLTC Plan Eligibility Assessments. To ensure that approved instruments are being used and applied appropriately and as necessary, and to ensure that individuals being served with LTSS meet the MLTC program eligibility requirements for plan enrollment. The state will also monitor assessments conducted by the plan where individuals are deemed ineligible for enrollment in an MLTC plan.
- Service Plans. To ensure that MCOs are appropriately creating and implementing service plans based on the enrollee's identified needs.
- MCO credentialing and/or verification policies. To ensure that LTSS services are provided by qualified providers.
- Access to Care, Network Adequacy and Coordination of Care Requirements for Long Term Services and Supports (LTSS). The state shall set specific access and coordination requirements for MCO. These standards should take into consideration individuals with special health care needs, out of network requirements if a provider is not available within the specific access standard, ensuring choice of provider with capacity to serve individuals, time/distance standards for providers who do not travel to the individual's home, and physical accessibility of covered services. The MLTC or MMMC plan is not permitted to set these standards.
- Demonstrating Network Adequacy. Annually, each MCO must provide adequate assurances that it has sufficient capacity to serve the expected enrollment in its service area and offers an adequate coverage of benefits as described for the anticipated number of enrollees in the service area.
- The state must verify these assurances by reviewing demographic, utilization and enrollment data for enrollees in the demonstration as well as:
- the number and types of providers available to provide covered services to the demonstration population;
- the number of network providers accepting the new demonstration population; and
- the geographic location of providers and demonstration populations, as shown through GeoAccess, similar software or other appropriate methods.
- The state must submit the documentation required in subparagraphs (i) - (iii) above to CMS with each annual report.
- Enrollees and their representatives must be provided with reference documents to maintain information about available providers and services in their plans.
- Advisory Committee as required in 42 CFR §438. The state must maintain for the duration of the demonstration a managed care advisory group comprised of individuals and interested parties appointed pursuant to state law by the Legislature and Governor. To the extent possible, the state will attempt to appoint individuals qualified to speak on behalf of seniors and persons with disabilities, including individuals with developmental disabilities, regarding the impact and effective implementation of the demonstration on individuals receiving LTSS.
- Health Services to Native Americans Populations. The plan currently in place for patient management and coordination of services for Medicaid-eligible Native Americans developed in consultation with the Indian tribes and/or representatives from the Indian health programs located in participating counties shall continue in force for this extension period.
VII. GENERAL MONITORING AND REPORTING REQUIREMENTS
- General Financial Requirements. The state must comply with all general financial requirements set forth in Section IX.
- Reporting Requirements Related to Budget Neutrality. The state must comply with all reporting requirements for monitoring budget neutrality set forth in Section X.
- Monitoring Calls. CMS will convene periodic conference calls with the state.
- The purpose of these calls is to discuss ongoing demonstration operation, including (but not limited to) any significant actual or anticipated developments affecting the demonstration. Examples include implementation activities, trends in reported data on metrics and associated mid-course adjustments, budget neutrality, and progress on evaluation activities.
- CMS will provide updates on any pending actions, as well as federal policies and issues that may affect any aspect of the demonstration.
- The state and CMS will jointly develop the agenda for the calls.
- Post-Award Forum. Pursuant to 42 CFR 431.420(c), within six (6) months of the demonstration's implementation, and annually thereafter, the state shall afford the public with an opportunity to provide meaningful comment on the progress of the demonstration. At least thirty (30) days prior to the date of the planned public forum, the state must publish the date, time and location of the forum in a prominent location on its website. The state must also post the most recent Annual Monitoring Report on its website with the public forum announcement. Pursuant to 42 CFR 431.420(c), the state must include a summary of the comments in the Monitoring Report associated with the quarter in which the forum was held, as well as in its compiled Annual Monitoring Report.
- Submission of Post-Approval Deliverables. The state shall submit all deliverables as stipulated by CMS and within the timeframes outlined within these STCs.
- Compliance with Federal Systems Innovation. As federal systems continue to evolve and incorporate 1115 demonstration reporting and analytics functions, the state shall work with CMS to:
- Revise the reporting templates and submission processes to accommodate timely compliance with the requirements of the new systems;
- Ensure all 1115, Transformed Medicaid Statistical Information System (T- MSIS), and other data elements that have been agreed to for reporting and analytics are provided by the state; and
- Submit all deliverables to the appropriate system as directed by CMS.
- Deferral for Failure to Submit Timely Demonstration Deliverables. CMS may issue deferrals in the amount of $5,000,000 per deliverable (federal share) when items required by these STCs (e.g., required data elements, analyses, reports, design documents, presentations, and other items specified in these STCs) (hereafter singly or collectively referred to as "deliverable(s)") are not submitted timely to CMS or are found to not be consistent with the requirements approved by CMS. A deferral shall not exceed the value of the federal amount for the current demonstration period. The state does not relinquish its rights provided under 42 CFR part 430 subpart C to challenge any CMS finding that the state materially failed to comply with the terms of this agreement.
The following process will be used: 1) thirty (30) days after the deliverable was due if the state has not submitted a written request to CMS for approval of an extension as described in subsection (b) below; or 2) thirty (30) days after CMS has notified the state in writing that the deliverable was not accepted for being inconsistent with the requirements of this agreement and the information needed to bring the deliverable into alignment with CMS requirements:As the purpose of a section 1115 demonstration is to test new methods of operation or service delivery, a state's failure to submit all required reports, evaluations, and other deliverables will be considered by CMS in reviewing any application for an extension, amendment, or for a new demonstration.
- CMS will issue a written notification to the state providing advance notification of a pending deferral for late or non-compliant submissions of required deliverable(s). For each deliverable, the state may submit a written request for an extension to submit the required deliverable that includes a supporting rationale for the cause(s) of the delay and the state's anticipated date of submission. Should CMS agree to the state's request, a corresponding extension of the deferral process described below can be provided.
- CMS may agree to a corrective action as an interim step before applying the deferral, if corrective action is proposed in the state's written extension request.
- If CMS agrees to an interim corrective process in accordance with subsection (b), and the state fails to comply with the corrective action steps or still fails to submit the overdue deliverable(s) that meets the terms of this agreement, CMS may proceed with the issuance of a deferral against the next Quarterly Statement of Expenditures reported in Medicaid Budget and Expenditure System/State Children's Health Insurance Program Budget and Expenditure System (MBES/CBES) following a written deferral notification to the state.
- If the CMS deferral process has been initiated for state non-compliance with the terms of this agreement for submitting deliverable(s), and the state submits the overdue deliverable(s), and such deliverable(s) are accepted by CMS as meeting the standards outline in these STCs, the deferral(s) will be released.
- Quarterly and Annual Monitoring Reports. The state must submit three (3) Quarterly Monitoring Reports and one (1) compiled Annual Monitoring Report each DY. The fourth quarter information that would ordinarily be provided in a separate report should be reported as distinct information within the Annual Monitoring Report. The Quarterly Monitoring Reports are due no later than sixty (60) days following the end of each demonstration quarter. The compiled Annual Monitoring Report (including the fourth quarter information) is due no later than ninety (90) days following the end of the DY. The state must submit a revised Monitoring Report within sixty (60) calendar days after receipt of CMS's comments, if any. The reports will include all required elements as per 42 CFR 431.428, and should not direct readers to links outside the report. Additional links not referenced in the document may be listed in a Reference/Bibliography section. The Monitoring Reports must follow the framework provided by CMS, which is subject to change as monitoring systems are developed/evolve, and be provided in a structured manner that supports federal tracking and analysis.
- Operational Updates - Per 42 CFR 431.428, the Monitoring Reports must document any policy or administrative difficulties in operating the demonstration. The reports shall provide sufficient information to document key operational and other challenges, underlying causes of challenges, how challenges are being addressed, as well as key achievements and to what conditions and efforts successes can be attributed. The discussion should also include any issues or complaints identified by beneficiaries; lawsuits or legal actions; unusual or unanticipated trends; legislative updates; and descriptions of any public forums held. In addition, Monitoring Reports should describe key achievements, as well as the conditions and efforts to which these successes can be attributed. Monitoring Reports should also include a summary of all public comments received through post-award public forums regarding the progress of the demonstration. The state must report on the effect of moving NEMT and pharmacy to FFS. Metrics could include items such as NEMT and pharmacy utilization to assess beneficiary impact. The state must also report on the effect that maintaining MMMC coverage after obtaining Medicare eligibility has on beneficiaries.
- Performance Metrics - Per applicable CMS guidance and technical assistance, the performance metrics will provide data on key policies under this demonstration, including, but not limited to, behavioral health, home and community-based services, and the provision of special services to certain populations (for example, through HARP or HIV SNPs). Additionally, per 42 CFR 431.428, the Monitoring Reports must document the impact of the demonstration in providing insurance coverage to beneficiaries and the uninsured population, as well as outcomes of care, quality and cost of care, and access to care. This may also include the results of beneficiary satisfaction surveys, if conducted, and grievances and appeals. The required monitoring and performance metrics must be included in the Monitoring Reports and may follow the framework provided by CMS to support federal tracking and analysis as applicable.
- Budget Neutrality and Financial Reporting Requirements - Per 42 CFR 431.428, the Monitoring Reports must document the financial performance of the demonstration. The state must provide an updated budget neutrality workbook with every Monitoring Report that meets all the reporting requirements for monitoring budget neutrality set forth in the General Financial Requirements section of these STCs, including the submission of corrected budget neutrality data upon request. In addition, the state must report quarterly expenditures associated with the populations affected by this demonstration on the Form CMS-64. Administrative costs for this demonstration should be reported separately on the CMS-64.
- Evaluation Activities and Interim Findings - Per 42 CFR 431.428, the Monitoring Reports must document any results of the demonstration to date per the evaluation hypotheses. Additionally, the state shall include a summary of the progress of evaluation activities, including key milestones accomplished, as well as challenges encountered and how they were addressed.
- The Annual Report must at a minimum include the requirements outlined below:
- All items included in the Quarterly Reports must be summarized to reflect the operation/activities throughout the DY;
- Total annual expenditures for the demonstration population for each DY, with administrative costs reported separately;
- Total contributions, withdrawals, balances, and credits; and
- Yearly unduplicated enrollment reports for demonstration enrollees for each DY (enrollees include all individuals enrolled in the demonstration) that include the member months, as required to evaluate compliance with the budget neutrality agreement.
- Compliance with Managed Care, Network Adequacy, Quality Strategy and EQR Reporting Requirements. The state must comply with all managed care reporting regulations at 42 CFR Part §438 et. seq., except as expressly identified as not applicable in the expenditure authorities incorporated into these STCs.
- State Data Collection. The state must collect data and information necessary to oversee service utilization and rate setting by provider/plan, comply with the Core Set of Children's Health Care Quality Measures for Medicaid and CHIP (Child Core Set) and the Core Set of Adult Health Care Quality Measures for Medicaid (Adult Core Set), collectively referred to as the CMS Child and Adult Core Measure Sets for Medicaid and CHIP, obtain NCQA and other accreditations that the state may seek, and comply with other existing federal measure sets.
- The state will use this information in ongoing monitoring of individual well-being, provider/plan performance, and continuous quality improvement efforts, in addition to complying with CMS reporting requirements.
- The state must maintain data dictionary and file layouts of the data collected.
- The raw and edited data will be made available to CMS within 30 days of a written request.
- Corrective Action Plan Related to Demonstration Monitoring. If monitoring indicates that demonstration features are not likely to assist in promoting the objectives of Medicaid, CMS reserves the right to require the state to submit a corrective action plan to CMS for approval. This may be an interim step to withdrawing waivers or expenditure authorities, as outlined in STC 10 section III. CMS will withdraw an authority, as described in STC 10 section III, when metrics indicate substantial, sustained directional change, inconsistent with state targets and goals, as applicable, and the state has not implemented corrective action. CMS would further have the ability to suspend implementation of the demonstration should corrective actions not effectively resolve these concerns in a timely manner.
- Reporting Requirements Related to Individuals using Long Term Services and Supports. In each quarterly report required by Section VIII the state shall report:
- Any critical incidents reported within the quarter and the resulting investigations as appropriate.
- The number and types of grievance and appeals for this population filed and/or resolved within the reporting quarter for this population.
- The total number of assessments for enrollment performed by the plans, with the number of individuals who did not qualify to enroll in an MLTC plan.
- The number of individuals referred to an MLTC plan that received an assessment within 30 days.
- The number of people who were not referred by the enrollment broker and contacted the plan directly and were provided MLTC materials.
- Rebalancing efforts performed by the MLTC and MMMC plans once the benefit is added. Rebalancing reporting should include but is not limited to the total number of individuals transitioning in and out of a nursing facility within the quarter.
- The total number of complaints, grievances and appeals by type of issue with a listing of the top 5 reasons for the event.
VIII. GENERAL FINANCIAL REQUIREMENTS
- Allowable Expenditures. This demonstration project is approved for expenditures applicable to services rendered during the demonstration approval period designated by CMS. CMS will provide FFP for allowable demonstration expenditures only so long as they do not exceed the pre-defined limits as specified in these STCs.4
- Standard Medicaid Funding Process. The standard Medicaid funding process will be used for this demonstration. The state will provide quarterly expenditure reports through the Medicaid and CHIP Budget and Expenditure System (MBES/CBES) to report total expenditures for services provided under this demonstration following routine CMS-37 and CMS-64 reporting instructions as outlined in section 2500 of the State Medicaid Manual. The state will estimate matchable demonstration expenditures (total computable and federal share) subject to the budget neutrality expenditure limit and separately report these expenditures by quarter for each federal fiscal year on the form CMS-37 for both the medical assistance payments (MAP) and state and local administration costs (ADM). CMS shall make federal funds available based upon the state's estimate, as approved by CMS. Within thirty (30) days after the end of each quarter, the state shall submit form CMS-64 Quarterly Medicaid Expenditure Report, showing Medicaid expenditures made in the quarter just ended. If applicable, subject to the payment deferral process, CMS shall reconcile expenditures reported on form CMS-64 with federal funding previously made available to the state and include the reconciling adjustment in the finalization of the grant award to the state.
- Extent of Federal Financial Participation for the Demonstration. Subject to CMS approval of the source(s) of the non-federal share of funding, CMS will provide FFP at the applicable federal matching rate for the demonstration as a whole for the following, subject to the budget neutrality expenditure limits described in section XI:
- Administrative costs, including those associated with the administration of the demonstration;
- Net expenditures and prior period adjustments of the Medicaid program that are paid in accordance with the approved Medicaid state plan; and
- Medical assistance expenditures and prior period adjustments made under section 1115 demonstration authority with dates of service during the demonstration approval period; including those made in conjunction with the demonstration, net of enrollment fees, cost sharing, pharmacy rebates, and all other types of third-party liability.
- Sources of Non-Federal Share. As a condition of demonstration approval, the state certifies that the non-federal share is obtained from permissible state and/or local funds that, unless permitted by law, are not other federal funds. The state further certifies that such funds must not be used to match any other federal grant or contract, except as permitted by law. CMS approval of this demonstration does not constitute direct or indirect approval of any underlying source of non-federal share or associated funding mechanisms and all sources of non-federal funding must be compliant with section 1903(w) of the Act and applicable regulations. In addition, CMS reserves the right to prohibit the use of any sources of non-federal share funding that it determines impermissible.
- If requested, the state must submit for CMS review and approval documentation of any sources of non-federal share that would be used to fund the demonstration.
- If CMS determines that any funding sources are not consistent with applicable federal regulations, the state must address CMS's concerns within the time frames allotted by CMS.
- Without limitation, CMS may request information about the non-federal share sources for any amendments that CMS determines may financially impact the demonstration.
- State Certification of Funding Conditions. As a condition of demonstration approval, the state certifies that the following conditions for non-federal share funding of demonstration expenditures have been met:
- Units of state or local government, including health care providers that are units of state or local government, certify that state or local monies have been expended as the non-federal share of funds under the demonstration.
- To the extent the state utilizes certified public expenditures (CPE) as the funding mechanism for the state share of title XIX payments, including expenditures authorized under a section 1115 demonstration, the state must obtain CMS approval for a cost reimbursement methodology. This methodology must include a detailed explanation of the process, including any necessary cost reporting protocols, by which the state would identify those costs eligible under title XIX (or under section 1115 authority) for purposes of certifying public expenditures.
- To the extent the state utilizes CPEs as the funding mechanism to claim federal match for expenditures under the demonstration, governmental entities to which general revenue funds are appropriated must certify to the state the amount of such state or local monies that are allowable under 42 CFR 433.51 to satisfy demonstration expenditures. If the CPE is claimed under a Medicaid authority, the federal matching funds received cannot be used as the non-federal share needed to receive other federal matching funds under 42 CFR 433.51(c). The entities that incurred the cost must also provide cost documentation to support the state's claim for federal match.
- The state may use intergovernmental transfers (IGT) to the extent that such funds are derived from state or local revenues and are transferred by units of government within the state. Any transfers from units of government must be made in an amount not to exceed the non-federal share of title XIX payments.
- Under all circumstances, health care providers must retain 100 percent of the reimbursement for claimed expenditures. Moreover, consistent with 42 CFR 447.10, no pre-arranged agreements (contractual, voluntary, or otherwise) may exist between health care providers and state and/or local governments to return and/or redirect to the state any portion of the Medicaid payments. This confirmation of Medicaid payment retention is made with the understanding that payments that are the normal operating expenses of conducting business, such as payments related to taxes, including health care provider- related taxes, fees, business relationships with governments that are unrelated to Medicaid and in which there is no connection to Medicaid payments, are not considered returning and/or redirecting a Medicaid payment.
- Financial Integrity for Managed Care and Other Delivery Systems. As a condition of demonstration approval, the state attests to the following, as applicable:
- All risk-based managed care organization, prepaid inpatient health plan (PIHP), and prepaid ambulatory health plan (PAHP) payments, comply with the requirements on payments in 42 CFR §438.6(b)(2), 438.6(c), 438.6(d), 438.60 and/or 438.74.
- For non-risk-based PIHPs and PAHPs, arrangements comply with the upper payment limits specified in 42 CFR §447.362, and if payments exceed the cost of services, the state will recoup the excess and return the federal share of the excess to CMS.
- Requirements for health care related taxes and provider donations. As a condition of demonstration approval, the state attests to the following, as applicable:
- All health care-related taxes as defined by Section 1903 (w)(3)(A) of the Social Security Act and 42 CFR § 433.55 are broad-based as defined by Section 1903 (w)(3)(B) of the Social Security Act and 42 CFR § 433.68 (c).
- All health care-related taxes are uniform as defined by Section 1903 (w)(3)(C) of the Social Security Act and 42 CFR § 433.68 (d).
- If the health care-related tax is either not broad-based or not uniform, the state has applied for and received a waiver of the broad-based and/or uniformity requirements as specified by 1903 (w)(3)(E)(i) of the Social Security Act and 42 CFR § 433.72.
- The tax does not contain a hold harmless arrangement as described by Section 1903 (w)(4) of the Social Security Act and 42 CFR § 433.68 (f).
- All provider related-donations as defined by 42 CFR § 433.52 are bona fide as defined by Section 1903 (w)(2)(B) of the Social Security Act, 42 CFR § 433.66, and 42 CFR § 433.54.
- Program Integrity. The state must have processes in place to ensure there is no duplication of federal funding for any aspect of the demonstration. The state must also ensure that the state and any of its contractors follow standard program integrity principles and practices including retention of data. All data, financial reporting, and sources of non-federal share are subject to audit.
- Medicaid Expenditure Groups (MEG). MEGs are defined for the purpose of identifying categories of Medicaid or demonstration expenditures subject to budget neutrality, components of budget neutrality expenditure limit calculations, and other purposes related to monitoring and tracking expenditures under the demonstration. The Master MEG Chart table provides a master list of MEGs defined for this demonstration.
Table 2: Master MEG Chart
MEG To Which BN Test Does This Apply? Without waiver (WOW) Per Capita WOW Aggregate WW Brief Description TANF Child Main X X Demonstration Population 1 (see Table 1) TANF Adult Main X X Demonstration Population 2 (see Table 1) SSI 0 through 64 Main X X Demonstration Population 3 (see Table 1) SSI 65 and above Main X X Demonstration Population 4 (see Table 1) Non-Duals 18-64 Main X X Demonstration Population 5 (see Table 1) Non-Duals 65+ Main X X Demonstration Population 6 (see Table 1) MLTC Adults 18 - 64 Duals Main X X Demonstration Population 7 (see Table 1) MLTC Age 65+ Duals Main X X Demonstration Population 8 (see Table 1) HCBS Expansion Main X Demonstration Population 9: Individuals who are not otherwise eligible, are receiving HCBS, and who are determined to be medically needy based on New York's medically needy income level, after application of community spouse and spousal impoverishment eligibility and post- eligibility rules consistent with section 1924 of the Act. Institution to Community Main X Demonstration Population 10: ndividuals moved from institutional nursing facility settings to community settings for long term services and supports who would not otherwise be eligible based on income, but whose income does not exceed the income standard described in STC 4(c) of section IV, and who receive services through the managed long-term care program under the demonstration BH HCBS Main X Demonstration Services 8: Expenditures made for BH HCBS for individuals enrolled in HARPs and HIV SNPs. Note: Expenditures under this EG will be claimed in the manner necessary to ensure the correct claiming of FMAP for all populations. (e.g., BH HCBS for the adult expansion groups will be claimed at the FMAP rate at STC 7 section IX) Demonstrat ion Only Services in MMMC Main X X Demonstration Services 9: Expenditures made for provision of residential addiction services, crisis intervention and licensed behavioral health practitioner services to MMMC enrollees only and are not provided under the state plan. New Adult Group Hypo1 X X Demonstration Population 11
- CMS 64.9 VIII Waiv - New Adult Group Newly Eligible
- CMS 64.9VIII Waiv - New Adult Group Not Newly Childless Adults
- CMS 64.9VIII Waiv - New Adult Group Not Newly Children 19-20
- CMS 64.9VIII Waiv - New Adult Group Not Newly Parents & Caretakers
Fo1 Children Hypo2 X X Demonstration Population 12 ADM None Demonstration related administrative costs, as discussed in STC VIII.10.d
- Reporting Expenditures and Member Months. The state must report all demonstration expenditures claimed under the authority of title XIX of the Act and subject to budget neutrality each quarter on separate forms CMS-64.9 WAIVER and/or 64.9P WAIVER, identified by the demonstration project number assigned by CMS (11-W-00114/2). Separate reports must be submitted by MEG (identified by Waiver Name) and Demonstration Year (identified by the two-digit project number extension). Unless specified otherwise, expenditures must be reported by DY according to the dates of service associated with the expenditure. All MEGs identified in the Master MEG Chart as WW must be reported for expenditures, as further detailed in the MEG Detail for Expenditure and Member Month Reporting table below. To enable calculation of the budget neutrality expenditure limits, the state also must report member months of eligibility for specified MEGs.
- Cost Settlements. The state will report any cost settlements attributable to the demonstration on the appropriate prior period adjustment schedules (form CMS-64.9P WAIVER) for the summary sheet line 10b, in lieu of lines 9 or 10c. For any cost settlement not attributable to this demonstration, the adjustments should be reported as otherwise instructed in the State Medicaid Manual. Cost settlements must be reported by DY consistent with how the original expenditures were reported.
- Allocation of cost settlements. The state will calculate the percentage of Medicaid expenditures for each demonstration eligibility group to expenditures for all Medicaid population groups from a DataMart file produced for the latest completed federal fiscal year. Quarterly recoveries will be allocated to the eligibility groups based on those percentages. These percentages will be updated annually to reflect the most recent completed federal fiscal year.
- Premiums and Cost Sharing Collected by the State. The state will report any premium contributions collected by the state from demonstration enrollees quarterly on the form CMS-64 Summary Sheet line 9D, columns A and B. In order to assure that these collections are properly credited to the demonstration, quarterly premium collections (both total computable and federal share) should also be reported separately by DY on form CMS-64 Narrative, and on the Total Adjustments tab in the Budget Neutrality Monitoring Tool. In the annual calculation of expenditures subject to the budget neutrality expenditure limit, premiums collected in the demonstration year will be offset against expenditures incurred in the demonstration year for determination of the state's compliance with the budget neutrality limits.
- Pharmacy Rebates. Because pharmacy rebates are included in the base expenditures used to determine the budget neutrality expenditure limit, the state must report the portion of pharmacy rebates applicable to the demonstration on the appropriate forms CMS-64.9 WAIVER and 64.9P waiver for the demonstration, and not on any other CMS-64.9 form (to avoid double counting). The state must have a methodology for assigning a portion of pharmacy rebates to the demonstration in a way that reasonably reflects the actual rebate- eligible pharmacy utilization of the demonstration population, and which identifies pharmacy rebate amounts with DYs. Use of the methodology is subject to the approval in advance by the CMS Regional Office, and changes to the methodology must also be approved in advance by the Regional Office. Each rebate amount must be distributed as state and federal revenue consistent with the federal matching rates under which the claim was paid.
- Allocation of pharmacy rebates. The state will calculate the percentage of pharmacy expenditures for each demonstration eligibility group to pharmacy expenditures for all population groups from a DataMart file produced for the latest completed federal fiscal year. Rebates will be allocated to the eligibility groups based on those percentages. These percentages will be updated annually to reflect the most recent completed federal fiscal year.
- Administrative Costs. The state will separately track and report additional administrative costs that are directly attributable to the demonstration. All administrative costs must be identified on the forms CMS-64.10 WAIVER and/or 64.10P WAIVER. Unless indicated otherwise on the Master MEG Chart table, administrative costs are not counted in the budget neutrality tests; however, these costs are subject to monitoring by CMS.
- Member Months. As part of the Quarterly and Annual Monitoring Reports described in section7.8, the state must report the actual number of "eligible member months" for all demonstration enrollees for all MEGs identified as WOW Per Capita in the Master MEG Chart table above, and as also indicated in the MEG Detail for Expenditure and Member Month Reporting table below. The term "eligible member months" refers to the number of months in which persons enrolled in the demonstration are eligible to receive services. For example, a person who is eligible for three months contributes three eligible member months to the total. Two individuals who are eligible for two months, each contribute two eligible member months, for a total of four eligible member months. The state must submit a statement accompanying the annual report certifying the accuracy of this information.
- Budget Neutrality Specifications Manual. The state will create and maintain a Budget Neutrality Specifications Manual that describes in detail how the state will compile data on actual expenditures related to budget neutrality, including methods used to extract and compile data from the state's Medicaid Management Information System, eligibility system, and accounting systems for reporting on the CMS-64, consistent with the terms of the demonstration. The Budget Neutrality Specifications Manual will also describe how the state compiles counts of Medicaid member months. The Budget Neutrality Specifications Manual must be made available to CMS on request.
Table 3: MEG Detail for Expenditure and Member Month Reporting
MEG (Waiver Name) Detailed Description Exclusions CMS-64.9 Line(s) To Use How Expend. Are Assigned to DY MAP or ADM Report Member Months
(Y/N)MEG
Start DateMEG
End DateTANF Child Expenditures for medical assistance MMMC benefits for TANF Child Exclude individuals described in Table 2.
Exclude BH HCBS and Demonstration Only Services in MMMC.Follow CMS-64.9 Base Category of Service Definitions Date of service MAP Y 10/01/97 03/31/27 TANF Adult Expenditures for medical assistance MMMC benefits for TANF Adult Exclude individuals described in Table 2.
Exclude BH HCBS and Demonstration Only Services in MMMC.Follow CMS-64.9 Base Category of Service Definitions Date of service MAP Y 10/01/97 03/31/27 SSI 0 through 64 Expenditures for medical assistance MMMC benefits for SSI
0 through-64Exclude individuals described in Table 2.
Exclude BH HCBS and Demonstration Only Services in MMMC.Follow CMS-64.9 Base Category of Service Definitions Date of service MAP Y 10/01/97 03/31/27 SSI 65 and above Expenditures for medical assistance MMMC benefits for SSI
65 and aboveExclude individuals described in Table 2.
Exclude BH HCBS and Demonstration Only Services in MMMC.>Follow CMS-64.9 Base Category of Service Definitions Date of service MAP Y 10/01/97 03/31/27 Non-Duals 18-64 Expenditures for medical assistance MLTC benefits for Non-Duals
18-64Exclude individuals described in Table 4. Follow CMS-64.9 Base Category of Service Definitions Date of service MAP Y 08/31/12 03/31/27 Non-Duals 65+ Expenditures for medical assistance MLTC benefits for Non-Duals
65+Exclude individuals described in Table 4. Follow CMS-64.9 Base Category of Service Definitions Date of service MAP Y 08/31/12 03/31/27 MLTC Adults 18-64 Duals Expenditures for medical assistance MLTC benefits for MLTC
Adults 18-64 DualsExclude individuals described in Table 4. Follow CMS-64.9 Base Category of Service Definitions Date of service MAP Y 08/31/12 03/31/27 MLTC Age
65+ DualsExpenditures for medical assistance MLTC benefits for MLTC Age
65+ DualsExclude individuals described in Table 4. Follow CMS-64.9 Base Category of Service Definitions Date of service MAP Y 08/31/12 03/31/27 HCBS Expansion Home and community- based services expenditures for Demonstration Population
9None Line 19A Date of service MAP N 04/08/10 03/31/27 Institution to Community All medical assistance expenditures for Institution to Community None Follow CMS-64.9 Base Category of Service Definitions Date of service MAP N 08/31/12 03/31/27 BH HCBS All medical assistance expenditures for BH HCBS None Line 19A Date of service MAP N 07/29/15 03/31/25 Demonstration Only Services in MMMC All medical assistance expenditures and Demonstration Only Services in MMMC None Follow CMS-64.9 Base Category of Service Definitions Date of service MAP N 07/29/15 03/31/27 New Adult Group Expenditures for medical assistance for New Adult Group None Follow CMS-64.9 Base Category of Service Definitions Date of service MAP Y 01/01/14 03/31/27 Fo1 Children All medical assistance expenditures for Fo1 Children None Follow CMS-64.9 Base Category of Service Definitions Date of service MAP Y 04/01/19 03/31/27 ADM Demonstration related administrative costs, as discussed in STC VIII.10.d None Follow CMS-64.10 Base Category of Service Definitions Date of payment ADM N 10/01/97 03/31/27
- Demonstration Years. Demonstration Years (DY) for this demonstration are defined in the Demonstration Years table below.
Table 4: Demonstration Years
Demonstration Year 24 April 1, 2022 to March 31, 2023 12 months Demonstration Year 25 April 1, 2023 to March 31, 2024 12 months Demonstration Year 26 April 1, 2024 to March 31, 2025 12 months Demonstration Year 27 April 1, 2025 to March 31, 2026 12 months Demonstration Year 28 April 1, 2026 to March 31, 2027 12 months
- Budget Neutrality Monitoring Tool. The state must provide CMS with quarterly budget neutrality status updates, including established baseline and member months data, using the Budget Neutrality Monitoring Tool provided through the Performance Metrics Database and Analytics (PMDA) system. The tool incorporates the "Schedule C Report" for comparing demonstration's actual expenditures to the budget neutrality expenditure limits described in section XI. CMS will provide technical assistance, upon request.5
- Claiming Period. The state will report all claims for expenditures subject to the budget neutrality agreement (including any cost settlements) within two years after the calendar quarter in which the state made the expenditures. All claims for services during the demonstration period (including any cost settlements) must be made within two years after the conclusion or termination of the demonstration. During the latter two-year period, the state will continue to identify separately net expenditures related to dates of service during the operation of the demonstration on the CMS-64 waiver forms in order to properly account for these expenditures in determining budget neutrality.
- Future Adjustments to Budget Neutrality. CMS reserves the right to adjust the budget neutrality expenditure limit:
- To be consistent with enforcement of laws and policy statements, including regulations and letters, regarding impermissible provider payments, health care related taxes, or other payments, CMS reserves the right to make adjustments to the budget neutrality limit if any health care related tax that was in effect during the base year, or provider-related donation that occurred during the base year, is determined by CMS to be in violation of the provider donation and health care related tax provisions of section 1903(w) of the Act. Adjustments to annual budget targets will reflect the phase out of impermissible provider payments by law or regulation, where applicable.
- To the extent that a change in federal law, regulation, or policy requires either a reduction or an increase in FFP for expenditures made under this demonstration. In this circumstance, the state must adopt, subject to CMS approval, a modified budget neutrality agreement as necessary to comply with such change. The modified agreement will be effective upon the implementation of the change. The trend rates for the budget neutrality agreement are not subject to change under this STC. The state agrees that if mandated changes in the federal law require state legislation, the changes shall take effect on the day such state legislation becomes effective, or on the last day such legislation was required to be in effect under the federal law.
- The state certifies that the data it provided to establish the budget neutrality expenditure limit are accurate based on the state's accounting of recorded historical expenditures or the next best available data, that the data are allowable in accordance with applicable federal, state, and local statutes, regulations, and policies, and that the data are correct to the best of the state's knowledge and belief. The data supplied by the state to set the budget neutrality expenditure limit are subject to review and audit, and if found to be inaccurate, will result in a modified budget neutrality expenditure limit.
IX. MONITORING BUDGET NEUTRALITY
- Limit on Title XIX Funding. The state will be subject to limits on the amount of federal Medicaid funding the state may receive over the course of the demonstration approval. The budget neutrality expenditure limits are based on projections of the amount of FFP that the state would likely have received in the absence of the demonstration. The limit may consist of a Main Budget Neutrality Test, and one or more Hypothetical Budget Neutrality Tests, as described below. CMS's assessment of the state's compliance with these tests will be based on the Schedule C CMS-64 Waiver Expenditure Report, which summarizes the expenditures reported by the state on the CMS-64 that pertain to the demonstration.
- Risk. The budget neutrality expenditure limits are determined on either a per capita or aggregate basis. If a per capita method is used, the state is at risk for the per capita cost of state plan and hypothetical populations, but not for the number of participants in the demonstration population. By providing FFP without regard to enrollment in the demonstration for all demonstration populations, CMS will not place the state at risk for changing economic conditions; however, by placing the state at risk for the per capita costs of the demonstration populations, CMS assures that the demonstration expenditures do not exceed the levels that would have been realized had there been no demonstration. If an aggregate method is used, the state accepts risk for both enrollment and per capita costs.
- Calculation of the Budget Neutrality Limits and How They Are Applied. To calculate the budget neutrality limits for the demonstration, separate annual budget limits are determined for each DY on a total computable basis. Each annual budget limit is the sum of one or more components: per capita components, which are calculated as a projected without-waiver PMPM cost times the corresponding actual number of member months, and aggregate components, which project fixed total computable dollar expenditure amounts. The annual limits for all DYs are then added together to obtain a budget neutrality limit for the entire demonstration period. The federal share of this limit will represent the maximum amount of FFP that the state may receive during the demonstration period for the types of demonstration expenditures described below. The federal share will be calculated by multiplying the total computable budget neutrality expenditure limit by the appropriate Composite Federal Share.
- Main Budget Neutrality Test. The Main Budget Neutrality Test allows the state to show that demonstration waivers granted have not resulted in increased costs to Medicaid, and that federal Medicaid "savings" have been achieved sufficient to offset the additional projected federal costs resulting from expenditure authority. The table below identifies the MEGs that are used for the Main Budget Neutrality Test. MEGs designated as "WOW Only" or "Both" are components used to calculate the budget neutrality expenditure limit. MEGs that are indicated as "WW Only" or "Both" are counted as expenditures against the budget neutrality expenditure limit. In addition, any expenditures in excess of limit from Hypothetical Budget Neutrality Tests count as expenditures under the Main Budget Neutrality Test. The Composite Federal Share for this test is calculated based on all MEGs indicated as "Both."
Table 5: Main Budget Neutrality Test
MEG PC or Agg* WOW
Only, WW Only, or BothBASE YEAR
SFY 2020TREND DY 24 DY 25 DY 26 DY 27 DY 28 TANF Child PC Both $274.63 2.8% $298.92 $306.70 $315.29 $324.12 $333.20 TANF Adult PC Both $724.05 5.3% $845.39 $890.20 $937.38 $987.06 $1,039.37 SSI
0 through-64PC Both $2,126.11 4.3% $2,412.34 $2,56.07 $2,624.26 $2,737.10 $2,865.80 SSI
65 and abovePC Both $1,973.08 3.9% $2,213.05 $2,299.36 $2,389.04 $2,482.21 $2,579.02 Non-Duals
18-64PC Both $6,763.46 4.3% $7,674.00 $8,003.98 $8,348.15 $8,707.12 $9,081.53 Non-Duals
65+PC Both $6,574.94 3.9% $7,374.60 $7,662.21 $7,961.04 $8,271.52 $8,594.11 MLTC Adults
18-64 DualsPC Both $3,643.74 4.3% $4,134.27 $4,312.04 $4,497.46 $4,690.85 $4,892.56 MLTC Age
65+ DualsPC Both $5,073.30 3.9% $5,690.32 $5,912.24 $6,142.82 $6,382.39 $6,631.30 HCBS Expansion Agg WW only N/A N/A N/A N/A N/A N/A N/A Institution to
CommunityAgg WW only N/A N/A N/A N/A N/A N/A N/A BH HCBS Agg WW only N/A N/A N/A N/A N/A N/A N/A Demonstration Only Services in MMMC Agg WW only N/A N/A N/A N/A N/A N/A N/A *PC = Per Capita, Agg = Aggregate
- Hypothetical Budget Neutrality. When expenditure authority is provided for coverage of populations or services that the state could have otherwise provided through its Medicaid state plan or other title XIX authority (such as a waiver under section 1915 of the Act), CMS considers these expenditures to be "hypothetical"; that is, the expenditures would have been eligible to receive FFP elsewhere in the Medicaid program. For these hypothetical expenditures, CMS makes adjustments to the budget neutrality test which effectively treats these expenditures as if they were for approved Medicaid state plan services. Hypothetical expenditures, therefore, do not necessitate savings to offset the otherwise allowable services. This approach reflects CMS's current view that states should not have to "pay for," with demonstration savings, costs that could have been otherwise eligible for FFP under a Medicaid state plan or other title XIX authority; however, when evaluating budget neutrality, CMS does not offset non-hypothetical expenditures with projected or accrued savings from hypothetical expenditures. That is, savings are not generated from a hypothetical population or service. To allow for hypothetical expenditures, while preventing them from resulting in savings, CMS currently applies a separate, independent Hypothetical Budget Neutrality Tests, which subject hypothetical expenditures to pre-determined limits to which the state and CMS agree, and that CMS approves, as a part of this demonstration approval. If the state's WW hypothetical spending exceeds the supplemental test's expenditure limit, the state agrees (as a condition of CMS approval) to offset that excess spending by savings elsewhere in the demonstration or to refund the FFP to CMS.
- Hypothetical Budget Neutrality Test 1: New Adult Group. The table below identifies the MEGs that are used for Hypothetical Budget Neutrality Test 1. MEGs that are designated "WOW Only" or "Both" are the components used to calculate the budget neutrality expenditure limit. The Composite Federal Share for the Hypothetical Budget Neutrality Test is calculated based on all MEGs indicated as "WW Only" or "Both." MEGs that are indicated as "WW Only" or "Both" are counted as expenditures against this budget neutrality expenditure limit. Any expenditures in excess of the limit from Hypothetical Budget Neutrality Test are counted as WW expenditures under the Main Budget Neutrality Test.
MEG PC or Agg* WOW
Only, WW
Only, or BothBASE YEAR SFY 2020 TREND DY 24 DY 25 DY 26 DY 27 DY 28 New Adult Group PC Both $624.56 5.8% $739.66 $782.56 $827.95 $875.97 $926.78 - Hypothetical Budget Neutrality Test 2 Fo1 Children. The table below identifies the MEGs that are used for Hypothetical Budget Neutrality Test 2. MEGs that are designated "WOW Only" or "Both" are the components used to calculate the budget neutrality expenditure limit. The Composite Federal Share for the Hypothetical Budget Neutrality Test is calculated based on all MEGs indicated as "WW Only" or "Both." MEGs that are indicated as "WW Only" or "Both" are counted as expenditures against this budget neutrality expenditure limit. Any expenditures in excess of the limit from Hypothetical Budget Neutrality Test are counted as WW expenditures under the Main Budget Neutrality Test.
MEG PC or Agg* WOW Only, WW Only, or Both BASE YEAR SFY 2020 TREND DY 24 DY 25 DY 26 DY 27 DY 28 Fo1 Children PC Both $4,764.24 0% $4,764.24 $4,764.24 $4,764.24 $4,764.24 $4,764.24 - Calculating the Federal Medical Assistance Percentage (FMAP) for Continuous Eligibility for the Adult Group. CMS anticipates that states that adopt continuous eligibility for adults would experience a 2 percent increase in enrollment. Based on this estimate, CMS has determined that 97.4 percent of the member months for newly eligible members in the Adult Group will be made at the enhanced FMAP rate and 2.6 percent will be matched at the regular FMAP rate.
- State Reporting for the FMAP Adjustment. Newly eligible individuals in the Adult Group shall be claimed at the enhanced FMAP rate. The state must make an adjustment in the CMS-64W that accounts for the proportion of member months in which beneficiaries are enrolled due to continuous eligibility and could have been disenrolled due to excess income in absence of continuous eligibility (i.e. 2.6 percent). For the purposes of budget neutrality, the members of the adult group within the 2.6 percent of the population described in this STC will be treated as a hypothetical population. The state is not subject to use its budget neutrality savings towards providing continuous eligibility for this population.
- Composite Federal Share. The Composite Federal Share is the ratio that will be used to convert the total computable budget neutrality limit to federal share. The Composite Federal Share is the ratio calculated by dividing the sum total of FFP received by the state on actual demonstration expenditures during the approval period by total computable demonstration expenditures for the same period, as reported through MBES/CBES and summarized on Schedule C. Since the actual final Composite Federal Share will not be known until the end of the demonstration's approval period, for the purpose of interim monitoring of budget neutrality, a reasonable estimate of Composite Federal Share may be developed and used through the same process or through an alternative mutually agreed to method. Each Main or Hypothetical Budget Neutrality Test has its own Composite Federal Share, as defined in the paragraph pertaining to each particular test.
- Exceeding Budget Neutrality. CMS will enforce the budget neutrality agreement over the life of the demonstration approval period, which extends from April 1, 2022, to March 31, 2027. The Main Budget Neutrality Test may incorporate net savings from the immediately prior demonstration period of April 1, 2016, through March 31, 2021 (but not from any earlier approval period). If at the end of the demonstration approval period the budget neutrality limit has been exceeded, the excess federal funds will be returned to CMS. If the demonstration is terminated prior to the end of the demonstration period, the budget neutrality test will be based on the time period through the termination date.
- Mid-Course Correction. If at any time during the demonstration approval period CMS determines that the demonstration is on course to exceed its budget neutrality expenditure limit, CMS will require the state to submit a corrective action plan for CMS review and approval. CMS will use the threshold levels in the tables below as a guide for determining when corrective action is required.
Table 9: Main Budget Neutrality Test Mid-Course Correction Calculations
Cumulative Target Definition Percentage DY 24 through DY 25 Cumulative budget neutrality limit plus: 2.0 percent DY 24 through DY 26 Cumulative budget neutrality limit plus: 1.50 percent DY 24 through DY 27 Cumulative budget neutrality limit plus: 1.0 percent DY 24 through DY 28 Cumulative budget neutrality limit plus: 0.5 percent DY 24 through DY 29 Cumulative budget neutrality limit plus: 0.0 percent X. EVALUATION OF THE DEMONSTRATION
- Independent Evaluator. Upon approval of the demonstration, the state must arrange with an independent party to conduct an evaluation of the demonstration to ensure that the necessary data is collected at the level of detail needed to research the approved hypotheses. The independent party must sign an agreement to conduct the demonstration evaluation in an independent manner in accord with the CMS-approved Evaluation Design. When conducting analyses and developing the evaluation reports, every effort should be made to follow the approved methodology. However, the state may request, and CMS may agree to, changes in the methodology in appropriate circumstances.
- Evaluation Budget. A budget for the evaluation shall be provided with the draft Evaluation Design. It will include the total estimated cost, as well as a breakdown of estimated staff, administrative and other costs for all aspects of the evaluation, such as any survey and measurement development, quantitative and qualitative data collection and cleaning, analyses, and report generation. A justification of the costs may be required by CMS if the estimates provided do not appear to sufficiently cover the costs of the design or if CMS finds that the design is not sufficiently developed, or if the estimates appear to be excessive.
- Draft Evaluation Design. The state must submit, for CMS comment and approval, a draft Evaluation Design no later than one hundred eighty (180) days after the approval date of the demonstration. Any modifications to an existing approved Evaluation Design will not affect previously established requirements and timelines for report submission for the demonstration, if applicable. The draft Evaluation Design must be developed in accordance with the following CMS guidance (including but not limited to): (1) Attachment G (Developing the Evaluation Design) of these STCs, and all applicable technical assistance on applying robust evaluation approaches, including using comparison groups and beneficiary surveys to develop a draft Evaluation Design; and (2) all applicable evaluation design guidance.
- Evaluation Design Approval and Updates. The state must submit a revised draft Evaluation Design within sixty (60) calendar days after receipt of CMS's comments. Upon CMS approval of the draft Evaluation Design, the document will be included as Attachment I of these STCs. Per 42 CFR 431.424(c), the state will publish the approved Evaluation Design to the state's website within thirty (30) days of CMS approval. The state must implement the Evaluation Design and submit a description of its evaluation implementation progress in each of the Monitoring Reports. Hypotheses must cover all policies and goals of the demonstration and should be crafted to not only evaluate whether overall demonstration goals were achieved but also the extent to which each component contributed to outcomes. Where demonstration components offer tailored service to specific populations, evaluation hypotheses must include an assessment of whether these programs improved quality of care outcomes and access to health care for the targeted population while also promoting the desired administrative and fiscal efficiencies. Once CMS approves the Evaluation Design, if the state wishes to make changes, the state must submit a revised Evaluation Design to CMS for approval if the changes are substantial in scope; otherwise, in consultation with CMS, the state may include updates to the Evaluation Design in Monitoring Reports.
- Interim Evaluation Reports. The state must submit Interim Evaluation Reports covering the completed years of the demonstration, and for each subsequent extension of the demonstration, as outlined in 42 CFR 431.412(c)(2)(vi). When submitting an application for extension, the Interim Evaluation Report should be posted to the state's website with the application for public comment.
- The interim evaluation reports will discuss evaluation progress and present findings to date as per the approved Evaluation Design.
- For demonstration authority that expires prior to the overall demonstration's expiration date, the Interim Evaluation Report must include an evaluation of the authority as approved by CMS.
- A Preliminary Interim Evaluation Report will be due March 2024 in advance of the submission of the Interim Evaluation Report, and will cover all programs through March 2023, inclusive of any unevaluated time period during the previous demonstration period.
- If the state is seeking to extend the demonstration, the draft Interim Evaluation Report is due when the application for extension is submitted. If the state made changes to the demonstration in its application for extension, the research questions and hypotheses, and how the design was adapted should be included. If the state is not requesting an extension for a demonstration, an Interim Evaluation report is due one (1) year prior to the end of the demonstration. For demonstration phase-outs prior to the expiration of the approval period, the draft Interim Evaluation Report is due to CMS on the date that will be specified in the notice of termination or suspension.
- The state must submit revised Interim Evaluation Reports sixty (60) calendar days after receiving CMS comments on the draft report. Once approved by CMS, the state must post the final report to the state's website.
- Summative Evaluation Report. The draft Summative Evaluation Report must be developed in accordance with Attachment H (Preparing the Interim and Summative Evaluation Reports) of these STCs. The state must submit a draft Summative Evaluation Report for the demonstration's approval period within eighteen (18) months of the end of the approval period represented by these STCs. The Summative Evaluation Report must include the information in the approved Evaluation Design.
- Unless otherwise agreed upon in writing by CMS, the state must submit a revised Summative Evaluation Report within sixty (60) calendar days of receiving comments from CMS on the draft.
- The final Summative Evaluation Report must be posted to the state's Medicaid website within thirty (30) calendar days of approval by CMS.
- Close-Out Report. Within 120 calendar days after the expiration of the demonstration, the state must submit a Draft Close-Out Report to CMS for comments
- The draft close-out report must comply with the most current guidance from CMS.
- The state will present to and participate in a discussion with CMS on the close-out report.
- The state must take into consideration CMS' comments for incorporation into the final close-out report.
- The final close-out report is due to CMS no later than thirty (30) calendar days after receipt of CMS' comments.
- A delay in submitting the draft or final version of the close-out report may subject the state to penalties described in STC 7 section VII.
- Corrective Action Plan Related to Evaluation. If evaluation findings indicate that demonstration features are not likely to assist in promoting the objectives of Medicaid, CMS reserves the right to require the District to submit a corrective action plan to CMS for approval. These discussions may also occur as part of a renewal process when associated with the District's Interim Evaluation Report. This may be an interim step to withdrawing waivers or expenditure authorities, as outlined in STC 10 section 3.
- State Presentations for CMS. CMS reserves the right to request that the state present and participate in a discussion with CMS on the Evaluation Design, the Interim Evaluation reports, and/or the Summative Evaluation Report. Presentations may be conducted remotely.
- Public Access. The state shall post the final documents (e.g., Monitoring Reports, Close Out Report, approved Evaluation Design, Interim Evaluation Reports, and Summative Evaluation Report) on the state's Medicaid website within thirty (30) calendar days of approval by CMS.
- Additional Publications and Presentations. For a period of twelve (12) months following CMS approval of the final reports, CMS will be notified prior to presentation of these reports or their findings, including in related publications (including, for example, journal articles), by the state, contractor, or any other third party directly connected to the demonstration. Prior to release of these reports, articles or other publications, CMS will be provided a copy including any associated press materials. CMS will be given ten (10) business days to review and comment on publications before they are released. CMS may choose to decline to comment or review some or all of these notifications and reviews. This requirement does not apply to the release or presentation of these materials to state or local government officials.
- Cooperation with Federal Evaluators. As required under 42 CFR 431.420(f), the state shall cooperate fully and timely with CMS and its contractors in any federal evaluation of the demonstration or any component of the demonstration. This includes, but is not limited to, commenting on design and other federal evaluation documents and providing data and analytic files to CMS, including entering into a data use agreement that explains how the data and data files will be exchanged, and providing a technical point of contact to support specification of the data and files to be disclosed, as well as relevant data dictionaries and record layouts. The state shall include in its contracts with entities who collect, produce or maintain data and files for the demonstration, that they shall make such data available for the federal evaluation as is required under 42 CFR 431.420(f) to support federal evaluation. The state may claim administrative match for these activities. Failure to comply with this STC may result in a deferral being issued as outlined in Section IV, STC 7.
XI. SCHEDULE OF DELIVERABLES FOR DEMONSTRATION
STC Section 1115 Deliverable Due Date Frequency VII Quarterly Monitoring Report Due to CMS 60 days after the end of each demonstration quarter Ongoing Quarterly Budget Neutrality Report VII Annual Report Due to CMS 90 days after the end of each demonstration year Ongoing X Evaluation Design Due to CMS 180 days after approval of the demonstration X Interim Evaluation Reports Preliminary Report due to CMS in March 2024; Interim Evaluation Report due to CMS 1 year prior to the end of the demonstration X Summative Evaluation Report Due to CMS 18 months after the end of the demonstration approval period X Close Out Report Due to CMS 120 calendar days after the expiration of the demonstration
ATTACHMENT A
Home and Community-Based Services Expansion Program Benefits
| Assistive Technology (including personal emergency response system) |
| Community Integration Counseling and Services |
| Community Transition Services |
| Congregate/Home Delivered Meals |
| Environmental Modifications |
| Home and Community Support Services |
| Home Maintenance |
| Home Visits by Medical Personnel |
| Independent Living Skills Training |
| Intensive Behavioral Programs |
| Medical Social Services |
| Moving Assistance |
| Nutritional Counseling/Education |
| Peer Mentoring |
| Positive Behavioral Interventions |
| Respiratory Therapy |
| Respite Care/Services |
| Service Coordination |
| Social Day Care (including transportation) |
| Structured Day Program |
| Substance Abuse Programs |
| Transportation |
| Wellness Counseling Services |
All HCBS Expansion program participants may not receive all benefits listed above. An individual participant's access to the benefits below may vary based on the individual's similarity to an individual determined eligible for and enrolled in the NHTD or TBI 1915(c) waiver program.
Home and community-based services (HCBS) must be provided in a setting that includes the following qualities:
- ☐ The setting is integrated in and supports full access of individuals receiving Medicaid HCBS to the greater community, including opportunities to seek employment and work in competitive integrated settings, engage in community life, control personal resources, and receive services in the community, to the same degree of access as individuals not receiving Medicaid HCBS.
- ☐ The setting is selected by the individual from among setting options including non- disability specific settings and an option for a private unit in a residential setting. The setting options are identified and documented in the person-centered service plan and are based on the individual's needs, preferences, and, for residential settings, resources available for room and board.
- ☐ Ensures an individual's rights of privacy, dignity and respect, and freedom from coercion and restraint.
- ☐ Optimizes, but does not regiment, individual initiative, autonomy, and independence in making life choices, including but not limited to, daily activities, physical environment, and with whom to interact.
- ☐ Facilitates individual choice regarding services and supports, and who provides them.
- ☐ In a provider-owned or controlled residential setting, in addition to the qualities specified above, the following additional conditions must be met:
- The unit or dwelling is a specific physical place that can be owned, rented, or occupied under a legally enforceable agreement by the individual receiving services, and the individual has, at a minimum, the same responsibilities and protections from eviction that tenants have under the landlord/tenant law of the State, county, city, or other designated entity. For settings in which landlord tenant laws do not apply, the State must ensure that a lease, residency agreement or other form of written agreement will be in place for each HCBS participant, and that the document provides protections that address eviction processes and appeals comparable to those provided under the jurisdiction's landlord tenant law.
- Each individual has privacy in their sleeping or living unit:
- ☐ Units have entrance doors lockable by the individual, with only appropriate staff having keys to doors.
- ☐ Individuals sharing units have a choice of roommates in that setting.
- ☐ Individuals have the freedom to furnish and decorate their sleeping or living units within the lease or other agreement.
- Individuals have the freedom and support to control their own schedules and activities and have access to food at any time.
- Individuals are able to have visitors of their choosing at any time.
- The setting is physically accessible to the individual.
- Any modification of the additional conditions specified in items 1 through 4 above, must be supported by a specific assessed need and justified in the person-centered service plan. The following requirements must be documented in the person-centered service plan:
- ☐ Identify a specific and individualized assessed need.
- ☐ Document the positive interventions and supports used prior to any modifications to the person-centered service plan.
- ☐ Document less intrusive methods of meeting the need that have been tried but did not work.
- ☐ Include a clear description of the condition that is directly proportionate to the specific assessed need.
- ☐ Include regular collection and review of data to measure the ongoing effectiveness of the modification.
- ☐ Include established time limits for periodic reviews to determine if the modification is still necessary or can be terminated.
- ☐ Include the informed consent of the individual.
- ☐ Include an assurance that interventions and supports will cause no harm to the individual.
Settings that are not Home and Community-Based:
For 1115 demonstrations that furnish HCBS services, settings that are not home and community-based are defined at §441.301(c)(5) as follows:
- ☐ A nursing facility;
- ☐ An institution for mental diseases;
- ☐ An intermediate care facility for individuals with intellectual disabilities; A hospital; or
- ☐ Any other locations that have qualities of an institutional setting, as determined by the Secretary.
ATTACHMENT B
Behavioral Health (BH) Home and Community Based Services (HCBS) and Community Oriented Recovery and Empowerment (CORE) Services in HARPS
| Behavioral Health HCBS BH HCBS Assessment |
|---|
BH HCBS Assessment
|
| Habilitation Services |
| Non-medical transportation |
|
|
*BH HCBS settings must adhere to the same HCBS setting qualities as listed in Attachment C.
Behavioral Health Community Oriented Recovery and Empowerment Services in HARPS and HIV SNPs
| Behavioral Health CORE |
|---|
|
|
|
|
ATTACHMENT C
Mandatory Managed Long-Term Care/Care Coordination Model (CCM)
Mandatory Population: Dual eligible, age 21 and over, receiving community based long term care services for over 120 days, excluding the following:
- Nursing Home Transition and Diversion waiver participants;
- Traumatic Brain Injury waiver participants;
- Assisted Living Program participants; and
- Dual eligible that do not require community based long term care services.
Voluntary Population: Dual eligible, age 18 through 20, in need of community based long term care services for over 120 days and assessed as nursing home eligible. Non-dual eligible age 18 and older assessed as nursing home eligible and in need of community based long term care services for over 120 days.
The following requires CMS approval to initiate and reflects the enrollment of the mandatory population only.
I. Phase I and II: New York City and the suburbs
July 1, 2012 - Any new dual eligible case new to service, fitting the mandatory definition in any New York City County will be identified for enrollment and referred to the Enrollment Broker for action.
- Enrollment Broker will provide with educational material, a list of plans/CCMs, and answer questions and provide assistance contacting a plan if requested.
- Plan/CCM will conduct assessment to determine if eligible for community based long term care.
- Plan/CCM transmits enrollment to Enrollment Broker.
In addition, the following identifies the enrollment plan for cases already receiving care. Enrollment will be phased in by service type by borough by zip code in batches. People will be given 60 days to choose a plan according to the following schedule.
July 1, 2012: Begin personal care cases in New York County
August 1, 2012: Continue personal care cases in New York County
September, 2012: Continue personal care cases in New York County and begin personal care in Bronx County; and begin consumer directed personal assistance program cases in New York and Bronx counties
October, 2012: Continue personal care and consumer directed personal assistance program cases in New York and Bronx counties and begin Kings County
November, 2012: Continue personal care and consumer directed personal assistance program cases in New York, Bronx and Kings Counties
December, 2012: Continue personal care and consumer directed personal assistance program cases in New York, Bronx and Kings Counties and begin Queens and Richmond counties
January, 2013: Continue personal care and consumer directed personal assistance program citywide.
February, 2013 (and until all people in service are enrolled): Personal care, consumer directed personal assistance program, citywide
March, 2013: Personal care, consumer directed personal assistance program, adult day health care, home health care over 120 days citywide
March, 2013: Personal care, consumer directed personal assistance program, adult day health care, home health care over 120 days in Nassau, Suffolk and Westchester counties
April, 2013: Personal care, consumer directed personal assistance program, adult day health care, home health care over 120 days and long-term home health care program citywide
April, 2013: Personal care, consumer directed personal assistance program, adult day health care, home health care over 120 days and long-term home health care program in Nassau, Suffolk and Westchester Counties
II. Phase III: Rockland and Orange Counties
June 2013: Dually eligible community based long term care service recipients in these additional counties as capacity
III. Phase IV: Albany, Erie, Onondaga and Monroe Counties
Fall 2013: Dually eligible community based long term care service recipients in these additional counties as capacity
IV. Phase V: Other Counties with capacity
Spring 2014: Dually eligible community based long term care service recipients in these additional counties as capacity
V. Phase VI:
Previously excluded dual eligible groups contingent upon development of appropriate program models:
- Nursing Home Transition and Diversion waiver participants;
- Traumatic Brain Injury waiver participants;
- Assisted Living Program participants; and
- Dual eligible that do not require community based long term care services.
ATTACHMENT D
List of Eligible Goods and Services Under BH HCBS Individual Directed Goods and Services
Non-treatment Goods and Services Eligible for Self-Direction
Non-Treatment Goods and Services may include the following:
- Wellness activities
- Gym/ health club membership
- Wellness coaching
- Smoking cessation tools/ education
- Dental care
- Eyeglasses/care
- Out of network health/BH/specialty services
- Family planning and sexual health education/ services
- Acupuncture/pressure
- Yoga classes/ meditation guidance
- Massage/ reiki/ shiatsu/ tai chi instruction
- Pet adoption funds, including appointments/resources related to pet health and maintenance
- Workout equipment and clothing
- Nutritional supplements and vitamins
- Occupational/ skills development
- Computer literacy
- Resume development
- Interview preparation
- PC/ communication technology
- Personal preparation/ resources to prepare for interviews or to enhance confidence during employment, including purchase of a wardrobe or maintenance of personal hygiene (including but not limited to skin and hair care)
- Resources for entrepreneurial development, including business cards, website development
- Course Fees and Educational course fees and materials
- Transportation
- Public transportation costs
- Car repair/ maintenance
- Bicycle and related costs
- In-home/ social/ community supports
- Training and supports for daily living including cooking and nutrition classes, sequencing, time management, etc.
- Housing start-up (down payments), non-recurring housing bills or costs related to home maintenance, including furniture or air conditioner
- Groceries
- Travel to and from family or social functions, including special trips to visit family members or friends
- Meetings in the community with friends or family members at restaurants, coffee houses, or other social venues, that promote the social inclusion of the participant
- Financial contributions at social activities including church services
- Registration fees for conferences, trainings, community activities
- Membership dues in groups, societies, guilds, leagues
ATTACHMENT E
Developing the Evaluation Design
Introduction
Both state and federal governments need rigorous quantitative and qualitative evidence to inform policy decisions. To that end, for states that are testing new approaches and flexibilities in their Medicaid programs through section 1115 demonstrations, evaluations are crucial to understand and disseminate information about these policies. The evaluations of new initiatives seek to produce new knowledge and direction for programs and inform Medicaid policy for the future. While a narrative about what happened during a demonstration provides important information, the principal focus of the evaluation of a section 1115 demonstration should be obtaining and analyzing data. Evaluations should include findings about the process (e.g., whether the demonstration is being implemented as intended), outcomes (e.g., whether the demonstration is having the intended effects on the target population), and impacts of the demonstration (e.g., whether the outcomes observed in the targeted population differ from outcomes in similar populations not affected by the demonstration).
Submission Timelines
There is a specified timeline for the state's submission of its draft Evaluation Design and subsequent evaluation reports. The graphic below depicts an example of this timeline for a 5-year demonstration. In addition, the state should be aware that section 1115 evaluation documents are public records. The state is required to publish the Evaluation Design to the state's website within thirty (30) calendar days of CMS approval, as per 42 CFR 431.424(e). CMS will also publish a copy to the Medicaid.gov website.
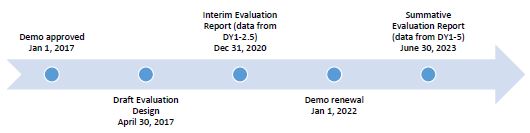
Expectations for Evaluation Designs
CMS expects Evaluation Designs to be rigorous, incorporate baseline and comparison group assessments, as well as statistical significance testing. Technical assistance resources for constructing comparison groups and identifying causal inferences are available on Medicaid.gov 1115 Demonstration State Monitoring & Evaluation Resources If the state needs technical assistance using this outline or developing the Evaluation Design, the state should contact its demonstration team.
All states with section 1115 demonstrations are required to conduct Interim and Summative Evaluation Reports, and the Evaluation Design is the roadmap for conducting these evaluations. The roadmap begins with the stated goals for the demonstration, followed by the measurable evaluation questions and quantifiable hypotheses, all to support a determination of the extent to which the demonstration has achieved its goals. When conducting analyses and developing the evaluation reports, every effort should be made to follow the approved methodology. However, the state may request, and CMS may agree to, changes in the methodology in appropriate circumstances.
The format for the Evaluation Design is as follows:
- General Background Information;
- Evaluation Questions and Hypotheses;
- Methodology;
- Methodological Limitations;
- Attachments.
- General Background Information - In this section, the state should include basic information about the demonstration, such as:
- The issue/s that the state is trying to address with its section 1115 demonstration and/or expenditure authorities, the potential magnitude of the issue/s, and why the state selected this course of action to address the issue/s (e.g., a narrative on why the state submitted an 1115 demonstration proposal).
- The name of the demonstration, approval date of the demonstration, and period of time covered by the evaluation.
- A description of the population groups impacted by the demonstration.
- A brief description of the demonstration and history of its implementation, and whether the draft Evaluation Design applies to an amendment, extension, renewal, or expansion of, the demonstration.
- For renewals, amendments, and major operational changes: a description of any changes to the demonstration during the approval period; the primary reason or reasons for the change; and how the Evaluation Design was altered or augmented to address these changes.
- Evaluation Questions and Hypotheses - In this section, the state should:
- Identify the state's hypotheses about the outcomes of the demonstration and discuss how the evaluation questions align with the hypotheses and the goals of the demonstration.
- Address how the hypotheses and research questions promote the objectives of Titles XIX and/or XXI.
- Describe how the state's demonstration goals are translated into quantifiable targets for improvement, so that the performance of the demonstration in achieving these targets can be measured.
- Include a Driver Diagram to visually aid readers in understanding the rationale behind the cause and effect of the variants behind the demonstration features and intended outcomes. A driver diagram, which includes information about the goals and features of the demonstration, is a particularly effective modeling tool when working to improve health and health care through specific interventions. A driver diagram depicts the relationship between the aim, the primary drivers that contribute directly to achieving the aim, and the secondary drivers that are necessary to achieve the primary drivers for the demonstration. For an example and more information on driver diagrams: https://innovation.cms.gov/files/x/hciatwoaimsdrvrs.pdf .
- Methodology - In this section, the state is to describe in detail the proposed research methodology. The focus is on showing that the evaluation meets the prevailing standards of scientific and academic rigor, that the results are statistically valid and reliable, and that it builds upon other published research, using references where appropriate.
This section also provides evidence that the demonstration evaluation will use the best available data. The state should report on, control for, and make appropriate adjustments for the limitations of the data and their effects on results, and discuss the generalizability of results. This section should provide enough transparency to explain what will be measured and how, in sufficient detail so that another party could replicate the results. Table A below is an example of how the state might want to articulate the analytic methods for each research question and measure. Specifically, this section establishes: - Methodological Design - Provide information on how the evaluation will be designed. For example, whether the evaluation will utilize pre/post data comparisons, pre-test or post-test only assessments. If qualitative analysis methods will be used, they must be described in detail.
- Target and Comparison Populations - Describe the characteristics of the target and comparison populations, incorporating the inclusion and exclusion criteria. Include information about the level of analysis (beneficiary, provider, or program level), and if populations will be stratified into subgroups. Additionally, discuss the sampling methodology for the populations, as well as support that a statistically reliable sample size is available.
- Evaluation Period - Describe the time periods for which data will be included.
- Evaluation Measures - List all measures that will be calculated to evaluate the demonstration. The state also should include information about how it will define the numerators and denominators. Furthermore, the state should ensure the measures contain assessments of both process and outcomes to evaluate the effects of the demonstration during the period of approval. When selecting metrics, the state shall identify opportunities for improving quality of care and health outcomes and controlling cost of care. The state also should incorporate benchmarking and comparisons to national and state standards, where appropriate. The state also should include the measure stewards (i.e., the organization(s) responsible for the evaluation data elements/sets by "owning", defining, validating, securing, and submitting for endorsement, etc.) Proposed health measures could include CMS's Core Set of Health Care Quality Measures for Children in Medicaid and CHIP, Consumer Assessment of Health Care Providers and Systems (CAHPS), the Initial Core Set of Health Care Quality Measures for Medicaid-Eligible Adults and/or measures endorsed by National Quality Forum. Proposed performance metrics can be selected from nationally recognized metrics, for example from sets developed by the Center for Medicare and Medicaid Innovation or for meaningful use under Health Information Technology.
- Data Sources - Explain from where the data will be obtained, describe any efforts to validate and clean the data, and discuss the quality and limitations of the data sources. If the state plans to collect primary data (i.e., data collected specifically for the evaluation), include the methods by which the data will be collected, the source of the proposed questions and responses, and the frequency and timing of data collection. Additionally, copies of any proposed surveys must be provided to CMS for approval before implementation.
- Analytic Methods - This section includes the details of the selected quantitative and/or qualitative analysis measures that will adequately assess the effectiveness of the demonstration. This section should:
- Identify the specific statistical testing which will be undertaken for each measure (e.g., t-tests, chi-square, odds ratio, ANOVA, regression).
- Explain how the state will isolate the effects of the demonstration from other initiatives occurring in the state at the same time (e.g., through the use of comparison groups).
- Include a discussion of how propensity score matching, and difference-in-differences designs may be used to adjust for differences in comparison populations over time, if applicable.
- Consider the application of sensitivity analyses, as appropriate.
- Other Additions - The state may provide any other information pertinent to the Evaluation Design for the demonstration.
- Measure 1
- Measure 2
- Measure 3
- Sample e.g. All attributed Medicaid beneficiaries
- Beneficiaries with diabetes diagnosis
- Medicaid fee-for-service and encounter claims records
- Interrupted time series
- Measure 1
- Measure 2
- Measure 3
- Measure 4
- Sample, e.g., PPS patients who meet survey selection requirements (used services within the last 6 months)
- Patient survey
- Measure 1
- Measure 2
- Sample, e.g., PPS administrators
- Key informants
- Methodological Limitations - This section provides more detailed information about the limitations of the evaluation. This could include limitations about the design, the data sources or collection process, or analytic methods. The state should also identify any efforts to minimize these limitations. Additionally, this section should include any information about features of the demonstration that effectively present methodological constraints that the state would like CMS to take into consideration in its review.
CMS also recognizes that there may be certain instances where a state cannot meet the rigor of an evaluation as expected by CMS. In these instances, the state should document for CMS why it is not able to incorporate key components of a rigorous evaluation, including comparison groups and baseline data analyses. For example, if a demonstration is long-standing, it may be difficult for the state to include baseline data because any pre-test data points may not be relevant or comparable. Other examples of considerations include:- When the demonstration is:
- Non-complex, unchanged, or has previously been rigorously evaluated and found to be successful; or
- Could now be considered standard Medicaid policy (CMS published regulations or guidance).
- When the demonstration is also considered successful without issues or concerns that would require more regular reporting, such as:
- Operating smoothly without administrative changes;
- No or minimal appeals and grievances;
- No state issues with CMS-64 reporting or budget neutrality; and
- No Corrective Action Plans for the demonstration.
- When the demonstration is:
| Research Question | Outcome measures used to address the research question | Sample or population subgroups to be compared | Data Sources | Analytic Methods |
|---|---|---|---|---|
| Hypothesis 1 | ||||
| Research question 1a | ||||
| Research question 1b | Descriptive statistics | |||
| Hypothesis 2 | ||||
| Research question 2a | Qualitative analysis of interview material | |||
- Independent Evaluator. This includes a discussion of the state's process for obtaining an independent entity to conduct the evaluation, including a description of the qualifications that the selected entity must possess, and how the state will assure no conflict of interest. Explain how the state will assure that the Independent Evaluator will conduct a fair and impartial evaluation and prepare objective Evaluation Reports. The Evaluation Design should include a "No Conflict of Interest" statement signed by the independent evaluator.
- Evaluation Budget. A budget for implementing the evaluation shall be provided with the draft Evaluation Design. It will include the total estimated costs, as well as a breakdown of estimated staff, administrative, and other costs for all aspects of the evaluation. Examples include but are not limited to: the development of all survey and measurement instruments; quantitative and qualitative data collection; data cleaning and analyses; and reports generation. A justification of the costs may be required by CMS if the estimates provided do not appear to sufficiently cover the costs of the draft Evaluation Design, if CMS finds that the draft Evaluation Design is not sufficiently developed, or if the estimates appear to be excessive.
- Timeline and Major Milestones. Describe the timeline for conducting the various evaluation activities, including dates for evaluation-related milestones, including those related to procurement of an outside contractor, if applicable, and deliverables. The final Evaluation Design shall incorporate milestones for the development and submission of the Interim and Summative Evaluation Reports. Pursuant to 42 CFR 431.424(c)(v), this timeline should also include the date by which the Final Summative Evaluation Report is due.
ATTACHMENT F
Preparing the Interim and Summative Evaluation Reports
Introduction
Both state and federal governments need rigorous quantitative and qualitative evidence to inform policy decisions. To that end, for states that are testing new approaches and flexibilities in their Medicaid programs through section 1115 demonstrations, evaluations are crucial to understand and disseminate information about these policies. The evaluations of new initiatives seek to produce new knowledge and direction for programs and inform Medicaid policy for the future. While a narrative about what happened during a demonstration provides important information, the principal focus of the evaluation of a section 1115 demonstration should be obtaining and analyzing data. Evaluations should include findings about the process (e.g., whether the demonstration is being implemented as intended), outcomes (e.g., whether the demonstration is having the intended effects on the target population), and impacts of the demonstration (e.g., whether the outcomes observed in the targeted population differ from outcomes in similar populations not affected by the demonstration).
Submission Timelines
There is a specified timeline for the state's submission of its draft Evaluation Design and subsequent evaluation reports. The graphic below depicts an example of this timeline for a 5-year demonstration. In addition, the state should be aware that section 1115 evaluation documents are public records. The state is required to publish the Evaluation Design to the state's website within thirty (30) calendar days of CMS approval, as per 42 CFR 431.424(e). CMS will also publish a copy to the Medicaid.gov website.
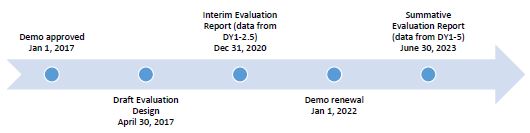
Expectations for Evaluation Designs
All states with section 1115 demonstrations are required to conduct Interim and Summative Evaluation Reports, and the Evaluation Design is the roadmap for conducting these evaluations. The roadmap begins with the stated goals for the demonstration, followed by the measurable evaluation questions and quantifiable hypotheses, all to support a determination of the extent to which the demonstration has achieved its goals. When conducting analyses and developing the evaluation reports, every effort should be made to follow the approved methodology. However, the state may request, and CMS may agree to, changes in the methodology in appropriate circumstances.
When submitting an application for renewal, the Interim Evaluation Report should be posted on the state's website with the application for public comment. Additionally, the Interim Evaluation Report must be included in its entirety with the application submitted to CMS.
CMS expects Interim and Summative Evaluation Reports to be rigorous, incorporate baseline and comparison group assessments, as well as statistical significance testing. Technical assistance resources for constructing comparison groups and identifying causal inferences are available on Medicaid.gov: 1115 Demonstration State Monitoring & Evaluation Resources. If the state needs technical assistance using this outline or developing the evaluation reports, the state should contact its demonstration team.
Intent of this Attachment
Title XIX of the Social Security Act (the Act) requires an evaluation of every section 1115 demonstration. In order to fulfill this requirement, the state's evaluation report submissions must provide comprehensive written presentations of all key components of the demonstration, and include all required elements specified in the approved Evaluation Design. This Attachment is intended to assist states with organizing the required information in a standardized format and understanding the criteria that CMS will use in reviewing the submitted Interim and Summative Evaluation Reports.
Required Core Components of Interim and Summative Evaluation Reports
The Interim and Summative Evaluation Reports present research and findings about the section 1115 demonstration. It is important that the reports incorporate a discussion about the structure of the Evaluation Design to explain the goals and objectives of the demonstration, the hypotheses related to the demonstration, and the methodology for the evaluation. The evaluation reports should present the relevant data and an interpretation of the findings; assess the outcomes (what worked and what did not work); explain the limitations of the design, data, and analyses; offer recommendations regarding what (in hindsight) the state would further advance, or do differently, and why; and discuss the implications on future Medicaid policy.
- Executive Summary;
- General Background Information;
- Evaluation Questions and Hypotheses;
- Methodology;
- Methodological Limitations;
- Results;
- Conclusions;
- Interpretations, and Policy Implications and Interactions with Other State Initiatives;
- Lessons Learned and Recommendations; and,
- Attachment(s).
- Executive Summary - A summary of the demonstration, the principal results, interpretations, and recommendations of the evaluation.
- General Background Information about the Demonstration - In this section, the state should include basic information about the demonstration, such as:
- The issue/s that the state is trying to address with its section 1115 demonstration and/or expenditure authorities, how the state became aware of the issue, the potential magnitude of the issue, and why the state selected this course of action to address the issues.
- The name of the demonstration, approval date of the demonstration, and period of time covered by the evaluation.
- A description of the population groups impacted by the demonstration.
- A brief description of the demonstration and history of the implementation, and if the evaluation is for an amendment, extension, renewal, or expansion of, the demonstration.
- For renewals, amendments, and major operational changes: A description of any changes to the demonstration during the approval period; whether the motivation for change was due to political, economic, and fiscal factors at the state and/or federal level; whether the programmatic changes were implemented to improve beneficiary health, provider/health plan performance, or administrative efficiency; and how the Evaluation Design was altered or augmented to address these changes. Additionally, the state should explain how this Evaluation Report builds upon and expands earlier demonstration evaluation findings (if applicable).
- Evaluation Questions and Hypotheses - In this section, the state should:
- Identify the state's hypotheses about the outcomes of the demonstration and discuss how the goals of the demonstration align with the evaluation questions and hypotheses.
- Address how the research questions / hypotheses of this demonstration promote the objectives of titles XIX and XXI.
- Describe how the state's demonstration goals were translated into quantifiable targets for improvement, so that the performance of the demonstration in achieving these targets could be measured.
- The inclusion of a Driver Diagram in the Evaluation Report is highly encouraged, as the visual can aid readers in understanding the rationale behind the demonstration features and intended outcomes.
- Methodology - In this section, the state is to provide an overview of the research that was conducted to evaluate the section 1115 demonstration, consistent with the approved Evaluation Design. The Evaluation Design should also be included as an attachment to the report. The focus is on showing that the evaluation builds upon other published research, (using references), meets the prevailing standards of scientific and academic rigor, and the results are statistically valid and reliable.
An Interim Evaluation Report should provide any available data to date, including both quantitative and qualitative assessments. The Evaluation Design should assure there is appropriate data development and collection in a timely manner to support developing an Interim Evaluation Report.
This section provides the evidence that the demonstration evaluation used the best available data and describes why potential alternative data sources were not used. The state also should report on, control for, and make appropriate adjustments for the limitations of the data and their effects on results, and discusses the generalizability of results. This section should provide enough transparency to explain what was measured and how, in sufficient detail so that another party could replicate the results. Specifically, this section establishes that the approved Evaluation Design was followed by describing:- Methodological Design - Whether the evaluation included an assessment of pre/post or post-only data, with or without comparison groups, etc.
- Target and Comparison Populations - Describe the target and comparison populations, describing inclusion and exclusion criteria.
- Evaluation Period - Describe the time periods for which data will be collected.
- Evaluation Measures - List the measures used to evaluate the demonstration and their respective measure stewards.
- Data Sources - Explain from where the data were obtained, and efforts to validate and clean the data.
- Analytic Methods - Identify specific statistical testing which was undertaken for each measure (t-tests, chi-square, odds ratio, ANOVA, regression, etc.).
- Other Additions - The state may provide any other information pertinent to the evaluation of the demonstration.
- Methodological Limitations - This section provides sufficient information for discerning the strengths and weaknesses of the study design, data sources/collection, and analyses.
- Results - In this section, the state presents and uses the quantitative and qualitative data to demonstrate whether and to what degree the evaluation questions and hypotheses of the demonstration were addressed. The findings should visually depict the demonstration results, using tables, charts, and graphs, where appropriate. This section should include findings from the statistical tests conducted.
- Conclusions - In this section, the state will present the conclusions about the evaluation results. Based on the findings, discuss the outcomes and impacts of the demonstration and identify the opportunities for improvements. Specifically, the state should answer the following questions:
- In general, did the results show that the demonstration was/was not effective in achieving the goals and objectives established at the beginning of the demonstration?
- If the state did not fully achieve its intended goals, why not?
- What could be done in the future that would better enable such an effort to more fully achieve those purposes, aims, objectives, and goals?
- Interpretations, Policy Implications and Interactions with Other State Initiatives - In this section, the state will discuss the section 1115 demonstration within an overall Medicaid context and long-range planning. This should include interrelations of the demonstration with other aspects of the state's Medicaid program, interactions with other Medicaid demonstrations, and other federal awards affecting service delivery, health outcomes and the cost of care under Medicaid. This section provides the state with an opportunity to provide interpretations of the data using evaluative reasoning to make judgments about the demonstration. This section should also include a discussion of the implications of the findings at both the state and national levels.
- Lessons Learned and Recommendations - This section of the evaluation report involves the transfer of knowledge. Specifically, it should include potential "opportunities" for future or revised demonstrations to inform Medicaid policymakers, advocates, and stakeholders. Recommendations for improvement can be just as significant as identifying current successful strategies. Based on the evaluation results, the state should address the following questions:
- What lessons were learned as a result of the demonstration?
- What would you recommend to other states which may be interested in implementing a similar approach?
ATTACHMENT G
Evaluation Design
[RESERVED]
_______________________________
1. Medically needy refers to those who have the option of spousal impoverishment budgeting, including post eligibility when it is more beneficial. Medically needy is defined as an individual who is not eligible for, or in receipt of public assistance or SSI (or the state supplement), because his/her income and/or resources are in excess of cash assistance standards, but who has insufficient income and/or resources to meet the cost of his/her necessary medical and remedial care (42 CFR 435.320 (aged), 435.322 (blind) and 435.324 (disabled)). 1
2. All beneficiary protections apply to MMMC, MLTC and HARPs, unless otherwise noted in STC 5 2
3. Throughout these STCs, the term "Health Home," unless otherwise noted, only refers to Health Homes approved under section 1945 of the Act and consistent with approved NY Health Home state plan benefits for Health Homes SPA for IDD, Health Homes SPA for children, and/or Health Home SPA for Chronic Medical and SSI Health Home program. 3
4. For a description of CMS's current policies related to budget neutrality for Medicaid demonstration projects authorized under section 1115(a) of the Act, see State Medicaid Director Letter #18-009. 4
5. 42 CFR §431.420(a)(2) provides that states must comply with the terms and conditions of the agreement between the Secretary (or designee) and the state to implement a demonstration project, and §431.420(b)(1) states that the terms and conditions will provide that the state will perform periodic reviews of the implementation of the demonstration. CMS's current approach is to include language in STCs requiring, as a condition of demonstration approval, that states provide, as part of their periodic reviews, regular reports of the actual costs which are subject to the budget neutrality limit. CMS has obtained Office of Management and Budget (OMB) approval of the monitoring tool under the Paperwork Reduction Act (OMB Control No. 0938 - 1148) and in states agree to use the tool as a condition of demonstration approval. 5
Follow Us