MRT Plan Current STCs - January 9, 2024
- Plan is also available in Portable Document Format (PDF)
CENTERS FOR MEDICARE & MEDICAID SERVICES
WAIVER AUTHORITIES
NUMBER: 11-W-00114/2
TITLE: Medicaid Redesign Team
AWARDEE: New York State Department of Health
All requirements of the Medicaid program expressed in law, regulation, and policy statement, not expressly waived in this list, shall apply to the demonstration.
The following waivers shall enable New York to implement the approved Special Terms and Conditions (STC) for the New York Medicaid Redesign Team (MRT) section 1115 demonstration (formerly the New York Partnership Plan) beginning April 1, 2022, and ending March 31, 2027.
1. Statewideness Section 1902(a)(1)
To permit New York to geographically phase in the Managed Long Term Care (MLTC) program and the Health and Recovery Plans (HARP) and to phase in Behavioral Health (BH) Home and Community Based Services (HCBS) into HIV Special Needs Plans (HIV SNP).
2. Comparability Section 1902(a)(10), section 1902(a)(17)
- To enable New York to apply a more liberal income standard for individuals who are deinstitutionalized and receive HCBS through the managed long-term care program than for other individuals receiving community-based long-term care.
- To the extent necessary to permit New York to waive cost sharing for non-drug benefit cost sharing imposed under the Medicaid state plan for beneficiaries enrolled in the Mainstream Medicaid Managed Care Plan (MMMC) - including HARP and HIV SNPs - and who are not otherwise exempt from cost sharing in 447.56(a)(1).
- Family of One Non-1915 Children, or "Fo1 Children" - To allow the state to target eligibility to, and impose a participation capacity limit on, medically needy children under age 21 who are otherwise described in 42 Code of Federal Regulations (CFR) § 435.308 of the regulations who: 1) receive Health Home Comprehensive Care Management under the state plan in replacement of the case management services such individuals formerly received through participation in New York's NY #.4125 1915(c) waiver and who no longer participate in such waiver due to the elimination of the case management services, but who continue to meet the targeting criteria, risk factors and clinical eligibility standard for such waiver; and 2) receive HCBS 1915(c) services who meet the risk factors, targeting criteria, and clinical eligibility standard for the above-identified 1915(c) waiver. Individuals who meet either targeting classification will have excluded from their financial eligibility determination the income and resources of third parties whose income and resources could otherwise be deemed available under 42 CFR §435.602(a)(2)(i). Such individuals will also have their income and resources compared to the medically needy income level (MNIL) and resource standard for a single individual, as described in New York's state Medicaid plan.
3. Amount, Duration & Scope Section 1902(a)(10)(B)
To enable New York to provide BH HCBS services and the Adult Rehabilitation Services named Community Oriented Recovery and Empowerment (CORE) Services, whether furnished as a state plan benefit or as a demonstration benefit to targeted populations that may not be consistent with the targeting authorized under the approved state plan, in amount, duration and scope that exceeds those available to eligible individuals not in those targeted populations.
4. Freedom of Choice Section 1902(a)(23)(A)
To the extent necessary to enable New York to require beneficiaries to enroll in managed care plans, including the MMMC, and MLTC (excluding individuals designated as "Long-Term Nursing Home Stays") and HARPs programs in order to obtain benefits offered by those plans. Beneficiaries shall retain freedom of choice of family planning providers.
5. Reasonable Promptness Section 1902(a)(8)
To enable the state to limit the number of medically needy Fo1 Children not otherwise enrolled in the Children's 1915(c) waiver.
Title XIX Requirements Not Applicable to Self-Direction Pilot Program
(see Expenditure Authority 8, "Self-Direction Pilot")
6. Direct Payment to Providers Section 1902(a)(32)
To the extent necessary to permit the state to make payments to beneficiaries enrolled in the Self Direction Pilot Program to the extent that such funds are used to obtain self-directed HCBS long term care (LTC) services and supports.
EXPENDITURE AUTHORITIES
NUMBER: 11-W-00114/2
TITLE: Medicaid Redesign Team
AWARDEE: New York State Department of Health
Under the authority of section 1115(a)(2) of the Social Security Act ("the Act"), expenditures made by New York for the items identified below, which are not otherwise included as expenditures under section 1903 of the Act shall, until the ending date specified for each authority as listed below, be regarded as expenditures under the state's title XIX plan. These expenditure authorities shall be effective from April 1, 2022, through March 31, 2027, except as otherwise noted.
The following expenditure authorities shall enable New York to implement the approved Special Terms and Conditions (STC) for the New York Medicaid Redesign Team Medicaid Section 1115 demonstration.
- Demonstration-Eligible Populations. Expenditures for healthcare related costs for the following populations that are not otherwise eligible under the Medicaid state plan.
- Demonstration Population 2 (Temporary Assistance for Needy Families (TANF) Adult). TANF Recipients. Expenditures for health care related costs for low-income adults enrolled in TANF. These individuals are exempt from receiving a Modified Adjusted Gross Income (MAGI) determination in accordance with 1902(e)(14)(D)(i)(I) of the Act.
- Demonstration Population 9 (HCBS Expansion). Individuals who are not otherwise eligible, are receiving HCBS, and who are determined to be medically needy based on New York's medically needy income level, after application of community spouse and spousal impoverishment eligibility and post-eligibility rules consistent with section 1924 of the Act.
- Demonstration Population 10 (Institution to Community). Expenditures for health care related costs for individuals moved from institutional nursing facility settings to community settings for long term services and supports who would not otherwise be eligible based on income, but whose income does not exceed the income standard described in STC 4.4(c), and who receive services through the managed long-term care program under the demonstration.
- Included in Demonstration Population 12 [Family of One (Fo1) Children]. Medically needy children Fo1 Demonstration children under age 21 with a waiver of 1902(a)(10)(C)(i)(III) who meet the targeting criteria, risk factors, and clinical eligibility standard for #NY.4125 waiver including intermediate care facilities (ICF), nursing facilities (NF), or Hospital Level of Care (LOC) who are not otherwise enrolled in the Children's 1915(c).
- Twelve-Month Continuous Eligibility Period. Expenditures for health care related costs for individuals who have been determined eligible under groups specified in Table 6 of STC 4.4(e) for continued benefits during any periods within a twelve-month eligibility period when these individuals would be found ineligible if subject to redetermination. This authority includes providing continuous coverage for the Adult Group determined financially eligible using MAGI based eligibility methods. For expenditures related to the Adult Group, specifically, the state shall make a downward adjustment of 2.6 percent in claimed expenditures for federal matching at the enhanced federal matching rate and will instead claim those expenditures at the regular matching rate.
- Facilitated Enrollment Services. Expenditures for enrollment assistance services provided by managed care organizations (MCO), the costs for which are included in the claimed MCO capitation rates.
- Demonstration Services for Behavioral Health Provided under Mainstream Medicaid Managed Care. Expenditures for provision of residential addiction services, crisis intervention and licensed behavioral health practitioner services to MMMC enrollees only and are not provided under the state plan [Demonstration Services 9].
- Targeted Behavioral Health HCBS and CORE Services. Expenditures for the provision of BH HCBS and CORE Services under HARP and HIV SNP that are not otherwise available under the approved state plan [Demonstration Services 8].
- Self-Direction Pilot. Expenditures to allow the state to make self-direction services available to HARP and HIV/SNP enrollees receiving BH HCBS or children meeting targeting criteria for the Children's 1915(c) Waiver and in MMMC receiving HCBS under the Children's Waiver. The program will be in effect from January 1, 2017, through March 31, 2027 [Demonstration Services 8].
- Residential and Inpatient Treatment for Individuals with Substance Use Disorder (SUD). Expenditures for Medicaid state plan services furnished to otherwise eligible individuals who are primarily receiving treatment and/or withdrawal management services for substance use disorder (SUD) who are short-term residents in facilities that meet the definition of an institution for mental diseases (IMD).
- Health-Related Social Needs (HRSN) Services. Expenditures for health-related social needs services not otherwise covered that are furnished to individuals who meet the qualifying criteria as described in Section 6. This expenditure authority is contingent on compliance with Section 7, as well as all other applicable STCs.
- Expenditures for HRSN Services Infrastructure. Expenditures for payments for allowable administrative costs and infrastructure not otherwise eligible for Medicaid payment, to the extent such activities are authorized in Section 6 of the STCs. This expenditure authority is contingent on compliance with Section 7 of the STCs, as well as all other applicable STCs.
- Medicaid Hospital Global Budget Initiative. Expenditures for incentive payments to eligible private not-for-profit hospitals with a 0 percent or less operating margin for meeting data collection requirements, reporting expectations, meeting milestones for transitioning to alternative payment models, and demonstrating improvement in health care quality and equity, as specified in the STCs.
- Designated State Health Programs (DSHP). Expenditures for designated programs, described in these STCs (Section 11), which are otherwise state-funded, and not otherwise eligible for Medicaid payment. These expenditures are subject to the terms and limitations and not to exceed specified amounts as set forth in these STCs. These expenditures are specifically contingent on compliance with Section 7, as well as all other applicable STCs.
- Health Equity Regional Organization (HERO). Expenditures for an independent contracted statewide entity designed to develop regionally focused approaches to reduce health disparities, advance health equity, and support the delivery of health-related social needs as described in Section 13.
- Workforce Initiatives. Expenditures for provider student loan repayment and Career Pathway Training programs that meet the criteria as specified in Section 12 of the STCs.
- Time limited expenditure authority is granted until four years following the demonstration, in order for the state to pay close-out administrative and monitoring service commitments.
Title XIX Requirements Not Applicable to the HRSN Expenditure Authorities
Comparability; Amount, Duration, and Scope Section 1902(a)(10)(B), Section 1902(a)(17)
To the extent necessary to enable the state to provide a varying amount, duration, and scope of HRSN services to a subset of beneficiaries, depending on beneficiary needs.
Comparability; Provision of Medical Assistance and Reasonable Promptness 1902(a)(17), 1902(a)(8) Sections 1902(a)(10)(B),
To the extent necessary to allow the state to offer HRSN services to an individual who meets the qualifying criteria for HRSN services, including delivery system enrollment, as described in Section 6 of the STCs.
To the extent necessary to allow the state to delay the application review process for HRSN services in the event the state does not have sufficient funding to support providing these services to eligible beneficiaries.
SPECIAL TERMS AND CONDITIONS
NUMBER: 11-W-00114/2
TITLE: Medicaid Redesign Team
AWARDEE: New York State Department of Health
1. PREFACE
The following are the STCs for the New York Medicaid Redesign Team section 1115(a) Medicaid demonstration (hereinafter "demonstration" or "MRT") to enable the New York State Department of Health (hereinafter "state" or "DOH") to operate this demonstration. The Centers for Medicare & Medicaid Services (CMS) has granted the state waivers of requirements under section 1902(a) of the Social Security Act (hereinafter "the Act") and expenditure authorities authorizing federal matching of demonstration costs that are not otherwise matchable and which are separately enumerated.
These STCs set forth in detail the nature, character, and extent of federal involvement in the Demonstration and New York's obligations to CMS related to this demonstration. The MRT demonstration will be statewide and is approved from April 1, 2022, through March 31, 2027.
The STCs have been arranged into the following sections:
- Preface
- Program Description and Objectives
- General Program Requirements
- Populations Affected by and Eligible Under the Demonstration
- Demonstration Benefits and Enrollment
- Health-Related Social Needs (HRSN) Services
- Provider Payment Rate Increase Requirement
- SUD Program and Benefits
- Medicaid Hospital Global Budget Initiative
- Delivery Systems
- Designated State Health Programs (DSHP)
- Workforce Initiatives
- Health Equity Regional Organization (HERO)
- Monitoring and Reporting Requirements
- General Financial Requirements
- Monitoring Budget Neutrality
- Evaluation of the Demonstration
- Schedule of Deliverables for the Demonstration
Additional attachments have been included to provide supplementary information and for specific STCs.
- Home and Community-Based Services (HCBS) Expansion Program Benefits
- Behavioral Health (BH) HCBS and Community Oriented Recovery and Empowerment (CORE) Services in Health and Recovery Plans (HARP)
- Mandatory Managed Long-Term Care/Care Coordination Model (CCM)
- List of Eligible Goods and Services Under BH HCBS Individual Directed Goods and Services
- Developing the Evaluation Design
- Preparing the Interim and Summative Evaluation Reports
- Evaluation Design [Reserved]
- SUD Implementation Plan
- SUD Monitoring Protocol [Reserved]
- HRSN Implementation Plan [Reserved]
- Assessment of Beneficiary Eligibility and Needs, Infrastructure Planning, and Provider Qualifications for HRSN Services Protocol [Reserved]
- Medicaid Hospital Global Budget Initiative Implementation Protocol [Reserved]
- Provider Rate Increase Attestation Table [Reserved]
- Approved List of DSHPs
- DSHP Claiming Protocol [Reserved]
- Monitoring Protocol for Other Policies [Reserved]
- DSHP Sustainability Plan [Reserved]
2. PROGRAM DESCRIPTION AND OBJECTIVES
The state's goal in implementing the Medicaid Redesign Team Section 1115(a) demonstration is to improve access to health services and outcomes for low-income New Yorkers by:
- Improving access to health care for the Medicaid population;
- Improving the quality of health services delivered;
- Expanding coverage with resources generated through managed care efficiencies to additional low-income New Yorkers;
- Advancing health equity, reducing health disparities, and supporting the delivery of HRSN services.
The demonstration is designed to permit New York to use a managed care delivery system to deliver benefits to Medicaid recipients, create efficiencies in the Medicaid program, and enable the extension of coverage to certain individuals who need long term care and supports. It was originally approved in 1997 to enroll most Medicaid recipients into MCOs (Medicaid managed care program). As part of the demonstration's renewal in 2006, authority to require some disabled and aged populations to enroll in mandatory managed care was transferred to a new demonstration, the Federal-State Health Reform Partnership (F-SHRP). Effective April 1, 2014, this authority was restored to this demonstration as F-SHRP was phased out.
In 2001, the Family Health Plus (FHPlus) program was implemented as an amendment to the demonstration, providing comprehensive health coverage to low-income uninsured adults, with and without dependent children, who have income greater than Medicaid state plan eligibility standards. FHPlus was further amended in 2007 to implement an employer sponsored health insurance (ESHI) component. Individuals eligible for FHPlus who have access to cost-effective ESHI are required to enroll in that coverage, with FHPlus providing any wrap-around services necessary to ensure that enrollees get all FHPlus benefits. FHPlus expired on December 31, 2013, and became a state-only program, but federal matching funding for state expenditures for FHPlus will continue to be available as a designated state health program through December 31, 2014.
In 2002, the demonstration was expanded to incorporate a family planning benefit under which family planning and family planning related services were provided to women losing Medicaid eligibility and to certain other adults of childbearing age (family planning expansion program). The family planning expansion program expired on December 31, 2013, and became a state plan benefit.
In 2010, the Home and Community Based Services Expansion program (HCBS Expansion program) was added to the demonstration. It covers cost-effective home and community-based services to certain adults with significant medical needs as an alternative to institutional care in a nursing facility. The benefits and program structure mirrors those of existing section 1915(c) waiver programs and aims to cover quality services for individuals in the community, ensure the well-being and safety of the participants and increase opportunities for self-advocacy and self-reliance.
As part of the 2011 extension, the state was authorized to develop and implement two new initiatives designed to improve the quality of care rendered to Partnership Plan recipients. The first, the Hospital-Medical Home (H-MH) project, provided funding and performance incentives to hospital teaching programs in order to improve the coordination, continuity and quality of care for individuals receiving primary care in outpatient hospital settings and facilitate certification of such programs by the National Committee for Quality Assurance as patient-centered medical homes. This demonstration initiative ended on December 31, 2014.
Under the second 2011 initiative, the state would have provided funding, on a competitive basis, to hospitals and/or collaborations or hospitals and other providers for the purpose of developing and implementing strategies to reduce the rate of Potentially Preventable Readmissions for the Medicaid population. The demonstration initiative was never implemented.
In 2011 CMS began providing matching funding for the state's program to address clinic uncompensated care through its Indigent Care Pool (ICP). This pool expired on December 31, 2014.
In 2012, New York added to the demonstration an initiative to improve service delivery and coordination of long-term care services and supports for individuals through a managed care model. Under the MLTC program, eligible individuals in need of more than 120 days of community-based long-term care are enrolled with managed care providers to receive long term services and supports as well as other ancillary services. Other covered services are available on a fee-for-service basis to the extent that New York has not exercised its option to include the individual in the MMMC program. Enrollment in MLTC was phased in geographically and by group.
The state's goals specific to MLTC are listed below:
- Expanding access to managed long-term care for Medicaid enrollees who are in need of long-term services and supports (LTSS)
- Improving patient safety and quality of care for enrollees in MLTC plans
- Reducing preventable inpatient and nursing home admissions
- Improving satisfaction, safety and quality of life
In April 2013, New York had three amendments approved. The first amendment was a continuation of the state's goal for transitioning more Medicaid beneficiaries into managed care. Under this amendment, the Long-Term Home Health Care Program (LTHHCP) participants began transitioning, on a geographic basis, from New York's 1915(c) waiver into the 1115 demonstration and into managed care. Second, this amendment eliminated the exclusion from MMMC of both foster care children placed by local social service agencies and individuals participating in the Medicaid buy-in program for the working disabled.
Additionally, the April 2013 amendment approved expenditure authority for New York to claim federal financial participation (FFP) for expenditures made for certain DSHP beginning April 1, 2013, through March 31, 2014. These DSHPs were aimed to improve health outcomes for Medicaid and other low-income individuals, and the federal funding was linked to requirements for the state to submit deliverables to demonstrate successful efforts to transform its health system for individuals with developmental disabilities.
A December 2013 amendment was approved to ensure that the demonstration made changes that were necessary in order to coordinate its programs with the Medicaid expansion and other changes made under the Affordable Care Act (ACA) implementation beginning January 1, 2014.
Effective April 1, 2014, CMS approved an amendment to extend several authorities that expired in calendar year 2014. As part of the amendment CMS extended authorities related to the transitioning of parents into state plan coverage and other authorities that provide administrative ease to the state's programs and continuing to provide services to vulnerable populations, i.e. HCBS Expansion program and individuals moved from institutional settings into community-based settings.
Also, effective April 1, 2014, populations receiving managed care or managed long-term care in the 14 counties that encompassed the Federal-State Health Reform Partnership (F-SHRP) demonstration were moved into this demonstration.
An amendment approved on April 14, 2014, allowed New York to take the first steps toward a major delivery system reform through a Delivery System Reform Incentive Payment (DSRIP) program. This amendment to the Partnership Plan demonstration provided for an Interim Access Assurance Fund (IAAF) to ensure that sufficient numbers and types of providers were available in the community to participate in the transformation activities contemplated by the DSRIP Program. The DSRIP program incentivized providers through additional payments beginning in 2015. The amendment also included expenditure authority for DSHPs to allow the state to concentrate resources on the investments necessary to implement its DSRIP program. Savings from the DSRIP program were anticipated to exceed the cost of the DSHP program.
On December 31, 2014, CMS amended the demonstration to enable New York to extend long term nursing facility services to enrollees of New York's MMMC and MLTC populations. Enrollment in MMMC and MLTC was extended to individuals entering residential health care facilities (RHCF) for stays that are classified as permanent. As part of the agreement, the state also instituted an independent LTSS assessment process via an enrollment broker and implemented its Independent Consumer Support Program in areas of the state where services and enrollment were being instituted.
In August 2015, CMS approved New York's request to implement HARP to integrate physical, behavioral health and BH HCBS for Medicaid enrollees with Serious Mental Illness (SMI) and/or SUD to receive services in their own homes and communities. Under the demonstration, HARPs are a separate coverage product that is targeted to Medicaid enrollees that meet need-based criteria for SMI and/or SUD established by the state. HIV SNP under MMMC will also offer BH HCBS services to eligible individuals meeting targeting, risk, and functional needs criteria. All MMMC plans will offer BH benefits in integrated plans including four new demonstration services.
The demonstration was also amended to effectuate eligibility flexibilities for the Adult Group, including allowing adults enrolled in TANF to be enrolled as a demonstration population, without a MAGI determination, extension of continuous eligibility for members of the Adult Group who turn 65 during their continuous eligibility period and temporary coverage for members of the Adult Group who are determined eligible to receive coverage through the Marketplace.
On November 30, 2016, CMS approved an extension of the demonstration, but in response to comments by the state, that extension was rescinded and superseded by a modified approval effective December 7, 2016. In December 2016, the Partnership Plan was renamed New York MRT. The extension included time-limited authorization to extend the DSRIP program first authorized in 2014, through March 31, 2020. The extension also included a new time-limited DSHP authority to the extent that the state increases its Medicaid expenditures through its DSRIP program and achieves metrics that will result in anticipated cost savings that offset the DSHP expenditures. DSHP funding will be phased down over the demonstration period. The DSRIP and DSHP authorities are intended to be a one-time investment in system transformation that can be sustained through ongoing payment mechanisms and/or state and local initiatives.
The Behavioral Health Self-Direction Pilot was included as part of the renewal. This pilot made self-direction services available to HARP and HIV SNP enrollees receiving BH HCBS. The program is authorized to be in effect from January 1, 2017, through March 31, 2027
On April 19, 2019, CMS approved an amendment to allow a waiver of comparability which permits managed care enrollees to only be assessed a drug copay. The state will not assess the non-drug benefit cost sharing described in the Medicaid state plan.
On August 2, 2019, CMS approved an amendment containing the following changes:
- Allow children with HCBS under the state's 1915(c) Children's Waiver and children placed in foster care through a Voluntary Foster Care Agency (VFCA) to enroll in Mainstream Managed Care or an HIV SNP.
- Continues Medicaid eligibility for Non-1915 children who would have been eligible under the Children's Waiver had case management not been moved under the State Plan as a Health Home service or who were in a non-SSI category and receive HCBS or Health Home (HH) comprehensive case management.
- Include Children's Waiver HCBS and State Plan behavioral health services in the Medicaid managed care benefit package.
- Include children receiving HCBS under the Children's waiver in the Self Direction Pilot for Individual Directed Goods and Services.
On December 19, 2019, CMS approved an amendment with the following changes for Partially Capitated MLTC plans:
- Implement a lock-in policy for partially capitated MLTC plans, pursuant to which enrollees of partially capitated MLTC plans are able to transfer to another partially capitated plan without cause during the first 90 days of a 12-month period and with good cause during the remainder of the period. A member of a partially capitated MLTC plan may transfer to another type of MLTC plan at any time.
- Limit the nursing home benefit in the partially capitated MLTC plan to three months for those enrollees who have been designated as Long-Term Nursing Home Stays (LTNHS) in a skilled nursing or residential health care facility, at which time the individual will be involuntarily disenrolled from the partially capitated MLTC plan and payment for nursing home services will be covered by Medicaid fee for service for individuals that qualify for institutional Medicaid coverage. Consistent with this partially capitated MLTC benefit change, individuals age 21 years of age or older who are dually eligible for Medicare and Medicaid and LTNHS in a nursing home will be excluded from enrollment in a partially capitated MLTC plan.
On October 5, 2021, CMS approved an amendment that added a set of rehabilitative services (as such term is defined in Section 1905(a)(13) of the Social Security Act) called CORE, substitutes for and improves upon four BH HCBS within the HARP and HIV SNP. CORE Services can be found in Attachment B and are available to HARP members and HIV SNP members meeting HARP eligibility criteria for whom such services are recommended by a physician or Licensed Practitioner of the Healing Arts as defined by New York State. Through the transition to CORE Services, the state will improve access to rehabilitation and recovery services for HARP beneficiaries. New York State will ensure continuity of care for individuals for BH HCBS including the four services transitioning to CORE. Individuals receiving or eligible for remaining BH HCBS and the BH HCBS, which directly transition to CORE Services will not receive a reduction in services and/or eligibility based on this demonstration amendment. The list of BH HCBS can also be found in Attachment B.
On March 23, 2022, CMS approved a 5-year extension of the New York Medicaid Redesign Team demonstration. As part of the extension, CMS approved the state's second component of its MLTC amendment request to allow dual eligibles to stay in Mainstream Managed Care Plans that offer D-SNPs once they become eligible for Medicare.
On January 9, 2024 CMS approved an amendment that provides authority for HRSN services and HRSN infrastructure, a Medicaid Hospital Global Budget Initiative, workforce initiatives, a HERO, and DSHP. The amendment also provided the state with SUD demonstration authority.
The overarching goal of this amendment is to advance health equity, reduce health disparities, and support the delivery of social care through Social Care Networks (SCNs) and improve overall quality and health. Through the combination of a Medicaid Hospital Global Budget Initiative, HRSN activities, workforce initiatives, and HERO, the state is working to improve health equity. As a result, CMS considers this amendment a Health Equity Initiative. Additionally, by the end of the demonstration, the state's goal is to have made significant movement towards value-based payment (VBP) strategies, multi-payor alignment, and population health accountability. Each program has individual goals that align with the overall goal:
- Investments in Health Related Social Needs (HRSN) via greater integration between primary care providers (PCPs) and community-based organizations (CBOs) with a goal of improved quality and health outcomes;
- Goal of improving quality and outcomes of enrollees in geographies that have a longstanding history of health disparities and disengagement from the health system;
- Focus on integrated primary care, BH, and HRSN with a goal to improve population health and health equity outcomes for high-risk enrollees including kids/youth, pregnant and postpartum individuals, the chronically homeless, and individuals with SMI and SUD;
- Workforce investments with a goal of equitable and sustainable access to care in Medicaid
- Developing regionally-focused approaches, including new value-based payment programs, with a goal of statewide accountability for improving health, outcomes, and equity.
Under the SUD demonstration authority, the state will maintain and enhance access to mental health services, opioid use disorder (OUD) and other SUD services and continue delivery system improvements for these services to provide more coordinated and comprehensive treatment of Medicaid beneficiaries with SUD. The demonstration amendment will provide the state with authority to provide high-quality, clinically appropriate treatment to beneficiaries with SUD while they are short-term residents in residential and inpatient treatment settings that qualify as an IMD. The amendment will also support state efforts to enhance provider capacity, improve the availability of Medication Assisted Treatment (MAT) and improve access to a continuum of SUD evidence-based services at varied levels of intensity, including withdrawal management services.
In alignment with the respective SUD demonstration State Medicaid Director Letter (SMDL)1, under the SUD program, during the demonstration period, the state seeks to achieve the following goals:
SUD Goals:
- Increase rates of identification, initiation, and engagement in treatment for SUD.
- Increase adherence to and retention in treatment.
- Reduce overdose deaths, particularly those due to opioids.
- Reduce utilization of emergency departments and inpatient hospital settings for treatment where the utilization is preventable or medically inappropriate through improved access to other continuum of care services.
- Fewer readmissions to the same or higher level of care where the readmission is preventable or medically inappropriate.
- Improve access to care for physical health conditions among beneficiaries with SUD.
3. GENERAL PROGRAM REQUIREMENTS
- 3.1 Compliance with Federal Non-Discrimination Statutes. The state must comply with all applicable federal statutes relating to non-discrimination. These include, but are not limited to, the Americans with Disabilities Act of 1990 (ADA), Title VI of the Civil Rights Act of 1964, section 504 of the Rehabilitation Act of 1973 (Section 504), the Age Discrimination Act of 1975, and section 1557 of the Patient Protection and Affordable Care Act (Section 1557).
- 3.2 Compliance with Medicaid and Children's Health Insurance Program (CHIP) Law, Regulation, and Policy. All requirements of the Medicaid and CHIP programs expressed in federal law, regulation, and policy statement, not expressly waived or identified as not applicable in the waiver and expenditure authority documents (of which these terms and conditions are part), apply to the demonstration.
- 3.3 Changes in Medicaid and CHIP Law, Regulation, and Policy. The state must, within the timeframes specified in federal law, regulation, or written policy, come into compliance with any changes in law, regulation, or policy affecting the Medicaid or CHIP programs that occur during this demonstration approval period, unless the provision being changed is expressly waived or identified as not applicable. In addition, CMS reserves the right to amend the STCs to reflect such changes and/or changes as needed without requiring the state to submit an amendment to the demonstration under STC 3.7. CMS will notify the state 30 business days in advance of the expected approval date of the amended STCs to allow the state to provide comment. Changes will be considered in force upon issuance of the approval letter by CMS. The state must accept the changes in writing.
- 3.4 Impact on Demonstration of Changes in Federal Law, Regulation, and Policy.
- To the extent that a change in federal law, regulation, or policy requires either a reduction or an increase in federal FFP for expenditures made under this demonstration, the state must adopt, subject to CMS approval, a modified budget neutrality agreement for the demonstration as necessary to comply with such change, as well as a modified allotment neutrality worksheet as necessary to comply with such change. The trend rates for the budget neutrality agreement are not subject to change under this subparagraph. Further, the state may seek an amendment to the demonstration (as per STC 3.7 of this section) as a result of the change in FFP.
- If mandated changes in the federal law require state legislation, unless otherwise prescribed by the terms of the federal law, the changes must take effect on the earlier of the day such state legislation becomes effective, or on the last day such legislation was required to be in effect under the law, whichever is sooner.
- 3.5 State Plan Amendments. The state will not be required to submit title XIX or XXI state plan amendments (SPA) for changes affecting any populations made eligible solely through the demonstration. If a population eligible through the Medicaid or CHIP state plan is affected by a change to the demonstration, a conforming amendment to the appropriate state plan is required, except as otherwise noted in these STCs. In all such cases, the Medicaid and CHIP state plans govern.
- 3.6 Changes Subject to the Amendment Process. Changes related to eligibility, enrollment, benefits, beneficiary rights, delivery systems, cost sharing, sources of non-federal share of funding, budget neutrality, and other comparable program elements must be submitted to CMS as amendments to the demonstration. All amendment requests are subject to approval at the discretion of the Secretary in accordance with section 1115 of the Act. The state must not implement changes to these elements without prior approval by CMS either through an approved amendment to the Medicaid or CHIP state plan or amendment to the demonstration. Amendments to the demonstration are not retroactive and no FFP of any kind, including for administrative or medical assistance expenditures, will be available under changes to the demonstration that have not been approved through the amendment process set forth in STC 3.7 below, except as provided in STC 3.3.
- 3.7 Amendment Process. Requests to amend the demonstration must be submitted to CMS for approval no later than 120 calendar days prior to the planned date of implementation of the change and may not be implemented until approved. CMS reserves the right to deny or delay approval of a demonstration amendment based on non-compliance with these STCs, including but not limited to the failure by the state to submit required elements of a complete amendment request as described in this STC, and failure by the state to submit required reports and other deliverables according to the deadlines specified therein. Amendment requests must include, but are not limited to, the following:
- An explanation of the public process used by the state, consistent with the requirements of STC 3.12. Such explanation must include a summary of any public feedback received and identification of how this feedback was addressed by the state in the final amendment request submitted to CMS;
- A detailed description of the amendment, including impact on beneficiaries, with sufficient supporting documentation;
- A data analysis which identifies the specific "with waiver" impact of the proposed amendment on the current budget neutrality agreement. Such analysis must include current total computable "with waiver" and "without waiver" status on both a summary and detailed level through the current approval period using the most recent actual expenditures, as well as summary and detailed projections of the change in the "with waiver" expenditure total as a result of the proposed amendment, which isolates (by Eligibility Group) the impact of the amendment;
- An up-to-date CHIP allotment worksheet, if necessary;
- The state must provide updates to existing demonstration reporting and quality and evaluation plans. This includes a description of how the evaluation design and annual progress reports will be modified to incorporate the amendment provisions, as well as the oversight, monitoring and measurement of the provisions.
3.8 Extension of the Demonstration. States that intend to request an extension of the demonstration must submit an application to CMS at least 12 months in advance from the Governor or Chief Executive Officer of the state in accordance with the requirements of 42 CFR 431.412(c). States that do not intend to request an extension of the demonstration beyond the period authorized in these STCs must submit phase-out plan consistent with the requirements of STC 3.9. 3.9 Demonstration Phase-Out. The state may only suspend or terminate this demonstration in whole, or in part, consistent with the following requirements.
- Notification of Suspension or Termination: The state must promptly notify CMS in writing of the reason(s) for the suspension or termination, together with the effective date and a transition and phase-out plan. The state must submit a notification letter and a draft transition and phase-out plan to CMS no less than six months before the effective date of the demonstration's suspension or termination. Prior to submitting the draft transition and phase-out plan to CMS, the state must publish on its website the draft transition and phase-out plan for a 30-day public comment period. In addition, the state must conduct tribal consultation in accordance with STC 3.12, if applicable. Once the 30-day public comment period has ended, the state must provide a summary of the issues raised by the public during the comment period and how the state considered the comments received when developing the revised transition and phase-out plan.
- Transition and Phase-out Plan Requirements: The state must include, at a minimum, in its phase-out plan the process by which it will notify affected beneficiaries, the content of said notices (including information on the beneficiary's appeal rights), the process by which the state will conduct administrative reviews of Medicaid or CHIP eligibility prior to the termination of the demonstration for the affected beneficiaries, and ensure ongoing coverage for eligible beneficiaries, as well as any community outreach activities the state will undertake to notify affected beneficiaries, including community resources that are available.
- Transition and Phase-out Plan Approval. The state must obtain CMS approval of the transition and phase-out plan prior to the implementation of transition and phase-out activities. Implementation of transition and phase-out activities must be no sooner than 14 calendar days after CMS approval of the transition and phase-out plan.
- Transition and Phase-out Procedures: The state must redetermine eligibility for all affected beneficiaries in order to determine if they qualify for Medicaid eligibility under a different eligibility category prior to making a determination of ineligibility as required under 42 CFR 35.916(f)(1), or for children in CHIP consider eligibility for other insurance affordability programs under 42 CFR 457.350. For individuals determined ineligible for Medicaid and CHIP, the state must determine potential eligibility for other insurance affordability programs and comply with the procedures set forth in 42 CFR 435.1200(e). The state must comply with all applicable notice requirements for Medicaid found in 42 CFR, part 431 subpart E, including Sections 431.206 through 431.214 or for CHIP found at 42 CFR 457.340(e), including information about a right to review consistent with 42 CFR 457.1180. In addition, the state must assure all applicable Medicaid appeal and hearing rights are afforded to Medicaid beneficiaries in the demonstration as outlined in 42 CFR, part 431 subpart E, including Sections 431.220 and 431.221. If a beneficiary in the demonstration requests a hearing before the date of action, the state must maintain Medicaid benefits as required in 42 CFR § 431.230.
- Exemption from Public Notice Procedures 42 CFR Section 431.416(g). CMS may expedite the federal and state public notice requirements under circumstances described in 42 CFR 431.416(g).
- Enrollment Limitation during Demonstration Phase-Out. If the state elects to suspend, terminate, or not extend this demonstration, during the last six months of the demonstration, enrollment of new individuals into the demonstration must be suspended. The limitation of enrollment into the demonstration does not impact the state's obligation to determine Medicaid eligibility in accordance with the approved Medicaid state plan.
- FFP. If the project is terminated or any relevant waivers are suspended by the state, FFP must be limited to normal closeout costs associated with the termination or expiration of the demonstration including services, continued benefits as a result of beneficiaries' appeals, and administrative costs of disenrolling beneficiaries.
3.10 Withdrawal of Waiver or Expenditure Authority. CMS reserves the right to withdraw waivers and/or expenditure authorities at any time it determines that continuing the waiver or expenditure authorities would no longer be in the public interest or promote the objectives of title XIX and title XXI. CMS will promptly notify the state in writing of the determination and the reasons for the withdrawal, together with the effective date, and afford the state an opportunity to request a hearing to challenge CMS' determination prior to the effective date. If a waiver or expenditure authority is withdrawn, FFP is limited to normal closeout costs associated with terminating the waiver or expenditure authority, including services, continued benefits as a result of beneficiary appeals, and administrative costs of disenrolling beneficiaries. 3.11 Adequacy of Infrastructure. The state will ensure the availability of adequate resources for implementation and monitoring of the demonstration, including education, outreach, and enrollment; maintaining eligibility systems; compliance with cost sharing requirements; and reporting on financial and other demonstration components. 3.12 Public Notice, Tribal Consultation, and Consultation with Interested Parties. The state must comply with the state notice procedures as required in 42 CFR 431.408 prior to submitting an application to extend the demonstration. For applications to amend the demonstration, the state must comply with the state notice procedures set forth in 59 Fed. Reg. 49249 (September 27, 1994) prior to submitting such request. The state must also comply with the Public Notice Procedures set forth in 42 CFR 447.205 for changes in statewide methods and standards for setting payment rates.
- The state must also comply with tribal and Indian Health Program/Urban Indian Organization consultation requirements at section 1902(a)(73) of the Act, 42 CFR 431.408(b), State Medicaid Director Letter #01-024, or as contained in the state's approved Medicaid State Plan, when any program changes to the demonstration, either through amendment as set out in STC 3.7 or extension, are proposed by the state.
3.13 FFP. No federal matching funds for expenditures for this demonstration, including for administrative and medical assistance expenditures, will be available until the effective date identified in the demonstration approval letter, or if later, as expressly stated within these STCs. 3.14 Administrative Authority. When there are multiple entities involved in the administration of the demonstration, the Single State Medicaid Agency must maintain authority, accountability, and oversight of the program. The State Medicaid Agency must exercise oversight of all delegated functions to operating agencies, MCOs, and any other contracted entities. The Single State Medicaid Agency is responsible for the content and oversight of the quality strategies for the demonstration. 3.15 Common Rule Exemption. The state must ensure that the only involvement of human subjects in research activities that may be authorized and/or required by this demonstration is for projects which are conducted by or subject to the approval of CMS, and that are designed to study, evaluate, or otherwise examine the Medicaid or CHIP program - including public benefit or service programs, procedures for obtaining Medicaid or CHIP benefits or services, possible changes in or alternatives to Medicaid or CHIP programs and procedures, or possible changes in methods or levels of payment for Medicaid benefits or services. CMS has determined that this demonstration as represented in these approved STCs meets the requirements for exemption from the human subject research provisions of the Common Rule set forth in 45 CFR 46.104(d)(5). 4. POPULATIONS AFFECTED BY AND ELIGIBILITY UNDER THE DEMONSTRATION
- 4.1 Eligible under the Medicaid State Plan (State Plan Eligibles). Mandatory and optional Medicaid state plan populations derive their eligibility through the Medicaid state plan and are subject to all applicable Medicaid laws and regulations in accordance with the Medicaid state plan, except as expressly waived and as further described in these STCs. Should the state amend the state plan to make any changes to eligibility for Medicaid mandatory populations, upon submission of the state plan amendment, the state must notify CMS in writing of the pending state plan amendment. The Medicaid Eligibility Groups (MEGs) listed in the Reporting and the Budget Neutrality sections of the STCs will be updated upon approval of changes to State plan eligibility and will be considered a technical change to the STCs.
- 4.2 Individuals Not Otherwise Eligible under the Medicaid State Plan. Beneficiary eligibility groups who are made eligible for the demonstration by virtue of the expenditure authorities expressly granted in this demonstration are subject to Medicaid laws or regulations, except for those identified as non-applicable in the expenditure authorities for this document. Eligibility criteria are described elsewhere in this section. Individuals made eligible under this demonstration by virtue of the expenditure authorities expressly granted include:
- Individuals in the HCBS Expansion program;
- Individuals moved from Institutional Settings to Community Settings and receiving MLTC but who would have excess income or resources under the state plan;
- Adults who are receiving TANF benefits and have not been determined eligible using MAGI-based methods;
- Individuals previously eligible in the adult group who are no longer eligible in that group but are still within a 12-month continuous eligibility period;
- Children under age 21 who are medically needy (both Supplemental Security Income (SSI)-related and non-SSI related) and have parental income and resources (if applicable) waived and otherwise meet eligibility criteria for 1915(c) waiver #.4125 as Fo1 Demonstration children;
- People who are not eligible under the Children's waiver. Note: Unlike the Fo1 Children's (Demonstration Population 12) expenditures authorized under section 1115(a)(2) in these STCs, additional Family of One Children (SSI-related) that receive their HCBS under the state's Children's 1915(c) Waiver do not require this demonstration's expenditure authority.
- 4.3 Program Components. The Medicaid Redesign demonstration includes two distinct components–MMMC and MLTC –each of which affects different populations, some of which are eligible under the state plan and some of which are eligible only as an expansion population underthe demonstration. In addition, subsets of MMMC and MLTC are eligible for additional benefits. Table 1 summarizes the Medicaid state plan populations that are affected by the demonstration. In addition, the following expansion populations must participate in MLTC: Demonstration Population 9 (HCBS Expansion) and Demonstration Population 10 (Institution to Community). More detailed descriptions follow.
Table 1: State Plan Populations Affected by the Demonstration State Plan Mandatory and Optional Groups MMMC: Medicaid-eligible; not otherwise excluded from MMMC enrollment (includes HARP and SNP for eligible individuals) MLTC: Need more than 120 days of community-based long-term care services Pregnant Women Pregnant women (42 CFR §435.116) Income up to 218% of FPL Pregnant minors under age 21 (42 CFR §435.222) No income test Demonstration Population 2 [TANF Adult] Without Medicare: Demonstration Population 5 [Non-Duals 18-64] With Medicare: Demonstration Population 7 [MLTC Adult Age 18-64 Duals] Children Infants (218% FPL) and children under age 19 (149% FPL) (42 CFR §435.117 and §435.118) Demonstration Population 1 [TANF Child] N/A Children age 19 and 20 (42 CFR §435.222) Income up to 133% of FPL if living alone and 150% if living with parents Demonstration Population 1 TANF CHILD Without Medicare: Demonstration Population 5 [Non-Duals 18-64] With Medicare: Demonstration Population 7 [MLTC Adult Age 18-64 Duals] Medically needy children age 19 and 20 (42 CFR §435.308) Income at or below the monthly income standard or with spenddown N/A Without Medicare: Demonstration Population 5 [Non-Duals 18-64] With Medicare: Demonstration Population 7 [MLTC Adult Age 18-64 Duals] Adults Adult group (42 CFR §435.119) Over age 18, under age 65, non-disabled, non-pregnant with income up to 133% of FPL, not eligible for Medicare Part A or B benefits, not eligible under the parents and other caretaker relative group, the foster care child group, or the former foster care child group. Demonstration Population 11 [New Adult Group] New Adult Group: Demonstration Population 11 Parents and Caretakers Parents and other caretaker relatives (42 CFR §435.110 and §435.220) Income up to 133% of FPL Includes low-income adults enrolled in TANF who are exempt from receiving a MAGI determination in accordance with §1902(e)(14)(D)(i)(I) of the Act. Includes Transitional Medical Assistance under sections 1902(a)(52) and (e)(1); 1925; and 1931(c)(2) of the Social Security Act Demonstration Population 2 [TANF Adult] Without Medicare: Demonstration Population 5 [Non-Duals 18-64] With Medicare: Demonstration Population 7 [MLTC Adult Age 18-64 Duals] Medically needy parents and other caretaker relatives (42 CFR §435.310) Income at or below the monthly income standard or with spenddown N/A Without Medicare, Demonstration population 5 [Non-Duals 18-64] With Medicare, Demonstration population 7 [MLTC Adult Age 18-64 Duals] Disabled Blind and disabled individuals age 64 and under receiving SSI (42 CFR §435.120) Voluntarily enrolled or required to enroll in managed care in those counties participating in the MRT (formerly Partnership Plan) as of October 1, 2006, Demonstration Population 3 [SSI 0 through-64] Without Medicare, Demonstration Population 5 [Non-Duals 18-64] With Medicare, Demonstration Population 7 [MLTC Adults 18-64 Duals] Medically needy adults/children aged 18 through 64 blind and disabled (42 CFR §435.322 and §324) Income at or below the monthly income standard, or with spend down to monthly income standard N/A Without Medicare, Demonstration Population 5 [Non-Duals 18-64] With Medicare, Demonstration Population 7 [MLTC Adults 18-64 Duals] Aged 18 through 64 Medicaid Buy In for Working People with Disabilities Income up to 250% of FPL Demonstration Population 2 [TANF Adult] Without Medicare, Demonstration Population 5 [Non-Duals 18-64] With Medicare, Demonstration Population 7 [MLTC Adults 18-64 Duals] Aged Aged Individuals Age 65 and Over Receiving SSI (42 CFR §435.120) Optional Adults aged 65 or older (42 CFR §435.210) Voluntarily enrolled or required to enroll in managed care in those counties participating in the MRT (formerly Partnership Plan) as of October 1, 2006, Demonstration Population 4, [SSI 65 and above] Without Medicare, Demonstration Population 6 [Non-Duals 65+] With Medicare, Demonstration Population 8 [MLTC age 65+ Duals] Medically needy age 65 and over (42 CFR §435.320) Income at or below the monthly income standard, or with spend down to monthly income standard N/A Without Medicare, Demonstration Population 6 [Non-Duals 65+] With Medicare, Demonstration Population 8 [MLTC age 65+ Duals] Foster Care Children with adoption assistance, foster care or guardianship under title IV-E (42 CFR §435.145)
No income testDemonstration Population 1 [TANF Child] N/A Children in state foster care Children receiving non IV-E guardianship assistance (42 CFR §435.222)
No income testDemonstration Population 1 [TANF Child] N/A Former foster care children up to age 26 (42 CFR §435.150)
No income testDemonstration Population 1 [TANF Child] N/A Independent Foster Care Adolescents 18 through 20 (In foster care on the date of 18th birthday) (42 CFR §435.226
No income testDemonstration Population 1 [TANF Child] Without Medicare, Demonstration Population 5 [Non-Duals 18-64] With Medicare, Demonstration Population 7 [MLTC Adults 18-64 Duals] Children receiving state adoption assistance (42 CFR 435.227) No income test Demonstration Population 1 [TANF Child] N/A
- MMMC. This component provides Medicaid state plan and demonstration benefits through a managed care delivery system comprised of MCOs and primary care case management (PCCM) arrangements to most recipients eligible under the state plan. All state plan eligibility determination rules apply to these individuals.
- Eligibility. Table 1 above lists the groups of individuals who receive Medicaid benefits through the mainstream Medicaid managed care component of the demonstration, as well as the relevant expenditure reporting category (demonstration population) for each.
- Exclusions and Exemptions from MMMC. Notwithstanding the eligibility criteria in STC 4.3, certain individuals cannot receive benefits through the MMMC program (i.e., excluded), while others may opt out from receiving benefits through the MMMC program (i.e., exempted). Excluded individuals are outside the demonstration and are not included in Demonstration Populations. Exempt individuals are included in the demonstration and in Demonstration Populations regardless of whether they enroll in managed care. Tables 2 and 3 list those individuals either excluded or exempted from MMMC.
* Aliessa Aliens are NOT excluded from Managed Care but are excluded from FFP.
Table 2: Individuals Excluded from MMMC (including HARP and HIV SNP) Individuals who become eligible for Medicaid only after spending down a portion of their income Residents of state psychiatric facilities and residents of Residential Treatment Facilities for Children and Youth Individuals under age 21 who are permanent residents of Residential Health Care Facilities or temporary residents of Residential Health Care Facilities at time of enrollment Medicaid eligible infants living with incarcerated mothers Youth in Office of Children and Family Services (OCFS) facilities and in the care and custody of the Office of Family & Children Services Individuals with access to comprehensive private health insurance Certified blind or disabled children living or expected to live separate and apart from their parents for 30 days or more Individuals expected to be Medicaid eligible for less than 6 months (except for pregnant women) Individuals receiving hospice services (at time of enrollment) Individuals with a "county of fiscal responsibility" code of 97, except for individuals in the New York Office of Mental Health family care program who other than their residence in district 97 would be eligible to enroll in MMMC Individuals with a "county of fiscal responsibility" code of 98 including Individuals in an Office for People with Developmental Disabilities (OPWDD) facility or treatment center Individuals who are under 65 years of age (screened and require treatment) in the Centers for Disease Control and Prevention breast, cervical, colorectal or prostate cancer, and who are not otherwise covered under creditable health coverage (Individuals with a "county of responsibility" code of 99) Individuals who are eligible for Emergency Medicaid Aliessa Court Ordered Individuals* Residents of Assisted Living Programs
Table 3: Individuals who may be exempted from MMMC (including HARP and HIV SNP) Individuals with chronic medical conditions who have been under active treatment for at least 6 months with a sub-specialist who is not a network provider for any Medicaid MCO in the service area or whose request has been approved by the New York State Department of Health Medical Director because of unusually severe chronic care needs. Exemption is limited to six months. Child and Youth residents of Residential Rehabilitation Services for Youth (RRSY). Note: as the RRSY services are phased into managed care through contract amendments, the children in RRSYs will mandatorily phase into the demonstration. Individuals designated as participating in Office for People with Developmental Disabilities (OPWDD)-sponsored programs Medicare recipients who enroll and remain enrolled in the MMMC plan's aligned Medicare D-SNP Native Americans Individuals in the following Section 1915(c) waiver programs: Traumatic Brain Injury (TBI) and Nursing Home Transition & Diversion (NHTD) Individuals in the Office for People with Developmental Disabilities Home and Community Based Services (OPWDD HCBS) Section 1915(c) waiver program - MLTC. This component provides a limited set of Medicaid state plan benefits including long-term services and supports through a managed care delivery system to individuals eligible through the state plan who require more than 120 days of community-based long-term care services as indicated on the uniform assessment tool. See Attachment B for a listing of MLTC services. Services not provided through the MLTC program are provided on a fee-for-service basis. The state has authority to expand mandatory enrollment into MLTC to all individuals identified in under the MLTC column in Table 1 (except those otherwise excluded or exempted as outlined in 3(a)(ii) of this section).
- Eligibility for MLTC. Table 1 above lists the groups of individuals who may be enrolled in the Managed Long Term Care component of the demonstration as well as the relevant expenditure reporting category (demonstration population) for each. To be eligible, all individuals in this program must need more than 120 days of community-based long-term care services and for MAP and PACE also have a nursing home level of care.
- Exclusions and Exemptions from MLTC. Notwithstanding the eligibility criteria in STC 3 of this section, certain individuals cannot receive benefits through the MLTC program (i.e., excluded) while others may request an exemption from receiving benefits through the MLTC program (i.e. exempted). Excluded individuals are outside the demonstration, and are not included in Demonstration Populations. Exempt individuals are included in the demonstration and in Demonstration Populations regardless of whether they enroll in managed care. Tables 4 and 5 list those individuals either excluded or exempted from MLTC.
- Non-duplication of Payment. MLTC Programs will not duplicate services included in an enrollee´s Individualized Education Program under the Individuals with Disabilities Education Act, or services provided under the Rehabilitation Act of 1973.
* Aliessa Aliens are NOT excluded from Managed Care but are excluded from FFP.
Table 4: Individuals excluded from MLTC Residents of psychiatric facilities (stays exceeding 30 days) Residents of skilled nursing or residential health care facilities who have been designated as Long Term Nursing Home Stays (LTNHS) in such facility are excluded from enrollment in a partially capitated MLTC plan. Residents of skilled nursing or residential health care facilities who are enrolled in a partially capitated MLTC plan are ineligible to continue their MLTC plan enrollment if they are LTNHS for more than three months. Individuals expected to be Medicaid eligible for less than six months Individuals eligible for Medicaid benefits only with respect to tuberculosis-related services Individuals with a "county of fiscal responsibility" code 99 in Medicaid Management Information System (MMIS) (Individuals eligible only for breast and cervical cancer services) Individuals receiving hospice services (at time of enrollment) Individuals with a "county of fiscal responsibility" code of 97 (Individuals residing in a state Office of Mental Health facility) Individuals with a "county of fiscal responsibility" code of 98 including Individuals in an Office for People with Developmental Disabilities (OPWDD) facility or treatment center Individuals who are under 65 years of age (screened and require treatment) in the Centers for Disease Control and Prevention (CDC) breast, cervical, colorectal and/or prostate early detection program and need treatment for breast, cervical, colorectal or prostate cancer and who are not otherwise covered under creditable health coverage Residents of intermediate care facilities for individuals with intellectual disabilities (ICF/IID) Individuals who could otherwise reside in an ICF/IID, but choose not to Residents of alcohol/substance abuse long term residential treatment programs Individuals eligible for Emergency Medicaid Individuals in the Office for People with Developmental Disabilities Home and Community Based Services (OPWDD HCBS) section 1915(c) waiver program Individuals in the following section 1915(c) waiver programs: Traumatic Brain Injury (TBI), Nursing Home Transition & Diversion (NHTD) (see Attachment C) Residents of Assisted Living Programs Individuals in receipt of Limited Licensed Home Care Services Individuals in the Foster Family Care Demonstration Aliessa Court Ordered Individuals*
Table 5: Individuals who may be exempted from MLTC Individuals aged 18 through 20 who are nursing home certifiable and require more than 120 days of community based long term care services Native Americans Individuals who are eligible for the Medicaid buy in for the working disabled and are nursing home certifiable - Home and Community Based Services Expansion Program (HCBS Expansion). This component provides home and community-based services similar to those provided under the state´s section 1915(c) HCBS waivers (Nursing Home Transition and Diversion Program/NHTD, and Traumatic Brain Injury Program/TBI) to certain medically needy individuals. These services enable these individuals to live at home with appropriate supports rather than in a nursing facility. See Attachment C for HCBS Expansion services. All HCBS Expansion individuals will be transitioned as appropriate to MLTC.
- Eligibility for the HCBS Expansion. This group, identified as Demonstration Population 9/HCBS Expansion, includes married medically needy individuals2:
- who meet a nursing home level of care;
- whose spouse lives in the community; and
- who would be income-eligible for Medicaid services in the community but for the application of the spousal impoverishment eligibility and post-eligibility rules of section 1924 of the Act.
- HARP: This component provides integrated Medicaid covered services and services specifically to address the needs of individuals with a SMI and SUD conditions under the demonstration. Members enrolled in the Health and Recovery Plans described below may elect to remain enrolled in mainstream MCOs. Within the HARPs, a benefit package of BH HCBS and Community Oriented Recovery and Empowerment (CORE) Services are provided, in addition to the existing MMMC benefit package (excluding long term nursing facility services). See Attachment B for a listing of BH HCBS and CORE Services.
- Eligibility for HARP. Eligible individuals include Medicaid adult beneficiaries age 21 or over eligible for Medicaid furnished in MMMC under the demonstration with a specified SMI and/or serious SUD diagnosis and who meet categorical criteria or risk factors specified by New York's Office of Mental Health (OMH) or New York's Office of Addiction Services and Supports (OASAS) identified by a:
- review of behavioral health service utilization, or
- receipt of a qualifying score on a state-approved assessment tool.
- 4.4 Population-Specific Program Requirements
- MMMC Enrollment of Individuals Living with HIV. The state is authorized to require individuals living with HIV to receive benefits through MMMC. Individuals living with HIV will have 30 days in which to select a health plan. If no selection is made, the individual will be auto-assigned to an MCO. Individuals living with HIV who are enrolled in an MCO (voluntarily or by default) may request transfer to an HIV SNP at any time if one or more HIV SNPs are in operation in the individual's district. Further, transfers between HIV SNPs will be permitted at any time. Individuals in HIV SNPs will be eligible for BH HCBS if meeting the targeting, risk and functional needs requirements for BH HCBS. Individuals in HIV SNPs will be eligible for CORE if they otherwise would meet HARP eligibility criteria. HIV SNPs will meet all requirements of MMMC plans providing LTSS as well as HARP plans relating to delivery of BH HCBS and CORE.
- Restricted Recipient Programs. The state may require individuals participating in a restricted recipient program administered under 42 CFR 431.54(e) to enroll in MMMC or MLTC. Furthermore, MCOs may establish and administer restricted recipient programs, through which they identify individuals that have utilized Medicaid services at a frequency or amount that is not medically necessary, as determined in accordance with utilization guidelines established by the state, and restrict them for a reasonable period of time to obtain Medicaid services from designated providers only. The state must adhere to the following terms and conditions in this regard.
- Restricted recipient programs operated by MCOs must adhere to the requirements in 42 CFR 431.54(e) (1) through (3), including the right to a hearing conducted by the state.
- The state must require MCOs to report to the state whenever they want to place a new person in a restricted recipient program. The state must maintain summary statistics on the numbers of individuals placed in restricted recipient programs, and the reasons for those placements, and must provide the information to CMS upon request.
- Individuals Moved from Institutional Settings to Community Settings for Long Term Services and Supports. Individuals discharged from a nursing facility who enroll into or remain enrolled in the MLTC program in order to receive community based long term services and supports or who move from an adult home as defined in subdivision 25 of section 2 of the social services law, to the community and, if applicable, enroll into the MLTC program, are eligible based on a special income standard. The special income standard is also available to MLTC members who were enrolled in the program as a result of the mandatory Nursing Facility transition, and subsequently able to be discharged to the community from the nursing facility, with the services of MLTC program in place. For married individuals who meet the criteria to be considered an "institutionalized spouse," spousal impoverishment rules shall apply. Eligibility is not based on the special income standard for individuals subject to spousal impoverishment rules. The special income standard will be determined by utilizing the average Department of Housing and Urban Development (HUD) Fair Market Rent (FMR) dollar amounts for each of the seven regions in the state, and subtracting from that average, 30 percent of the Medicaid income level (as calculated for a household of one) that is considered available for housing. The seven regions of the state include: Central, Northeastern, Western, Northern Metropolitan, New York City, Long Island and Rochester.
The state shall work with Nursing Home Administrators, nursing home discharge planning staff, family members and the MLTC health plans to identify individuals who may qualify for the housing disregard as they are able to be discharged from a nursing facility back into the community and remain enrolled in or newly enrolled into the MLTC program.
Enrollees receiving community based long term services and supports must be provided with nursing facility coverage through managed care, if nursing facility care is needed for 120 days or less and there is an expectation that the enrollee will return to community-based settings. During the short-term nursing facility stay, the state must retain the enrollees' community maintenance needs allowance. In addition, the state will ensure that the MLTC MCOs work with individuals, their families, nursing home administrators, and discharge planners to help plan for the individual's move back into the community, as well as to help plan for the individual's medical care once he/she has successfully moved into his/her home. For dually eligible enrollees, the MCO is responsible for implementing and monitoring the plan of care between Medicare and Medicaid. The MCO must assure the services are available to the enrollee.- Continuous Eligibility Period
- Duration. The state is authorized to provide a 12-month continuous eligibility period to the groups of individuals specified in Table 6, regardless of the delivery system through which they receive Medicaid benefits. Each newly eligible individual's 12-month period shall begin at the initial determination of eligibility; for those individuals who are re-determined eligible consistent with Medicaid state plan rules, the 12-month period begins at that point. At each annual eligibility redetermination thereafter, if an individual is re-determined eligible under the Medicaid state plan the individual is guaranteed a subsequent 12-month continuous eligibility period. 12-month continuous eligibility is also authorized for the Adult Group under section 1902(a)(10)(A)(i)(VIII) of the Act.
- Exceptions. Notwithstanding subparagraph (a), if any of the following circumstances occur during an individual's 12-month continuous eligibility period, the individual's Medicaid eligibility shall be terminated, suspended or re-determined:
- The individual cannot be located;
- The individual is no longer a New York State resident;
- The individual requests termination of eligibility;
- The individual dies;
- The individual fails to provide, or cooperate in obtaining a Social Security Number, if otherwise required;
- The individual provided an incorrect or fraudulent Social Security Number;
- The individual was determined eligible for Medicaid in error;
- The individual is receiving treatment in a setting where Medicaid eligibility is not available (e.g. institution for mental disease);
- The individual is receiving care, services or other supplies under a section 1915 waiver;
- The individual was previously otherwise qualified for emergency medical assistance benefits only, based on immigration status, but is no longer qualified because the emergency has been resolved;
- The individual fails to provide the documentation of citizenship or immigration status required under federal law;
- The individual is incarcerated;
- The individual turns 65 years of age and is no longer eligible for the Adult Group;
- The individual policy holder fails to provide documentation of third-party health insurance.
Table 6: Groups Eligible for a 12 Month Continuous Eligibility Period State Plan Mandatory and Optional Groups Statutory or Regulatory Reference Individuals determined eligible as pregnant women 42 CFR § 435.116 Individuals determined eligible as the Adult Group 42 CFR § 435.119 Individuals determined eligible as parents or other caretaker relatives 42 CFR § 435.110 Low-income families, except for children § 1931 of the SSA 5. DEMONSTRATION BENEFITS AND ENROLLMENT
- 5.1 Alternative Benefit Plan. The Affordable Care Act Adult Group will receive benefits provided through the state's approved Alternative Benefit Plan (ABP) SPA.
- 5.2 Demonstration Benefits. The following benefits are provided through the indicated delivery system to individuals eligible for the Medicaid managed care components of the demonstration:
- MMMC. State plan and demonstration benefits are delivered through MCOs with the exception of certain services carved out of the MMMC contract and delivered directly by the state on a fee-for-service basis. All MMMC benefits (regardless of delivery method), as well as the co-payments charged to MMMC recipients. In addition to state plan benefits, there are three demonstration services provided only to all enrollees in MMMC under the demonstration.
- Cost Sharing for MMMC. MMMC beneficiaries including HARPs and HIV-SNPs, who are not otherwise exempt from cost sharing consistent with 447.56(a)(1), will be charged drug copays that are approved in the Medicaid state plan. MMMC beneficiaries will not be subject to any non-drug copays that are described in the Medicaid state plan.
- Children's HCBS. MMMC plans will provide HCBS for children not otherwise excluded or exempted from MMMC under the concurrent authority of the 1915(c) Children's waiver and this 1115 demonstration. Independent assessments and person-centered services planning for HCBS under the Children's waiver will be conducted by a State Plan Health Home provider or the state's Independent Entity as described and included in the approved Children's waiver. All HCBS benefits are listed in the approved Children's waiver or the approved State Plan for Community First Choice Option (CFCO). All reimbursement for Children's Waiver HCBS will be non-risk for the first 24 months subject to the non-risk UPL at 42 CFR 447.362. The MCO must pay the FFS fee schedule for non-risk services as long as the HCBS are non-risk (i.e., 24 months). There are no co-payments for Children's waiver services.
- Managed Long Term Care. State plan benefits are delivered through MCOs or, in certain districts, prepaid inpatient health plans, with the exception of certain services carved out of the MLTC contract and delivered directly by the state on a fee-for-service basis.
- For those individuals receiving a nursing home benefit in the partially capitated MLTC plan they will be limited to three months for those enrollees who have been designated as LTNHS in a skilled nursing or residential health care facility as of the effective date of this amendment. After three months the individual will be involuntarily disenrolled from the partially capitated MLTC plan and payment for nursing home services will be covered by Medicaid fee for service for individuals who qualify for institutional Medicaid coverage.
- Should an individual prefer discharge–and an assessment of the individual's medical needs indicates they may be safely discharged to the community–they may remain enrolled in their MLTC plan, while residing in the nursing home on a temporary basis for more than three months, until their discharge plans are resolved, and the individual is transitioned out of the nursing home.
- Health and Recovery Plans (HARP). State plan and demonstration benefits that are identical to MMMC with an additional component that provides BH HCBS and CORE for SMI and SUD needs will be provided by the HARPs. Long term care services (in excess of 120 days) or permanent placement in a Nursing facility, however, are not provided by HARPs. There are no co-payments for HARP services. All BH HCBS and CORE benefits are listed in Attachment B. CORE Services for HARP enrollees and BH HCBS for HARP enrollees meeting targeting, risk, and need-based functional criteria are only provided under the demonstration. The state must update the Medicaid state plan for rehabilitation and other mental health and substance use disorder services as identified through a companion letter to TN 10-38 as well as substance use disorder demonstration services not described in the current state plan. HIV SNPs also provide CORE to enrollees meeting HARP eligibility criteria and BH HCBS to enrollees meeting targeting, risk, and need-based criteria. The state will adhere to all state plan requirements pertaining to comparability. Below is a table showing how the state defines its services under CORE, and how this compares to services under BH HCBS.
Table 7 - BH HCBS and CORE Existing BH HCBS before CORE Service Crosswalk after CORE Transition BH HCBS Community Psychiatric Support & Treatment (CPST) CORE Community Psychiatric Support & Treatment (CPST) BH HCBS Family Support and Training (FST) CORE Family Support and Training (FST) BH HCBS Empowerment Services – Peer Support CORE Empowerment Services – Peer Support BH HCBS Psychosocial Rehabilitation (PSR) CORE Psychosocial Rehabilitation (PSR) BH HCBS Short-Term Crisis Respite Crisis Intervention, including Short-Term Crisis Respite – already available to all Medicaid managed care recipients BH HCBS Intensive Crisis Respite Crisis Intervention, including Intensive Crisis Respite – already available to all Medicaid managed care recipients BH HCBS Education Support Services No change BH HCBS Pre-Vocational Services No change BH HCBS Transitional Employment No change BH HCBS Intensive Supported Employment No change BH HCBS Ongoing Supported Employment No change BH HCBS Habilitation No change BH HCBS Non-Medical Transportation No change
- HARPs Services Tiers. HARP enrollees receive BH HCBS services under the following tier structure in accordance with their person-centered plan of care. HARP enrollees are permitted to appeal any service denial decisions.
- Tier 1 BH HCBS services include:
- Employment supports
- Education supports
- Tier 2 includes all Tier 1 BH HCBS services plus additional services as specified in Attachment J to individuals whose medical need surpasses the need for Tier 1 services.
- HARPs Services Utilization Thresholds. The following thresholds will limit coverage of HARPs-specific services for individual HARPs enrollees. These limits will not affect state plan or other demonstration benefits. The state will track and report overall utilization, including any utilization threshold exceeded for clinical reasons, to ensure cost containment as well as compile sufficient fee for service data to submit HARPs capitation rates to CMS for approval.
- Tier 1 -- Threshold of $8,000 per person, per 12-month period. Up to $10,000 in services are permitted. For ROS, the thresholds will be adjusted to reflect the HCBS rate differentials.
- Tier 2 -- Threshold of $16,000 per person, per 12-month period. Up to $20,000 in services are permitted. For ROS, the thresholds will be adjusted to reflect the HCBS rate differentials.
- Self-Direction Pilot. The Self-direction Demonstration will be available to HARP and HIV/SNP enrollees eligible for receiving BH HCBS services or children meeting the target criteria of the Children's waiver and receiving HCBS under the Children's waiver through MMMC. The program will be in effect from January 1, 2017, through March 31, 2027. It will include 8 pilot sites phased in over the demonstration.
- Voluntary Enrollment and Disenrollment from Self-Direction Pilot. Participation in the Self-Direction pilot is voluntary, and participants may opt out at any time.
- Enrollee Notification. The state must notify eligible enrollees about the option to self-direct services. The state must develop a waiting list for enrollees who wish to participate in the pilot should the demand exceed capacity.
- Choice of Providers. Self-direction pilot participants will have a choice of support broker within the service center. Each participant should have the choice of provider and location for self-directed services, except as noted in 5.2(c)(iii)(5) below.
- Services Eligible for Self-Direction: This pilot includes all behavioral health HCBS services offered by HARPs and HIV SNPs and Individual Directed Goods and Services (IDGS) detailed in Attachment D. Children meeting targeting criteria of the 1915(c) Children's waiver and receiving HCBS through MMMC are eligible to self-direct up to $2,000 in IDGS only using a Fiscal Management Services provider within the service center. Each participant will have the choice of provider and location for IDGS. Children's IDGS should be used as the funding source of last resort - only for those costs that cannot be covered by any other source and that are vital to the implementation of the POC. Individual Directed Goods and Services are services, equipment, or supplies not otherwise provided through this waiver, the 1915(c) Children's Waiver, or through the Medicaid State Plan that address an identified need in the service plan. The item or service must be identified in the service plan and either:
- decrease the need for other Medicaid services;
- promote inclusion in the community; or
- increase the participant's safety in the home environment.
- To be an eligible service:
- the participant must lack funds to purchase the item or service; and
- the service is not available through another source.
- Services Ineligible for Self-Direction: Individual goods and services that are not eligible are listed below.
- Experimental or prohibited treatments;
- Purchases for or from third parties who are family members, friends, or significant others aside from family or social functions that promote social inclusion and are incorporated in the service plan;
- Room and Board in a residential facility, including assisted living facilities;
- Tobacco products, alcohol products, firearms, contraband or illegal items;
- Pornographic materials, prostitution services, escort services;
- Payment of court-ordered costs, attorney fees, fines, restitution, or similar debts;
- Credit card payments of any kind, or similar debts;
- Items purchased for the purpose of resale;
- Gift cards or prepaid debit cards;
- Services or goods that are recreational in nature;
- Goods and services not in the service plan or related to a recovery goal, or that is solely for recreation that a household does not include a person with a disability would be expected to pay for as a household expense (e.g. subscription to a cable television service).
- Evaluation. The state shall follow the evaluation requirements specified in Section 17 below.
- Reporting. Information from the pilot must be incorporated into the quarterly and annual reports detailed in STC 14.7.
- Protocols. Payment and operational protocols must be submitted by New York to CMS within 120 days of award.
- 5.3 Home and Community Settings Qualities. Enrollees receiving Medicaid HCBS and LTSS services furnished through the 1115 demonstration, including individuals who receive services under the demonstration´s HCBS Expansion program, MMMC and HARP, including HIV SNP, must receive services in residential and non-residential settings located in the community, which meet CMS standards for HCBS settings as articulated in current 1915(c) policy, including regulations at 42 CFR §441.301. The Statewide Transition Plan must include HARPs BH HCBS settings and meet CMS approval for required settings to be funded beyond November 30, 2015. A full list of home and community-based qualities are provided in Attachment C.
- 5.4 Individuals Provided with LTSS under the Demonstration. The state is authorized to require certain individuals using long-term services and supports to enroll in either Mainstream Medicaid Managed Care, or Managed Long-Term Care as identified in Section I. Once these individuals are enrolled in managed care, the state is required to provide the following protections for the population.3
- 5.5 Person Centered Service Planning. All individuals utilizing long-term services and supports will have a person-centered individual service plan maintained at the MCO. Person-centered planning includes consideration of the current and unique psycho-social and medical needs and history of the enrollee, as well as the person´s functional level, and support systems. The person-centered plan is developed by the enrollee with the assistance of the MCO and individuals the enrollee chooses to include.
When a service provider is an approved State Plan Health Home4 provider and also a HCBS provider, this entity may conduct person-centered service planning, care coordination, and provision of HCBS provision as long as firewalls are constructed between the service planning, care coordination, and service provision. A home and community-based service provider who is not also an approved State Plan Health Home provider may not conduct person-centered service planning with individuals who they also provide HCBS, unless that service provider is the only qualified and willing entity available to conduct the service planning. If a service provider is the only willing and qualified entity to conduct service planning, the state must require such provider to establish firewalls between the service provision and planning functions. The person-centered plan is developed in accordance with 42 CFR §441.301(c)(4)(F)(1) through (8).
- Health home program will have administrative safeguards in place when providing person-centered planning and care coordination and services that have transitioned from 1915(c) waivers to eligible health home individuals. In addition, the state agrees to meet all health home requirements including reporting annually on quality and utilization measures.
- 5.6 Verification of MLTC Plan Enrollment. The state shall implement a process for MLTC plans, network and non-network providers for the state to confirm enrollment of enrollees who do not have an enrollee identification card or seek services from a provider before developing a person-centered service plan.
- 5.7 Health and Welfare of Enrollees. The state shall ensure a system is in place to identify, address, and seek to prevent instances of abuse, neglect, and exploitation of its enrollees on a continuous basis. This should include provisions such as critical incident monitoring and reporting to the state, investigations of any incident including, but not limited to, wrongful death, restraints, or medication errors that resulted in an injury. In each quarterly report, the state will provide information regarding any such incidents by plan. The state will also ensure that children and adults receiving MLTC or LTSS are afforded linkages to child and/or adult protective services through all service entities, including the MCOs.
- 5.8 Maintaining Accurate Beneficiary Address. New York will complete return mail tracking for enrollment notification mailings. The state will use information gained from returned mail to make additional outreach attempt through other methods (phone, email, analysis of prior claims, etc.).
- 5.9 Network of Qualified Providers. The provider credentialing criteria described at 42 CFR §438.214 must apply to all providers participating in the state´s Medicaid managed care and managed long-term care programs. To the extent possible, the MCO shall incorporate criminal background checks, reviewing abuse registries as well as any other mechanism the state includes within the MCO contract.
- 5.10 MMMC or MLTC Enrollment and Transition of Care Period. For initial transitions into MLTC or MMMC from fee-for-service, each enrollee receiving community-based LTSS must continue to receive services under the enrollee´s pre-existing service plan for at least 90 days after enrollment or until a care assessment has been completed. Any reduction, suspension, denial or termination of previously authorized services shall trigger the required notice under 42 CFR § 438.404 and applicable appeal rights.
- 5.11 Option for Consumer Directed Personal Assistance Program (CDPAP). Enrollees shall have the option to elect self-direction of Personal Assistance under the MMMC program. The state shall ensure through its contracts with the MCOs that enrollees are afforded the option to select self-direction and enrollees are informed of CDPAP as a voluntary option. Individuals who select self-direction must have the opportunity to have choice and control over how services are provided and who provides the service, except as noted in STC 2(E) of this section.
- 5.12 Information and Assistance in Support of Participant Direction. The state/MCO shall have a support system that provides participants with information, training, counseling, and assistance, as needed or desired by each participant, to assist the participant to effectively direct and manage their self-directed services. Participants shall be informed about self-directed care, including feasible alternatives, before electing the self-direction option.
- 5.13 Participant Direction by Representative. The participant who self-directs the personal care service may appoint a volunteer designated representative to assist with or perform employer responsibilities to the extent approved by the participant. Services may be directed by a legal representative of the participant. Consumer-directed services may be directed by a non-legal representative freely chosen by the participant. A person who serves as a representative of a participant for the purpose of directing services cannot serve as a provider of personal attendant services for that participant.
- 5.14 Participant Employer Authority. The participant (or the participant´s representative) must have decision making authority over workers who provide personal care services.
- Participant. The participant (or the participant´s representative) provides training, supervision and oversight to the worker who provides services. A Fiscal/Employer Agent that follows IRS and local tax code laws functions as the participant´s agent in performing payroll and other employer responsibilities that are required by federal and state law.
- Decision-Making Authorities. The participants exercise the following decision-making authorities: recruit staff, hire staff, verify staff´s ability to perform identified tasks, schedule staff, evaluate staff performance, verify time worked by staff and approve time sheets, and discharge staff.
- Disenrollment from Self-Direction. A participant may voluntarily disenroll from the self-directed option at any time and return to a traditional service delivery system through the MMMC, or MLTC program. To the extent possible, the member shall provide his/her intent to withdraw from participant direction. A participant may also be involuntarily disenrolled from the self-directed option if continued participation in the consumer-directed services option would not permit the participant´s health, safety, or welfare needs to be met, or the participant demonstrates the inability to self-direct by consistently demonstrating a lack of ability to carry out the tasks needed to self-direct services, or if there is fraudulent use of funds such as substantial evidence that a participant has falsified documents related to participant-directed services. If a participant is terminated voluntarily or involuntarily from the self-directed service delivery option, the MCO must transition the participant to the traditional agency direction option and must have safeguards in place to ensure continuity of services.
- Payment for Services Will be Made Following the Service Being Rendered and only upon receipt of an acceptable receipt, invoice or signed and approved timesheet, as applicable.
- Appeals. The following actions shall be considered adverse action under both 42 CFR §431 subpart E and 42 CFR §438 subpart F:
- a reduction, suspension or termination of authorized CDPAP services;
- A denial of a request to change Consumer Directed Personal Assistance Program services.
- 5.15 Adding Services to the MMMC, and/or MLTC Plan Benefit Package. At any point in time the state intends to add to either the MMMC, or MLTC plan benefit package currently authorized state plan or demonstration services that have been provided on a fee-for-service basis, the state must provide CMCS, Disabled and Elderly Health Programs Group, Division of Managed Care Plans (DMCP) the following information, with at least 30 days´ notice prior to the inclusion of the benefit, in writing:
- A description of the benefit being added to the benefit package;
- A detailed description of the state´s oversight of the MCO´s readiness to administer the benefit including:
- readiness and implementation of activities, including onsite reviews, phone meetings and desk audits that review policies and procedures for new services;
- data sharing to allow plans to create services plans as appropriate;
- process to communicate the change to enrollees;
- MCO network development to include providers of that service; and
- any other activity performed by the state to ensure plan readiness.
- Information concerning the changes being made to the MMMC and/or MLTC contract provisions and capitation payment rates in accordance with STC 2 in Section VI.
- DMCP reserves the right to delay implementation of the benefit transition until such time as appropriate documentation is provided showing evidence of MCO readiness. In addition, new services that are not currently authorized under the state plan or demonstration may be added only through approved amendments to the state plan or demonstration.
- DMCP will notify the state of concerns within 10 days of receiving the state´s written notice of the change. If no comments are received, the state may proceed with the scheduled benefit transition.
- 5.16 Adding Populations to MMMC and/or MLTC Enrollment. Any time the state is ready to expand mandatory MMMC and /or MLTC plan enrollment into a new Medicaid population, the state must submit an 1115 amendment in accordance with STC 7 in Section III. The amendment request must include the following:
- a description of the population and the list of the counties that will have populations moving to mandatory enrollment;
- a list of MCO with an approved state certificate of authority to operate in those counties demonstrating that enrollees will be afforded choice of plan that will be providing services;
- confirmation that the MCO have met the network requirements in STC 10 in Section VI for each MCO; and
- an analysis of why the most appropriate authority to implement mandatory MMMC and/or MLTC for the new population, i.e. what the state is demonstrating by implementing the change to the demonstration.
- 5.17 Assurances During LTSS Expansion for MMMC, HIV SNP, and HARP Enrollees. To provide and demonstrate seamless transitions for enrollees, the state must (where applicable):
- Send sample notification letters. Existing Medicaid providers must receive sample beneficiary notification letters via widely distributed methods (mail, email, provider website, etc.) so that providers are informed of the information received by enrollees regarding their managed care transition.
- Provide continued comprehensive outreach, including educational tours for enrollees and providers. The educational tour should educate enrollees and providers regarding plan enrollment options, rights and responsibilities and other important program elements. The state must provide webinars, meeting plans, and send notices through outreach and other social media (e.g. state´s website). The enrollment broker, choice counseling entities, ombudsman and any group providing enrollment support must participate.
- Operate a call center independent of the MLTC, and MMMC, HIV SNP, and HARP plans. This entity must be able to help enrollees in making independent decisions about plan choice and be able to document complaints about the plans. During the first 60 days of implementation the state must review all call center response statistics to ensure all contracted plans are meeting requirements in their contracts. After the first 60 days, if all entities are consistently meeting contractual requirements the state can decrease the frequency of the review of call center statistics, but no more than 120 days should elapse between reviews.
- Review the outcomes of the auto-assignment algorithm to ensure that MLTC and MMMC plans with more limited networks do not receive the same or larger number of enrollees as plans with larger networks.
- Require MCO to maintain the current worker/recipient relationship for no less than 90 days.
- 5.18 Assessment of LTSS needs for MLTC, and MMMC and Behavioral Health Assessments for HARPs and HIV SNPs. LT SS needs assessments must be conflict free plans will not complete any LTSS needs assessments for individuals requesting such services prior to enrollment in a plan. Non-dually eligible individuals requesting LT SS will be assessed for criteria necessitating enrollment in MLTC or an alternate waiver program. An independent LT SS assessment must be in place in any geographic location where MLTC or, LT SS in MMMC will be mandated. An independent BH HCBS assessment system must be in place in any geographic location where HARP enrollment is an option for eligible individuals. LT SS assessments for skilled nursing facility services in MMMC, and BH HCBS assessments of enrollees aged 21 and over for HARPs and HIV SNPs will be conflict free prior to implementation and geographic phase in.
- 5.19 Post Assessment Education. New Medicaid applicants must be provided the results of their assessment and educated on the steps in the Medicaid eligibility determination, including denial and fair hearing procedures. Individuals who are currently Medicaid eligible must be provided information regarding choice of plan.
- 5.20 Operation of the HCBS Expansion Program. The individuals eligible for this component of the demonstration will receive the same HCBS as those individuals determined eligible for and enrolled in the state´s Nursing Home Transition and Diversion Program (NHTDP) and Traumatic Brain Injury Program (TBIP) authorized under section 1915(c) of the Act. The specific benefits provided to participants in this program are listed in Attachment C. The state will operate the HCBS Expansion program in a manner consistent with approved NHTDP and TBIP 1915(c) waiver programs and must comply with all administrative, operational, quality improvement and reporting requirements contained therein. The state shall provide enrollment and financial information about the individuals enrolled in the HCBS Expansion program.
- 5.21 Facilitated Enrollment. Facilitated enrollers, which may include MCOs, health care providers, community-based organizations, and other entities under state contract, will engage in those activities described in 42 CFR § 435.904(d)(2), as permitted by 42 CFR §435.904(e)(3)(ii), within the following parameters:
- Facilitated enrollers will provide program information to applicants and interested individuals as described in 42 CFR §435.905(a).
- Facilitated enrollers must afford any interested individual the opportunity to apply for Medicaid without delay as required by 42 CFR §435.906.
- If an interested individual applies for Medicaid by completing the information required under 42 CFR §435.907(a) and (b) and 42 CFR §435.910(a) and signing a Medicaid application, that application must be transmitted to New York State Department of Health for determination of eligibility.
- The protocols for facilitated enrollment practices between the state and the facilitated enrollers must:
- ensure that choice counseling activities are closely monitored to minimize adverse risk selection; and
- Specify that determinations of Medicaid eligibility are made solely by the Medicaid agency or its designee.
- 5.22 Passive Enrollment. For any component that requires passive enrollment of potential enrollees, individuals must have the ability to "opt out" Where the notice is sent 30 days in advance of the passive enrollment. The individual may opt out at any time after receipt of the notice and within the first 90 days following the passive enrollment. The individual may also change after the 12-month lock-in period at any time. Enrollees who enrolled through the health exchange or the local social services district in an MMMC plan whose MCO also operates a HARP line of business will be passively enrolled with the ability to opt-out within the first 90 days following passive enrollment and return to their original MMMC plan. Following the 90 day opt out period, HARP enrollees may not change plans again until the remainder of the twelve-month lock-in period has lapsed. HARP eligible enrollees in an MMMC plan who´s MCO does not operate a HARP line of business will be allowed to voluntarily enroll in a HARP. The enrollee must be given the choice of HARPs available for enrollment and the current plan must assist the enrollee in transferring to the HARP. The state will notify CMS and the public at least 60 days before exercising the option to modify needs-based eligibility criteria. When a HARP enrollee leaves the HARP and transfers into another plan, care must be coordinated for physical and behavioral health during the transition to best meet the needs of the enrollee. The current and new plans must work together when an enrollee transfers to another plan.
- 5.23 HCBS Electronic Visit Verification System. The state will demonstrate compliance with the Electronic Visit Verification System (EVV) requirements for personal care services (PCS) by January 1, 2020 and home health services by January 1, 2023 in accordance with section 12006 of the 21st Century CURES Act.
- 5.24 HCBS Quality Systems and Strategy. The state is expected to implement systems that measure and improve its performance to meet the waiver assurances set forth in 42 CFR and 441.302. The Quality Review provides a comprehensive assessment of the state´s capacity to ensure adequate program oversight, detect and remediate compliance issues and evaluate the effectiveness of implemented quality improvement activities.
- 5.25 For 1915(c)-Approvable HCBS, for services that could have been authorized to individuals served under a 1915(c) waiver, the state must have an approved Quality Improvement Strategy and is required to develop and measure performance indicators for the following waiver assurances:
- Administrative Authority: A performance measure should be developed and tracked any authority that the State Medicaid Agency (SMA) delegates to another agency, unless already captured in another performance measure.
- Level of Care: Performance measures are required for the following two sub-assurances: applicants with reasonable likelihood of needing services receive a level of care determination and the processes for determining level of care are followed as documented. While a performance measure for annual levels of care is not required to be reported, the state is expected to be sure that annual levels of care are determined.
- Qualified Providers: The state must have performance measures that track that providers meet licensure/certification standards, that non-certified providers are monitored to assure adherence to waiver requirements, and that the state verifies that training is given to providers in accordance with the waiver.
- Service Plan: The state must demonstrate it has designed and implemented an effective system for reviewing the adequacy of service plans for HCBS participants. Performance measures are required for choice of waiver services and providers, service plans address all assessed needs and personal goals, and services are delivered in accordance with the service plan including the type, scope, amount, duration, and frequency specified in the service plan.
- Health and Welfare: The state must demonstrate it has designed and implemented an effective system for assuring HCBS participants health and welfare. The state must have performance measures that track that on an ongoing basis it identifies, addresses and seeks to prevent instances of abuse, neglect, exploitation and unexplained death; that an incident management system is in place that effectively resolves incidents and prevents further singular incidents to the extent possible; that state policies and procedures for the use or prohibition of restrictive interventions are followed; and, that the state establishes overall health care standards and monitors those standards based on the responsibility of the service provider as stated in the approved waiver.
- Financial Accountability: The state must demonstrate that it has designed and implemented an adequate system for insuring financial accountability of the HCBS program. The state must have performance measures that track that it provides evidence that claims are coded and paid for in accordance for services rendered, and that it provides evidence that rates remain consistent with the approved rate methodology throughout the five-year waiver cycle.
- The state will submit a report to CMS which includes evidence on the status of the HCBS quality assurances and measures that adheres to the requirements outlined in the March 12, 2014, CMS Informational Bulletin, Modifications to Quality Measures and Reporting in §1915(c) Home and Community-Based Waivers. (1915(c) and 1915(i) HCBS). NOTE: This information could be captured in the 1115 Summary report detailed in section VIII.
- 5.26 The state must report annually the deficiencies found during the monitoring and evaluation of the HCBS waiver assurances, an explanation of how these deficiencies have been or are being corrected, as well as the steps that have been taken to ensure that these deficiencies do not reoccur. The state must also report on the number of substantiated instances of abuse, neglect, exploitation and/or death, the actions taken regarding the incidents and how they were resolved. Submission is due no later than 6 months following the end of the demonstration year. NOTE: This information could be included in the annual reports submitted for 1115 waivers detailed in section VIII.
- 5.27 For 1915(i)-Approvable HCBS, for services that could have been authorized to individuals served under a 1915(i) waiver, the state must have an approved Quality Improvement Strategy and is required to develop performance measures to address the following requirements:
- Service plans that:
- address assessed needs of 1915(i) participants;
- are updated annually; and
- document choice of services and providers.
- Eligibility Requirements: The state will ensure that:
- an evaluation for 1915(i) State plan HCBS eligibility is provided to all applicants for whom there is reasonable indication that 1915(i) services may be needed in the future;
- the processes and instruments described in the approved program for determining 1915(i) eligibility are applied appropriately; and
- the 1915(i) benefit eligibility of enrolled individuals is reevaluated at least annually (end of demonstration year) or if more frequent, as specified in the approved program.
- Providers meet required qualifications.
- Settings meet the home and community-based setting requirements as specified in the benefit and in accordance with 42 CFR 441.710(a)(1) and (2).
- The SMA retains authority and responsibility for program operations and oversight.
- The SMA maintains financial accountability through payment of claims for services that are authorized and furnished to 1915(i) participants by qualified providers.
- The state identifies, addresses, and seeks to prevent incidents of abuse, neglect, and exploitation.
- The state must also describe the process for systems improvement as a result of aggregated discovery and remediation activities.
- 5.28 Person-centered planning. The state assures there is a person-centered service plan for each individual determined to be eligible for HCBS. The person-centered service plan is developed using a person-centered service planning process in accordance with 42 CFR 441.301(c)(1) (1915(c)) or 42 CFR 441.725(c) (1915(i)), and the written person-centered service plan meets federal requirements at 42 CFR 441.301(c)(2) (1915(c)) or 42 CFR 441.725(b) (1915(i)). The person-centered service plan is reviewed and revised upon reassessment of functional need as required by 42 CFR 441.365(e), at least every 12-months, when the individual´s circumstances or needs change significantly, or at the request of the individual.
- 5.29 Conflict of Interest: The state agrees that the entity that authorizes the services is external to the agency or agencies that provide the HCB services. The state also agrees that appropriate separation of assessment, treatment planning and service provision functions are incorporated into the state´s conflict of interest policies except for as stated in section V, STC 4(a).
- Each beneficiary eligible for long-term services and supports will have informed choice on their option to self-direct LTSS, have a designated representative direct LTSS on their behalf, or select traditional agency-based service delivery. Both level of care and person-centered service planning personnel will receive training on these options. (MLTSS with self-direction)
- The state, either directly or through its MCO contracts must ensure that participants´ engagement and community participation is supported to the fullest extent desired by each participant. (MLTSS)
- The state will assure compliance with the characteristics of HCBS settings as described in 1915(c) and 1915(i) regulations in accordance with implementation/effective dates as published in the Federal Register.
- Beneficiaries may change managed care plans if their residential or employment support provider is no longer available through their current plan. (MLTSS)
6. HEALTH-RELATED SOCIAL NEEDS (HRSN) SERVICES
- 6.1 HRSN Services. The state may claim FFP for expenditures for certain qualifying HRSN services identified in Attachment J and this STC, subject to the restrictions described below, including STC 7. HRSN will be delivered by social service providers in cooperation with Social Care Networks (SCN), which are contracted entities in each of the state's nine regions that will provide HRSN screening and referral services to otherwise eligible Medicaid beneficiaries that are targeted populations for HRSN services. Expenditures are limited to expenditures for items and services not otherwise covered under title XIX, but consistent with Medicaid demonstration objectives that enable the state to continue to increase the efficiency and quality of care. HRSN services must be clinically appropriate for the beneficiary and based on medical appropriateness using clinical and other health related-social needs criteria; such HRSN services must have a reasonable expectation of improving or maintaining the health or overall function of the beneficiary. The state is required to align clinical and health-related social criteria across services and with other non-Medicaid social support agencies, to the extent possible. The HRSN services may not supplant any other available funding sources such as housing or nutrition supports available to the beneficiary through local, state, or federal programs. The HRSN services will be the choice of the beneficiary; a beneficiary can opt out of HRSN services at any time; and the HRSN services do not absolve the state or its managed care plans of their responsibilities to provide required coverage for other medically necessary services. Under no circumstances will the state be permitted to condition Medicaid coverage, or coverage of any benefit or service, on receipt of HRSN services. The state must submit additional details on covered services as outlined in STC 6.8 (Service Delivery) and Attachment J.
- 6.2 Allowable HRSN Services. The state may cover the following HRSN services:
- Housing supports, including:
- Medically necessary air conditioners, humidifiers, air filtration devices and asthma remediation, and refrigeration units as needed for medical treatment.
- Medically necessary home modifications and remediation services such as accessibility ramps, handrails, grab bars, repairing or improving ventilation systems, and mold/pest remediation.
- Recuperative care and short-term pre-procedure and post-hospitalization housing for individuals experiencing homelessness, or involving a lower-intensity care setting for individuals who would otherwise lack a safe option for discharge or recovery or who would require a hospital stay. Additional requirements for this service are listed in STC 6.3.
- Rent/ temporary housing for up to 6 months for the demonstration period. Limited to individuals transitioning out of institutional care/congregate settings or individuals who are homeless, such as nursing facilities, large group homes, congregate residential settings, IMDs, correctional facilities, and acute care hospitals; individuals who are Medicaid high utilizers who are homeless as defined by 24 CFR 91.5; and youth transitioning out of the child welfare system including foster care.
- Utility costs for individuals receiving rent/temporary housing, for up to 6 months for the demonstration period, including activation expenses and back payments to secure utilities, limited to individuals receiving rent/temporary housing as described in STC 6.2(a)(iv).
- Pre-tenancy services.
- Assistance with navigating the complexities of the housing application process through the progression of prospective tenant to tenant such as supporting the beneficiary when undergoing tenant screening, completing rental applications, negotiating lease agreements, and preparing for and attending tenant interviews.
- Assistance with the housing search and application process, including contacting prospective housing options for availability and information, as well as researching the availability of rental assistance.
- Tenancy sustaining services, including tenant rights education and eviction prevention.
- Assistance in linking beneficiaries to free or affordable legal services for beneficiaries facing housing-related issues.
- Connecting the individual to available resources to assist in establishing a bank account and bill paying.
- Assistance in connecting the individual with social services to assist with filling out applications and appropriate documentation in order to obtain sources of income necessary for community living, establishing credit, and in understanding and meeting the obligations of tenancy.
- Assistance in addressing circumstances and/or behaviors that may jeopardize housing. This should include both direct interventions to address risks and connection of the beneficiary to relevant community resources that may offer assistance.
- Assistance in resolving disputes with landlords and/or neighbors to reduce risk of eviction or other adverse action.
- Assistance with housing recertification processes, including lease renewals and housing subsidy renewals.
- Housing transition navigation services, including:
- One-time transition and moving costs (e.g., security deposit, first month's rent, brokerage fees, utility activation fees, movers, relocation expenses, pest eradication, inspection fees, pantry stocking, and the purchase of household goods and furniture).
- Assistance with the set-up of the new housing unit, to address needs identified in the person-centered care plan, including clinically appropriate residential modifications to allow the beneficiary to move in, and identify needs for assistance with arranging the move and supporting the details of the move, as appropriate.
- Connecting the individual to resources aiding with housing costs and other expenses, including linkages to rental assistance vouchers, security deposits, application fees, moving costs, non-medical transportation to tour units and attend tenant interviews, furnishings, adaptive aids, environmental modifications, and food and clothing needed at transition, and other related expenses.
- Providing a review of the living environment to ensure that it meets the clinical needs of the individual and appropriately supports his/her medical needs and is ready for move-in, including collaboration with relevant provider staff of where the individual is institutionalized (e.g., hospital or facility social worker) to ensure a seamless transition to the community.
- Case Management:
- Level One Case Management: Linkages to existing local, state, and federal benefits and programs, outside of the 1115 demonstration HRSN services.
- Level Two Case Management: Case management, outreach, and education including linkages to other state and federal benefit programs, benefit program application assistance, and benefit program application fees. Connections to providers, MCOs, crisis services, and behavioral health services. Connections to employment, education, childcare, legal assistance, and interpersonal violence resources. Follow up after services and linkages which includes follow-up after services which includes linkages to additional services that are existing state/federal/local-funded services, if needed.
- Nutrition Supports:
- Nutrition counseling and education for members, including on healthy meal preparation and connecting the individual with grocery budget resources.
- Up to 3 prepared meals a day, delivered to the home or private residence, for up to 6 months. Meals will be approved by a registered dietician nutritionist (RDN). Must have a health or medical condition that would benefit from medically tailored meals. Meals are either medically tailored, or clinically appropriate, depending on the individual needs of the beneficiary. High-risk pregnant individuals may receive up to 11 months but not to exceed up to 2 months postpartum in meals. Additional meal support is permitted when provided to the household of a child identified as high risk or pregnant individual, as defined in the risk and needs-based criteria in Attachment J. Beneficiaries who receive delivered meals cannot also receive pantry stocking or nutrition prescriptions.
- Medically tailored or nutritionally-appropriate food prescriptions (e.g., fruit and vegetable prescriptions, protein box), delivered in various forms such as nutrition vouchers and food boxes, for up to 6 months. High-risk pregnant individuals may receive up to 11 months but not to exceed up to 2 months postpartum in food prescriptions. Additional support is permitted when provided to the household of a child identified as high risk or pregnant individual, as defined in the risk and needs-based criteria in Attachment J. Beneficiaries who receive delivered food prescriptions cannot also receive pantry stocking or meals.
- Fresh produce and nonperishable groceries, for up to 6 months. Limited to pregnant persons and children as defined in Attachment J. High-risk pregnant individuals may receive up to 11 months but not to exceed up to 2 months postpartum in groceries. Additional support is permitted when provided to the household of a child identified as high risk or pregnant individual, as defined in the risk and needs-based criteria in Attachment J. Beneficiaries who receive delivered food prescriptions cannot also receive pantry stocking or meals.
- Up to 3 prepared meals a day, delivered to the home or private residence, medically tailored or nutritionally-appropriate food prescriptions, or fresh produce and nonperishable groceries may be renewed for additional 6-month periods if a follow up assessment, as provided in STCs 6.6 and 6.7, and the HRSN Protocol at Attachment K, determines the beneficiary still meets the clinical and needs-based criteria. The requirements pertaining to each of these services in STCs 6.2 c.ii.-iv. still apply to renewed services.
- Cooking supplies that are necessary for meal preparation and nutritional welfare of a beneficiary when not available through other programs (e.g., pots and pans, utensils, microwave, refrigerator).
- Private and public transportation to transport members to covered HRSN services and case management activities.
- 6.3 Recuperative Care and Short-Term Pre-procedure and Post-Hospitalization Care
- Recuperative care and short-term post hospitalization housing settings provide a safe and stable place for eligible individuals transitioning out of institutions, and who are at risk of incurring other Medicaid state plan services, such as inpatient hospitalizations or emergency department visits (as determined by a provider at the plan or network level), to receive treatment on a short-term basis. Pre-procedure housing is for individuals that are experiencing homelessness and are scheduled for surgery that has been indicated as needing preparation or pre-surgical care by a medical professional. Eligible settings for recuperative care and short-term pre-procedure and post hospitalization housing must have clinicians who can provide appropriate medical and/or behavioral health care. Short-term pre-procedure and post hospitalization housing settings must also offer transitional supports to help enrollees secure stable housing and avoid future readmissions. Recuperative care may be offered for up to ninety (90) days in duration once every 12 months (assessed on a rolling basis). The combination of pre-procedure and post-hospitalization housing may not exceed 6 months, once every 12 months. Pre-procedure stays are limited to a clinically appropriate amount of time. Electing organizations will implement recuperative care, pre-procedure care, and short-term post-hospitalization housing in accordance with the detailed service definitions, standards and requirements in Attachment J.
- The HRSN Services Protocol, described in STC 6.7, must include a description of the state's documented process to authorize Recuperative Care and Short-Term Pre-procedure and Post Hospitalization Housing Service for beneficiaries for whom there is an assessed risk of a need for other Medicaid state plan services, such as inpatient hospitalizations or emergency department visits. This process must document that a provider using their professional judgement has determined it to be medically appropriate for the specific beneficiary as provision of the Recuperative Care, Short-Term Pre-procedure, and Post Hospitalization Housing Service is likely to reduce or prevent the need for acute care or other Medicaid services. This documentation could be included in a care plan developed for the beneficiary. In addition to this clinical documentation requirement, states may also impose additional provider qualifications or other limitations and protocols, and these must be documented within the managed care plan contracts, HRSN Services Protocol, and state guidance.
- Eligible settings for recuperative care, short-term pre-procedure, and post-hospitalization housing must have appropriate clinicians who can provide medical and/or behavioral health care. The facility cannot be primarily used for room and board without the necessary additional recuperative support services. For example, a hotel room in a commercial hotel, where there are no medical or behavioral health supports provided onsite appropriate to the level of need, would not be considered an appropriate setting, but if a hotel had been converted to a recuperative care facility with appropriate clinical supports, then it would be an eligible setting.
- 6.4 HRSN Infrastructure.
- The state may claim FFP in infrastructure investments in order to support the development and implementation of HRSN services, subject to Section 6.1. This FFP will be available for the following activities:
- Technology - e.g., electronic referral systems, shared data platforms, electronic health record (EHR) modifications or integrations, screening tool and/or case management systems, databases/data warehouses, interoperability with the State Health Information Network for New York, information security, data analytics and reporting, data protections and privacy, accounting and billing systems.
- Development of business or operational practices, including Social Care Network administration - e.g., procurement and planning, screening and referral processes, capacity building for social service providers and network development, developing policies and workflows for referral management, privacy, quality improvement, trauma-informed practices, evaluation, member navigation.
- Workforce development - e.g., cultural competency training, trauma-informed training, traditional health worker certification, training staff on new policies and procedures.
- Outreach, education, and stakeholder convening - e.g., design and production of outreach and education materials, translation, obtaining community input, investments in stakeholder convening.
- The state may claim FFP in HRSN infrastructure expenditures for no more than the annual amounts outlined in Table 8. In the event that the state does not claim the full amount of FFP for a given demonstration year, the unspent amounts will roll over to one or more demonstration years not to exceed this demonstration period and the state may claim the remaining amount in a subsequent demonstration year.
Table 8. Annual Limits of Total Computable Expenditures for HRSN Infrastructure
DY 25 DY26 DY 27 DY 28 Total Total Computable Expenditures $0 $260M $190M $50M $500M - Infrastructure investments will receive the applicable administrative match for the expenditure.
- This infrastructure funding is separate and distinct from the payment to the applicable managed care plans for delivery of HRSN services. The state must ensure that HRSN infrastructure expenditures described in STC 6.4 are not factored into managed care capitation payments, and that there is no duplication of funds.
- The state may not claim any FFP in HRSN infrastructure expenditures until the Protocol for Assessment of Beneficiary Eligibility and Needs, Infrastructure Planning, and Provider Qualification is approved, as described in STC 6.6. Once approved, the state can claim FFP in HRSN infrastructure expenditures retrospectively to the beginning of the demonstration approval date.
- To the extent the state requests any additional infrastructure funding, or changes to its scope as described within this STC, it must submit an amendment to the demonstration for CMS's consideration.
- 6.5 Excluded HRSN Services. Excluded items, services, and activities that are not covered as HRSN services include, but are not limited to:
- Construction costs (bricks and mortar) except as needed for approved medically necessary home modifications as described in STC 6.2(a)(ii).
- Capital investments;
- Room and board outside of specifically enumerated care or housing transitions or beyond 6 months, except as specified in STC 6.1 and 6.3;
- Research grants and expenditures not related to monitoring and evaluation;
- Costs for services in prisons, correctional facilities or services for people who are civilly committed and unable to leave an institutional setting;
- Services provided to individuals who are not lawfully present in the United States or are undocumented;
- Expenditures that supplant services and activities funded by other state and federal governmental entities;
- School based programs for children that supplant Medicaid state plan programs, or that are funded under the Department of Education or state, and the local education agency;
- General workforce activities, not specifically linked to Medicaid or Medicaid beneficiaries; and
- Any other projects or activities not specifically approved by CMS as qualifying for demonstration coverage as a HRSN item or service under this demonstration.
- 6.6 Covered Populations. Expenditures for HRSN services may be made for the targeted populations specified below, consistent with this STC. To receive HRSN services, individuals in the target populations must have a documented medical need for the services and the services must be determined medically appropriate, as described in the HRSN Services Section in STC 6.2, for the documented need. Medical appropriateness must be based on clinical and health-related social risk factors, including whether the service would have a reasonable expectation of improving maintaining the health or overall function of the beneficiary. This determination must be documented in the beneficiary's care plan or medical record. Additional detail on targeted populations, including the clinical and other health related-social needs criteria, is outlined in Attachment J.
- Populations Eligible for Level One Services. Level One Services includes screening and Level One Case Management. If a member does not meet the criteria for Level Two HRSN services, then they will receive navigation to state, federal, and local programs outside of the 1115 demonstration to address their HRSN needs. Beneficiaries may be in either fee-for-service or managed care and receive this service.
- Populations Eligible for Level Two Services. Level Two services include Level Two Case Management, and all HRSN Housing, Nutrition, and Transportation Services. Beneficiaries must be enrolled in Medicaid Managed Care and meet one or more of the following criteria, plus be individually assessed for medically needing services per STC 6.6 above:
- Medicaid high utilizers (defined by Emergency Department, Inpatient, or Medicaid spend, or transitioning from an institutional setting), including those who meet the Department of Housing and Urban Development's definition of homeless as defined by 24 CFR 91.5;
- Individuals enrolled in a New York State designated Health Home which currently includes individuals with HIV/AIDS, Sickle Cell Disease, Serious Mental Illness, Substance Use Disorder, Serious Emotional Disturbance, Complex Trauma, or two or more chronic conditions (e.g., Diabetes and Chronic Obstructive Pulmonary Disease);
- Individuals with SUD;
- Individuals with SMI;
- Individuals with Intellectual and Developmental Disabilities;
- Pregnant persons, up to 12 months postpartum;
- Post-release criminal justice-involved population with serious chronic conditions, SUD, or chronic Hepatitis-C;
- Juvenile justice involved youth, foster care youth, and those under kinship care.
- Children under the age of six; and
- Children under the age of 18 with one or more chronic condition.
- 6.7 Protocol for Assessment of Beneficiary Eligibility and Needs, Infrastructure Planning, and Provider Qualifications for HRSN Services. The state must submit, for CMS approval, a Protocol for Assessment of Beneficiary Eligibility and Needs, Infrastructure Planning, and Provider Qualifications to CMS no later than 90 days after approval of these authorities. The protocol(s) must include, as appropriate, a list of the HRSN services and service descriptions, the criteria for defining a medically appropriate population for each service, the process by which that criteria will be applied including care plan requirements or other documented processes, proposed uses of HRSN infrastructure funds, and provider qualification criteria for each service. Each protocol may be submitted and approved separately. The state must resubmit an updated protocol, as required by CMS feedback on the initial submission. The protocol may be updated as details are changed or added. The state may not claim FFP in HRSN services or HRSN infrastructure expenditures until CMS approves the associated protocol, except as otherwise provided herein. Once the associated protocol is approved, the state can claim FFP in HRSN services and HRSN infrastructure expenditures retrospectively to the beginning of the demonstration approval date. The approved protocol(s) will be appended to the STCs as Attachment K.
Specifically, the protocol must include the following information:
- Proposed uses of HRSN infrastructure expenditures, including the type of entities to receive funding, the intended purpose of the funding, the projected expenditure amounts, and an implementation timeline.
- A list of the covered HRSN services (not to exceed those allowed under STC 6.2), with associated service descriptions and service-specific provider qualification requirements.
- A description of the process for identifying beneficiaries with health-related social needs, including outlining beneficiary eligibility, implementation settings, screening tool selection, and rescreening approach and frequency, as applicable.
- A description of the process by which clinical criteria will be applied, including a description of the documented process wherein a provider, using their professional judgment, may deem the service to be medically appropriate.
- Plan to identify medical appropriateness based on clinical and social risk factors.
- Plan to publicly maintain these clinical/social risk criteria to ensure transparency for beneficiaries and stakeholders.
- A description of the process for developing care plans based on assessment of need.
- Plan to initiate care plans and closed-loop referrals to social services and community providers based on the outcomes of screening.
- Description of how the state will ensure that HRSN screening and service delivery are provided to beneficiaries in ways that are culturally responsive and/or trauma-informed.
- Plan to avoid duplication/ displacement of existing food assistance/nutrition services including how the state will prioritize and wrap around SNAP and/or WIC enrollment, appropriately adjust Medicaid benefits for individuals also receiving SNAP and/or WIC services, and ensure eligible beneficiaries are enrolled to receive SNAP and/or WIC services.
- An affirmation that the state agrees to meet the enhanced monitoring and evaluation requirements stipulated in STC 14.7.b.ii and STC 17.6.a which require the state to monitor and evaluate how the renewals of recurring nutrition services in STC 6.2.c.v affect care utilization and beneficiary physical and mental health outcomes, as well as the cost of providing such services. As required in STC 14.6 and STC 17.3, the monitoring protocol and evaluation design are subject to CMS approval.
- 6.8 Service Delivery: HRSN services will be primarily provided in the managed care delivery system with limited case management services being provided in the FFS delivery system. As outlined in STC 6.1, HRSN services will be delivered by HRSN service providers in cooperation with SCNs. Terms applicable to all HRSN Services:
- HRSN screening and HRSN 1115 Level One Case Management services will be paid on a FFS basis when those HRSN services are provided to beneficiaries enrolled in Medicaid FFS.
- When HRSN services are provided to beneficiaries enrolled in Medicaid managed care, the SCNs will be contracted providers with the managed care plans. The following terms will also apply:
- As of April 1, 2024, HRSN Services will be provided as a non-risk basis in Medicaid managed care. For a non-risk payment, the MCO is not at financial risk for changes in utilization or for costs incurred under the contract that do not exceed the upper payment limits specified in 42 CFR 447.362 and may be reimbursed by the state at the end of the contract period on the basis of the incurred costs, subject to the specified limits. For the purposes of this demonstration, fee-for-service as defined in 42 CFR 447.362 is the fee-for-service authorized in this demonstration for HRSN Services paid on a fee-for-service basis by the state. The managed care plan contracts must clearly document the process and methodology for non-risk payments.
- No later than April 1, 2027, the state will incorporate the HRSN Services into the risk-based capitation rates in Medicaid managed care, and must comply with all applicable Federal requirements, including but not limited to 42 CFR 438.4, 438.5, 438.6, and 438.7, and the state may no longer utilize non-risk payments.
- Any applicable HRSN 1115 services that are delivered by managed care plans in a risk arrangement, must be included in the managed care contracts and rate certifications submitted to CMS for review and approval in accordance with 42 CFR 438.3(a) and 438.7(a). The state must monitor and provide narrative updates through its Quarterly and Annual Monitoring Reports on the inclusion of HRSN services in managed care programs.
- When HRSN (i.e., HRSN services defined in STC 6.1 for the covered populations outlined in STC 6.6) is included in capitation rates to managed care plans under risk-based contracts, and only then, HRSN services should be reported in the medical loss ratio (MLR) reporting as incurred claims. The state must develop an MLR monitoring and oversight process specific to HRSN services. This process must be submitted to CMS, for review and approval, no later than 6 months prior to the implementation of HRSN services in risk-based managed care contracts and capitation rates. The state should submit this process to CMS at DMCPMLR@cms.hhs.gov. This process must specify how HRSN services will be identified for inclusion in capitation rate setting and in the MLR numerator. The state's plan must indicate how expenditures for HRSN administrative costs and infrastructure will be identified and reported in the MLR as non-claims costs.
- In accordance with STC 6.14, CMS expects the state to have appropriate encounter data associated with each HRSN service. This is necessary to ensure appropriate fiscal oversight for HRSN services as well as monitoring and evaluation. This is also critical to ensure appropriate base data for Medicaid managed care rate development purposes as well as appropriate documentation for claims payment in both managed care and FFS. Therefore, CMS requires that for HRSN services provided in a managed care delivery system, the state must include the name and definition of each HRSN service as well as the coding to be used on claims and encounter data in the managed care plan contracts. For example, the state must note specific Healthcare Common Procedure Coding System (HCPCS) or Current Procedural Terminology costs that identify each HRSN service. Additionally, for HRSN services provided in an FFS delivery system, this information must be clearly documented for Social Care Networks. CMS will also consider this documentation necessary for approval of any rate methodologies per STC 6.15.
- The state must monitor and provide narrative updates through its Quarterly and Annual Monitoring Reports on the inclusion of HRSN services in managed care programs and in FFS.
- 6.9 Contracted Providers. Consistent with the managed care contract and applicable to all HRSN services:
- Managed care plans will contract with SCNs ("Contracted Providers") to deliver the elected HRSN services authorized under the demonstration.
- SCNs must establish a network of providers and ensure the Social Service Providers have sufficient experience and training in the provision of the HRSN services being offered. Social Service Providers do not need to be licensed, however, staff offering services through Social Service Providers must be licensed when appropriate and applicable.
- The managed care plan and SCN will use rates set by the state for the provision of applicable HRSN services, consistent with state guidance for these services, and in compliance with all related federal requirements.
- Any state direction of managed care plan expenditures under risk-based contract(s) and risk-based payments would only be considered a state directed payment subject to the requirements in 42 CFR 438.6(c).
- 6.10 Provider Network Capacity. Managed care plans must ensure the HRSN services authorized under the demonstration are provided to eligible beneficiaries in a timely manner, and shall develop policies and procedures outlining its approach to managing provider shortages or other barriers to timely provision of the HRSN services, in accordance with the managed care plan contracts and other state Medicaid/operating agency guidance.
- 6.11 Compliance with Federal Requirements. The state shall ensure HRSN services are delivered in accordance with all applicable federal statute, regulation or guidance.
- 6.12 Person Centered Plan. The state shall ensure there is a person-centered service plan for each individual receiving HRSN services that is person-centered, identifies the member's needs and individualized strategies and interventions for meeting those needs, and be developed in consultation with the member and the member's chosen support network as appropriate. The service plan is reviewed and revised at least every 12 months, when the individual's circumstances or needs change significantly, or at the request of the individual.
- 6.13 Conflict of Interest. The state shall ensure appropriate protections against conflicts of interest in the service planning. The state also agrees that appropriate separation of service planning and service provision functions are incorporated into the state conflict of interest policies.
- 6.14 CMS Approval of Managed Care Contracts. As part of the state's submission of associated Medicaid managed care plan contracts to implement HRSN services through managed care, the state must include contract requirements including, but not limited to:
- Beneficiary and plan protections, including but not limited to:
- HRSN services must not be used to reduce, discourage, or jeopardize Medicaid beneficiaries' access to Medicaid covered services.
- Medicaid beneficiaries always retain their right to receive the Medicaid covered service on the same terms as would apply if HRSN services were not an option.
- Medicaid beneficiaries who are offered or utilized an HRSN retain all rights and protections afforded under 42 CFR 438.
- Managed care plans are not permitted to deny a beneficiary a medically appropriate Medicaid covered service on the basis that they are currently receiving HRSN services, have requested those services, or have previously received these services.
- Managed care plans are prohibited from requiring a beneficiary to utilize HRSN services.
- Managed care plans must timely submit data requested by the state or CMS, including, but not limited to:
- Data to evaluate the utilization and effectiveness of the HRSN services.
- Any data necessary to monitor health outcomes and quality of care metrics at the individual and aggregate level through encounter data and supplemental reporting on health outcomes and equity of care. When possible, metrics must be stratified by age, sex (including sexual orientation and gender identify), race, ethnicity, disability status and preferred language to inform health quality improvement efforts, which may thereby mitigate health disparities.
- Any data necessary to monitor appeals and grievances for beneficiaries.
- Documentation to ensure appropriate clinical support for the medical appropriateness of HRSN services.
- Any data determined necessary by the state or CMS to monitor and oversee the HRSN initiatives.
- All data and related documentation necessary to monitor and evaluate the HRSN services initiatives, including cost assessment, to include but not limited to:
- The managed care plans must submit timely and accurate encounter data to the state for beneficiaries eligible for HRSN services. When possible, this encounter data must include data necessary for the state to stratify analyses by age, sex (including sexual orientation and gender identity), race, ethnicity, disability status and preferred language to inform health quality improvement efforts and subsequent efforts to mitigate health disparities undertaken by the state.
- Any additional information requested by CMS, the state or legally authorized oversight body to aid in on-going evaluation of the HRSN services or any independent assessment or analysis conducted by the state, CMS, or a legally authorized independent entity.
- The state must monitor and provide narrative updates through its Quarterly and Annual Monitoring Reports its progress in building and sustaining its partnership with existing housing agencies and nutrition agencies to utilize their expertise and existing housing resources and avoid duplication of efforts.
- Any additional information determined reasonable, appropriate and necessary by CMS.
- 6.15 HRSN Rate Methodologies. All rate and/or payment methodologies for authorized HRSN services outlined in these STCs must be submitted to CMS for review and approval prior to implementation, including but not limited to FFS payment, as well as non-risk payments, state directed payment preprints, and capitation rates in managed care delivery systems, as part of the HRSN Implementation Plan (see STC 6.19) at least 60 days prior to implementation. The state must submit all documentation requested by CMS, including but not limited to the payment rate methodology (or methodologies) as well as other documentation and supporting information (e.g., state responses to Medicaid non-federal share financing questions). The state must also notify CMS if they intend to direct their managed care plans on how to pay for HRSN services at least 60 days prior to implementation.
- 6.16 Maintenance of Effort (MOE). The state must maintain a baseline level of state funding for ongoing social services related to the categories of housing transition supports and nutrition supports comparable to those authorized under this demonstration, for the populations authorized under this demonstration, and for the duration of this demonstration, not including one time or non-recurring funding. Within 90 days of demonstration approval, the state will submit a plan to CMS as part of the HRSN Implementation Plan that specifies how the state will determine baseline spending on these services throughout the state. The annual MOE will be reported and monitored as part of the Annual Monitoring Report described in STC 14.7, with any justifications, including declines in available state resources, necessary to describe the findings, if the level of state funding is less than the comparable amount of the pre-demonstration baseline.
- 6.17 Partnerships with State and Local Entities. The state must have in place partnerships with other state and local entities (e.g., HUD Continuum of Care Program, local housing authority, Supplemental Nutrition Assistance Program (SNAP) state agency) to assist beneficiaries in obtaining non-Medicaid funded housing and nutrition supports, if available, upon the conclusion of temporary Medicaid payment for such supports, in alignment with beneficiary needs identified in the care plans as appropriate. The state will submit a plan to CMS as part of the HRSN Implementation Plan that outlines how it will put into place the necessary arrangements with other state and local entities and also work with those entities to assist beneficiaries in obtaining available non-Medicaid funded housing and nutrition supports upon conclusion of temporary Medicaid payment as stated above. The plan must provide a timeline for the activities outlined. As part of the Monitoring Reports described in STC 14.7, the state will provide the status of the state's fulfillment of its plan and progress relative to the timeline, and whether and to what extent the non-Medicaid funded supports are being accessed by beneficiaries as planned. Once the state's plan is fully implemented, the state may conclude its status updates in the Monitoring Reports.
- 6.18 Provider Payment Rate Increase. As a condition of the HRSN services and infrastructure expenditure authorities, New York must comply with the provider rate increase requirements in Section 7 of the STCs.
- 6.19 HRSN Implementation Plan
- The state is required to submit a HRSN Implementation Plan that will elaborate upon and further specify requirements for the provision of HRSN services and will be expected to provide additional details not captured in the STCs regarding implementation of demonstration policies that are outlined in the STCs. The Implementation Plan can be updated as initiatives are changed or added. CMS will provide a template to support this reporting that the state will be required to use to help structure the information provided and prompt the state for information CMS would find helpful in approving the Implementation Plan. The state must submit the MOE information required by STC 6.16 for CMS approval no later than 90 calendar days after approval of this demonstration. All other Implementation Plan requirements outlined in this STC must be submitted for CMS approval no later than 9 months after the approval of this demonstration. Once approved, the Implementation Plan will be appended as Attachment J and, once appended, may be altered only with CMS approval.
- At a minimum, the Implementation Plan must provide a description of the state's strategic approach to implementing the policy, including timelines for meeting critical implementation stages or milestones, as applicable, to support successful implementation. The Implementation Plan does not need to repeat any information submitted to CMS under the Protocol for Assessment of Beneficiary Eligibility and Needs, Infrastructure Planning, and Provider Qualifications for HRSN services; however, as applicable, the information provided in the two deliverables must be aligned and consistent with one another.
- The Implementation Plan must include information on, but not limited to, the following:
- A plan for establishing and/or improving data sharing and partnerships with an array of health system and social services stakeholders to the extent those entities are vital to provide needed administrative and HRSN-related data on screenings, referrals, and provision of services, which are critical for understanding program implementation and conducting demonstration monitoring and evaluation;
- Information about key partnerships related to HRSN service delivery, including plans for capacity building for community partners and for soliciting and incorporating input from impacted groups (e.g., community partners, health care delivery system partners, and beneficiaries);
- Plans for changes to IT infrastructure that will support HRSN-related data exchange, including development and implementation of data systems necessary to support program implementation, monitoring, and evaluation. These existing or new data systems should, at a minimum, collect data on beneficiary characteristics, eligibility and consent, screening, referrals, and service provision;
- A plan for tracking and improving the share of Medicaid beneficiaries in the state who are eligible and enrolled in the SNAP, the Special Supplemental Nutrition Program for Women, Infants and Children (WIC), Temporary Assistance for Needy Families (TANF), and federal and state housing assistance programs, relative to the number of total eligible beneficiaries in the state;
- An implementation timeline and evaluation considerations impacted by the timeline, such as staged rollout, that can facilitate robust evaluation designs;
- Information as required per STC 6.15 (HRSN Rate Methodologies);
- Information as required per STC 6.16 (MOE); and
- Information as required per STC 6.17 (Partnerships with State and Local Entities).
- Failure to submit the Implementation Plan will be considered a material failure to comply with the terms of the demonstration project as described in 42 CFR 431.420(d) and, as such, would be grounds for termination or suspension of authority for HRSN Infrastructure and HRSN Services, under this demonstration.
7. PROVIDER RATE INCREASE REQUIREMENTS
- 7.1. The provider payment rate increase requirements described hereafter are a condition for the DSHP, Health Equity Initiative, and HRSN expenditure authorities, as referenced in expenditure authorities #8-13. CMS considers the combination of the following initiatives– Medicaid Hospital Global Budget Initiative Authority, HRSN, Workforce Initiatives, and HERO– to constitute a Health Equity Initiative.
- 7.2. As a condition of approval and ongoing provision of FFP for the DSHP, Equity Initiative, and HRSN expenditures over this demonstration period of performance, DY 24 through DY 28, the state will in accordance with these STCs increase and (at least) subsequently sustain Medicaid fee-for-service provider base rates, and require any relevant Medicaid managed care plan to increase and (at least) subsequently sustain network provider payment rates, by at least two percentage points in the ratio of Medicaid to Medicare provider rates for one of the service categories that comprise the state's definition of primary care, behavioral health care, or obstetric care, as relevant, if the average Medicaid to Medicare provider payment rate ratio for a representative sample of these services for any of these three categories of services is below 80 percent. If the average Medicaid to Medicare provider payment rate ratio for a representative sample of these services for any of these three categories of services is below 80 percent for only the state's Medicaid fee-for-service program or only Medicaid managed care, the state shall only be required to increase provider payments for the delivery system for which the ratio is below 80 percent. New York is also required to invest $199,072,125 (total computable) in rate increases as part of the demonstration amendment, which must be sustained by the state once implemented. This requirement is applicable even if no Medicaid rates are below 80 percent of Medicare rates. The state may make the rate increases in any demonstration year, but the net provider rate increases must amount to $199,072,125 by the end of the demonstration period.
- 7.3. The state may not decrease provider payment rates for other Medicaid or demonstration covered services to make state funds available to finance provider rate increases required under this STC (i.e., cost-shifting).
- 7.4. The state will, for the purpose of complying with these requirements to derive the Medicaid to Medicare provider payment rate ratio and to apply the rate increases as may be required under this section 7, identify the applicable service codes and provider types for each of the primary care, behavioral health, and obstetric care services, as relevant, in a manner consistent with other state and federal Medicaid program requirements, except that inpatient behavioral health services may be excluded from the state's definition of behavioral health care services.
- 7.5. No later than 90 days of the demonstration effective date, and if the state makes fee for service payments, the state must establish and report to CMS the state's average Medicaid to Medicare fee-for-service provider rate ratio for each of the three service categories - primary care, behavioral health and obstetric care, using either of the methodologies below:
- Provide to CMS the average Medicaid to Medicare provider rate ratios for each of the three categories of services as these ratios are calculated for the state and the service category as noted in the following sources:
- for primary care and obstetric care services in Zuckerman, et al. 2021. "Medicaid Physician Fees Remained Substantially Below Fees Paid by Medicare in 2019." Health Affairs 40(2): 343-348 (Exhibit 3); AND
- for behavioral health services (the category called, ‘Psychotherapy' in Clemans-Cope, et al. 2022. "Medicaid Professional Fees for Treatment of Opioid Use Disorder Varied Widely Across States and Were Substantially Below Fees Paid by Medicare in 2021." Substance Abuse Treatment, Prevention, and Policy (2022) 17:49 (Table 3)); OR
- Provide to CMS for approval for any of the three services categories the average ratio, as well as the code sets, code level Medicaid utilization, Medicaid and Medicare rates, and other data used to calculate the ratio, and the methodology for the calculation of the ratio under this alternative approach as specified below:
- Service codes must be representative of each service category as defined in STC 7.4;
- Medicaid and Medicare data must be from the same year and not older than 2019.
- The state's methodology for selecting the year of data, determining Medicaid code-level utilization, the service codes within the category, geographic rate differentials for Medicaid and/or Medicare services and their incorporation into the determination of the category average rate, the selection of the same or similar Medicare service codes for comparison, and the timeframes of data and how alignment is ensured should be comprehensively discussed in the methodology as provided to CMS for approval.
- 7.6 To establish the state's ratio for each service category identified in STC 7.4 as it pertains to managed care plans' provider payment rates in the state, the state must provide to CMS either:
- The average fee-for-service ratio as provided in STC 7.5(a), if the state and CMS determine it to be a reasonable and appropriate estimate of, or proxy for, the average provider rates paid by managed care plans (e.g., where managed care plans in the State pay providers based on state plan fee-for-service payment rate schedules); OR
- The data and methodology for any or all of the service categories as provided in STC 7.5(b) using Medicaid managed care provider payment rate and utilization data.
- 7.7 In determining the ratios required under STC 7.5 and 7.6, the state may not incorporate fee-for-service supplemental payments that the State made or plans through March 31, 2027, to make to providers, or Medicaid managed care pass-through payments in accordance with 42 CFR § 438.6(a) and 438.6(d).
- 7.8 If the state is required to increase provider payment rates for managed care plans per STC 7.2 and 7.6, the state must:
- Comply with the requirements for state directed payments in accordance with 42 CFR 438.6(c), as applicable; and
- Ensure that the entirety of a two-percentage point increase applied to the provider payments rates in the service category whose Medicaid to Medicare average payment rate ratio is below 80 percent is paid to providers, and none of such payment rate increase is retained by managed care plans.
- 7.9 For the entirety of DY 26 through DY 28, the provider payment rate increase for each service in a service category and delivery system for which the average ratio is less than 80 percent will be an amount necessary so that the Medicaid to Medicare ratio increases by two percentage points over the highest rate for each service in DY24, and such rate will be in effect on the first day of DY26. A required payment rate increase shall apply to all services in a service category as defined under STC 7.4.
- 7.10 If the state uses a managed care delivery system for any of the service categories defined in STC 7.4, for the beginning of the first rating period as defined in 42 CFR 438.2(a) that starts in each demonstration year from DY 26 through DY 28, the managed care plans' provider payment rate increase for each service in the affected categories will be no lower than the highest rate in DY 24 plus an amount necessary so that the Medicaid to Medicare ratio for that service increases by two percentage points. The payment increase shall apply to all services in a service category as defined under STC 7.4.
- 7.11 If the state has a biennial legislative session that requires provider payment rate approval and the timing of that session precludes the state from implementing a required payment rate increase by the first day of DY 26 (or, as applicable, the first day of the first rating period that starts in DY 26), the State will provide an alternative effective date and rationale for CMS review and approval.
- 7.12 New York will provide the information to document the payment rate ratio required under STC 7.5 and 7.6, via submission to the Performance Metrics Database and Analytics (PDMA) portal for CMS review and approval.
- 7.13 For demonstration years following the first year of provider payment rate increases, if any, New York will provide an annual attestation within the State's annual demonstration monitoring report that the provider payment rate increases subject to these STCs were at least sustained from, if not higher than, in the previous year.
- 7.14 No later than 90 days following the demonstration effective date, the state will provide to CMS the following information and Attestation Table signed by the State Medicaid Director, or by the Director's Chief Financial Officer (or equivalent position), to Performance Metrics Database and Analytics (PMDA), along with a description of the state's methodology and the state's supporting data for establishing ratios for each of the three service categories in accordance with STC 7.5 and 7.6 for CMS review and approval, at which time the Attestation Table will be appended to the STCs as Attachment M:
Table 9 - New York HRSN and DSHP Related Provider Payment Increase Assessment - Attestation Table The reported data and attestations pertain to HRSN, Health Equity Initiative, and DSHP related provider payment increase requirements for the demonstration period of performance DY 25 through DY 28 Category of Service Medicaid Fee-for-Service to Medicare Fee-for-service Ratio Medicaid Managed Care to Medicare Fee-for-service Ratio Primary Care Services [insert percent, or N/A if state does not make Medicaid fee-for-service payments] [insert percent, or N/A if state does not utilize a Medicaid managed care delivery system for applicable covered service categories] [insert approach, either ratio derived under STC 7.5(a) or STC 7.5(a)] [insert approach, either ratio derived under STC 7.6(a) or STC 7.6(b) insert data source and time period (e.g., applicable 12-month rating period) for each of Medicaid and Medicare to derive the ratio] Obstetric Care Services [insert percent, or N/A if state does not make fee-for-service payments] [insert percent, or N/A if state does not utilize a Medicaid managed care delivery system for providers of covered service categories] [insert approach, either ratio derived under STC 7.5(a) or STC 7.5(b)] [insert approach, either ratio derived under STC 7.6(a) or STC 7.6(b) insert data source and time period (e.g., applicable 12-month rating period) for each of Medicaid and Medicare to derive the ratio] Behavioral Health Care Services [insert percent, or N/A if state does not make fee-for-service payments] [insert percent, or N/A if state does not utilize a Medicaid managed care delivery system for applicable covered service categories] [insert approach, either ratio derived under STC 7.5(a) or STC 7.5(b)] [insert approach, either ratio derived under STC 7.6(a) or STC 7.6(b)]; insert data source and time period (e.g., applicable 12-month rating period) for each of Medicaid and Medicare to derive the ratio] In accordance with STCs 7.1 through 7.12, including that the Medicaid provider payment rates used to establish the ratios do not reflect fee-for-service supplemental payments or Medicaid managed care pass-through payments under 42 CFR 438.6(a) and 438.6(d), I attest that at least a two percentage point payment rate increase will be applied to each of the services in each of the three categories with a ratio below 80 percent in both fee-for-service and managed care delivery systems as applicable to the state’s Medicaid or demonstration service delivery model. Such provider payment increases for each service will be effective beginning on [insert date] and will not be lower than the highest rate for that service code in DY 24 plus a two-percentage point increase relative to the rate for the same or similar Medicare billing code through at least [insert date].
For the purpose of deriving the Medicaid to Medicare provider payment rate ratio, and to apply the rate increase as may be required under a fee-for-service delivery system or under managed care delivery system, as applicable, the state agrees to define primary care, behavioral health and obstetric care, and to identify applicable service codes and providers types for each of these service categories in a manner consistent with other state and federal Medicaid program requirements, except that inpatient behavioral health services may be excluded from the state’s definition.
The services that comprise each service category to which the rate increase must be applied will include all service codes that fit under the state’s definition of the category, except the behavioral health codes do not have to include inpatient care services.
For provider payment rates paid under managed care delivery system, the data and methodology for any one of the service categories as provided in STC 7.6(b) will be based on Medicaid managed care provider payment rate and utilization data.
[Select the applicable effective date, must check either a. or b. below]
☐ a. The effective date of the rate increases is the first day of DY [3, provide the actual year] and will be at least sustained, if not higher, through DY [5, provide the actual year]
☐ b. New York has a biennial legislative session that requires provider payment approval, and the timing of that session precludes the state from implementing the payment increase on the first day of DY [3, provide the actual year]. New York will effectuate the rate increases no later than the CMS approved date of [insert date], and will sustain these rates, if not made higher, through DY [5, provide the accrual year].New York [insert does or does not] make Medicaid state plan fee-for-service payments for the following categories of service for at least some populations: primary care, behavioral health, and / or obstetric care.
For any such payments, as necessary to comply with the DSHP, Health Equity Initiative, and HRSN STCs, I agree to submit by no later than [insert date] for CMS review and approval the Medicaid state plan fee-for-service payment increase methodology, including the Medicaid code set to which the payment rate increases are to be applied, code level Medicaid utilization, Medicaid and Medicare rates for the same or similar Medicare billing codes, and other data used to calculate the ratio, and the methodology, as well as other documents and supporting information (e.g., state responses to Medicaid financing questions) as required by applicable statutes, regulations and CMS policy, through the submission of a new state plan amendment, following the normal SPA process including publishing timely tribal and public notice and submitting to CMS all required SPA forms (e.g., SPA transmittal letter, CMS-179, Attachment 4.19-B pages from the state), by no later than [insert date]New York [insert does or does not] include the following service categories within a Medicaid managed care delivery system for which the managed care plans make payments to applicable providers for at least some populations: primary care, behavioral health, and or obstetric care.
For any such payments, as necessary to comply with the DSHP, Health Equity Initiative, and HRSN STCs, I agree to submit the Medicaid managed care plans’ provider payment increase methodology, including the information listed in STC 7.7 through the state directed payments submission process and in accordance with 42 CFR 438.6(c), as applicable, by no later than [insert date]If the state utilizes a managed care delivery system for the applicable service categories, then in accordance with STC 7.8, I attest that necessary arrangements will be made to assure that 100 percent of the two-percentage point managed care plans’ provider payment increase will be paid to the providers of those service categories and none of this payment rate increase is retained by the managed care plans. New York further agrees not to decrease provider payment rates for other Medicaid- or demonstration-covered services to make state funds available to finance provider rate increases required under this STC Section 7. I, [insert name of SMD or CFO (or equivalent position)] [insert title], attest that the above information is complete and accurate.
[Provide signature _______________________________] [Provide date ______________]
[Provide printed name of signatory]8. SUBSTANCE USE DISORDER (SUD) PROGRAM AND BENEFITS
- 8.1 SUD Program Benefits. Effective upon CMS's approval of the SUD Implementation Plan, the demonstration benefit package for Medicaid beneficiaries will include SUD treatment services, including services provided in residential and inpatient treatment settings that qualify as an IMD, which are not otherwise matchable expenditures under section 1903 of the Act. The state will be eligible to receive FFP for Medicaid beneficiaries who are short-term residents in IMDs under the terms of this demonstration for coverage of medical assistance, including OUD/SUD services, that would otherwise be matchable if the beneficiary were not residing in an IMD once CMS approves the state's Implementation Plan. The state will aim for a statewide average length of stay of 30 days or less in residential treatment settings, to be monitored pursuant to the SUD Monitoring Protocol as outlined in STC 14.5, to ensure short-term residential stays.
Under this demonstration beneficiaries will have access to high quality, evidence-based OUD/SUD treatment services across a comprehensive continuum of care, ranging from residential and inpatient treatment to ongoing chronic care for these conditions in cost-effective community-based settings.- 8.2 SUD Implementation Plan and HIT Plan.
- The state must submit the SUD Implementation Plan within ninety (90) calendar days after approval of this demonstration. The state must submit the revised SUD Implementation Plan within sixty (60) days after receipt of CMS's comments. The state may not claim FFP for services provided in IMDs to beneficiaries who are primarily receiving SUD treatment and withdrawal management services until CMS has approved the SUD Implementation Plan. Once approved, the SUD Implementation Plan will be incorporated into the STCs as Attachment H and once incorporated, may be altered only with CMS approval. After approval of the applicable implementation plans required by these STCs, FFP will be available prospectively, not retrospectively.
- Failure to submit a SUD Implementation Plan will be considered a material failure to comply with the terms of the demonstration project as described in 42 CFR 431.420(d) and, as such, would be grounds for termination or suspension of the SUD program under this demonstration. Failure to progress in meeting the milestone goals agreed upon by the state and CMS will result in a funding deferral as described in STC 14.1.
- At a minimum, the SUD Implementation Plan must describe the strategic approach and detailed project implementation plan, including timetables and programmatic content where applicable, for meeting the following milestones which reflect the key goals and objectives for the program:
- Access to Critical Levels of Care for OUD and other SUDs. Coverage of OUD/SUD treatment services across a comprehensive continuum of care including: outpatient; intensive outpatient; medication assisted treatment (medication as well as counseling and other services with sufficient provider capacity to meet needs of Medicaid beneficiaries in the state); intensive levels of care in residential and inpatient settings; and medically supervised withdrawal management, within 12-24 months of demonstration approval;
- Use of Evidence-based SUD-specific Patient Placement Criteria. Establishment of a requirement that providers assess treatment needs based on SUD-specific, multidimensional assessment tools, such as the American Society of Addiction Medicine (ASAM) Criteria or other assessment and placement tools that reflect evidence-based clinical treatment guidelines within 12-24 months of demonstration approval;
- Patient Placement. Establishment of a utilization management approach such that beneficiaries have access to SUD services at the appropriate level of care and that the interventions are appropriate for the diagnosis and level of care, including an independent process for reviewing placement in residential treatment settings within 12-24 months of demonstration approval;
- Use of Nationally Recognized SUD-specific Program Standards to set Provider Qualifications for Residential Treatment Facilities. Currently, residential treatment service providers must meet the requirements specified in Part 820 "Residential Services" of the Codes, Rules, and Regulations of the State of New York, Title 14 Department of Mental Hygiene, Chapter XXI of the Office of Alcoholism and Substance Abuse Services. The state must establish residential treatment provider qualifications in licensure, policy or provider manuals, managed care contracts or credentialing, or other requirements or guidance that meet program standards in the ASAM Criteria or other nationally recognized, SUD-specific program standards regarding in particular the types of services, hours of clinical care, and credentials of staff for residential treatment settings within 12-24 months of demonstration approval;
- Standards of Care. Establishment of a provider review process to ensure that residential treatment providers deliver care consistent with the specifications in the ASAM Criteria or other comparable, nationally recognized SUD program standards based on evidence-based clinical treatment guidelines for types of services, hours of clinical care, and credentials of staff for residential treatment settings within 12-24 months of demonstration approval;
- Standards of Care. Establishment of a requirement that residential treatment providers offer MAT on-site or facilitate access to MAT off-site within 12-24 months of demonstration approval;
- Sufficient Provider Capacity at each Level of Care including Medication Assisted Treatment for SUD/OUD. An assessment of the availability of providers in the critical levels of care throughout the state, or in the regions of the state participating under this demonstration, including those that offer MAT within 12 months of demonstration approval;
- Implementation of Comprehensive Treatment and Prevention Strategies to Address Opioid Abuse and SUD/OUD. Implementation of opioid prescribing guidelines along with other interventions to prevent prescription drug abuse and expand coverage of and access to naloxone for overdose reversal as well as implementation of strategies to increase utilization and improve functionality of prescription drug monitoring programs;
- Improved Care Coordination and Transitions between Levels of Care. Establishment and implementation of policies to ensure residential and inpatient facilities link beneficiaries with community-based services and supports following stays in these facilities within 24 months of demonstration approval;
- SUD HIT Plan. Implementation of a Substance Use Disorder Health Information Technology Plan which describes technology that will support the aims of the demonstration. Further information which describes milestones and metrics are detailed in STC 8.2.d and Attachment H.
- SUD Health Information Technology Plan ("HIT Plan"). The SUD Health information technology (HIT) plan applies to all states where the HIT functionalities are expected to impact beneficiaries within the demonstration. As outlined in SMDL #17-003, states must submit to CMS the applicable HIT Plan(s), to be included as a section(s) of the associated Implementation Plan(s) (see STC 8.2.a and 8.2.c), to develop infrastructure and capabilities consistent with the requirements outlined in each demonstration-type.
- The HIT Plan should describe how technology can support outcomes through care coordination; linkages to public health and prescription drug monitoring programs; establish data and reporting structure to monitor outcomes and support data driven interventions. Such technology should, per 42 CFR 433.112(b), use open interfaces and exposed application programming interfaces and ensure alignment with, and incorporation of, industry standards adopted by the Office of the National Coordinator for HIT in accordance with 42 CFR part 170, subpart B.
- The state must include in its Monitoring Protocol (see STC 14.7[a]) an approach to monitoring its SUD HIT Plan which will include performance metrics to be approved in advance by CMS.
- The state must monitor progress, each DY, on the implementation of its SUD HIT Plan in relationship to its milestones and timelines–and report on its progress to CMS within its Annual Report (see STC 15.9).
- As applicable, the state should advance the standards identified in the ‘Interoperability Standards Advisory–Best Available Standards and Implementation Specifications' (ISA) in developing and implementing the state's SUD HIT policies and in all related applicable State procurements (e.g., including managed care contracts) that are associated with this demonstration.
- Where there are opportunities at the state- and provider-level (up to and including usage in MCO or accountable care organization (ACO) participation agreements) to leverage federal funds associated with a standard referenced in 45 CFR 170 Subpart B, the state should use the federally recognized standards.
- Where there are opportunities at the state- and provider-level to leverage federal funds associated with a standard not already referenced in 45 CFR 170 but included in the ISA, the state should use the federally recognized ISA standards.
- Components of the HIT Plan include:
- The HIT Plan must describe the state's alignment with Section 5042 of the SUPPORT Act requiring Medicaid providers to query a Qualified Prescription Drug Monitoring Program (PDMP)5.
- The HIT Plan must address how the state's Qualified PDMP will enhance ease of use for prescribers and other state and federal stakeholders.6 States should favor procurement strategies that incorporate qualified PDMP data into electronic health records as discrete data without added interface costs to Medicaid providers, leveraging existing federal investments in RX Check for Interstate data sharing.
- The HIT Plan will describe how technology will support substance use disorder prevention and treatment outcomes described by the demonstration.
- In developing the HIT Plan, states should use the following resources:
- States may use federal resources available on HIT.Gov (https://www.healthit.gov/topic/behavioral-health) including but not limited to "Behavioral Health and Physical Health Integration" and "Section 34: Opioid Epidemic and HIT" (https://www.healthit.gov/playbook/health-information- exchange/).
- States may also use the CMS 1115 HIT resources available on "Medicaid Program Alignment with State Systems to Advance HIT, HIE and Interoperability" located here. States should review the "1115 HIT Toolkit" for HIT considerations in conducting an assessment and developing their HIT Plans.
- States may request from CMS technical assistance to conduct an assessment and develop plans to ensure they have the specific HIT infrastructure with regards to PDMP interoperability, electronic care plan sharing, care coordination, and behavioral health-physical health integration, to meet the goals of the demonstration.
- States should review the Office of the National Coordinator's Interoperability Standards Advisory (https://www.healthit.giv/isa/) for information on appropriate standards which may not be required per 45 CFR part 170, subpart B for enhanced funding, but still should be considered industry standards per 42 CFR 433.112(b)(12).
- 8.3 Unallowable Expenditures Under the SUD Expenditure Authority. In addition to the other unallowable costs and caveats already outlined in these STCs, the state may not receive FFP under any expenditure authority approved under this demonstration for any of the following:
- Room and board costs for residential treatment service providers unless they qualify as inpatient facilities under section 1905(a) of the Act.
9. MEDICAID HOSPITAL GLOBAL BUDGET INITIATIVE
The state is eligible to receive $2.2 billion total computable over 4 years or $550 million annually, contingent on it meeting the requirements below. A key goal of the state is to improve quality of care and promote adoption of alternative payment models that will stabilize finances of certain safety net hospitals and advance accountability and health equity. Under the demonstration, the state is providing financial support to certain hospitals located in Brooklyn, Bronx, Queens, and Westchester Counties in part due to the significant lower health factors and health outcomes in this area.
- 9.1 Medicaid Hospital Global Budget Initiative Criteria. The eligible hospitals must meet the following three criteria:
- Private Not-For-Profit Hospitals in the Bronx, Kings, Queens, and Westchester Counties with a Medicaid and Uninsured Payor Mix of at least 45 percent;
- Private Not-For-Profit Hospitals with an average operating margin that is less than or equal to 0 percent over the past four years (Calendar Years 2019-2022) based on audited Hospital Institutional Cost Reports (excluding COVID relief funding and state-only subsidy); and
- Private Not-For-Profit Hospitals or their affiliates that received state-only subsidies due to financial distress in State Fiscal Years 2023 and/or 2024.
- 9.2 Requirements for the Medicaid Hospital Global Budget Initiative. The state must submit a plan to implement a Medicaid Hospital Global Budget Model. If the state applies for and is chosen as a participant in the Center for Medicare and Medicaid Innovation (CMMI) model, entitled States Advancing All-Payer Health Equity Approaches and Development (AHEAD) and completes criteria a-e below as part of its participation in the model, it will be deemed to have met this requirement. Nothing in these STCs binds CMS to approve any future proposal from the state. If the state is not chosen under a CMMI AHEAD model, it must submit a Medicaid Hospital Global Budget methodology that meets the following requirements:
- The state must specify the Medicaid services proposed under the hospital global budget;
- The state must describe its methodology for constructing the hospital global budget, including how any section 1115 demonstration authority provided via the January 2024 amendment through March 31, 2027, will be incorporated into the budget;
- The state must specify a proposed methodology to determine updates for the budget;
- The state may propose adjustments similar to adjustments that align with the CMMI AHEAD model hospital global budget methodology for Medicare fee for service; and
- The state must propose a quality and health equity improvement strategy.
- 9.3 Requirements for Funding. To be eligible for any Medicaid Hospital Global Budget Initiative incentive payments, New York and certain, eligible individual hospitals must complete all of the requirements described below. If a hospital does not submit the required LOI, data, or application for CMMI AHEAD model, or other information specified below by the deadline, it will not be eligible for any future year incentive payments. New York intends to use state general revenue as its source of non-federal share for this initiative.
- 9.4 Requirements for DY 0 of Amendment (January 9, 2024 through March 31, 2024). The state must submit documentation in its annual monitoring report showing it met the following requirements no later than March 31, 2024.
- The state must submit an initial Letter of Intent (LOI) and then an application in response to a forthcoming Notice of Funding Opportunity (NOFO) for a CMMI state AHEAD model which will include hospital global budgets and primary care transformation (in either the first or second application period);
- The state must secure LOIs from eligible hospitals expressing intent to participate in a CMS model or another global payment model. The state must report to CMS in its standard 1115 monitoring reports which eligible hospitals have expressed interest in the model; and
- The state must submit a detailed plan showing how it and its providers will collect beneficiary-reported demographic and HRSN data7 and ensure completeness of the data.
- 9.5 Requirements for DY 1 of Amendment (April 1, 2024 to March 31, 2025). The state must submit documentation in its annual monitoring report showing it met the following requirements no later than March 31, 2025.
- If the state does not apply in the first CMMI AHEAD model application cohort, then the state must apply in the second application cohort of the CMMI AHEAD model by mid-2024.
- Each eligible hospital must reconfirm via an LOI that it will participate in the hospital global budget as a part of the CMMI AHEAD model. The state will submit documentation, in collaboration with participating hospitals, showing that they are on track for developing a Medicaid global payment methodology effective April 1, 2027 (the start of the next 1115 extension period).
- If the state and its eligible hospitals do not participate in the CMMI AHEAD model, the state must submit a proposal to CMS that includes details on an alternative Medicaid-only hospital global budget model to launch in the state as of April 1, 2027 (the start of the next 1115 extension period).
- Each participating hospital that receives Medicaid Hospital Global Budget Initiative incentive payments must submit a health equity plan to the state. These plans must be aligned with the statewide health equity plan described in (h) below.
- Each participating hospital must submit complete quality data on quality metrics to be specified in the state's post-approval Medicaid Hospital Global Budget Initiative to Medicaid Hospital Global Budget Initiative Implementation Protocol, appended to these STC once approved by CMS as Attachment L. The quality metrics should align to the extent reasonable to CMS's Disparities-Sensitive Measure Set.
- The state must confirm in the demonstration monitoring reports that each participating hospital submitted a common fact base for their health system to the state, including information such as:
- Key statistics on population served, degree of patient engagement/ satisfaction;
- Competitive landscape, including payor/provider and regulatory impacts;
- Overview of current financial performance and payment models;
- Evaluation of IT infrastructure, interoperability capabilities, data infrastructure, and reporting and analytics capabilities;
- Evaluation of physical plant infrastructure and necessary capital investments to support population health;
- Assessment of historical/projected operating expenses with specific focus on variable and non-variable expenses; and
- Opportunities for Quality Improvement.
- Each participating hospital must submit a custom roadmap to the state of key targeted activities required to transition to a global budget model, including considerations on where to invest versus build, required partnerships, talent change management, and technology gaps. The state must confirm submission in the demonstration monitoring reports.
- The state must develop an Implementation Plan that describes how it will develop a robust health equity plan to identify underserved communities and implement initiatives to measurably reduce health disparities within their beneficiary populations and prepare for statewide quality/equity measurements, appended to these STC once approved by CMS as Attachment L. The state must include the quality/ equity measures selected for hospital-level reporting and performance, which must include Pay for Performance (P4P) quality measures. The quality metrics should align to the extent reasonable to CMS's Disparities-Sensitive Measure Set. The state will identify baseline data, adequacy, and needs in communities as part of this plan. This plan must be submitted to CMS prior to April 1, 2025, and will be appended to these STCs as Attachment L once approved by CMS.
- 9.6 Requirements for DY 2 of Amendment (April 1, 2025 through March 31, 2026). The state must submit documentation in its annual monitoring report showing it met the following requirements no later than March 31, 2026 or sooner, as otherwise specified below.
- Each hospital must submit quality measures approved in the Implementation Protocol described in STC 9.5(e);
- Each hospital must execute key milestones on their state-approved roadmap in at least the following areas:
- Data, interoperability, analytics, and reporting;
- Financial modeling;
- Care coordination and management;
- Quality improvement;
- Compliance and business operations;
- Network and physician engagement;
- Patient experience and engagement;
- Opportunities for Service Line Rationalization based on community need; and
- Leadership, governance, and talent change management.
- The state must provide updates regarding its statewide health equity plan in the annual monitoring reports.
- The state must submit its plan and methodology for a Medicaid hospital global budget 18 months prior to the expiration of the current demonstration period or by September 30, 2025.
- The state must submit an updated plan regarding its methodology for a Medicaid hospital global budget as part of its 1115 extension request due March 31, 2026.
- 9.7 Requirements for DY 3 of Amendment (April 1, 2026 through March 31, 2027). The state must submit documentation showing in its annual monitoring report it met the following requirements no later than March 31, 2027.
- The state must work collaboratively with all components of CMS to achieve the proper Medicaid authorities to launch a Medicaid hospital global budget as of April 1, 2027.
- Each hospital must provide a progress report and, where appropriate, provide updates to their state-approved transformation roadmap to the state for approval.
The state must provide updates regarding its statewide health equity plan in the annual monitoring reports.- The state and hospitals must submit achievement on the Initiative's incentive metrics, including readiness to adopt global payment methodologies, as well as any funding forfeited by the state or hospitals due to a lack of performance. The state must provide achievement updates in the demonstration monitoring reports.
- 9.8 Medicaid Hospital Global Budget Initiative Funding by Demonstration Year. Below is a chart that specifies the funding for each year of the demonstration. The funding may roll over to the next year.
Table 10: Medicaid Hospital Global Budget Initiative DY 25 DY 26 DY 27 DY 28 Total 01/09/2024 to 03/31/2024 04/01/2024 to 03/31/2025 04/01/2025 to 03/31/2026 04/01/2026 to 03/31/2027 Total Computable Expenditures $550M $550M $550M $550M $2.2B - 9.9 Budget Neutrality Treatment for Medicaid Hospital Global Budget Initiative. The expenditure authority for the Medicaid Hospital Global Budget Initiative must be supported out of budget neutrality savings.
- 9.10 Federal Matching Rate for Medicaid Hospital Global Budget Initiative. All expenditures for the Medicaid Hospital Global Budget Initiative must be claimed as administrative on the applicable CMS 64.10 waiver form(s). The state must ensure that Medicaid Hospital Global Budget Initiative incentive expenditures described in STC 9 are not factored into managed care capitation payments, and that there is no duplication of funds.
- 9.11 Medicaid Hospital Global Budget Initiative Incentive Payments. Incentive payments under the Medicaid Hospital Global Budget Initiative are not direct reimbursement for expenditures or payments for services. Incentive payments under the Medicaid Hospital Global Budget Initiative shall not be considered patient care revenue and shall not be offset against disproportionate share hospital expenditures or other Medicaid expenditures that are related to the cost of patient care.
10. DELIVERY SYSTEMS
- 10.1 Contracts. Procurement and the subsequent final contracts developed to implement selective contracting by the state with any provider group shall be subject to CMS approval prior to implementation. Payments under contracts with public agencies, that are not competitively bid in a process involving multiple bidders, shall not exceed the documented costs incurred in furnishing covered services to eligible individuals (or a reasonableestimate with an adjustment factor no greater than the annual change in the consumer price indexthat shall be rebased based on actual documented costs no less than every two years).
- 10.2 Managed Care Contracts. No FFP is available for activities covered under contracts and/or modifications to existing contracts that are subject to 42 CFR 438 requirements prior to CMS approval of model contract language. The state shall submit any supporting documentation deemed necessary by CMS. The state must provide CMS with a minimum of 45 days to review and approve changes. CMS reserves the right, as a corrective action, to withhold FFP (either partial or full) for the demonstration, until the contract compliance requirement is met.
- 10.3 Compliance with Managed Care Requirements. The state must meet the requirements of 4242 CFR part 438 unless a requirement of part 438 has been identified in the waiver authorities as expressly waived or specified as not applicable to an expenditure authority for this demonstration.
- 10.4 Interpretation Services and Culturally Competent Care. The MCOs and other entities acting on behalf of the state Medicaid agency, including, but not limited to enrollment brokers, must have interpretation services and provide care that is consistent with the individual's culture. MCOs must conduct analyses to determine any gaps in access to these services and will expand its workforce accordingly. The MCOs may also require the use of remote video and voice technology when necessary.
- 10.5 Marketing Oversight.
- The state shall require each MCO to meet 42 CFR 438.104 and state marketing guidelines regarding prohibition of cold calls, use of government logos, and other standards.
- All materials used to market the MCO shall receive prior approval from the state.
- The state shall require through its contracts that each MCO provide all individuals who were not referred to the plan by the enrollment broker with information (in a format determined by the state) describing managed long-term care, a list of available plans and contact information to reach the enrollment broker for questions or other assistance.
- 10.6 Managed Care Benefit Packages. Individuals enrolled in managed care plans under the demonstration must receive from the managed care program the benefits as identified in Attachments A through D. As noted in plan readiness and contract requirements, the state must require that, for enrollees in receipt of LTSS, each MCO/ prepaid inpatient health plan (PIHP) coordinate, as appropriate, needs state plan services that are excluded from the managedcare delivery system but available through a fee-for-service delivery system, and must alsoassure coordination with services not included in the established benefit package. Plans will be at risk for any Medicaid covered service that is currently delivered. BH HCBS in HARPs and HIV SNPs will be non-risk for the initial years in accordance with STC 5.2. If the MCO network is unable to provide necessary medical services covered under the contract to a particular enrollee, the MCO will be required to cover these services out of network for the enrollee. The costs of room and board may not be covered and cannot be included when determining the MCO payment rates.
- 10.7 Managed Care Rates Transition for HARPs. While working towards a managed care capitated rate for HARPs, the state may not proceed with implementation in a region until it has approved HCBS fee for service rates for such region. The state must submit HARP capitation rates to CMS for approval no later than December 31, 2017. Should the state not have the ability to submit proposed rates, it must request a temporary extension to continue using the most recently approved rates.
- 10.8 Managed Care Rate Transition for Nursing Facilities (NF). As of February 1, 2015, plans are required to pay contracted nursing homes either the existing FFS rate or a negotiated rate which allows the nursing home and the plan to engage in other financing arrangements. MLTC and MMMC plans will be reimbursed with an actuarial sound rate in compliance with 42 CFR § 438.44. MLTC will develop a blended rate structure to promote community integration of institutional/HCBS. MMMC will develop a separate rate cell for the nursing home population and will include an HCBS "rate cohort" in its non-nursing home rate cells. The state shall submit an actuarial certification to CMS for approval of the April 1, 2015 rates that contains the following modifications:
- MLTC transition rates must be phased out;
- Documentation must be submitted identifying the unique and cumulative impact of the various capitation rate withholds;
- Documentation must be submitted assessing gaps in rate setting for MLTC plans that necessitate funds to mitigate risks.
- 10.9 Behavioral Health Services Furnished by MMMC, HIV SNPs, and HARPs. To the extent that an MCO is not able to meet the requirements for the management of the expanded behavioral health services, the MCO must contract with a managed care behavioral health organization to manage those services for enrollees. If the MCO network is unable to provide necessary medical services covered under the contract to a particular enrollee, the MCO will be required to cover these services out of network for the enrollee. This includes up to at least 2023 during which time the MCO will reimburse OMH ambulatory licensed and OASAS certified providers the FFS fee schedule to ensure continuity of care. MCOs must pay at least the FFS fee schedule for 24 months for the following services: Other Licensed Practitioner (OLP), Crisis Intervention, Community Psychiatric Support and Treatment (CPST), Psychosocial Rehabilitation (PSR), and Family and Youth Peer Support. After 90 days, the MCO may apply utilization review criteria to individuals under the care of non-participating providers. Plans will be required to authorize services and reimburse providers whether the behavioral health provider is contracted with the health plans or is an out of network provider. New York will reimburse MCOs for VFCA perdiem/Preventive Residential Treatment Services on a non-risk basis subject to the non-risk UPL at 42 CFR 447.362. The MCO must pay the FFS fee schedule as long as the Preventive Residential Treatment Services are non-risk.
- For SUD services and the delivery system changes associated with the new demonstration services and resulting state plan amendments including changes under the CMS Innovation Accelerator Program (IAP) and with CMS approval, the state may require the MCOs through their contracts to adopt system-wide changes and rates to ensure that the innovations are adopted in a consistent manner statewide.
- 10.10 Independent Consumer Support Program. To support the beneficiary's experience receiving and applying to receive long term services and supports in a managed care environment, the state shall create and maintain a permanent independent consumer support program to assist beneficiaries in understanding the coverage model and in the resolution of problems regarding services, coverage, access and rights.
- 10.11 Organizational Structure. The Independent Consumer Support Program shall operate independently from any MRT MCO. Additionally, to the extent possible, the program shall also operate independently of the state Medicaid agency.
- 10.12 Accessibility. The services of the Independent Consumer Support Program shall be available to all Medicaid beneficiaries enrolled in MRT who need LTSS (institutional, residential and community based) and must be accessible through multiple entryways (e.g., phone, internet, office) and also provide outreach in the same manner as appropriate.
- 10.13 Functions. The Independent Consumer Support Program shall assist beneficiaries to navigate and access covered LTSS, including the following activities:
- offer beneficiaries support in the pre-enrollment state, such as unbiased health plan choice counseling and general program-related information;
- serve as an access point for complaints and concerns about health plan enrollment, access to services and other related matters;
- help enrollees understand the fair hearing, grievance and appeal rights and processes within the health plan and at the state level, and assist them through the process if needed/requested; and
- conduct trainings with MRT MCO and providers oncommunity-based resources and supports that can be linked with covered plan benefits.
- 10.14 Staffing. The Independent Consumer Support Program must employ individuals who are knowledgeable about the state's Medicaid programs; beneficiary protections and rights under Medicaid managed care arrangements; and the health and service needs of persons with complex needs, including those with a chronic condition, disability, and cognitive or behavioral needs.
- 10.15 Data Collection and Reporting. The Independent Consumer Support Program shall track the volume and nature of beneficiary contacts and the resolution of such contacts on a schedule and manner determined by the state, but no less frequently than quarterly.
- 10.16 Geographic expansion of MLTC and LTSS in MMMC. In any geographic location where the state is mandating MLTC or LTSS in MMMC, the state must have the Independent Consumer Support Program in place at least 30 days prior to enrollment procedures for that geographic location.
- 10.17 Required Monitoring Activities by the State and/or External Quality Review Organization (EQRO). The state's EQR process for the MMMC and MLTC plans shall meet all the requirements of 42 CFR §438 Subpart E. In addition, the state, or its EQRO shall monitor and annually evaluate the MCO/PIHPs performance on specific new requirements under mandatory enrollment of individuals utilizing long term services and supports. The state shall provide an update of the processes used to monitor the following activities as well as the outcomes of the monitoring activities within the annual report in STC 14.7. The new requirements include, but are not limited to the following:
- MLTC Plan Eligibility Assessments. To ensure that approved instruments are being used and applied appropriately and as necessary, and to ensure that individuals being served with LTSS meet the MLTC program eligibility requirements for plan enrollment. The state will also monitor assessments conducted by the plan where individuals are deemed ineligible for enrollment in an MLTC plan.
- Service Plans. To ensure that MCOs are appropriately creating and implementing service plans based on the enrollee's identified needs.
- MCO credentialing and/or verification policies. To ensure that LTSS services are provided by qualified providers.
- 10.18 Access to Care, Network Adequacy and Coordination of Care Requirements for Long Term Services and Supports (LTSS). The state shall set specific access and coordination requirements for MCO. These standards should take into consideration individuals with special health care needs, out of network requirements if a provider is not available withinthe specific access standard, ensuring choice of provider with capacity to serve individuals, time/distance standards for providers who do not travel to the individual's home, and physical accessibility of covered services. The MLTC or MMMC plan is not permitted to set these standards.
- 10.19 Demonstrating Network Adequacy. Annually, each MCO must provide adequate assurances that it has sufficient capacity to serve the expected enrollment in its servicearea and offers an adequate coverage of benefits as described for the anticipated number of enrollees in the service area.
- The state must verify these assurances by reviewing demographic, utilizationand enrollment data for enrollees in the demonstration as well as:
- the number and types of providers available to provide covered services to the demonstration population;
- the number of network providers accepting the new demonstration population; and
- the geographic location of providers and demonstration populations, as shown through GeoAccess, similar software or other appropriate methods.
- The state must submit the documentation required in subparagraphs (i) - (iii) above to CMS with each annual report.
- Enrollees and their representatives must be provided with reference documents to maintain information about available providers and services in their plans.
- 10.20 Advisory Committee as required in 42 CFR §438. The state must maintain for the duration of the demonstration a managed care advisory group comprised of individualsand interested parties appointed pursuant to state law by the Legislature and Governor. To the extent possible, the state will attempt to appoint individuals qualified to speak on behalf of seniors and persons with disabilities, including individuals with developmental disabilities, regarding the impact and effective implementation of the demonstration on individuals receiving LTSS.
- 10.21 Health Services to Native Americans Populations. The plan currently in place for patient management and coordination of services for Medicaid-eligible Native Americans developed in consultation with the Indian tribes and/or representatives from the Indian health programs located in participating counties shall continue in force for this extension period.
- 10.22 Requirements for risk-based managed care plans.
- For risk-based plans, the state must submit the plan-generated reports detailed in 42 CFR 438.8(k) as well as any other documentation used to determine compliance with 42 CFR 438.8(k) to CMS at DMCPMLR@cms.hhs.gov.
- For managed care plans that delegate risk to subcontractors, the state's review of compliance with 42 CFR 438.8(k) must consider MLR requirements related to such subcontractors; see https://www.medicaid.gov/federal-policy- guidance/downloads/cib051919.pdf. The state must submit its plan to operationalize STC 10.22.a.i through 10.22.a.v no later than six months after the demonstration approval. This plan must outline key deliverables and timelines to meet the requirements of STC 10.22.a. through 10.22.e.
- Effective April 1, 2025, the state must require risk-based plans contracted with the state to impose reporting requirements equivalent to the information required in 42 CFR 438.8(k) on their subcontractor plans or entities.
- No later than 1 year from date in 10.22.b, the state must require risk-based plans contracted with the state to impose remittance requirements equivalent to 42 CFR 438.8(j) on their subcontractor plans or entities.
- STC 10.22.a., 10.22.b, and 10.22.c must apply for all of the following entities:
- Risk-based plans for which the state receives federal financial participation for associated expenditures;
- Full and partially delegated plans;
- Other subcontractors, as applicable, that assume delegated risk from either the primary managed care plan contracted with the state, or plans referenced in STC 10.22.d.ii; and
- Other subcontractors, as applicable, that assume delegated risk from entities referenced in STC 10.22.d.iii.
- The state must work with CMS to effectuate an audit of the MLR data for all complete rating periods (i.e., MLR reporting periods) in this 1115 demonstration package. Final audit results and reporting must be provided to CMS no later than two years after the expiration of the current demonstration period.
- The state will update the managed care plan contract language to require managed care plans to provide HRSN services as described in STC 6.19. When HRSN services are included in risk-based capitation rates, as outlined in STC 6.15, HRSN services should be reported in the MLR reports as incurred claims. Managed care plans should not report HRSN services in the MLR until after the transition to include HRSN services in risk-based capitation rates. Managed care plans should report HRSN services paid on an at-risk basis, including care coordination, in the MLR.
- The state must develop an MLR monitoring and oversight process specific to HRSN services. This process must be submitted to CMS, for review and approval, no later than 18 months prior to the implementation of HRSN services in risk-based capitation rates. The state shall submit this process to CMS at DMCPMLR@cms.hhs.gov. This process must specify how HRSN services will be identified for inclusion in capitation rate setting and in the MLR numerator. The state's plan must indicate how expenditures for HRSN administrative costs and infrastructure will be identified and reported in the MLR as non-claims costs.
11. DESIGNATED STATE HEALTH PROGRAMS
- 11.1 The state may claim FFP for designated state health programs subject to the limits described below. This DSHP authority will allow the state to support DSHP-Funded Initiatives, as described in STC 11.3. This DSHP authority will be available from DY 25-DY 28.
- The DSHP will have an established limit in the amount of $3,981,442,500 total computable expenditures, in aggregate, for DY 25-DY 28.
- The state may claim FFP for up to the annual amounts outlined in Table 11, plus any unspent amounts from prior years. In the event that the state does not claim the full amount of FFP for a given demonstration year, the unspent amounts will roll over to one or more demonstration years not to exceed this demonstration period, and the state may claim the remaining amount in a subsequent demonstration year.
Table 11. Annual Limits in Total Computable Expenditures for DSHP
DY 25 DY 26 DY 27 DY 28 Total 01/09/2024 to 03/31/2024 04/01/2024 to 03/31/2025 04/01/2025 to 03/31/2026 04/01/2026 to 03/31/2027 Total Computable Expenditures $1.51B $916M $836M $717M $3.981B - The state must contribute $351,303,750 (state share) in original, non-freed up DSHP funds, for the remaining demonstration period ending on March 31, 2027, towards its initiatives described in STC 11.3. These funds may only derive from other allowable sources of non-federal share and must otherwise meet all applicable requirements of these STCs and the Medicaid statute and regulations.
- The state attests, as a condition of receipt of FFP under the DSHP expenditure authority, that all non-federal share for the DSHP is allowable under all applicable statutory and regulatory requirements, including section 1903(w) of the Act and its implementing regulations. The state acknowledges that approval of the DSHP expenditure authority does not constitute approval of the underlying sources of non-federal share, which may be subject to CMS financial review.
- As a post-approval protocol, the state shall submit an Approved DSHP List identifying the specific state programs for which FFP in expenditures can be claimed within 90 days of the demonstration approval date. The Approved DSHP List will be subject to CMS approval and will be limited to programs that are population- or public health-focused, aligned with the objectives of the Medicaid program with no likelihood that the program will frustrate or impede the primary objective of Medicaid to provide coverage of services for low-income and vulnerable populations, and serve a community largely made up of low-income individuals. Only after CMS approves the list and ensures that none of the requested state programs fall within the exclusions listed in STC 11.2 can the state begin claiming FFP for DSHP expenditures. The Approved DSHP List will be appended to the STCs as Attachment N.
- 11.2 Prohibited DSHP Expenditures.
- Allowable DSHP expenditures do not include any expenditures that are funded by federal grants or other federal sources (for example, American Rescue Plan Act funding, grants from the Health Resources and Services Administration, the Centers for Disease Control and Prevention, etc.) or that are included as part of any maintenance of effort or non-federal share expenditure requirements of any federal grant.
- Additionally, allowable DSHP expenditures do not include expenditures associated with the provision of non-emergency care to individuals who do not meet citizenship or immigration status requirements to be eligible for Medicaid. To implement this limitation, 9.2 percent of total provider expenditures or claims through DSHP identified as described in STC 11.1 will be treated as expended for non-emergency care to individuals who do not meet citizenship or immigration status requirements, and thus not matchable. This adjustment is reflected in the total computable amounts of DSHP described in STC 11.1 and will be made prior to the state submitting claims via the CMS-64/ MBES system.
- The following types of expenditures are not permissible DSHP expenditures: expenditures that are already eligible for federal Medicaid matching funds or other sources of federal funding, that are generally part of normal operating costs that would be included in provider payment rates, that are not likely to promote the objectives of Medicaid, or are otherwise prohibited by federal law. Exclusions that have historically fallen into these categories include, but are not limited to:
- Bricks and mortar;
- Shelters, vaccines, and medications for animals;
- Coverage/services specifically for individuals who are not lawfully present or are undocumented;
- Revolving capital funds; and
- Non-specific projects for which CMS lacks sufficient information to ascertain the nature and character of the project and whether it is consistent with these STCs.
- 11.3 DSHP-Funded Initiatives.
- Definition. DSHP-funded initiatives are Medicaid or CHIP section 1115 demonstration activities supported by DSHPs.
- Requirements. Expenditures for DSHP-funded initiatives are limited to costs not otherwise matchable under the state plan. CMS will only approve those DSHP-funded initiatives that it determines to be consistent with the objectives of the Medicaid statute; specifically, to expand coverage (e.g., new eligibility groups or benefits), improve access to covered services including home-and community-based services and behavioral health services, improve quality by reducing health disparities, or increase the efficiency and quality of care. Funding for DSHP-funded initiatives will not be supplanting, nor merely supplementing existing services or programs. DSHP-funded initiatives must be new services or programs within the state. Funding for DSHP-funded initiatives specifically associated with infrastructure start-up costs for new initiatives is time limited to the current demonstration period and will not be renewed.
- Approved DSHP-Funded Initiatives. The initiatives listed below are approved DSHP-funded initiatives for this demonstration. Any new DSHP-funded initiative requires approval from CMS via an amendment to the demonstration that meets the applicable transparency requirements.
- HRSN Services
- HRSN Infrastructure
- Transportation, Cooking Supplies, and Brokerage Fees
- HERO
- Workforce Initiatives
- The state must not use freed up dollars from the state workforce DSHPs to fund the 1115 demonstration workforce initiatives.
- 11.4 DSHP Claiming Protocol. The state will develop and submit to CMS, within 150 calendar days of the approval of the demonstration, a DSHP Claiming Protocol subject to CMS approval with which the state will be required to comply in order to receive FFP in DSHP expenditures. State expenditures for the DSHP must be documented in accordance with the protocol. The state is not eligible to receive FFP until the protocol is approved by CMS, and upon approval, the state may only claim FFP for DSHP expenditures retrospectively to the effective date of the demonstration amendment that added this STC. Once approved by CMS, the protocol will be appended as Attachment O to these STCs, and thereafter may be changed or updated only with CMS approval. Changes and updates are to be applied prospectively. In order to claim FFP for DSHP expenditures, the state will provide CMS a summary worksheet that identifies DSHP expenditures by program each quarter.
- For all eligible DSHP expenditures, the state will maintain and make available to CMS upon request:
- Certification or attestation of expenditures.
- Actual expenditure data from state financial information system or state client sub-system. The Claiming Protocol will describe the procedures used that ensure that FFP is not claimed for the non-permissible expenditures listed in STC 11.2.
- The state will claim FFP for DSHP quarterly based on actual expenditures.
- 11.5 DSHP Claiming Process. Documentation of all DSHP expenditures must be clearly outlined in the state's supporting work papers and be made available to CMS. Federal funds must be claimed within two years after the calendar quarter in which the state disburses expenditures for the DSHPs.
- Sources of non-federal funding must be compliant with section 1903(w) of the Act and applicable implementing regulations. To the extent that the DSHPs receive federal funds from any other federal programs, such funds shall not be used as a source of non-federal share to support expenditures for DSHPs or DSHP-funded initiatives under this demonstration.
- The administrative costs associated with DSHPs (that are not generally part of normal operating costs for service delivery) shall not be included in any way as demonstration and/or other Medicaid expenditures.
- DSHP will be claimed at the general administrative matching rate of 50 percent.
- Expenditures will be claimed in accordance with CMS-approved DSHP Claiming Protocol in Attachment O.
- 11.6 Sustainability Plan. The DSHP Sustainability Plan will describe the scope of DSHP-funded initiatives the state wants to maintain and the strategy to secure resources to maintain these initiatives beyond the current approval period. The state shall submit the DSHP Sustainability Plan to CMS no later than December 31, 2025, after the approval of this authority. Upon CMS approval, the plan will be appended as Attachment Q to these STCs. Any future modifications for the DSHP Sustainability Plan will require CMS approval.
12. WORKFORCE INITIATIVES
To support workforce recruitment and retention to promote the increased availability of certain health care practitioners who serve Medicaid and demonstration beneficiaries, the state shall implement two statewide workforce initiatives–the Student Loan Repayment for Qualified Providers and Career Pathways Training programs. Funding for these two workforce initiatives must not supplant state and federal funding or duplicate existing workforce loan repayment and professional training programs. New York will consult with the Health Resources and Services Administration (HRSA) as it works on these programs. The aim of these programs is to address shortages in qualified providers serving Medicaid members.
- 12.1 Student Loan Repayment for Qualified Providers. The state will make available the following student loan repayments:
- Psychiatrists, with a priority on child/adolescent psychiatrists - Up to $300,000, per provider, who make a 4-year full-time commitment to maintaining a personal practice panel, or working at an organization with a panel, that includes at least 30 percent Medicaid and/or uninsured members.
- Primary care physicians and dentists - Up to $100,000 per provider, who make a 4-year full-time commitment to maintaining a personal practice panel, or working at an organization with a panel, that includes at least 30 percent Medicaid and/or uninsured members.
- Nurse practitioners and pediatric clinical nurse specialists - Up to $50,000, per provider, who make a 4-year full-time commitment to maintaining a personal practice panel, or working at an organization with a panel, that includes at least 30 percent Medicaid and/or uninsured members.
- 12.2 Additional Terms and Operations of the Student Loan Repayment for Qualified Providers Program. For the demonstration student loan repayment program, the following shall apply:
- Loan repayments must be made directly only to the student loan servicer by either the state or a procured vendor. Funds will not be provided to individual practitioners. Payments will be made no less than annually.
- If the state procures a vendor, the state will first pay the managing vendor, the funds, so that it can then in turn make payments to the loan servicers.
- The state may have multiple rounds/cohorts of disbursements (i.e., awards to new individuals each year), so long as it does not extend beyond the applicable authorized level of funding for each program over the course of the demonstration or demonstration year, as applicable.
- The state shall have a process for ensuring that providers are continuing to meet the qualifying service commitment no less than every 6 months before making loan repayment disbursements. If the service commitment is not met, except in extraordinary circumstances as determined by the state (for example, circumstances such as disability or death), the state shall not make the loan disbursement and the state shall recoup any student loan payments made on behalf of the program participant. In the case of recoupment, the state shall return the federal share of those payments to CMS. Suspension or revocation of a professional license does not constitute an extraordinary circumstance for purposes of not meeting the service commitment.
- The state may only repay an amount up to the student loan amount owed by the provider. It may not pay an amount that exceeds an individual provider's student loan. Only the student loan for educational costs associated with the course of study that led to the highest degree earned as a prerequisite to obtaining the relevant clinical credential may qualify for reimbursement under one of the student loan repayment programs.
- For the student loan repayment program, the state will define application criteria and eligibility, and select awardees through a competitive process that will allow the state to evaluate the applicants relative to the criteria established. The state may prioritize providers with cultural and linguistic competence that is likely to reflect and respond to the needs of the Medicaid population. The criteria must comply with federal civil rights law and not impermissibly discriminate based on race, ethnicity, national origin, or any other federally protected classes or characteristics.
- 12.3 Career Pathways Training Program. The Career Pathways Training (CPT) Program is designed to build up the allied health and other healthcare workforce by funding training and education that focus on career advancement and unemployed individuals in order to create a reliable healthcare workforce pipeline to address health workforce shortages throughout the state. The CPT program will be organized into no more than three regions to support statewide implementation and is divided into two career pipelines–Healthcare Career Advancement and New Careers in Healthcare.
- Healthcare Career Advancement Pipeline. Individuals participating in the Healthcare Career Advancement Pipeline must be employed at a NY healthcare provider and accepted to participate in one of the CPT professional education programs described in STC 12.5. Participation will be conditioned on a 3-year commitment of service, in the new professional title, to healthcare providers enrolled in the Medicaid program that serve at least 30 percent Medicaid members and/or uninsured individuals.
- New Careers in Healthcare Pipeline. Individuals participating in the New Careers in Healthcare Pipeline must be unemployed or not employed by a NY healthcare provider and are accepted in one of the professional education programs described in STC 12.5. Participation will be conditioned on a 3-year commitment of service to healthcare providers enrolled in the Medicaid program that serve at least 30 percent Medicaid members and/or uninsured individuals.
- The state shall develop a process to routinely monitor and verify that CPT program participants remain in compliance with the training curriculum and qualifying service commitment. If the training or service commitment is not met, except in extraordinary circumstances as determined by the state (for example, circumstances such as disability or death), the state shall recoup from the program participant all payments for tuition and associated fees made on behalf of the program participant and return the federal share of those payments to CMS within 1 year of the breach in the service commitment. Suspension or revocation of a professional license or certification does not constitute an extraordinary circumstance for purposes of not meeting the service commitment. CPT program participants must pass required professional state licensing or certification examinations and obtain requisite licensure or certification no later than 1 year of completing the degree programs listed in STC 12.5, except in extraordinary circumstances as determined by the state (for example, circumstances such as disability or death). Failure to obtain requisite licensure or certification will constitute a breach in the service commitment requirement.
- The state may have multiple rounds/cohorts of disbursements (i.e., awards to new individuals each year), so long as it does not extend beyond the applicable authorized level of funding for each program over the course of the demonstration or demonstration year, as applicable. The cohorts will be structured to ensure that each program can be completed within the demonstration period.
- 12.4 Workforce Investment Organizations. The state will contract with Workforce Investment Organizations (WIOs) for the implementation, management, and oversight of the CPT Program in each region. The state will define WIO criteria and eligibility, and then select WIOs through a selection process that will allow the state to evaluate the applicants relative to the criteria established. The state must conduct oversight of the WIOs and use of funds through periodic WIO assessments of performance. The state has the authority to revoke designation of any WIO that no longer meets the state's qualifications, has failed to meet performance requirements, or does not comply with the conflict-of-interest requirements.
- Partnerships. WIOs must establish the necessary partnerships to directly work with training and educational institutions, health systems, and CPT participants to coordinate training and education opportunities, provide meaningful support of the participants to assure successful completion of programs, and job placement to meet service commitments.
- Reporting to the state. WIOs will be required to meet workforce training performance metrics identified by the state and CMS. WIOs must monitor and report CPT program participant compliance with service commitments no less than every quarter. The state may require WIOs to report necessary data to the Health Equity Regional Organization (HERO) responsible for data aggregation and statewide monitoring of WIOs.
- Conflicts of Interest. The state must ensure that there are no conflicts of interest between WIOs (including WIO governance boards) and education institutions, healthcare entities and any other CPT program partner in which the WIO or the state will be responsible for selecting to provide CPT services. WIOs must be independent entities and must not be affiliated with any CPT program partners the WIOs will be paying for CPT related program costs (i.e., tuition, program fees, and backfill costs described in STC 12.6). WIOs with education institutions, healthcare entities and any other CPT program partners on their existing governance boards must establish a separate governance board for the oversight and management of CPT programs that excludes these partners to ensure no conflict of interest.
- 12.5 CPT Professional Education Programs. The CPT education and training offerings shall be limited to the course curriculums necessary to achieve the professional titles listed in STC 12.5(a)-(c). The state may identify additional healthcare occupations that may emerge as part of the state's initiative to address health related social needs for inclusion in CPT backed up by data/evidence supporting that there are workforce shortages similar to the categories below, but it must not alter the allowable funding in STC 12.7, and the state must receive prior CMS approval. The state must conduct oversight of WIOs and ensure CPT trainings are limited to the course curriculums listed in STC 12.5(a)-(c) and additional curriculums approved by CMS. The state will identify, screen, and select institutional entities that will provide the education and training to the CPT participants. The training programs must be certified or accredited by the state or organizations recognized by the state. WIOs must work with the institutional entities that meet the state's requirements.
- Nursing Titles.
- Licensed Practical Nurse
- Associate Registered Nurse
- Registered Nurse to Bachelor of Science in Nursing
- Nurse Practitioner
- Professional Technical Titles
- Physician Assistant
- Licensed Mental Health Counselor
- Master of Social Work
- Credentialed Alcoholism and Substance Abuse Counselor
- Certified Pharmacy Technician
- Certified Medical Assistant
- Respiratory Therapist
- Frontline Public Health Workers
- Community Health Worker
- Patient Care Manager/Coordinator
- 12.6 Allowable Use of CPT Funds. The state has authority for CPT expenditures within the limits specified in STC 12.7 for implementation of the CPT initiative. The CPT funds may only be used for the following:
- Educational case management, WIO outreach to secure appropriate program partners, participant recruitment and academic support such as tutoring.
- Program tuition and required program fees for course curriculums necessary to achieve the professional titles in STC 12.5.
- Textbooks and supplies as required by the educational program curriculum.
- Backfill for participants in the Health System Career Advancement Pipeline. To avoid reduced access to care when a participant is in training during participant working hours and recognizing the absence requires a temporary or covering worker to perform duties, the state may use funds to pay the health system employer to backfill the participant. Backfill costs must not exceed the following rates and no more than 2 days per week for participants in the following programs:
- $175 per day for licensed practical nurse, associate registered nurse, credentialed alcohol and substance abuse counselor, certified pharmacy technician, respiratory therapist, certified medical assistant, community health worker, and patient care manager/coordinator.
- $259 per day for nurse practitioners, physician's assistants, Master of Social Work, and licensed mental health counselor.
- $300 per day for Registered Nurse to Bachelor of Science in Nursing.
- Administrative expenses for operational and accounting expenses.
- 12.7 Workforce Initiatives Funding. The funding table below shows the maximum amount of funding for each workforce initiative (including 15 percent administrative costs) by demonstration year.
Table 12: Workforce Initiatives Funding DY 26 DY 27 DY 28 Total 04/01/2024 to 03/31/2025 04/01/2025 to 03/31/2026 04/01/2026 to 03/31/2027 Student Loan Repayment for Qualified Providers $12.08M $24.15M $12.08M $48.30M Career Pathways Training $175.77M $310.48M $159.50M $645.75M Total Computable $187.85M $334.63M $171.58M $694.05M
- Subject to the total funding for each initiative in STC 12.7, the state may carry forward prior year student loan repayment and CPT unused expenditure authority from one year to the next. The state must notify CMS of any changes to annual amounts in the quarterly and annual monitoring reports.
- All expenditures for the student loan repayment and CPT programs are only matchable as administrative expenditures. The state must ensure that the Workforce Initiatives Funding expenditures described in Section 12 are not factored into managed care capitation payments and that there is no duplication of funds.
- The state must require that all CPT participants in programs listed in STC 12.5(a)-(b), make application to the Free Application for Federal Student Aid (FAFSA) and New York State's Tuition Assistance Program (TAP). The WIO may not make tuition payments on behalf of a program participant until both the FAFSA and New York's TAP applications have been submitted and a determination has been made on the amount of grant funding that will be received by the program participant.
- Time limited expenditure authority is granted from April 1, 2027 until March 31, 2031, to allow the state to pay close-out administrative costs of operating the student loan repayment and CPT programs and monitor remaining service commitments. The state must adhere with federal timely filing requirements during this time-limited expenditure authority period. The expenditures will continue to be claimed on the CMS 64 on the specified waiver lines if the date where claims are made go beyond the demonstration period as part of this demonstration period. No payments for student loans, tuition and fees, books and required training supplies, case management, and outreach may be made following the demonstration period's expiration (March 31, 2027).
- The state must follow all federal statutes, regulations, and policies regarding individual eligibility requirements for Federal educational funding support.
- 12.8 Workforce Initiatives Monitoring. The state must report on the student loan repayment and CPT activities in quarterly and annual monitoring reports described in STC 15.16. The state must provide details regarding statewide and regional program recruitment, participation, completion, and status of service commitments. This must include performance rates, progress in reaching statewide targets (e.g., CPT participation by pipeline as described in STC 12.3), and the corrective actions taken if targets are not achieved. Additionally, the state must annually report statewide provider vacancy rates for the professional titles included in the CPT and the student loan repayment programs.
13. HEALTH EQUITY REGIONAL ORGANIZATION (HERO)
The HERO is a contracted statewide entity designed to develop regionally-focused approaches to reduce health disparities, advance health equity, and support the delivery of HRSN services. The HERO will coordinate data from various sources including, but not limited to, the SCNs, WIOs, and the Statewide Health Information Network for New York (SHIN-NY) to assess and address areas for improvement in health care quality and equity outcomes including the identification of disparities in health care delivery. This information will assist New York in developing and designing VBP goals to address HRSN and the most impactful health equity priorities. This authority does not presuppose approval of any particular VBP arrangement submitted by the state under any authority.
- 13.1 HERO Activities - The HERO will conduct the following activities:
- Data aggregation: Data aggregation, analytics, and reporting on statewide demonstration implementation based on managed care organization (MCO)/ SCN/WIO/provider-submitted data, integrating different datasets across health and social services and systems to evaluate needs/ gaps in access to physical health, behavioral health, and HRSN services;
- Regional needs assessment and planning: The HERO will conduct a regional needs assessment as part of its planning, perform data-driven annual regional planning, and draft and publish a statewide health equity plan (informed by regional health equity plans). The assessment must be made publicly available. The HERO will identify health care workforce-related needs and gaps. The state will include managed care contract provisions requiring plans to share data with the HERO;
- Stakeholder engagement: Convene regional stakeholder engagement sessions.
- Make recommendations to support advanced VBP arrangements and develop options for incorporating HRSN into VBP methodologies for the state to use by the end of the demonstration period; and
- Program analysis, such as publishing initial health equity plans and health factor baseline data on Medicaid populations.
- 13.2 Funding. The allowable HERO funding is in the amount $125 million (total computable) for DY 25 through DY 28. Any amount of funding left may roll over from year to year. However, the total computable maximum amount available for HERO over the demonstration period is $125 million. The funding table below shows the maximum amount of funding for the HERO by demonstration year.
Table 13: HERO Funding DY 26 DY 27 DY 28 Total 04/01/2024 to 03/31/2025 04/01/2025 to 03/31/2026 04/01/2026 to 03/31/2027 HERO (Total Computable) Expenditure Authority $50M $40M $35M $125M - 13.3 State Assurances. The state must provide assurances of the following:
- None of the HERO funding may be used to supplant any existing state-only funding.
- None of the HERO funding may be used to support or duplicate any services by the New York eHealth Collaborative (NYeC) or SHIN-NY.
- The HERO must be independent from the state or other government entities.
- The state must ensure that the HERO funding expenditures described in STC 13 are not factored into managed care capitation payments, and that there is no duplication of funds.
- 13.4 Accountability. The state must report on the activities of the HERO in the quarterly and annual monitoring reports. The state must include the recommendations and conclusions based on the HERO's data aggregation, stakeholder engagement, and future VBP arrangements for the delivery of HRSN services to be enacted in the extension request due March 31, 2026.
14. MONITORING AND REPORTING REQUIREMENTS
- 14.1 Deferral for Failure to Submit Timely Demonstration Deliverables. CMS may issue deferrals in accordance with 42 CFR part 430 subpart C, in the amount of $5,000,000 per deliverable (federal share) when items required by these STCs (e.g., required data elements, analyses, reports, design documents, presentations, and other items specified in these STCs) (hereafter singly or collectively referred to as "deliverable(s)") are not submitted timely to CMS or are found to not be consistent with the requirements approved by CMS. A deferral shall not exceed the value of the federal amount for the current demonstration period. The state does not relinquish its rights provided under 42 CFR part 430 subpart C to challenge any CMS finding that the state materially failed to comply with the terms of this agreement.
The following process will be used: 1) thirty (30) days after the deliverable was due if the state has not submitted a written request to CMS for approval of an extension as described in subsection (b) below; or 2) thirty (30) days after CMS has notified the state in writing that the deliverable was not accepted for being inconsistent with the requirements of this agreement and the information needed to bring the deliverable into alignment with CMS requirements:
- CMS will issue a written notification to the state providing advance notification of a pending deferral for late or non-compliant submissions of required deliverable(s).
- For each deliverable, the state may submit to CMS a written request for an extension to submit the required deliverable that includes a supporting rationale for the cause(s) of the delay and the state's anticipated date of submission. Should CMS agree to the state's request, a corresponding extension of the deferral process described below can be provided. CMS may agree to a corrective action plan submitted by the state as an interim step before applying the deferral, if the state proposes a corrective action plan in the state's written extension request.
- If CMS agrees to an interim corrective process in accordance with subsection (b), and the state fails to comply with the corrective action plan or, despite the corrective action plan, still fails to submit the overdue deliverable(s) with all required contents in satisfaction of the terms of this agreement, CMS may proceed with the issuance of a deferral against the next Quarterly Statement of Expenditures reported in Medicaid Budget and Expenditure System/Children's Health Insurance Program Budget and Expenditure System (MBES/CBES) following a written deferral notification to the state.
- If the CMS deferral process has been initiated for state non-compliance with the terms of this agreement with respect to the required deliverable(s), and the state submits the overdue deliverable(s), and such deliverable(s) are accepted by CMS as meeting the standards outline in these STCs, the deferral(s) will be released.
- As the purpose of a section 1115 demonstration is to test new methods of operation or service delivery, a state's failure to submit all required reports, evaluations, and other deliverables will be considered by CMS in reviewing any application for an extension, amendment, or for a new demonstration.
- 14.2 Deferral of FFP from IMD claiming for Insufficient Progress Toward Milestones. Up to $5 million in FFP for services in IMDs may be deferred if the state is not making adequate progress on meeting the milestones and goals as evidenced by reporting on the milestones in STC 8.2 and the required performance measures in the monitoring protocol agreed upon by the state and CMS. Once CMS determines the state has not made adequate progress, up to $5 million will be deferred in the next calendar quarter and each calendar quarter thereafter until CMS has determined sufficient progress has been made.
- 14.3 Submission of Post-Approval Deliverables. The state must submit all required analyses, reports, design documents, presentations, and other items specified in these STCs ("deliverables"). The state shall use the processes as stipulated by CMS and within the timeframes outlined within these STCs.
- 14.4 Compliance with Federal Systems Updates. As federal systems continue to evolve and incorporate section 1115 demonstration reporting and analytics functions, the state will work with CMS to:
- Revise the reporting templates and submission processes to accommodate timely compliance with the requirements of the new systems;
- Ensure all section 1115, Transformed Medicaid Statistical Information System (T-MSIS), and other data elements that have been agreed to for reporting and analytics are provided by the state; and
- Submit deliverables to the appropriate system as directed by CMS.
- 14.5 SUD Monitoring Protocol. The state must submit to CMS a Monitoring Protocol for the SUD program authorized by this demonstration within 150 calendar days after approval of the demonstration amendment. The SUD Monitoring Protocol must be developed in cooperation with CMS and is subject to CMS approval. The state must submit a revised Monitoring Protocol within 60 calendar days after receipt of CMS's comments, if any. Once approved, the SUD Monitoring Protocol will be incorporated into the STCs as Attachment I. Progress on the performance measures identified in the SUD Monitoring Protocol must be reported via the Quarterly and Annual Monitoring Reports. Components of the SUD Monitoring Protocol must include:
- An assurance of the state's commitment and ability to report information relevant to each of the program implementation areas listed in STCs 8.3 and 9.2, and information relevant to the state's HIT Plan described in STCs 8.3;
- A description of the methods of data collection and timeframes for reporting on the state's progress on required measures as part of the general reporting requirements described in Section 14 of the demonstration; and
- A description of baselines and targets to be achieved by the end of the demonstration. Where possible, baselines will be informed by state data, and target will be benchmarked against performance in best practice settings.
- 14.6 Monitoring Protocol for Other Policies. The state must submit to CMS a Monitoring Protocol addressing components of the demonstration not covered by the SUD Monitoring Protocol within 150 calendar days after the approval of the demonstration amendment. The state must submit a revised Monitoring Protocol within 60 calendar days after receipt of CMS's comments, if any. Once approved, the Monitoring Protocol for Other Policies will be incorporated in the STCs as Attachment P. In addition, the state must submit an updated or a separate Monitoring Protocol for any amendments to the demonstration no later than 150 calendar days after the approval of the amendment. Such amendment Monitoring Protocols are subject to same requirement of revisions and CMS approval, as described above.
At a minimum, the Monitoring Protocol must affirm the state's commitment to conduct Quarterly and Annual Monitoring Reports in accordance with CMS's guidance and technical assistance and using CMS-provided reporting templates, if applicable and relevant for different policies. Any proposed deviations from CMS's guidance should be documented in the Monitoring Protocol. The Monitoring Protocol must describe the quantitative and qualitative elements on which the state will report through Quarterly and Annual Monitoring Reports. For the overall demonstration as well as for specific policies where CMS provides states with a suite of quantitative monitoring metrics (e.g., the performance metrics described in STC 14.7), the state is required to calculate and report such metrics leveraging the technical specifications provided by CMS. The Monitoring Protocol must specify the methods of data collection and timeframes for reporting on the demonstration's progress as part of the Quarterly and Annual Monitoring Reports. In alignment with CMS guidance, the Monitoring Protocol must additionally specify the state's plans and timeline on reporting metrics data stratified by key demographic subpopulations of interest (e.g., by sex, age, race/ethnicity, English language proficiency, primary language, disability status, and geography) and demonstration component.
For the HRSN services authorized through this demonstration, the Monitoring Protocol requires specifying a selection of quality of care and health outcomes metrics and population stratifications based on CMS's upcoming guidance on the Disparities-Sensitive Measure Set, and outlining the corresponding data sources and reporting timelines, as applicable to the demonstration initiatives and populations. This set of measures represents a critical set of equity-focused metrics known to be important for closing key equity gaps in Medicaid/CHIP (e.g., the National Quality Forum (NQF) "disparities-sensitive" measures) and prioritizes key outcome measures and their clinical and non-clinical (i.e., social) drivers. The Monitoring Protocol must also outline the state's planned approaches and parameters to track implementation progress and performance relative to the goals and milestones, as provided in the Implementation Plan, for the HRSN infrastructure investments.
The state will also be expected to set up its HRSN service delivery system to allow screening of beneficiaries for identified needs, and to develop an appropriate closed-loop referral system or other feedback loop to ensure beneficiaries receive service referrals and provisions, and provide any applicable update on this process via the Monitoring Reports, in alignment with information provided in the Monitoring Protocol for Other Policies.
In addition, the state must describe in the Monitoring Protocol methods and timeline to collect and analyze non-Medicaid administrative data to help calculate applicable monitoring metrics. These sources may include, but are not limited to: (1) community resource referral platforms; (2) records of social services receipt from other agencies (such as SNAP or TANF benefits, or HUD assistance); (3) other data from social services organizations linked to beneficiaries (e.g., services rendered, resolution of identified need, as applicable); and (4) social needs screening results from electronic health records, health plans, or other partner agencies, as applicable. Across data sources, the state must make efforts and consult with relevant non-Medicaid social service agencies to collect data in ways that support analyses of data on beneficiary subgroups.
For the qualitative elements (e.g., operational updates as described in STC 14.7.a), CMS will provide the state with guidance on narrative and descriptive information, which will supplement the quantitative metrics on key aspects of the demonstration policies. The quantitative and qualitative elements will comprise the state's Monitoring Reports.- 14.7 Quarterly and Annual Monitoring Reports. The state must submit three Quarterly Monitoring Reports and one Annual Monitoring Report each DY. The Quarterly Monitoring Reports are due no later than 60 calendar days following the end of each demonstration quarter. The Annual Monitoring Report (including the fourth-quarter information) is due no later than 90 calendar days following the end of the DY. The state must submit a revised Monitoring Report within 60 calendar days after receipt of CMS's comments, if any. The reports will include all required elements as per 42 CFR 431.428 and should not direct readers to links outside the report. Additional links not referenced in the document may be listed in a Reference/ Bibliography section. The Quarterly and Annual Monitoring Reports must follow the framework to be provided by CMS, which is subject to change as monitoring systems are developed/evolve and be provided in a structured manner that supports federal tracking and analysis.
- Operational Updates - Per 42 CFR 431.428, the Monitoring Reports must document any policy or administrative difficulties in operating the demonstration. The reports must provide sufficient information to document key operational and other challenges, underlying causes of challenges, and how challenges are being addressed. The discussion should also include any issues or complaints identified by beneficiaries; lawsuits or legal actions; unusual or unanticipated trends; legislative updates; and descriptions of any public forums held. In addition, Monitoring Reports should describe key achievements, as well as the conditions and efforts to which these successes can be attributed. Monitoring Reports should also include a summary of all public comments received through post-award public forums regarding the progress of the demonstration. The state must provide in monitoring reports operational progress and any challenges encountered and associated mitigation effects with moving non-emergency medical transportation (NEMT) and pharmacy to FFS.
- Performance Metrics - Per applicable CMS guidance and technical assistance, the performance metrics will provide data to demonstrate how the state is progressing toward meeting the goals and milestones - including relative to their projected timelines - of the demonstration's program and policy implementation and infrastructure investments. Metrics in the state's Monitoring Reports must cover all key policies under this demonstration including, but not limited to, behavioral health, home and community-based services, and the provision of special services to certain populations (for example, through HARP or HIV SNPs), the Medicaid Hospital Global Budget Initiative, Workforce Initiatives, HRSN, HERO, and SUD components. Additionally, per 42 CFR 431.428, the Monitoring Reports must document the effects of the demonstration on beneficiaries' outcomes of care, quality and cost of care, and access to care. This should also include the results of beneficiary satisfaction or experience of care surveys, if conducted, and grievances and appeals. The required monitoring and performance metrics must be included in the Monitoring Reports and must follow the framework provided by CMS to support federal tracking and analysis as applicable.
- The demonstration's metrics reporting must cover categories including, but not limited to enrollment and renewal, including enrollment duration, access to providers, utilization of services, and quality of care and health outcomes. The state must undertake robust reporting of quality of care and health outcomes metrics aligned with the demonstration's policies and objectives, to be reported for all demonstration populations. Such reporting must also be stratified by key demographic subpopulations of interest (e.g., by sex, age, race/ethnicity, English language proficiency, primary language, disability status, and geography) and by demonstration components, to the extent feasible. Subpopulation reporting will support identifying any existing shortcomings or disparities in quality of care and health outcomes and help track whether the demonstration's initiatives help improve outcomes for the state's Medicaid population, including the narrowing of any identified disparities. To that end, CMS underscores the importance of the state's reporting of quality of care and health outcomes metrics known to be important for closing key equity gaps in Medicaid/CHIP (e.g., NQF "disparities-sensitive" measures) and prioritizing key outcome measures and their clinical and non-clinical (i.e. social) drivers of health. In coordination with CMS, the state is expected to select such measures for reporting in alignment with a critical set of equity-focused measures CMS is finalizing as part of its upcoming guidance on the Disparities-Sensitive Measure Set.
- For HRSN components, in addition to reporting on the metrics described above, the state must track beneficiary participation, screening, rescreening, receipt of referrals, recurring nutrition services, and social services over time, as well as narratively report on the adoption of information technology infrastructure to support data sharing between the state or partner entities assisting in the administration of the demonstration and social services organizations, and the contracted providers of applicable services (e.g., managed care plans and their contracted HRSN providers). In alignment with STC 6.17, the state must additionally monitor and provide narrative updates on its progress in building and sustaining its partnership with existing housing and nutrition agencies, leverage their expertise and existing housing and nutrition resources instead of duplicating services. Furthermore, the state's enrollment and renewal metrics must also capture baseline data and track progress via Monitoring Reports for the percent of Medicaid renewals completed ex-parte (administratively), as well as the percentage of Medicaid beneficiaries enrolled in other public benefit programs (such as SNAP and WIC) for which they are eligible. The Monitoring Reports must also provide status updates in accordance with the Monitoring Protocol on the implementation of infrastructure investments tied to the HRSN initiatives.
- For the SUD component, the state's monitoring must cover metrics in alignment with the respective milestones as outlined in the State Medicaid Director Letter (SMDL) dated November 1, 2017 (SMD #17-003).
- For the Workforce Initiatives, the state must report on the student loan repayment and CPT activities in the Monitoring Reports described in STC 14.5. The state must provide details regarding statewide and regional program recruitment, participation, completion, and status of service commitments. This must include performance rates, progress in reaching statewide targets (e.g., CPT participation by pipeline), and the corrective actions taken if targets are not achieved. Additionally, the state must annually report statewide provider vacancy rates for the professional titles included in the CPT and the student loan repayment programs. Narrative should also be included on the operations of the WIOs, including but not limited to WIO data reported to the state, data reported to the HERO, workforce data reporting issues, and general summary information on WIO collaboration with stakeholders and the HERO.
- For the HERO component, the state must provide narrative and data around the HERO's five main operations:
- Data aggregation. Each Monitoring Report should include summary narrative on what data the HERO attained, what is analyzed, and its main findings. Narrative should also be included on which organizations, if any, are having data reporting issues and what steps are being taken to alleviate the problem.
- Regional Needs Assessment and Planning. Each Monitoring Report should include narrative on HERO activities in regard to regional needs assessments, health equity plans, and workforce gaps. The current status of data sharing arrangements with managed care organizations should also be included.
- Stakeholder engagement. Each Monitoring Report should include summaries of any conducted regional stakeholder engagement sessions, which should include attendee information and public comment. If, at any point, stakeholders raise significant concerns with the HERO's performance, Monitoring Reports should include summary of the issue and steps toward resolution.
- Future VBP arrangements. Each Monitoring Report should include status of development of future VBP arrangements. At the initial phase of implementation of the HERO, Monitoring Reports should contain initial stakeholder/state ideas for arrangements and process on how future VBP arrangements will be developed (e.g., what criteria, etc.). For the second year of the HERO's activities, the Monitoring Reports should include preliminary data and takeaways, as well as an initial skeleton proposal of a future VBP arrangement. Final future VBP arrangements should be included in subsequent Monitoring Reports as well as evaluation reports.
- Program Analysis. Monitoring Reports should include an overview of any work done on health equity plans and health factor baseline data.
- For the Medicaid Hospital Global Budget Initiative, Monitoring Reports should include the required data and reports outlined in STC 9.3-9.7, as well as data on relevant quality measures, including their progress toward pre-stipulated targets for the program. By the end of the first year of the initiative's implementation, the state must submit data that confirms each hospital's eligibility in accordance with STC 9.1.a, 9.1.b, and 9.1.c. Reports should include payor mix calculations, operating margin calculations, data on state-only subsidies received, as well as data on hospital uncompensated care costs, including bad debt and charity care. Each Annual Monitoring Report should also include narrative on which hospitals are intending to adopt the AHEAD CMMI model.
- In order to ensure a link between DSHP-funded initiatives and improvements in health equity and beneficiary health outcomes, CMS and the state will coordinate to use the critical set of disparities-sensitive metrics described above, with applicable demographic stratification. In addition, the state must demonstrate through its annual monitoring reporting to CMS improvements in Medicaid fee-for-service base provider reimbursement rates and reimbursement rates for providers enrolled in managed care to the extent required by STC 15.
- As applicable, if the state, health plans, or health care providers will contract or partner with organizations to implement the demonstration, the state must use monitoring metrics that track the number and characteristics of contracted or participating organizations in specific demonstration programs and corresponding payment-related metrics; these metrics are specifically relevant for the state's HRSN initiatives and the DSHP-funded initiatives.
- Budget Neutrality and Financial Reporting Requirements - Per 42 CFR § 431.428, the Monitoring Reports must document the financial performance of the demonstration. The state must provide an updated budget neutrality workbook with every Quarterly and Annual Monitoring Report that meets all the reporting requirements for monitoring budget neutrality set forth in the General Financial Requirements section of these STCs, including the submission of corrected budget neutrality data upon request. In addition, the state must report quarterly and annual expenditures associated with the populations affected by this demonstration on the Form CMS-64. Administrative costs for this demonstration should be reported separately on the CMS-64.
- Evaluation Activities and Interim Findings - Per 42 CFR § 431.428, the Monitoring Reports must document any results of the demonstration to date per the evaluation hypotheses. Additionally, the state shall include a summary of the progress of evaluation activities, including key milestones accomplished, as well as challenges encountered and how they were addressed.
- 14.8 SUD Mid-Point Assessment. The state must contract with an independent entity to conduct an independent Mid-Point Assessment by September 30, 2026. This timeline will allow for the Mid-Point Assessment Report to capture approximately the first two-and-a-half years of demonstration program data, accounting for data run-out and data completeness. In addition, if applicable, the state should use the prior approval period experiences as context, and conduct the Mid-Point Assessment in light of the data from any such prior approval period(s). In the design, planning, and conduct of the Mid-Point Assessment, the state must require that the independent assessor consult with key stakeholders including, but not limited to representatives of MCOs, health care providers (including SUD treatment providers), beneficiaries, community groups, and other key partners.
The state must require that the assessor provide a Mid-Point Assessment Report to the state that includes the methodologies used for examining progress and assessing risk, the limitations of the methodologies, its determinations, and any recommendations. The state must provide a copy of the report to CMS no later than 60 calendar days after September 30, 2026, and the state must brief CMS on the report. The state must submit a revised Mid-Point Assessment Report within 60 calendar days after receipt of CMS's comments, if any.- 14.9 For milestones and measure targets at medium to high risk of not being achieved, the state must submit to CMS proposed modifications to the SUD Implementation Plan and SUD Monitoring Protocol, for ameliorating these risks. Modifications to any of these plans or protocols are subject to CMS approval.
- 14.10 Elements of the Mid-Point Assessment must include at least:
- An examination of progress toward meeting each milestone and timeframe approved in the SUD Implementation Plan, and toward meeting the targets for performance measures as approved in the SUD Monitoring Protocol;
- A determination of factors that affected achievement on the milestones and performance measure gap closure percentage points to date;
- A determination of selected factors likely to affect future performance in meeting milestones and targets not yet met and information about the risk of possibly missing those milestones and performance targets;
- For milestones or targets identified by the independent assessor as at medium to high risk of not being met, recommendations for adjustments in the state's SUD Plan or to other pertinent factors that the state can influence that will support improvement; and
- An assessment of whether the state is on track to meet the budget neutrality requirements in these STCs.
- 14.11 Compliance with Managed Care, Network Adequacy, Quality Strategy and EQR Reporting Requirements. The state must comply with all managed care reporting regulations at 42 CFR Part 438 et. seq., except as expressly identified as not applicable in the expenditure authorities incorporated into these STCs.
- 14.12 Reporting Requirements Related to Individuals using Long Term Services and Supports. In each quarterly report required by STC 14.7 the state shall report:
- Any critical incidents reported within the quarter and the resulting investigations as appropriate.
- The number and types of grievance and appeals for this population filed and/or resolved within the reporting quarter for this population.
- The total number of assessments for enrollment performed by the plans, with the number of individuals who did not qualify to enroll in an MLTC plan.
- The number of individuals referred to an MLTC plan that received an assessment within 30 days.
- The number of people who were not referred by the enrollment broker and contacted the plan directly and were provided MLTC materials.
- Rebalancing efforts performed by the MLTC and MMMC plans once the benefit is added. Rebalancing reporting should include, but is not limited to, the total number of individuals transitioning in and out of a nursing facility within the quarter.
- The total number of complaints, grievances and appeals by type of issue with a listing of the top 5 reasons for the event.
- 14.13 Corrective Action Plan Related to Demonstration Monitoring. If monitoring indicates that demonstration features are not likely to assist in promoting the objectives of Medicaid, CMS reserves the right to require the state to submit a corrective action plan to CMS for approval. A corrective action plan could include a temporary suspension of implementation of demonstration programs in circumstances where monitoring data indicate substantial and sustained directional change inconsistent with demonstration goals, such as substantial and sustained trends indicating increased difficulty accessing services. A corrective action plan may be an interim step to withdrawing waivers or expenditure authorities, as outlined in STC 3.10. CMS will withdraw an authority, as described in STC 3.10, when metrics indicate substantial, sustained directional change, inconsistent with state targets and goals, as applicable, and the state has not implemented corrective action. CMS further has the ability to suspend implementation of the demonstration should corrective actions not effectively resolve these concerns in a timely manner.
- 14.14 Close-Out Report. Within 120 calendar days after the expiration of the demonstration, the state must submit a draft Close-Out Report to CMS for comments.
- The Close-Out Report must comply with the most current guidance from CMS.
- The state will present to and participate in a discussion with CMS on the Close-Out Report.
- The state must take into consideration CMS's comments for incorporation into the final Close-Out Report.
- A revised Close-Out Report is due to CMS no later than 30 calendar days after receipt of CMS's comments.
- A delay in submitting the draft or final version of the Close-Out Report may subject the state to penalties described in STC 14.1.
- 14.15 Monitoring Calls. CMS will convene periodic conference calls with the state.
- The purpose of these calls is to discuss ongoing demonstration operation, including (but not limited to) any significant actual or anticipated developments affecting the demonstration. Examples include implementation activities, trends in reported data on metrics and associated mid-course adjustments, budget neutrality, and progress on evaluation activities.
- CMS will provide updates on any pending actions, as well as federal policies and issues that may affect any aspect of the demonstration.
- The state and CMS will jointly develop the agenda for the calls.
- 14.16 Post Award Forum. Pursuant to 42 CFR 431.420(c), within 6 months of the demonstration's implementation, and annually thereafter, the state must afford the public with an opportunity to provide meaningful comment on the progress of the demonstration. At least 30 days prior to the date of the planned public forum, the state must publish the date, time and location of the forum in a prominent location on its website. The state must also post the most recent Annual Monitoring Report on its website with the public forum announcement. Pursuant to 42 CFR 431.420(c), the state must include a summary of the comments in the Monitoring Report associated with the quarter in which the forum was held, as well as in its compiled Annual Monitoring Report.
15. GENERAL FINANCIAL REQUIREMENTS
- 15.1 Allowable Expenditures. This demonstration project is approved for authorized demonstration expenditures applicable to services rendered and for costs incurred during the demonstration approval period designated by CMS. CMS will provide FFP for allowable demonstration expenditures only so long as they do not exceed the pre-defined limits as specified in these STCs.8
- 15.2 Standard Medicaid Funding Process. The standard Medicaid funding process will be used for this demonstration. The state will provide quarterly expenditure reports through the Medicaid and CHIP Budget and Expenditure System (MBES/CBES) to report total expenditures under this Medicaid section 1115 demonstration following routine CMS-37 and CMS-64 reporting instructions as outlined in section 2500 of the State Medicaid Manual. The state will estimate matchable demonstration expenditures (total computable and federal share) subject to the budget neutrality expenditure limit and separately report these expenditures by quarter for each federal fiscal year on the form CMS-37 for both the medical assistance payments (MAP) and state and local administration costs (ADM). CMS shall make federal funds available based upon the state's estimate, as approved by CMS. Within 30 days after the end of each quarter, the state shall submit form CMS-64 Quarterly Medicaid Expenditure Report, showing Medicaid expenditures made in the quarter just ended. If applicable, subject to the payment deferral process, CMS shall reconcile expenditures reported on form CMS-64 with federal funding previously made available to the state, and include the reconciling adjustment in the finalization of the grant award to the state.
- 15.3 Extent of Federal Financial Participation for the Demonstration. Subject to CMS approval of the source(s) of the non-federal share of funding, CMS will provide FFP at the applicable federal matching rate for the demonstration as a whole for the following, subject to the budget neutrality expenditure limits described in section 16:
- Administrative costs, including those associated with the administration of the demonstration;
- Net expenditures and prior period adjustments of the Medicaid program that are paid in accordance with the approved Medicaid state plan; and
- Medical assistance expenditures and prior period adjustments made under section 1115 demonstration authority with dates of service during the demonstration approval period; including those made in conjunction with the demonstration, net of enrollment fees, cost sharing, pharmacy rebates, and all other types of third-party liability.
- 15.4 Sources of Non-Federal Share. As a condition of demonstration approval, the state certifies that its funds that make up non-federal share are obtained from permissible state and/or local funds that, unless permitted by law, are not other federal funds. The state further certifies federal funds provided under this section 1115 demonstration must not be used as the non-federal share required under any other federal grant or contract, except as permitted by law. CMS approval of this demonstration does not constitute direct or indirect approval of any underlying source of non-federal share or associated funding mechanisms and all sources of non-federal funding must be compliant with section 1903(w) of the Act and applicable regulations. CMS reserves the right to deny FFP in expenditures for which it determines that the sources of non-federal share are impermissible.
- If requested, the state must submit for CMS review and approval documentation of any sources of non-federal share that would be used to support payments under the demonstration.
- If CMS determines that any funding sources are not consistent with applicable federal statutes or regulations, the state must address CMS's concerns within the time frames allotted by CMS.
- Without limitation, CMS may request information about the non-federal share sources for any amendments that CMS determines may financially impact the demonstration.
- 15.5 State Certification of Funding Conditions. As a condition of demonstration approval, the state certifies that the following conditions for non-federal share financing of demonstration expenditures have been met:
- If units of state or local government, including health care providers that are units of state or local government, supply any funds used as non-federal share for expenditures under the demonstration, the state must certify that state or local monies have been expended as the non-federal share of funds under the demonstration in accordance with section 1903(w) of the Act and applicable implementing regulations.
- To the extent the state utilizes certified public expenditures (CPE) as the funding mechanism for the non-federal share of expenditures under the demonstration, the state must obtain CMS approval for a cost reimbursement methodology. This methodology must include a detailed explanation of the process, including any necessary cost reporting protocols, by which the state identifies those costs eligible. The certifying unit of government that incurs costs authorized under the demonstration must certify to the state the amount of public funds allowable under 42 CFR 433.51 it has expended. The federal financial participation paid to match CPEs may not be used as the non-federal share to obtain additional federal funds, except as authorized by federal law, consistent with 42 CFR 433.51(c). for purposes of certifying public expenditures.
- The state may use intergovernmental transfers (IGT) to the extent that the transferred funds are public funds within the meaning of 42 CFR 433.51 and are transferred by units of government within the state. Any transfers from units of government to support the non-federal share of expenditures under the demonstration must be made in an amount not to exceed the non-federal share of the expenditures under the demonstration.
- Under all circumstances, health care providers must retain 100 percent of their payments for or in connection with furnishing covered services to beneficiaries. Moreover, no pre-arranged agreements (contractual, voluntary, or otherwise) may exist between health care providers and state and/or local governments, or third parties to return and/or redirect to the state any portion of the Medicaid payments in a manner inconsistent with the requirements in section 1903(w) of the Act and its implementing regulations. This confirmation of Medicaid payment retention is made with the understanding that payments that are the normal operating expenses of conducting business, such as payments related to taxes, including health care provider-related taxes, fees, business relationships with governments that are unrelated to Medicaid and in which there is no connection to Medicaid payments, are not considered returning and/or redirecting a Medicaid payment.
- The State Medicaid Director or his/her designee certifies that all state and/or local funds used as the state's share of the allowable expenditures reported on the CMS-64 for this demonstration were in accordance with all applicable federal requirements and did not lead to the duplication of any other federal funds.
- 15.6 Financial Integrity for Managed Care Delivery Systems. As a condition of demonstration approval, the state attests to the following, as applicable:
- All risk-based managed care organization, PIHP, and prepaid ambulatory health plan (PAHP) payments, comply with the requirements on payments in 42 CFR 438.6(b)(2), 438.6(c), 438.6(d), 438.8, 438.60 and 438.74.
- 15.7 Requirements for health care related taxes and provider donations. As a condition of demonstration approval, the state attests to the following, as applicable:
- All health care-related taxes as defined by Section 1903(w)(3)(A) of the Social
- Except as provided in paragraph (c) of this STC, all health care-related taxes as defined by Section 1903(w)(3)(A) of the Act and 42 CFR 433.55 are broad-based as defined by Section 1903(w)(3)(B) of the Act and 42 CFR 433.68(c).
- Except as provided in paragraph (c) of this STC, all health care-related taxes are uniform as defined by Section 1903(w)(3)(C) of the Act and 42 CFR 433.68(d).
- If the health care-related tax is either not broad-based or not uniform, the state has applied for and received a waiver of the broad-based and/or uniformity requirements as specified by 1903(w)(3)(E)(i) of the Act and 42 CFR 433.72.
- The tax does not contain a hold harmless arrangement as described by Section 1903(w)(4) of the Act and 42 CFR 433.68(f).
- All provider-related donations as defined by 42 CFR 433.52 are bona fide as defined by Section 1903(w)(2)(B) of the Social Security Act, 42 CFR 433.66, and 42 CFR 433.54.
- 15.8 State Monitoring of Non-federal Share. If any payments under the demonstration are funded in whole or in part by a locality tax, then the state must provide a report to CMS regarding payments under the demonstration no later than 60 days after demonstration approval. This deliverable is subject to the deferral as described in STC 14.1. This report must include:
- A detailed description of and a copy of (as applicable) any agreement, written or otherwise agreed upon, regarding any arrangement among the providers including those with counties, the state, or other entities relating to each locality tax or payments received that are funded by the locality tax;
- Number of providers in each locality of the taxing entities for each locality tax;
- Whether or not all providers in the locality will be paying the assessment for each locality tax;
- The assessment rate that the providers will be paying for each locality tax;
- Whether any providers that pay the assessment will not be receiving payments funded by the assessment;
- Number of providers that receive at least the total assessment back in the form of Medicaid payments for each locality tax;
- The monitoring plan for the taxing arrangement to ensure that the tax complies with section 1903(w)(4) of the Act and 42 CFR 433.68(f); and
- Information on whether the state will be reporting the assessment on the CMS form 64.11A as required under section 1903(w) of the Act.
- 15.9 Extent of Federal Financial Participation for the Demonstration. Subject to CMS approval of the source(s) of the non-federal share of funding, CMS will provide FFP at the applicable federal matching rate for the following demonstration expenditures, subject to the budget neutrality expenditure limits described in the STCs in section 16:
- Administrative costs, including those associated with the administration of the demonstration;
- Net expenditures and prior period adjustments of the Medicaid program that are paid in accordance with the approved Medicaid state plan; and
- Medical assistance expenditures and prior period adjustments made under section 1115 demonstration authority with dates of service during the demonstration extension period; including those made in conjunction with the demonstration, net of enrollment fees, cost sharing, pharmacy rebates, and all other types of third party liability.
- 15.10 Program Integrity. The state must have processes in place to ensure there is no duplication of federal funding for any aspect of the demonstration. The state must also ensure that the state and any of its contractors follow standard program integrity principles and practices including retention of data. All data, financial reporting, and sources of non-federal share are subject to audit.
- 15.11 Medicaid Expenditure Groups (MEGs). MEGs are defined for the purpose of identifying categories of Medicaid or demonstration expenditures subject to budget neutrality, components of budget neutrality expenditure limit calculations, and other purposes related to monitoring and tracking expenditures under the demonstration. The Master MEG Chart table provides a master list of MEGs defined for this demonstration.
Table 14: Main MEG Chart MEG To Which BN Test Does This Apply? Without waiver (WOW) Per Capita WOW Aggregate WW Brief Description TANF Child Main X X Demonstration Population 1 (see Table 1) TANF Adult Main X X Demonstration Population 2 (see Table 1) SSI 0 through-64 Main X X Demonstration Population 3 (see Table 1) SSI 65 and above Main X X Demonstration Population 4 (see Table 1) Non-Duals 18-64 Main X X Demonstration Population 5 (see Table 1) Non-Duals 65+ Main X X Demonstration Population 6 (see Table 1) MLTC Adults 18 -64 Duals Main X X Demonstration Population 7 (see Table 1) MLTC Age 65+ Duals Main X X Demonstration Population 8 (see Table 1) HCBS Expansion Main X Demonstration Population 9: Individuals who are not otherwise eligible, are receiving HCBS, and who are determined to be medically needy based on New York's medically needy income level, after application of community spouse and spousal impoverishment eligibility and post-eligibility rules consistent with section 1924 of the Act. Institution to Community Main X Demonstration Population 10: Individuals moved from institutional nursing facility settings to community settings for long term services and supports who would not otherwise be eligible based on income, but whose income does not exceed the income standard described in STC 4.4(c), and who receive services through the managed long-term care program under the demonstration BH HCBS Main X Demonstration Services 8: Expenditures made for BH HCBS for individuals enrolled in HARPs and HIV SNPs. Note: Expenditures under this EG will be claimed in the manner necessary to ensure the correct claiming of FMAP for all populations (e.g., BH HCBS for the adult expansion groups will be claimed at the FMAP rate at STC 15.15). Demonstration Only Services in MMMC Main X Demonstration Services 9: Expenditures made for provision of residential addiction services, crisis intervention and licensed behavioral health practitioner services to MMMC enrollees only and are not provided under the state plan. New Adult Group Hypo1 X X Demonstration Population 11
- CMS 64.9 VIII Waiv – New Adult Group Newly Eligible
- CMS 64.9VIII Waiv – New Adult Group Not Newly Childless Adults
- CMS 64.9VIII Waiv – New Adult Group Not Newly Children 19-20
- CMS 64.9VIII Waiv – New Adult Group Not Newly Parents & Caretakers
Fo1 Children Hypo2 X X Demonstration Population 12 ADM None Demonstration related administrative costs, as discussed in STC 15.12(d) Transportation Main X All expenditures for Transportation provided under HRSN Cooking Supplies Main X All expenditures for cooking supplies provided under HRSN outside of one-time transitions. Brokerage Fees Main X All expenditures for brokerage fees provided under HRSN HRSN Services Capped Hypo X X All expenditures for certain HRSN initiatives. HRSN Infrastructure Capped Hypo X X All infrastructure expenditures for certain HRSN initiatives. SUD IMD Hypo 3 X X All expenditures for services provided to an individual while they are a patient in an IMD for SUD treatment described in Section 8. Medicaid Hospital Global Budget and Equity Initiative Main X All expenditures for the Medicaid Hospital Global Budget and Equity Initiative described in Section 9. DSHP Main X All expenditures for DSHP described in Section 11. Student Loan Repayment Main X All expenditures for the Student Loan Repayment for Qualified Providers program described in Section 12. CPT Main X All expenditures for the Career Pathways Training program described in Section 12. HERO Main X All expenditures for the HERO described in Section 13. - 15.12 Reporting Expenditures and Member Months. The state must report all demonstration expenditures claimed under the authority of title XIX of the Act and subject to budget neutrality each quarter on separate forms CMS-64.9 WAIVER and/or 64.9P WAIVER, identified by the demonstration project number assigned by CMS (11-W-00114/2). Separate reports must be submitted by MEG (identified by Waiver Name) and Demonstration Year (identified by the two-digit project number extension). Unless specified otherwise, expenditures must be reported by DY according to the dates of service associated with the expenditure. All MEGs identified in the Master MEG Chart as WW must be reported for expenditures, as further detailed in the MEG Detail for Expenditure and Member Month Reporting table below. To enable calculation of the budget neutrality expenditure limits, the state also must report member months of eligibility for specified MEGs.
- Cost Settlements. The state will report any cost settlements attributable to the demonstration on the appropriate prior period adjustment schedules (form CMS-64.9P WAIVER) for the summary sheet line 10b (in lieu of lines 9 or 10c), or line 7. For any cost settlement not attributable to this demonstration, the adjustments should be reported as otherwise instructed in the State Medicaid Manual. Cost settlements must be reported by DY consistent with how the original expenditures were reported.
- Premiums and Cost Sharing Collected by the State. The state will report any premium contributions collected by the state from demonstration enrollees quarterly on the form CMS-64 Summary Sheet line 9D, columns A and B. In order to assure that these collections are properly credited to the demonstration, quarterly premium collections (both total computable and federal share) should also be reported separately by demonstration year on form CMS-64 Narrative, and on the Total Adjustments tab in the Budget Neutrality Monitoring Tool. In the annual calculation of expenditures subject to the budget neutrality expenditure limit, premiums collected in the demonstration year will be offset against expenditures incurred in the demonstration year for determination of the state's compliance with the budget neutrality limits.
- Pharmacy Rebates. Because pharmacy rebates are included in the base expenditures used to determine the budget neutrality expenditure limit, the state must report the portion of pharmacy rebates applicable to the demonstration on the appropriate forms CMS-64.9 WAIVER and 64.9P waiver for the demonstration, and not on any other CMS-64.9 form (to avoid double counting). The state must have a methodology for assigning a portion of pharmacy rebates to the demonstration in a way that reasonably reflects the actual rebate-eligible pharmacy utilization of the demonstration population, and which identifies pharmacy rebate amounts with DYs. Use of the methodology is subject to the approval in advance by the CMS Regional Office, and changes to the methodology must also be approved in advance by the Regional Office. Each rebate amount must be distributed as state and federal revenue consistent with the federal matching rates under which the claim was paid.
- Administrative Costs. The state will separately track and report additional administrative costs that are directly attributable to the demonstration. All administrative costs must be identified on the forms CMS-64.10 WAIVER and/or 64.10P WAIVER. Unless indicated otherwise on the MEG Charts and in the STCs in section 16, administrative costs are not counted in the budget neutrality tests; however, these costs are subject to monitoring by CMS.
- Member Months. As part of the Quarterly and Annual Monitoring Reports described in STC 14.7, the state must report the actual number of "eligible member months" for all demonstration enrollees for all MEGs identified as WOW Per Capita in the Master MEG Chart table above, and as also indicated in the MEG Detail for Expenditure and Member Month Reporting table below. The term "eligible member months" refers to the number of months in which persons enrolled in the demonstration are eligible to receive services. For example, a person who is eligible for three months contributes three eligible member months to the total. Two individuals who are eligible for two months, each contribute two eligible member months, for a total of four eligible member months. The state must submit a statement accompanying the annual report certifying the accuracy of this information.
- Budget Neutrality Specifications Manual. The state will create and maintain a Budget Neutrality Specifications Manual that describes in detail how the state will compile data on actual expenditures related to budget neutrality, including methods used to extract and compile data from the state's Medicaid Management Information System, eligibility system, and accounting systems for reporting on the CMS-64, consistent with the terms of the demonstration. The Budget Neutrality Specifications Manual will also describe how the state compiles counts of Medicaid member months. The Budget Neutrality Specifications Manual must be made available to CMS on request.
Table 15: MEG Detail for Expenditure and Member Month Reporting MEG (Waiver Name) Detailed Description Exclusions CMS-64.9 Line(s) To Use How Expend. Are Assigned to DY MAP or ADM Report Memb er Months (Y/N) MEG Start Date MEG End Date TANF Child Expenditures for medical assistance MMMC benefits for TANF Child Exclude individuals described in Table 2. Exclude BH HCBS and Demonstration Only Services in MMMC. Follow CMS-64.9 Base Category of Service Definitions Date of service MAP Y 10/01/97 3/31/27 TANF Adult Expenditures for medical assistance MMMC benefits for TANF Adult Exclude individuals described in Table 2. Exclude BH HCBS and Demonstration Only Services in MMMC. Follow CMS-64.9 Base Category of Service Definitions Date of service MAP Y 10/01/97 3/31/27 SSI 0 through 64 Expenditures for medical assistance MMMC benefits for SSI 0 through-64 Exclude individuals described in Table 2. Exclude BH HCBS and Demonstration Only Services in MMMC. Follow CMS-64.9 Base Category of Service Definitions Date of service MAP Y 10/01/97 3/31/27 SSI 65 and above Expenditures for medical assistance MMMC benefits for SSI 65 and above Exclude individuals described in Table 2. Exclude BH HCBS and Demonstration Only Services in MMMC. Follow CMS-64.9 Base Category of Service Definitions Date of service MAP Y 10/01/97 3/31/27 Non-Duals 18-64 Expenditures for medical assistance MLTC benefits for Non-Duals 18-64 Exclude individuals described in Table 4. Follow CMS-64.9 Base Category of Service Definitions Date of service MAP Y 8/31/12 3/31/27 Non-Duals 65+ Expenditures for medical assistance MLTC benefits for Non-Duals 65+ Exclude individuals described in Table 4. Follow CMS-64.9 Base Category of Service Definitions Date of service MAP Y 8/31/12 3/31/27 MLTC Adults 18 -64 Duals Expenditures for medical assistance MLTC benefits for MLTC Adults 18 -64 Duals Exclude individuals described in Table 4. Follow CMS-64.9 Base Category of Service Definitions Date of service MAP Y 8/31/12 3/31/27 MLTC Age 65+ Duals Expenditures for medical assistance MLTC benefits for MLTC Age 65+ Duals Exclude individuals described in Table 4. Follow CMS-64.9 Base Category of Service Definitions Date of service MAP Y 8/31/12 3/31/27 HCBS Expansio n Home and community-based services expenditures for Demonstration Population 9 None Line 19A Date of service MAP N 4/08/10 3/31/27 Institution to Communi ty All medical assistance expenditures for Institution to Community None Follow CMS-64.9 Base Category of Service Definitions Date of service MAP N 8/31/12 3/31/27 BH HCBS All medical assistance expenditures for BH HCBS None Line 19A Date of service MAP N 7/29/15 3/31/25 Demonstr ation Only Services in MMMC All medical assistance expenditures and Demonstration Only Services in MMMC None Follow CMS-64.9 Base Category of Service Definitions Date of service MAP N 7/29/15 3/31/27 New Adult Group Expenditures for medical assistance for New Adult Group None Follow CMS-64.9 Base Category of Service Definitions Date of service MAP Y 1/01/14 3/31/27 Fo1 Children All medical assistance expenditures for Fo1 Children None Follow CMS-64.9 Base Category of Service Definitions Date of service MAP Y 4/01/19 3/31/27 ADM Demonstration related administrative costs, as discussed in STC 1616.10(e) None Follow CMS-64.10 Base Category of Service Definitions Date of payment ADM N 10/01/97 3/31/27 HRSN Services Reimburse the state for expenditures on HRSN services None Follow CMS-64.9 Base Category of Service Definitions Date of service MAP N 1/09/24 3/31/27 HRSN Infrastruct ure Reimburse the state for expenditures on HRSN infrastructure None Follow CMS-64.10 Base Category of Service Definitions Date of service ADM N 1/09/24 3/31/27 Transport ation Report all expenditure for the transportation benefit under HRSN None Follow CMS-64.10 Base Category of Service Definitions Date of service ADM N 1/09/24 3/31/27 Cooking Supplies Report all expenditure for the cooking supplies benefit under HRSN None Follow CMS-64.10 Base Category of Service Definitions Date of service ADM N 1/09/24 3/31/27 Brokerage Fees Report all expenditures for the brokerage fee benefit under HRSN None Follow CMS-64.10 Base Category of Service Definitions Date of service ADM N 1/09/24 3/31/27 DSHP Report all DSHP expenditures. None Follow CMS-64.10 Base Category of Service Definitions Date of service ADM N 1/09/24 3/31/27 HERO Report all HERO expenditures None Follow CMS-64.10 Base Category of Service Definitions Date of service ADM N 1/09/24 3/31/27 Medicaid Hospital Global Budget Initiative Report all Medicaid Hospital Global Budget Initiative expenditures None Follow CMS-64.10 Base Category of Service Definitions Date of service ADM N 1/09/24 3/31/27 SUD IMD TANF Children 1-20 Report all medical assistance expenditures for services provided to an individual while they are a patient in an IMD for SUD treatment described in Section 8. None Follow CMS-64.9 Base Category of Service Definitions Date of service MAP Y 1/09/24 3/31/27 SUD IMD TANF Adults 21-64 Report all medical assistance expenditures for services provided to an individual while they are a patient in an IMD for SUD treatment described in Section 8. None Follow CMS-64.9 Base Category of Service Definitions Date of service MAP Y 1/09/24 3/31/27 SUD IMD SSI 0-64 Report all medical assistance expenditures for services provided to an individual while they are a patient in an IMD for SUD treatment described in Section 8. None Follow CMS-64.9 Base Category of Service Definitions Date of service MAP Y 1/09/24 3/31/27 SUD IMD New Adult Group Report all medical assistance expenditures for services provided to an individual while they are a patient in an IMD for SUD treatment described in Section 8. None Follow CMS-64.9 Base Category of Service Definitions Date of service MAP Y 1/09/24 3/31/27 SUD IMD FFS Report all medical assistance expenditures for services provided to an individual while they are a patient in an IMD for SUD treatment described in Section 8. None Follow CMS-64.9 Base Category of Service Definitions Date of service MAP Y 1/09/24 3/31/27 Student Loan Repayme nt Report all expenditures for the student loan repayment program. None Follow CMS-64.10 Base Category of Service Definitions Date of payment ADM N 1/09/24 3/31/27 CPT Report all expenditures for the Career Pathways Training initiative. None Follow CMS-64.10 Base Category of Service Definitions Date of payment ADM N 1/09/24 3/31/27 - 15.13 Demonstration Years. Demonstration Years (DY) for this demonstration are defined in the Demonstration Years table below.
Table 16: Demonstration Years Demonstration Year 24 April 1, 2022 to March 31, 2023 12 months Demonstration Year 25 April 1, 2023 to March 31, 2024 12 months Demonstration Year 26 April 1, 2024 to March 31, 2025 12 months Demonstration Year 27 April 1, 2025 to March 31, 2026 12 months Demonstration Year 28 April 1, 2026 to March 31, 2027 12 months - 15.14 Calculating the Federal Medical Assistance Percentage (FMAP) for Continuous Eligibility for the Adult Group. Because not all "newly eligible" individuals in the Adult Group as defined in 42 CFR 433.204(a)(1) would be eligible for the entire continuous eligibility period if the state conducted redeterminations, CMS has determined that 97.4 percent of expenditures for individuals defined in 42 CFR 433.204(a)(1) will be matched at the "newly eligible" FMAP rate as defined in 42 CFR 433.10(c)(6) and 2.6 percent will be matched at the state's regular title XIX FMAP rate. Should state data indicate that there is an estimate more accurate than 2.6 percent by which to adjust claiming for individuals defined in 42 CFR 433.204(a)(1), CMS will work with the state to update this percentage to the more accurate figure, as supported by the state's proposed methodology and data.
- 15.15 State Reporting for the Continuous Eligibility FMAP Adjustment. 97.4 percent of expenditures for "newly eligible" individuals in the Adult Group as defined in 42 CFR 433.204(a)(1) shall be claimed at the "newly eligible" FMAP rate as defined in 42 CFR 433.10(c)(6), unless otherwise adjusted as described in STC 15.14 above. The state must make adjustments on the applicable CMS-64 waiver forms to claim the remaining 2.6 percent or other applicable percentage of expenditures for individuals defined in 42 CFR 433.204(a)(1) at the state's regular Title XIX FMAP rate.
- 15.16 Budget Neutrality Monitoring Tool. The state must provide CMS with quarterly budget neutrality status updates, including established baseline and member months data, using the Budget Neutrality Monitoring Tool provided through the PMDA system. The tool incorporates the "Schedule C Report" for comparing demonstration's actual expenditures to the budget neutrality expenditure limits described in section 16. CMS will provide technical assistance, upon request.9
- 15.17 Claiming Period. The state will report all claims for expenditures subject to the budget neutrality agreement (including any cost settlements) within two years after the calendar quarter in which the state made the expenditures. All claims for services during the demonstration period (including any cost settlements) must be made within two years after the conclusion or termination of the demonstration. During the latter two-year period, the state will continue to identify separately net expenditures related to dates of service during the operation of the demonstration on the CMS-64 waiver forms in order to properly account for these expenditures in determining budget neutrality.
- 15.18 Future Adjustments to Budget Neutrality. CMS reserves the right to adjust the budget neutrality expenditure limit:
- To be consistent with enforcement of laws and policy statements, including regulations and guidance, regarding impermissible provider payments, health care related taxes, or other payments, CMS reserves the right to make adjustments to the budget neutrality limit if any health care related tax that was in effect during the base year, or provider-related donation that occurred during the base year, is determined by CMS to be in violation of the provider donation and health care related tax provisions of section 1903(w) of the Act. Adjustments to annual budget targets will reflect the phase out of impermissible provider payments by law or regulation, where applicable.
- To the extent that a change in federal law, regulation, or policy requires either a reduction or an increase in FFP for expenditures made under this demonstration. In this circumstance, the state must adopt, subject to CMS approval, a modified budget neutrality agreement as necessary to comply with such change. The modified agreement will be effective upon the implementation of the change. The trend rates for the budget neutrality agreement are not subject to change under this STC. The state agrees that if mandated changes in the federal law require state legislation, the changes shall take effect on the day such state legislation becomes effective, or on the last day such legislation was required to be in effect under the federal law.
- The state certifies that the data it provided to establish the budget neutrality expenditure limit are accurate based on the state's accounting of recorded historical expenditures or the next best available data, that the data are allowable in accordance with applicable federal, state, and local statutes, regulations, and policies, and that the data are correct to the best of the state's knowledge and belief. The data supplied by the state to set the budget neutrality expenditure limit are subject to review and audit, and if found to be inaccurate, will result in a modified budget neutrality expenditure limit.
- 15.19 Budget Neutrality Mid-Course Correction Adjustment Request. No more than once per demonstration year, the state may request that CMS make an adjustment to its budget neutrality agreement based on changes to the state's Medicaid expenditures that are unrelated to the demonstration and/or outside the state's control, and/or that result from a new expenditure that is not a new demonstration-covered service or population and that is likely to further strengthen access to care.
- Contents of Request and Process. In its request, the state must provide a description of the expenditure changes that led to the request, together with applicable expenditure data demonstrating that due to these expenditures, the state's actual costs have exceeded the budget neutrality cost limits established at demonstration approval. The state must also submit the budget neutrality update described in STC 15.19.c. If approved, an adjustment could be applied retrospectively to when the state began incurring the relevant expenditures, if appropriate. Within 120 days of acknowledging receipt of the request, CMS will determine whether the state needs to submit an amendment pursuant to STC 3.7. CMS will evaluate each request based on its merit and will approve requests when the state establishes that an adjustment to its budget neutrality agreement is necessary due to changes to the state's Medicaid expenditures that are unrelated to the demonstration and/or outside of the state's control, and/or that result from a new expenditure that is not a new demonstration-covered service or population and that is likely to further strengthen access to care.
- Types of Allowable Changes. Adjustments will be made only for actual costs as reported in expenditure data. CMS will not approve mid-demonstration adjustments for anticipated factors not yet reflected in such expenditure data. Examples of the types of mid-course adjustments that CMS might approve include the following:
- Provider rate increases that are anticipated to further strengthen access to care;
- CMS or state technical errors in the original budget neutrality formulation applied retrospectively, including, but not limited to the following:
mathematical errors, such as not aging data correctly; or unintended omission of certain applicable costs of services for individual MEGs;- Changes in federal statute or regulations, not directly associated with Medicaid, which impact expenditures;
- State legislated or regulatory change to Medicaid that significantly affects the costs of medical assistance;
- When not already accounted for under Emergency Medicaid 1115 demonstrations, cost impacts from public health emergencies;
- High cost innovative medical treatments that states are required to cover; or,
- Corrections to coverage/service estimates where there is no prior state experience (e.g., SUD) or small populations where expenditures may vary widely.
- Budget Neutrality Update. The state must submit an updated budget neutrality analysis with its adjustment request, which includes the following elements:
- Projected without waiver and with waiver expenditures, estimated member months, and annual limits for each DY through the end of the approval period; and,
- Description of the rationale for the mid-course correction, including an explanation of why the request is based on changes to the state's Medicaid expenditures that are unrelated to the demonstration and/or outside the state's control, and/or is due to a new expenditure that is not a new demonstration-covered service or population and that is likely to further strengthen access to care.
16. MONITORING BUDGET NEUTRALITY
- 16.1 Limit on Title XIX Funding. The state will be subject to limits on the amount of federal Medicaid funding the state may receive over the course of the demonstration approval. The budget neutrality expenditure limits are based on projections of the amount of FFP that the state would likely have received in the absence of the demonstration. The limit consists of a Main Budget Neutrality Test, one or more Hypothetical Budget Neutrality Tests, and a Capped Hypothetical Budget Neutrality Test, if applicable, as described below. CMS's assessment of the state's compliance with these tests will be based on the Schedule C CMS-64 Waiver Expenditure Report, which summarizes the expenditures reported by the state on the CMS-64 that pertain to the demonstration.
- 16.2 Risk. The budget neutrality expenditure limits are determined on either a per capita or aggregate basis as described in Table 17, Master MEG Chart and Table 13, MEG Detail for Expenditure and Member Month Reporting. If a per capita method is used, the state is at risk for the per capita cost of state plan and hypothetical populations, but not for the number of participants in the demonstration population. By providing FFP without regard to enrollment in the demonstration for all demonstration populations, CMS will not place the state at risk for changing economic conditions, however, by placing the state at risk for the per capita costs of the demonstration populations, CMS assures that the demonstration expenditures do not exceed the levels that would have been realized had there been no demonstration. If an aggregate method is used, the state accepts risk for both enrollment and per capita costs.
- 16.3 Calculation of the Budget Neutrality Limits and How They Are Applied. To calculate the budget neutrality limits for the demonstration, separate annual budget limits are determined for each DY on a total computable basis. Each annual budget limit is the sum of one or more components: per capita components, which are calculated as a projected without-waiver per member per month (PMPM) cost times the corresponding actual number of member months, and aggregate components, which project fixed total computable dollar expenditure amounts. The annual limits for all DYs are then added together to obtain a budget neutrality limit for the entire demonstration period. The federal share of this limit will represent the maximum amount of FFP that the state may receive during the demonstration period for the types of demonstration expenditures described below. The federal share will be calculated by multiplying the total computable budget neutrality expenditure limit by the appropriate Composite Federal Share.
- 16.4 Main Budget Neutrality Test. The Main Budget Neutrality Test allows the state to show that approval of the demonstration has not resulted in Medicaid costs to the federal government that are greater than what the federal government's Medicaid costs would likely have been absent the demonstration, and that federal Medicaid "savings" have been achieved sufficient to offset the additional projected federal costs resulting from expenditure authority. The table below identifies the MEGs that are used for the Main Budget Neutrality Test. MEGs designated as "WOW Only" or "Both" are components used to calculate the budget neutrality expenditure limit. MEGs that are indicated as "WW Only" or "Both" are counted as expenditures against the budget neutrality expenditure limit. In addition, any expenditures in excess of the limit from Hypothetical Budget Neutrality Tests count as expenditures under the Main Budget Neutrality Test. However, excess expenditures from the Capped Hypothetical Budget Neutrality Test do not count as expenditures under the Main Budget Neutrality Test. The state is at risk for any amount over the capped hypothetical amount. The Composite Federal Share for this test is calculated based on all MEGs indicated as "Both."
*PC = Per Capita, Agg = Aggregate
Table 17: Main Budget Neutrality Test MEG PC or Agg* WOW Only, WW Only, or Both BASE YEAR SFY 2020 TREND DY 24 DY 25 DY 26 DY 27 DY 28 TANF Child PC Both $274.63 2.8% $280.79 $307.49 $316.30 $325.36 $334.68 TANF Adult PC Both $724.05 5.3% $645.25 $813.50 $837.54 $862.29 $887.77 SSI 0 through 64 PC Both $2,126.11 4.3% $1,482.78 $2,623.27 $2,764.76 $2,913.88 $3,071.04 SSI 65 and above PC Both $1,973.08 3.9% $1,258.60 $2,434.45 $2,565.75 $2,704.14 $2,849.99 Non-Duals 18-64 PC Both $6,763.46 4.3% $7,099.76 $6,990.06 $7,047.89 $7,106.20 $7,164.99 Non-Duals 65+ PC Both $6,574.94 3.9% $4,683.43 $6,795.23 $6,85145 $6,908.13 $6,965.28 MLTC Adults 18-64 Duals PC Both $3,643.74 4.3% $4,399.60 $3,765.82 $3,796.97 $3,828.38 $3,860.05 MLTC Age 65+ Duals PC Both $5,073.30 3.9% $4,655.45 $5,243.28 $5,286.26 $5,330.40 $5,374.50 HCBS Expansion Agg WW only n/a n/a n/a n/a n/a n/a n/a Institution to Community Agg WW only n/a n/a n/a n/a n/a n/a n/a BH HCBS Agg WW only n/a n/a n/a n/a n/a n/a n/a Demonstration Only Services in MMMC Agg WW only n/a n/a n/a n/a n/a n/a n/a Transportation Agg WW Only n/a n/a n/a n/a n/a n/a n/a Cooking Supplies Agg WW Only n/a n/a n/a n/a n/a n/a n/a Brokerage Fees Agg WW Only n/a n/a n/a n/a n/a n/a n/a Student Loan Repayment Agg WW only n/a n/a n/a n/a n/a n/a n/a CPT Agg WW only n/a n/a n/a n/a n/a n/a n/a SUD TANF 1-20 PC Hypo $298.35 4.9% n/a $312.97 $328.31 $344.40 $361.28 SUD TANF 21-64 PC Hypo $845.39 4.8% n/a $885.97 $928.50 $973.07 $1,019.78 SUD SSI 0-64 PC Hypo $2,412.34 5.0% n/a $2,532.96 $2,659.61 $2,792.59 $2,932.22 SUD New Adult PC Hypo $739.66 4.6% n/a $773.68 $809.27 $846.50 $885.44 SUD PC Hypo $7,449.29 4.8% n/a $7,806.86 $8,181.59 $8,574.31 $8,985.88 HERO Agg WW only n/a n/a n/a n/a n/a n/a n/a DSHP Agg WW only n/a n/a n/a n/a n/a n/a n/a Medicaid Hospital Agg WW only n/a n/a n/a n/a n/a n/a n/a Global Budget Initiative - 16.5 Hypothetical Budget Neutrality. When expenditure authority is provided for coverage of populations or services that the state could have otherwise provided through its Medicaid state plan or other title XIX authority (such as a waiver under section 1915 of the Act), or when a WOW spending baseline for certain WW expenditures is difficult to estimate due to variable and volatile cost data resulting in anomalous trend rates, CMS considers these expenditures to be "hypothetical," such that the expenditures are treated as if the state could have received FFP for them absent the demonstration. For these hypothetical expenditures, CMS makes adjustments to the budget neutrality test which effectively treats these expenditures as if they were for approved Medicaid state plan services. Hypothetical expenditures, therefore, do not necessitate savings to offset the expenditures on those services. When evaluating budget neutrality, however, CMS does not offset non-hypothetical expenditures with projected or accrued savings from hypothetical expenditures; that is, savings are not generated from a hypothetical population or service. To allow for hypothetical expenditures, while preventing them from resulting in savings, CMS currently applies separate, independent Hypothetical Budget Neutrality Tests, which subject hypothetical expenditures to pre-determined limits to which the state and CMS agree, and that CMS approves, as a part of this demonstration approval. If the state's WW hypothetical spending exceeds the Hypothetical Budget Neutrality Test's expenditure limit, the state agrees (as a condition of CMS approval) to offset that excess spending through savings elsewhere in the demonstration or to refund the FFP to CMS.
- Hypothetical Budget Neutrality Test 1: New Adult Group. The table below identifies the MEGs that are used for Hypothetical Budget Neutrality Test 1. MEGs that are designated "WOW Only" or "Both" are the components used to calculate the budget neutrality expenditure limit. The Composite Federal Share for the Hypothetical Budget Neutrality Test is calculated based on all MEGs indicated as "WW Only" or "Both." MEGs that are indicated as "WW Only" or "Both" are counted as expenditures against this budget neutrality expenditure limit. Any expenditures in excess of the limit from Hypothetical Budget Neutrality Test are counted as WW expenditures under the Main Budget Neutrality Test.
Table 18: New Adult Group MEG PC or Agg* WOW Only, WW Only, or Both BASE YEAR SFY 2020 TREND DY 24 DY 25 DY 26 DY 27 DY 28 New Adult Group PC Both $624.56 5.8% $739.66 $782.56 $827.95 $875.97 $926.78 - Hypothetical Budget Neutrality Test 2: Fo1 Children. The table below identifies the MEGs that are used for Hypothetical Budget Neutrality Test 2. MEGs that are designated "WOW Only" or "Both" are the components used to calculate the budget neutrality expenditure limit. The Composite Federal Share for the Hypothetical Budget Neutrality Test is calculated based on all MEGs indicated as "WW Only" or "Both." MEGs that are indicated as "WW Only" or "Both" are counted as expenditures against this budget neutrality expenditure limit. Any expenditures in excess of the limit from Hypothetical Budget Neutrality Test are counted as WW expenditures under the Main Budget Neutrality Test.
Table 19: Fo1 Children MEG PC or Agg* WOW Only, WW Only, or Both BASE YEAR SFY 2020 TREND DY 24 DY 25 DY 26 DY 27 DY 28 Fo1 Children PC Both $4,764.24 0% $4,764.24 $4,764.24 $4,764.24 $4,764.24 $4,764.24 - Hypothetical Budget Neutrality Test 3: SUD. The table below identifies the MEGs that are used for Hypothetical Budget Neutrality Test 3. MEGs that are designated "WOW Only" or "Both" are the components used to calculate the budget neutrality expenditure limit. The Composite Federal Share for the Hypothetical Budget Neutrality Test is calculated based on all MEGs indicated as "WW Only" or "Both." MEGs that are indicated as "WW Only" or "Both" are counted as expenditures against this budget neutrality expenditure limit. Any expenditures in excess of the limit from Hypothetical Budget Neutrality Test 3 are counted as WW expenditures under the Main Budget Neutrality Test.
Table 20: SUD IMD Expenditures MEG PC or Agg* WOW Only, WW Only, or Both BASE YEAR SFY 2023 TREND DY 24 DY 25 DY 26 DY 27 DY 28 SUD IMD TANF Children 1-20 PC Both $845.39 4.8% N/A $312.97 $328.31 $344.40 $361.28 SUD IMD TANF Adults 21-64 PC Both $845.39 4.8% N/A $312.97 $328.31 $344.40 $361.28 SUD IMD SSI 0-64 PC Both $2,412,34 5.0% N/A $2,532.96 $2,659.611 $2,792.59 $2,932.22 SUD IMD New Adult Group PC Both $739.66 4.6% N/A $773.68 $809.27 $846.50 $885.44 SUD IMD FFS PC Both $7,449.29 4.8% N/A $7,806.86 $8,181.59 $8,574.31 $8,985.88 - 16.6 Capped Hypothetical Budget Neutrality for Evidence-Based HRSN Initiatives. When expenditure authority is provided for specified HRSN initiatives in the demonstration (in this approval, as specified in section 6), CMS considers these expenditures to be "capped hypothetical" expenditures; that is, the expenditures are eligible to receive FFP up to a specific aggregate spending cap per demonstration year, based on the state's expected expenditures. States can also receive FFP for capacity-building, infrastructure, and operational costs for the HRSN initiatives; this FFP is limited by a sub-cap of the aggregate spending cap and is determined by CMS based on the amount the state expects to spend. Like all hypothetical expenditures, capped hypothetical expenditures do not need to be offset by savings, and cannot produce savings; however, unspent expenditure authority allocated for HRSN infrastructure in a given demonstration year can be applied to HRSN services in the same demonstration year. Any unspent HRSN services expenditure authority may not be used to fund HRSN infrastructure. To allow for capped hypothetical expenditures and to prevent them from resulting in savings that would apply to the rest of the demonstration, CMS currently applies a separate, independent Capped Hypothetical Budget Neutrality Test, which subjects capped hypothetical expenditures to pre-determined aggregate limits to which the state and CMS agree, and that CMS approves, as a part of this demonstration approval. If actual HRSN initiative spending is less than the Capped Hypothetical Budget Neutrality Test's expenditure limit for a given demonstration year, the difference is not considered demonstration savings. Unspent HRSN expenditure authority under the cap for each demonstration year can be carried, shifted, or transferred across future demonstration years. However, unspent HRSN expenditure authority cannot roll over to the next demonstration approval period. If the state's capped hypothetical spending exceeds the Capped Hypothetical Budget Neutrality Test's expenditure limit, the state agrees (as a condition of CMS approval) to refund any FFP in excess of the cap to CMS. Demonstration savings from the Main Budget Neutrality Test cannot be used to offset excess spending for the capped hypothetical.
- 16.7 Capped Hypothetical Budget Neutrality Test: HRSN. The table below identifies the MEGs that are used for the Capped Hypothetical Budget Neutrality Test. MEGs that are designated "WOW Only" or "Both" are the components used to calculate the budget neutrality expenditure limit. The Composite Federal Share for the Capped Hypothetical Budget Neutrality Test is calculated based on all MEGs indicated as "WW Only" or "Both." MEGs that are indicated as "WW Only" or "Both" are counted as expenditures against this budget neutrality expenditure limit. Any expenditures in excess of the limit from the Capped Hypothetical Budget Neutrality Test cannot be offset by savings under the Main Budget Neutrality Test or the Hypothetical Budget Neutrality Tests.
Table 21: Capped Hypothetical Budget Neutrality Test MEG PC or Agg* WOW Only, WW Only, or Both DY 24 DY 25 DY 26 DY 27 DY 28 HRSN Services Agg Both n/a n/a $766,098,515 $1,105,504,87 1 $2,190,343,07 6 HRSN Infrastructure Agg Both n/a $20,000,000 $275,000,000 $225,000,000 $79,990,000 - 16.8 Composite Federal Share. The Composite Federal Share is the ratio that will be used to convert the total computable budget neutrality limit to federal share. The Composite Federal Share is the ratio calculated by dividing the sum total of FFP received by the state on actual demonstration expenditures during the approval period by total computable demonstration expenditures for the same period, as reported through MBES/CBES and summarized on Schedule C. Since the actual final Composite Federal Share will not be known until the end of the demonstration's approval period, for the purpose of interim monitoring of budget neutrality, a reasonable estimate of Composite Federal Share may be developed and used through the same process or through an alternative mutually agreed to method. Each Main or Hypothetical Budget Neutrality Test has its own Composite Federal Share, as defined in the paragraph pertaining to each particular test.
- 16.9 Corrective Action Plan. If at any time during the demonstration approval period CMS determines that the demonstration is on course to exceed its budget neutrality expenditure limit, CMS will require the state to submit a corrective action plan for CMS review and approval. CMS will use the threshold levels in the table below as a guide for determining when corrective action is required.
Table 22: Budget Neutrality Test Corrective Action Plan Calculation Demonstration Year Cumulative Target Definition Percentage DY 1 Cumulative budget neutrality limit plus: 2.0 percent DY 1 through DY 2 Cumulative budget neutrality limit plus: 1.5 percent DY 1 through DY 3 Cumulative budget neutrality limit plus: 1.0 percent DY 1 through DY 4 Cumulative budget neutrality limit plus: 0.5 percent DY 1 through DY 5 Cumulative budget neutrality limit plus: 0.0 percent 17. EVALUATION OF THE DEMONSTRATION
- 17.1 Cooperation with Federal Evaluators and Learning Collaborative. As required under 42 CFR 431.420(f), the state must cooperate fully and timely with CMS and its contractors in any federal evaluation of the demonstration or any component of the demonstration. This includes, but is not limited to, commenting on design and other federal evaluation documents and providing data and analytic files to CMS, including entering into a data use agreement that explains how the data and data files will be exchanged, and providing a technical point of contact to support specification of the data and files to be disclosed, as well as relevant data dictionaries and record layouts. The state must include in its contracts with entities who collect, produce or maintain data and files for the demonstration, that they must make such data available for the federal evaluation as is required under 42 CFR 431.420(f) to support federal evaluation. This may also include the state's participation–including representation from the state's contractors, independent evaluators, and organizations associated with the demonstration operations, as applicable–in a federal learning collaborative aimed at cross state technical assistance, and identification of lessons learned and best practices for demonstration measurement, data development, implementation, monitoring, and evaluation. The state may claim administrative match for these activities. Failure to comply with this STC may result in a deferral being issued as outlined in Section 14.1.
- 17.2 Independent Evaluator. The state must use an independent party to conduct an evaluation of the demonstration to ensure that the necessary data is collected at the level of detail needed to research the approved hypotheses. The independent party must sign an agreement to conduct the demonstration evaluation in an independent manner in accordance with the CMS-approved Evaluation Design. When conducting analyses and developing the evaluation reports, every effort should be made to follow the approved methodology. However, the state may request, and CMS may agree to, changes in the methodology in appropriate circumstances.
- 17.3 Draft Evaluation Design. The state must submit, for CMS comment and approval, a draft Evaluation Design no later than 180 calendar days after the approval date of the demonstration. Any modifications to an existing approved Evaluation Design will not affect previously established requirements and timelines for report submission for the demonstration, if applicable. The draft Evaluation Design must be drafted in accordance with Attachment G (Evaluation Design) of these STCs, and any applicable evaluation guidance and technical assistance for the demonstration's policy components. The Evaluation Design must also be developed in alignment with CMS guidance on applying robust evaluation approaches, such as quasi-experimental methods like difference-in-differences and interrupted time series, as well as establishing valid comparison groups and assuring causal inferences in demonstration evaluations. In addition to these requirements, if determined culturally appropriate for the communities impacted by the demonstration, the state is encouraged to consider implementation approaches involving randomized control trials and staged rollout (for example, across geographic areas, by service setting, or by beneficiary characteristic)–as these implementation strategies help create strong comparison groups and facilitate robust evaluation.
The state is strongly encouraged to use the expertise of the independent party in the development of the draft Evaluation Design. The draft Evaluation Design also must include a timeline for key evaluation activities, including the deliverables outlined in STC 18.
For any amendment to the demonstration, the state will be required to update the approved Evaluation Design to accommodate the amendment components. The amended Evaluation Design must be submitted to CMS for review no later than 180 calendar days after CMS's approval of the demonstration amendment. Depending on the scope and timing of the amendment, in consultation with CMS, the state may provide the details on necessary modifications to the approved Evaluation Design via the monitoring reports.
The amendment Evaluation Design must also be reflected in the state's Interim and Summative Evaluation Reports, described below.- 17.4 Evaluation Budget. A budget for the evaluation must be provided with the draft Evaluation Design. It will include the total estimated cost, as well as a breakdown of estimated staff, administrative and other costs for all aspects of the evaluation, such as any survey and measurement development, quantitative and qualitative data collection and cleaning, analyses, and report generation. A justification of the costs may be required by CMS if the estimates provided do not appear to sufficiently cover the costs of the design or if CMS finds that the design is not sufficiently developed, or if the estimates appear to be excessive.
- 17.5 Evaluation Design Approval and Updates. The state must submit a revised draft Evaluation Design within 60 calendar days after receipt of CMS's comments, if any. Upon CMS approval of the draft Evaluation Design, the document will be included as an attachment to these STCs. Per 42 CFR 431.424(c), the state will publish the approved Evaluation Design to the state's website within 30 calendar days of CMS approval. The state must implement the Evaluation Design and submit a description of its evaluation implementation progress in each of the Monitoring Reports. Once CMS approves the Evaluation Design, if the state wishes to make changes, the state must submit a revised Evaluation Design to CMS for approval if the changes are substantial in scope; otherwise, in consultation with CMS, the state may include updates to the Evaluation Design in Monitoring Reports.
- 17.6 Evaluation Questions and Hypotheses. Consistent with Attachments E and F (Developing the Evaluation Design and Preparing the Interim and Summative Evaluation Reports) of these STCs, the evaluation deliverables must include a discussion of the evaluation questions and hypotheses that the state intends to test. In alignment with applicable CMS evaluation guidance and technical assistance, the evaluation must outline and address well-crafted hypotheses and research questions for all key demonstration policy components that support understanding the demonstration's impact and its effectiveness in achieving the goals.
The hypothesis testing should include, where possible, assessment of both process and outcome measures. Proposed measures should be selected from nationally recognized sources and national measures sets, where possible. Measures sets could include CMS's Core Set of Health Care Quality Measures for Children in Medicaid and CHIP (Child Core Set) and the Core Set of Adult Health Care Quality Measures for Medicaid (Adult Core Set), collectively referred to as the CMS Child and Adult Core Measure Sets for Medicaid and CHIP; Consumer Assessment of Health Care Providers and Systems (CAHPS); the Behavioral Risk Factor Surveillance System (BRFSS) survey; and/or measures endorsed by NQF.
CMS underscores the importance of the state undertaking a well-designed beneficiary survey and/or interviews to assess, for instance, beneficiary understanding of and experience with the various demonstration policy components, including but not limited to the HRSN demonstration components, and housing related support services. In addition,
the state is also strongly encouraged to evaluate the implementation of the demonstration components in order to better understand whether implementation of certain key and novel demonstration initiatives happened as envisioned during the demonstration design process and whether specific factors acted as facilitators of–or barriers to–successful implementation. Implementation research questions can also focus on beneficiary and provider experience with the demonstration. The implementation evaluation can inform the state's crafting and selection of testable hypotheses and research questions for the demonstration's outcome and impact evaluations and provide context for interpreting the findings.
Hypotheses must cover all policies and goals of the demonstration and should be crafted to not only evaluate whether overall demonstration goals were achieved but also the extent to which each component contributed to outcomes. Where demonstration components offer tailored service to specific populations, evaluation hypotheses must include an assessment of whether these programs improved quality of care outcomes and access to health care for the targeted population while also promoting the desired administrative and fiscal efficiencies. The evaluation questions and hypotheses should address the impacts of the following demonstration initiatives, including but not be limited to:Finally, the state must accommodate data collection and analyses stratified by key subpopulations of interest (e.g., by sex, age, race/ethnicity, primary language, disability status, and geography). Such stratified data analyses will provide a fuller understanding of existing disparities in access to and quality of care and health outcomes, and help inform how the demonstration's various policies might support reducing such disparities.
- Evaluation hypotheses for the HRSN demonstration components must focus on areas such as assessing the effectiveness of the HRSN services in mitigating identified needs of beneficiaries. Such assessment is expected to use applicable demonstration monitoring and other data on prevalence and severity of beneficiaries' HRSNs and the provision of beneficiary utilization of HRSN services. Furthermore, the HRSN evaluation must include analysis of how the initiatives affect utilization of preventive and routine care; utilization of and costs associated with potentially avoidable, high-acuity health care; utilization of hospital and institutional care; and beneficiary physical and mental health outcomes.
In addition, the state must coordinate with its managed care plans to secure necessary data–for a representative beneficiary population eligible for the HRSN services–to conduct a robust evaluation of the effectiveness of the HRSN services in mitigating identified needs of beneficiaries. Such an assessment will require setting up a data infrastructure and/or data sharing arrangement to collect data on beneficiary screening and rescreening and prevalence and severity of beneficiaries' HRSNs, among others. If the data system is not operational to capture necessary data for a quantitative evaluation by the time the state's evaluation activities must be conducted, the state must provide applicable qualitative assessment to this effect leveraging suitable primary data collections efforts (e.g., beneficiary surveys).
Hypotheses must be designed to help understand, in particular, the impact of housing supports, case management, nutritional services, and transportation support toward accessing covered HRSN services and case management activities on beneficiary health outcomes and experience. In alignment with the demonstration's objectives
to improve outcomes for the state's overall beneficiary populations eligible for the HRSN initiatives, the state must also include research questions and hypotheses focused on understanding the impact of the HRSN initiatives on advancing health quality, including through the reduction of health disparities, for example, by assessing the effects of the initiatives in reducing disparities in health care access, quality of care, or health outcomes at the individual, population, and/or community level. As specified in STC 6.7.g., the state must also include research questions and hypotheses focused on how renewals of recurring nutrition services affect care utilization and beneficiary physical and mental health outcomes, as well as the cost of providing such services.
The evaluation must also assess the effectiveness of the infrastructure investments authorized through the demonstration to support the development and implementation of the HRSN initiatives. The state must also examine whether and how local investments in housing supports and nutrition services change over time in concert with new Medicaid funding toward those services. In addition, considering how the demonstration's HRSN expenditures are being treated for purposes of budget neutrality, the evaluation of the HRSN initiative must include a cost analysis to support developing comprehensive and accurate cost estimates of providing such services. Evaluation of the HRSN initiative is also required to include a robust assessment of potential improvements in the quality and effectiveness of downstream services that can be provided under the state plan authority, and associated cost implications.- Hypotheses for the SUD program must include an assessment of the objectives of the SUD component of this section 1115 demonstration. Examples include, but are not limited to, initiative and engagement; compliance with treatment, utilization of health services (e.g., emergency department and inpatient hospital settings), and a reduction in key outcomes, such as deaths due to overdose.
- The state's evaluation efforts must develop robust hypotheses and research questions to assess the effectiveness of the state's DSHP-funded initiatives in meeting the desired goals of such programs in advancing and complementing its broader HRSN and other applicable initiatives for its Medicaid beneficiaries and other low-income populations. The analysis must be designed to help demonstrate how these programs support, for example, expanding coverage, improving access, reducing health disparities, and/or enhancing home-and-community-based services or services to address HRSN or behavioral health.
- For the Workforce Initiatives, the state must develop hypotheses and research questions to evaluate the effects of the initiatives on beneficiary access to care, as compared to what may be achieved through direct interventions such as rate increases. The state should also evaluate how close estimated costs and positions awarded of each CPT were to actual costs and awards, how effective backfill costs were at retaining work levels while the backfilled individual left for CPT, improvements in overall staffing levels, the quality of the WIO workforce training performance measures, and long-term effects of the workforce programs on retention. The Evaluation Design must outline hypotheses and research questions to assess whether these initiatives sustainably reduce workforce shortages and increase provider retention, especially in the concentration areas such as primary care, behavioral health, and family practice. Because these initiatives may affect a small number of providers, the state is strongly encouraged to use a mixed-methods approach that would incorporate qualitative data sources, including interviews and/or focus groups with participating providers, and beneficiary experience surveys. Any qualitative component should also include evaluation of WIO performance.
- The state's evaluation efforts must also include developing hypotheses and research questions to assess the effectiveness of the Medicaid Hospital Global Budget Initiative in ensuring provision of consistent high-quality care to all beneficiaries, as well as progress toward adopting global payment methodologies. Evaluation is expected to assess progress toward the quality and completeness of reporting on stratified data elements. Quantitative evaluation should focus on the effects of the Medicaid Hospital Global Budget Initiative payments toward improving hospital operating margins, as well as analyses of hospital financial health, identifying any hospitals that continued to have negative margin after payments, or had greater than 5 percent margin after payments, and potential mitigation strategies. Qualitative interviews should be conducted with hospitals and stakeholders to inform understanding of what led to hospital financial distress, how the Medicaid Hospital Global Budget Initiative payments have helped, and what other steps could be taken to improve long-term financial viability of hospitals accepting a large uninsured/Medicaid payor mix.
- The state is expected to evaluate the effectiveness of the HERO in conducting the five main activities: data aggregation, regional needs assessment, stakeholder, engagement, designing value-based payment, and program analysis. The state is strongly encouraged to add a qualitative component in which interviews with entities interacting with the HERO are conducted to inform on its effectiveness.
- As part of its evaluation efforts, the state must conduct a demonstration cost assessment to include, but not be limited to, administrative costs of demonstration implementation and operation, Medicaid health services expenditures, and provider uncompensated care costs. The state must analyze the budgetary effects of the HRSN services, and the overall medical assistance service expenditures and uncompensated care and associated costs for populations eligible for continuous eligibility, including in comparison to populations not eligible for such policies. In addition, the state must use findings from hypothesis tests aligned with other demonstration goals and cost analyses to assess the demonstration's effects on the fiscal sustainability of the state's Medicaid program.
- 17.7 Interim Evaluation Report. The state must submit an Interim Evaluation Report for the completed years of the demonstration, and for each subsequent extension of the demonstration, as outlined in 42 CFR 431.412(c)(2)(vi). When submitting an application for extension of the demonstration, the Interim Evaluation Report should be posted to the state's Medicaid website with the application for public comment.
- The Interim Evaluation Report will discuss evaluation progress and present findings to date as per the approved Evaluation Design.
- For demonstration authority or any components within the demonstration that expire prior to the overall demonstration's expiration date, the Interim Evaluation Report must include an evaluation of the authority, to be collaboratively determined by CMS and the state.
- If the state is seeking to extend the demonstration, the draft Interim Evaluation Report is due when the application for extension is submitted. If the state is not requesting an extension for a demonstration, an Interim Evaluation report is due one (1) year prior to the end of the demonstration. The state must submit revised Interim Evaluation Reports 60 calendar days after receiving CMS comments on the draft report, if any.
- Once approved by CMS, the state must post the final Interim Evaluation Report to the state's Medicaid website within 30 calendar days.
- The Interim Evaluation Report must comply with Attachment F (Preparing the Interim and Summative Evaluation Reports) of these STCs.
- 17.8 Summative Evaluation Report. The state must submit a draft Summative Evaluation Report for the demonstration's approval period within 18 months of the end of the approval period represented by these STCs. The draft Summative Evaluation Report must be developed in accordance with Attachment F (Preparing the Interim and Summative Evaluation Reports) of these STCs. The Summative Evaluation Report must include the information in the approved Evaluation Design.
c. The state must submit a revised Summative Evaluation Report within 60 calendar days of receiving comments from CMS on the draft, if any.
a. Once approved by CMS, the state must post the final Summative Evaluation Report to the state's Medicaid website within 30 calendar days.- 17.9 Corrective Action Plan Related to Evaluation. If evaluation findings indicate that demonstration features are not likely to assist in promoting the objectives of Medicaid, CMS reserves the right to require the state to submit a corrective action plan to CMS for approval. These discussions may also occur as part of an extension process when associated with the state's Interim Evaluation Report, or as part of the review of the Summative Evaluation Report. A corrective action plan could include a temporary suspension of implementation of demonstration programs, in circumstances where evaluation findings indicate substantial and sustained directional change inconsistent with demonstration goals, such as substantial and sustained trends indicating increased difficulty accessing services. A corrective action plan may be an interim step to withdrawing waivers or expenditure authorities, as outlined in STC 3.10. CMS further has the ability to suspend implementation of the demonstration should corrective actions not effectively resolve these concerns in a timely manner.
- 17.10 State Presentations for CMS. CMS reserves the right to request that the state present and participate in a discussion with CMS on the Evaluation Design, the Interim Evaluation reports, and/or the Summative Evaluation Report. Presentations may be conducted remotely.
- 17.11 Public Access. The state shall post the final documents (e.g., Implementation Plans, Monitoring Protocols, Monitoring Reports, Mid-Point Assessment, Close Out Report, approved Evaluation Design, Interim Evaluation Report, and Summative Evaluation Report) on the state's Medicaid website within 30 calendar days of approval by CMS.
- 17.12 Additional Publications and Presentations. For a period of 12 months following CMS approval of the final reports, CMS will be notified prior to presentation of these reports or their findings, including in related publications (including, for example, journal articles), by the state, contractor, or any other third party directly connected to the demonstration, over which the state has control. Prior to release of these reports, articles or other publications, CMS will be provided a copy including any associated press materials. CMS will be given 30 calendar days to review and comment on publications before they are released. CMS may choose to decline to comment or review some or all of these notifications and reviews. This requirement does not apply to the release or presentation of these materials to state or local government officials.
18. SCHEDULE OF DELIVERABLES FOR DEMONSTRATION
In general, all deliverables are subject to revisions upon CMS review and feedback. Revised
deliverables are generally due to CMS 60 days after receipt of CMS feedback.
Table 23: Schedule of Demonstration Deliverables STC Section Demonstration Deliverable Due Date Frequency 6 Protocol for Assessment of Beneficiary Eligibility and Needs, Infrastructure Planning, and Provider Qualifications for HRSN Services. Due to CMS 90 calendar days after the approval of the amendment. One-time 6 HRSN Implementation Plan Within 9 months of the amendment's approval One-time 9 Medicaid Hospital Global Budget Initiative Implementation Protocol By April 1, 2025 One-time 8 SUD Implementation Plan Within 90 days of the amendment's approval One-time 14 SUD Monitoring Protocol Due to CMS 150 days after the amendment approval One-time 14 Monitoring Protocol for Other Policies Due to CMS 150 days after the amendment approval One-time 14 SUD Mid-Point Assessments No later than 60 calendar days after September 31, 2026 One-time 17 Evaluation Design Due to CMS 180 days after approval of the demonstration amendment One-time 17 Interim Evaluation Reports One year prior to current expiration date, March 31, 2026 One-time STC Section Demonstration Deliverable Due Date Frequency 17 Summative Evaluation Report Due to CMS 18 months after the end of the demonstration approval period One-time 14 Close-Out Report (applicable if demonstration or demonstration component expires) Due to CMS 120 calendar days after the expiration of the demonstration One-time 11 Approved DSHP List Within 90 calendar days of the amendment's approval One-time 11 DSHP Claiming Protocol Within 150 calendar days of the amendment's approval One-time 11 DSHP Sustainability Plan By December 1, 2025 One-time 7 Provider Rate Increase Attestation Table and Supporting Information Within 90 days of the amendment's approval One-time 7 Annual Attestation of Provider Rate Increase Annually, as part of demonstration annual report. Ongoing 14 Quarterly Monitoring Report Due to CMS 60 days after the end of each demonstration quarter Ongoing 14 Quarterly Budget Neutrality Report Due to CMS 60 days after the end of each demonstration quarter Ongoing 14 Annual Monitoring Report Due to CMS 90 days after the end of each demonstration year Ongoing
ATTACHMENT A
Home and Community-Based Services Expansion Program Benefits
| Assistive Technology (including personal emergency response system) |
| Community Integration Counseling and Services |
| Community Transition Services |
| Congregate/Home Delivered Meals |
| Environmental Modifications |
| Home and Community Support Services |
| Home Maintenance |
| Home Visits by Medical Personnel |
| Independent Living Skills Training |
| Intensive Behavioral Programs |
| Medical Social Services |
| Moving Assistance |
| Nutritional Counseling/Education |
| Peer Mentoring |
| Positive Behavioral Interventions |
| Respiratory Therapy |
| Respite Care/Services |
| Service Coordination |
| Social Day Care (including transportation) |
| Structured Day Program |
| Substance Abuse Programs |
| Transportation |
| Wellness Counseling Services |
All HCBS Expansion program participants may not receive all benefits listed above. An individual participant's access to the benefits below may vary based on the individual's similarity to an individual determined eligible for and enrolled in the NHTD or TBI 1915(c) waiver program.
Home and community-based services (HCBS) must be provided in a setting that includes the following qualities:
- ☐ The setting is integrated in and supports full access of individuals receiving Medicaid HCBS to the greater community, including opportunities to seek employment and work in competitiveintegrated settings, engage in community life, control personal resources, and receive services in the community, to the same degree of access as individuals not receiving MedicaidHCBS.
- ☐ The setting is selected by the individual from among setting options including non-disability specific settings and an option for a private unit in a residential setting.
- ☐ The setting options are identified and documented in the person-centered service plan and are based on theindividual's needs, preferences, and, for residential settings, resources available for room and board.
- ☐ Ensures an individual's rights of privacy, dignity and respect, and freedom from coercion and restraint.
- ☐ Optimizes, but does not regiment, individual initiative, autonomy, and independence in makinglife choices, including but not limited to, daily activities, physical environment, and with whom to interact.
- ☐ Facilitates individual choice regarding services and supports, and who provides them.
- ☐ In a provider-owned or controlled residential setting, in addition to the qualitiesspecified above, the following additional conditions must be met:
- The unit or dwelling is a specific physical place that can be owned, rented, or occupied under a legally enforceable agreement by the individual receiving services, and the individual has, at a minimum, the same responsibilities and protections from eviction that tenants have under the landlord/tenant law of the state, county, city, or other designated entity. For settings in which landlord tenant laws do not apply, the state must ensure that a lease, residency agreement or other form of written agreement will be in place for each HCBS participant, and that the document provides protections that address eviction processes and appeals comparable to those provided under the jurisdiction's landlord tenant law.
- Each individual has privacy in their sleeping or living unit:
- ☐ Units have entrance doors lockable by the individual, with only appropriate staff having keys to doors.
- ☐ Individuals sharing units have a choice of roommates in that setting.
- ☐ Individuals have the freedom to furnish and decorate their sleeping or living units within the lease or other agreement.
- Individuals have the freedom and support to control their own schedules and activities, andhave access to food at any time.
- Individuals are able to have visitors of their choosing at any time.
- The setting is physically accessible to the individual.
- Any modification of the additional conditions specified in items 1 through 4 above, must be supported by a specific assessed need and justified in the person-centered service plan. The following requirements must be documented in the person-centered service plan:
- ☐ Identify a specific and individualized assessed need.
- ☐ Document the positive interventions and supports used prior to any modifications to the person-centered service plan.
- ☐ Document less intrusive methods of meeting the need that have been tried but did not work.
- ☐ Include a clear description of the condition that is directly proportionate to the specificassessed need.
- ☐ Include regular collection and review of data to measure the ongoing effectiveness ofthe modification.
- ☐ Include established time limits for periodic reviews to determine if the modification isstill necessary or can be terminated.
- ☐ Include the informed consent of the individual.
- ☐ Include an assurance that interventions and supports will cause no harm to the individual.
Settings that are not Home and Community-Based:
For 1115 demonstrations that furnish HCBS services, settings that are not home and community-based are defined at §441.301(c)(5) as follows:
- ☐ A nursing facility;
- ☐ An institution for mental diseases;
- ☐ An intermediate care facility for individuals with intellectual disabilities; A hospital; or
- ☐ Any other locations that have qualities of an institutional setting, as determined bythe Secretary.
ATTACHMENT B
Behavioral Health (BH) Home and Community Based Services (HCBS) and Community Oriented Recovery and Empowerment (CORE) Services in HARPS
| Behavioral Health HCBS |
|---|
BH HCBS Assessment
|
| Habilitation Services |
| Non-medical transportation |
|
|
*BH HCBS settings must adhere to the same HCBS setting qualities as listed in Attachment A.
Behavioral Health Community Oriented Recovery and Empowerment Services in HARPS and HIV SNPs
| Behavioral Health CORE |
|---|
|
|
|
|
ATTACHMENT C
Mandatory Managed Long-Term Care/Care Coordination Model (CCM)
Mandatory Population: Dual eligible, age 21 and over, receiving community based long term care services for over 120 days, excluding the following:
- Nursing Home Transition and Diversion waiver participants;
- Traumatic Brain Injury waiver participants;
- Assisted Living Program participants; and
- Dual eligible that do not require community based long term careservices.
Voluntary Population: Dual eligible, age 18 through 20, in need of community based long term care services for over 120 days and assessed as nursing home eligible. Non-dual eligible age 18 and older assessed as nursing home eligible and in need of community based long term care services for over 120 days.
The following requires CMS approval to initiate and reflects the enrollment of the mandatory population only.
I. Phase I and II: New York City and the suburbs
July 1, 2012 - Any new dual eligible case new to service, fitting the mandatory definition in any New York City County will be identified for enrollment and referred to the Enrollment
Broker for action.
- Enrollment Broker will provide with educational material, a list of plans/CCMs, and answer questions and provide assistance contacting a plan if requested.
- Plan/CCM will conduct assessment to determine if eligible for community based long term care.
- Plan/CCM transmits enrollment to Enrollment Broker.
In addition, the following identifies the enrollment plan for cases already receiving care. Enrollment will be phased in by service type by borough by zip code in batches. People will be given 60 days to choose a plan according to the followingschedule.
July 1, 2012: Begin personal care cases in New York County
August 1, 2012: Continue personal care cases in New York County
September, 2012: Continue personal care cases in New York County and begin personal care in Bronx County; and begin consumer directed personal assistance program cases in New York and Bronx counties
October, 2012: Continue personal care and consumer directed personal assistance program cases in New York and Bronx counties and begin Kings County
November, 2012: Continue personal care and consumer directed personal assistance program cases in New York, Bronx and Kings Counties
December, 2012: Continue personal care and consumer directed personal assistance program cases in New York, Bronx and Kings Counties and begin Queens and Richmond counties
January, 2013: Continue personal care and consumer directed personal assistance program citywide.
February, 2013 (and until all people in service are enrolled): Personal care, consumer directed personal assistance program, citywide
March, 2013: Personal care, consumer directed personal assistance program, adult day health care, home health care over 120 days citywide
March, 2013: Personal care, consumer directed personal assistance program, adult day health care, home health care over 120 days in Nassau, Suffolk and Westchester counties
April, 2013: Personal care, consumer directed personal assistance program, adult day health care, home health care over 120 days and long-term home health care program citywide
April, 2013: Personal care, consumer directed personal assistance program, adult day health care, home health care over 120 days and long-term home health care program in Nassau, Suffolk and Westchester Counties
Phase III: Rockland and Orange Counties
June 2013: Dually eligible community based long term care service recipients in these additional counties as capacity
Phase IV: Albany, Erie, Onondaga and Monroe Counties
Fall 2013: Dually eligible community based long term care service recipients in these additional counties as capacity
Phase V: Other Counties with capacity
Spring 2014: Dually eligible community based long term care service recipients in these additional counties as capacity
Phase VI:
Previously excluded dual eligible groups contingent upon development of appropriate program models:
- Nursing Home Transition and Diversion waiver participants;
- Traumatic Brain Injury waiver participants;
- Assisted Living Program participants; and
- Dual eligible that do not require community based long term careservices.
ATTACHMENT D
List of Eligible Goods and Services Under BH HCBS Individual Directed Goods and Services
Non-treatment Goods and Services Eligible for Self-Direction
Non-Treatment Goods and Services may include the following:
- Wellness activities
- Gym/ health club membership
- Wellness coaching
- Smoking cessation tools/ education
- Dental care
- Eyeglasses/care
- Out of network health/BH/specialty services
- Family planning and sexual health education/ services
- Acupuncture/pressure
- Yoga classes/ meditation guidance
- Massage/ reiki/ shiatsu/ tai chi instruction
- Pet adoption funds, including appointments/resources related to pet health and maintenance
- Workout equipment and clothing
- Nutritional supplements and vitamins
- Occupational/ skills development
- Computer literacy
- Resume development
- Interview preparation
- PC/ communication technology
- Personal preparation/ resources to prepare for interviews or to enhance confidence during employment, including purchase of a wardrobe or maintenance of personal hygiene (including but not limited to skin and hair care)
- Resources for entrepreneurial development, including business cards, website development
- Course Fees and Educational course fees and materials
- Transportation
- Public transportation costs
- Car repair/ maintenance
- Bicycle and related costs
- In-home/ social/ community supports
- Training and supports for daily living including cooking and nutrition classes, sequencing, time management, etc.
- Housing start-up (down payments), non-recurring housing bills or costs related to home maintenance, including furniture or air conditioner
- Groceries
- Travel to and from family or social functions, including special trips to visit family members or friends
- Meetings in the community with friends or family members at restaurants, coffee houses, or other social venues, that promote the social inclusion of the participant
- Financial contributions at social activities including church services
- Registration fees for conferences, trainings, community activities
- Membership dues in groups, societies, guilds, leagues
ATTACHMENT E
Developing the Evaluation Design
Introduction
Both state and federal governments need rigorous quantitative and qualitative evidence to inform policy decisions. To that end, for states that are testing new approaches and flexibilities in their Medicaid programs through section 1115 demonstrations, evaluations are crucial to understand and disseminate information about these policies. The evaluations of new initiatives seek to produce new knowledge and direction for programs and inform Medicaid policy for the future.
While a narrative about what happened during a demonstration provides important information, the principal focus of the evaluation of a section 1115 demonstration should be obtaining and analyzing data. Evaluations should include findings about the process (e.g., whether the demonstration is being implemented as intended), outcomes (e.g., whether the demonstration is having the intended effects on the target population), and impacts of the demonstration (e.g., whether the outcomes observed in the targeted population differ from outcomes in similar populations not affected by the demonstration).
Submission Timelines
There is a specified timeline for the state's submission of its draft Evaluation Design and subsequent evaluation reports. The graphic below depicts an example of this timeline for a 5-year demonstration. In addition, the state should be aware that section 1115 evaluation documents are public records. The state is required to publish the Evaluation Design to the state's website within thirty (30) calendar days of CMS approval, as per 42 CFR 431.424(e). CMS will also publish a copy to the Medicaid.gov website.
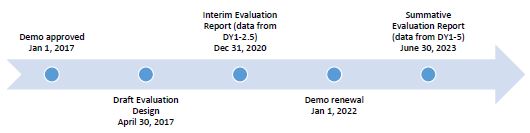
Expectations for Evaluation Designs
CMS expects Evaluation Designs to be rigorous, incorporate baseline and comparison group assessments, as well as statistical significance testing. Technical assistance resources for constructing comparison groups and identifying causal inferences are available on Medicaid.gov. If the state needs technical assistance using this outline or developing the Evaluation Design, the state should contact its demonstration team.
All states with section 1115 demonstrations are required to conduct Interim and Summative Evaluation Reports, and the Evaluation Design is the roadmap for conducting these evaluations. The roadmap begins with the stated goals for the demonstration, followed by the measurable evaluation questions and quantifiable hypotheses, all to support a determination of the extent to which the demonstration has achieved its goals. When conducting analyses and developing the evaluation reports, every effort should be made to follow the approved methodology. However, the state may request, and CMS may agree to, changes in the methodology in appropriate circumstances.
The format for the Evaluation Design is as follows:
- General Background Information;
- Evaluation Questions and Hypotheses;
- Methodology;
- Methodological Limitations;
- Attachments.
A. General Background Information - In this section, the state should include basic information about the demonstration, such as:
- The issue/s that the state is trying to address with its section 1115 demonstration and/or expenditure authorities, the potential magnitude of the issue/s, and why the state selected this course of action to address the issue/s (e.g., a narrative on why the state submitted an 1115 demonstration proposal).
- The name of the demonstration, approval date of the demonstration, and period of time covered by the evaluation.
- A description of the population groups impacted by the demonstration.
- A brief description of the demonstration and history of its implementation, and whether the draft Evaluation Design applies to an amendment, extension, renewal, or expansion of, the demonstration.
- For renewals, amendments, and major operational changes: a description of any changes to the demonstration during the approval period; the primary reason or reasons for the change; and how the Evaluation Design was altered or augmented to address these changes.
B. Evaluation Questions and Hypotheses - In this section, the state should:
- Identify the state's hypotheses about the outcomes of the demonstration, and discuss how the evaluation questions align with the hypotheses and the goals of the demonstration.
- Address how the hypotheses and research questions promote the objectives of Titles XIX and/or XXI.
- Describe how the state's demonstration goals are translated into quantifiable targets for improvement, so that the performance of the demonstration in achieving these targets can be measured.
- Include a Driver Diagram to visually aid readers in understanding the rationale behind the cause and effect of the variants behind the demonstration features and intended outcomes. A driver diagram, which includes information about the goals and features of the demonstration, is a particularly effective modeling tool when working to improve health and health care through specific interventions. A driver diagram depicts the relationship between the aim, the primary drivers that contribute directly to achieving the aim, and the secondary drivers that are necessary to achieve the primary drivers for the demonstration. For an example and more information on driver diagrams: https://innovation.cms.gov/files/x/hciatwoaimsdrvrs.pdf.
C. Methodology - In this section, the state is to describe in detail the proposed research methodology. The focus is on showing that the evaluation meets the prevailing standards of scientific and academic rigor, that the results are statistically valid and reliable, and that it builds upon other published research, using references where appropriate.
This section also provides evidence that the demonstration evaluation will use the best available data. The state should report on, control for, and make appropriate adjustments for the limitations of the data and their effects on results, and discuss the generalizability of results. This section should provide enough transparency to explain what will be measured and how, in sufficient detail so that another party could replicate the results. Table A below is an example of how the state might want to articulate the analytic methods for each research question and measure. Specifically, this section establishes:
- Methodological Design - Provide information on how the evaluation will be designed. For example, whether the evaluation will utilize pre/post data comparisons, pre-test or post-test only assessments. If qualitative analysis methods will be used, they must be described in detail.
- Target and Comparison Populations - Describe the characteristics of the target and comparison populations, incorporating the inclusion and exclusion criteria. Include information about the level of analysis (beneficiary, provider, or program level), and if populations will be stratified into subgroups. Additionally, discuss the sampling methodology for the populations, as well as support that a statistically reliable sample size is available.
- Evaluation Period - Describe the time periods for which data will be included.
- Evaluation Measures - List all measures that will be calculated to evaluate the demonstration. The state also should include information about how it will define the numerators and denominators. Furthermore, the state should ensure the measures contain assessments of both process and outcomes to evaluate the effects of the demonstration during the period of approval. When selecting metrics, the state shall identify opportunities for improving quality of care and health outcomes, and controlling cost of care. The state also should incorporate benchmarking and comparisons to national and state standards, where appropriate. The state also should include the measure stewards (i.e., the organization(s) responsible for the evaluation data elements/sets by "owning", defining, validating, securing, and submitting for endorsement, etc.) Proposed health measures could include CMS's Core Set of Health Care Quality Measures for Children in Medicaid and CHIP, Consumer Assessment of Health Care Providers and Systems (CAHPS), the Initial Core Set of Health Care Quality Measures for Medicaid-Eligible Adults and/or measures endorsed by National Quality Forum. Proposed performance metrics can be selected from nationally recognized metrics, for example from sets developed by the Center for Medicare and Medicaid Innovation or for meaningful use under Health Information Technology.
- Data Sources - Explain from where the data will be obtained, describe any efforts to validate and clean the data, and discuss the quality and limitations of the data sources. If the state plans to collect primary data (i.e., data collected specifically for the evaluation), include the methods by which the data will be collected, the source of the proposed questions and responses, and the frequency and timing of data collection. Additionally, copies of any proposed surveys must be provided to CMS for approval before implementation.
- Analytic Methods - This section includes the details of the selected quantitative and/or qualitative analysis measures that will adequately assess the effectiveness of the demonstration. This section should:
- Identify the specific statistical testing which will be undertaken for each measure (e.g., t-tests, chi-square, odds ratio, ANOVA, regression).
- Explain how the state will isolate the effects of the demonstration from other initiatives occurring in the state at the same time (e.g., through the use of comparison groups).
- Include a discussion of how propensity score matching and difference-in-differences designs may be used to adjust for differences in comparison populations over time, if applicable.
- Consider the application of sensitivity analyses, as appropriate.
- Other Additions - The state may provide any other information pertinent to the Evaluation Design for the demonstration.
| Research Question | Outcome measures used to address the research question | Sample or population subgroups to be compared | Data Sources | Analytic Methods |
|---|---|---|---|---|
| Hypothesis 1 | ||||
| Research question 1a | -Measure 1 -Measure 2 -Measure 3 |
-Sample e.g. All attributed Medicaid beneficiaries -Beneficiaries with diabetes diagnosis |
-Medicaid fee-for-service and encounter claims records | -Interrupted time series |
| Research question 1b | -Measure 1 -Measure 2 -Measure 3 -Measure 4 |
-Sample, e.g., PPS patients who meet survey selection requirements (used services within the last 6 months) | -Patient survey | Descriptive statistics |
| Hypothesis 2 | ||||
| Research question 2a | -Measure 1 -Measure 2 |
-Sample, e.g., PPS administrators | -Key informants | Qualitative analysis of interview material |
D. Methodological Limitations - This section provides more detailed information about the limitations of the evaluation. This could include limitations about the design, the data sources or collection process, or analytic methods. The state should also identify any efforts to minimize these limitations. Additionally, this section should include any information about features of the demonstration that effectively present methodological constraints that the state would like CMS to take into consideration in its review.
CMS also recognizes that there may be certain instances where a state cannot meet the rigor of an evaluation as expected by CMS. In these instances, the state should document for CMS why it is not able to incorporate key components of a rigorous evaluation, including comparison groups and baseline data analyses. For example, if a demonstration is long-standing, it may be difficult for the state to include baseline data because any pre-test data points may not be relevant or comparable. Other examples of considerations include:
- When the demonstration is:
- Non-complex, unchanged, or has previously been rigorously evaluated and found to be successful; or
- Could now be considered standard Medicaid policy (CMS published regulations or guidance).
- When the demonstration is also considered successful without issues or concerns that would require more regular reporting, such as:
- Operating smoothly without administrative changes;
- No or minimal appeals and grievances;
- No state issues with CMS-64 reporting or budget neutrality; and
- No Corrective Action Plans for the demonstration.
E. Attachments
- Independent Evaluator. This includes a discussion of the state's process for obtaining an independent entity to conduct the evaluation, including a description of the qualifications that the selected entity must possess, and how the state will assure no conflict of interest. Explain how the state will assure that the Independent Evaluator will conduct a fair and impartial evaluation and prepare objective Evaluation Reports. The Evaluation Design should include a "No Conflict of Interest" statement signed by the independent evaluator.
- Evaluation Budget. A budget for implementing the evaluation shall be provided with the draft Evaluation Design. It will include the total estimated costs, as well as a breakdown of estimated staff, administrative, and other costs for all aspects of the evaluation. Examples include, but are not limited to: the development of all survey and measurement instruments; quantitative and qualitative data collection; data cleaning and analyses; and reports generation. A justification of the costs may be required by CMS if the estimates provided do not appear to sufficiently cover the costs of the draft Evaluation Design, if CMS finds that the draft Evaluation Design is not sufficiently developed, or if the estimates appear to be excessive.
- Timeline and Major Milestones. Describe the timeline for conducting the various evaluation activities, including dates for evaluation-related milestones, including those related to procurement of an outside contractor, if applicable, and deliverables. The final Evaluation Design shall incorporate milestones for the development and submission of the Interim and Summative Evaluation Reports. Pursuant to 42 CFR 431.424(c)(v), this timeline should also include the date by which the Final Summative Evaluation Report is due.
ATTACHMENT F
Preparing the Interim and Summative Evaluation Reports
Introduction
Both state and federal governments need rigorous quantitative and qualitative evidence to inform policy decisions. To that end, for states that are testing new approaches and flexibilities in their Medicaid programs through section 1115 demonstrations, evaluations are crucial to understand and disseminate information about these policies. The evaluations of new initiatives seek to produce new knowledge and direction for programs and inform Medicaid policy for the future.
While a narrative about what happened during a demonstration provides important information, the principal focus of the evaluation of a section 1115 demonstration should be obtaining and analyzing data. Evaluations should include findings about the process (e.g., whether the demonstration is being implemented as intended), outcomes (e.g., whether the demonstration is having the intended effects on the target population), and impacts of the demonstration (e.g., whether the outcomes observed in the targeted population differ from outcomes in similar populations not affected by the demonstration).
Submission Timelines
There is a specified timeline for the state's submission of Evaluation Designs and Evaluation Reports. These dates are specified in the demonstration Special Terms and Conditions (STCs). The graphic below depicts an example of a deliverables timeline for a 5-year demonstration. In addition, the state should be aware that section 1115 evaluation documents are public records. In order to assure the dissemination of the evaluation findings, lessons learned, and recommendations, the state is required to publish the Interim and Summative Evaluation Reports to the state's website within thirty (30) calendar days of CMS approval, as per 42 CFR 431.424(d). CMS will also publish a copy to the Medicaid.gov website.
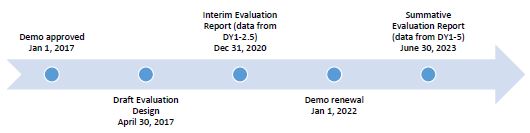
Expectations for Evaluation Reports
All states with Medicaid section 1115 demonstrations are required to conduct evaluations that are valid (the extent to which the evaluation measures what it is intended to measure), and reliable (the extent to which the evaluation could produce the same results when used repeatedly). The already-approved Evaluation Design is a map that begins with the demonstration goals, then transitions to the evaluation questions, and to the specific hypotheses,
which will be used to investigate whether the demonstration has achieved its goals. When conducting analyses and developing the evaluation reports, every effort should be made to follow the methodology outlined in the approved Evaluation Design. However, the state may request, and CMS may agree to, changes in the methodology in appropriate circumstances.
When applying for renewal, the Interim Evaluation Report should be posted on the state's website with the application for public comment. Additionally, the Interim Evaluation Report must be included in its entirety with the application submitted to CMS.
CMS expects Interim and Summative Evaluation Reports to be rigorous, incorporate baseline and comparison group assessments, as well as statistical significance testing. Technical assistance resources for constructing comparison groups and identifying causal inferences are available on Medicaid.gov: https://www.medicaid.gov/medicaid/section-1115- demonstrations/1115-demonstration-monitoring-evaluation/1115-demonstration-state- monitoring-evaluation-resources/index.html. If the state needs technical assistance using this outline or developing the evaluation reports, the state should contact its demonstration team.
Intent of this Attachment
Title XIX of the Social Security Act (the Act) requires an evaluation of every section 1115 demonstration. In order to fulfill this requirement, the state's evaluation report submissions must provide comprehensive written presentations of all key components of the demonstration, and include all required elements specified in the approved Evaluation Design. This Attachment is intended to assist states with organizing the required information in a standardized format and understanding the criteria that CMS will use in reviewing the submitted Interim and Summative Evaluation Reports.
Required Core Components of Interim and Summative Evaluation Reports
The Interim and Summative Evaluation Reports present research and findings about the section 1115 demonstration. It is important that the reports incorporate a discussion about the structure of the Evaluation Design to explain the goals and objectives of the demonstration, the hypotheses related to the demonstration, and the methodology for the evaluation. The evaluation reports should present the relevant data and an interpretation of the findings; assess the outcomes (what worked and what did not work); explain the limitations of the design, data, and analyses; offer recommendations regarding what (in hindsight) the state would further advance, or do differently, and why; and discuss the implications on future Medicaid policy.
The format for the Interim and Summative Evaluation reports is as follows:
- Executive Summary;
- General Background Information;
- Evaluation Questions and Hypotheses;
- Methodology;
- Methodological Limitations;
- Results;
- Conclusions;
- Interpretations, and Policy Implications and Interactions with Other State Initiatives;
- Lessons Learned and Recommendations; and,
- Attachment(s).
A. Executive Summary - A summary of the demonstration, the principal results, interpretations, and recommendations of the evaluation.
B. General Background Information about the Demonstration - In this section, the state should include basic information about the demonstration, such as:
- The issue/s that the state is trying to address with its section 1115 demonstration and/or expenditure authorities, how the state became aware of the issue, the potential magnitude of the issue, and why the state selected this course of action to address the issues.
- The name of the demonstration, approval date of the demonstration, and period of time covered by the evaluation.
- A description of the population groups impacted by the demonstration.
- A brief description of the demonstration and history of the implementation, and if the evaluation is for an amendment, extension, renewal, or expansion of, the demonstration.
- For renewals, amendments, and major operational changes: A description of any changes to the demonstration during the approval period; whether the motivation for change was due to political, economic, and fiscal factors at the state and/or federal level; whether the programmatic changes were implemented to improve beneficiary health, provider/health plan performance, or administrative efficiency; and how the Evaluation Design was altered or augmented to address these changes. Additionally, the state should explain how this Evaluation Report builds upon and expands earlier demonstration evaluation findings (if applicable).
C. Evaluation Questions and Hypotheses - In this section, the state should:
- Identify the state's hypotheses about the outcomes of the demonstration, and discuss how the goals of the demonstration align with the evaluation questions and hypotheses.
- Address how the research questions / hypotheses of this demonstration promote the objectives of titles XIX and XXI.
- Describe how the state's demonstration goals were translated into quantifiable targets for improvement, so that the performance of the demonstration in achieving these targets could be measured.
- The inclusion of a Driver Diagram in the Evaluation Report is highly encouraged, as the visual can aid readers in understanding the rationale behind the demonstration features and intended outcomes.
D. Methodology - In this section, the state is to provide an overview of the research that was conducted to evaluate the section 1115 demonstration, consistent with the approved Evaluation Design. The Evaluation Design should also be included as an attachment to the report. The focus is on showing that the evaluation builds upon other published research, (using references), meets the prevailing standards of scientific and academic rigor, and the results are statistically valid and reliable.
An Interim Evaluation Report should provide any available data to date, including both quantitative and qualitative assessments. The Evaluation Design should assure there is appropriate data development and collection in a timely manner to support developing an Interim Evaluation Report.
This section provides the evidence that the demonstration evaluation used the best available data and describes why potential alternative data sources were not used. The state also should report on, control for, and make appropriate adjustments for the limitations of the data and their effects on results, and discusses the generalizability of results. This section should provide enough transparency to explain what was measured and how, in sufficient detail so that another party could replicate the results. Specifically, this section establishes that the approved Evaluation Design was followed by describing:
- Methodological Design - Whether the evaluation included an assessment of pre/post or post-only data, with or without comparison groups, etc.
- Target and Comparison Populations - Describe the target and comparison populations, describing inclusion and exclusion criteria.
- Evaluation Period - Describe the time periods for which data will be collected.
- Evaluation Measures - List the measures used to evaluate the demonstration and their respective measure stewards.
- Data Sources - Explain from where the data were obtained, and efforts to validate and clean the data.
- Analytic Methods - Identify specific statistical testing which was undertaken for each measure (t-tests, chi-square, odds ratio, ANOVA, regression, etc.).
- Other Additions - The state may provide any other information pertinent to the evaluation of the demonstration.
E. Methodological Limitations - This section provides sufficient information for discerning the strengths and weaknesses of the study design, data sources/collection, and analyses.
F. Results - In this section, the state presents and uses the quantitative and qualitative data to demonstrate whether and to what degree the evaluation questions and hypotheses of the demonstration were addressed. The findings should visually depict the demonstration results, using tables, charts, and graphs, where appropriate. This section should include findings from the statistical tests conducted.
G. Conclusions - In this section, the state will present the conclusions about the evaluation results. Based on the findings, discuss the outcomes and impacts of the demonstration and identify the opportunities for improvements. Specifically, the state should answer the following questions:
- In general, did the results show that the demonstration was/was not effective in achieving the goals and objectives established at the beginning of the demonstration?
- If the state did not fully achieve its intended goals, why not?
- What could be done in the future that would better enable such an effort to more fully achieve those purposes, aims, objectives, and goals?
H. Interpretations, Policy Implications and Interactions with Other State Initiatives - In this section, the state will discuss the section 1115 demonstration within an overall Medicaid context and long-range planning. This should include interrelations of the demonstration with other aspects of the state's Medicaid program, interactions with other Medicaid demonstrations, and other federal awards affecting service delivery, health outcomes and the cost of care under Medicaid. This section provides the state with an opportunity to provide interpretations of the data using evaluative reasoning to make judgments about the demonstration. This section should also include a discussion of the implications of the findings at both the state and national levels.
I. Lessons Learned and Recommendations - This section of the evaluation report involves the transfer of knowledge. Specifically, it should include potential "opportunities" for future or revised demonstrations to inform Medicaid policymakers, advocates, and stakeholders. Recommendations for improvement can be just as significant as identifying current successful strategies. Based on the evaluation results, the state should address the following questions:
- What lessons were learned as a result of the demonstration?
- What would you recommend to other states which may be interested in implementing a similar approach?
ATTACHMENT G
Evaluation Design (Reserved)
ATTACHMENT H
SUD Implementation Plan
Approved January 9, 2024
OVERVIEW
This Implementation Plan is submitted in conjunction with the New York Department of Health submission of a substance use disorder (SUD) demonstration pursuant to Section 1115 of the Social Security Act. New York is committed to providing a full continuum of care for people with opioid use disorder (OUD) and other SUDs and expanding access and improving outcomes in the most cost-effective manner possible.
Goals:
- Increased rates of identification, initiation and engagement in treatment for OUD and other SUDs;
- Increased adherence to and retention in treatment for OUD and other SUDs;
- Reductions in overdose deaths, particularly those due to opioids;
- Reduced utilization of emergency departments and inpatient hospital settings for OUD and other SUD treatment where the utilization is preventable or medically inappropriate through improved access to other continuum of care services;
- Fewer readmissions to the same or higher level of care where readmissions is preventable or medically inappropriate for OUD and other SUDs; and
- Improved access to care for physical health conditions among beneficiaries with OUD or other SUDs.
Milestones:
- Access to critical levels of care for OUD and other SUDs;
- Widespread use of evidence-based, SUD-specific patient placement criteria;
- Use of nationally recognized, evidence-based, SUD program standards to set residential treatment provider qualifications;
- Sufficient provider capacity at each level of care, including medication assisted treatment (MAT);
- Implementation of comprehensive treatment and prevention strategies to address opioid misuse and OUD; and
- Improved care coordination and transitions between levels of care.
Section I - Implementation Plan Milestone Completion
This section contains information detailing New York's strategies for meeting the six milestones over the course of the demonstration. Specifically, this section:
- Includes a summary of how, to the extent applicable, New York already meets each milestone, in whole or in part, and any actions needed to meet each milestone, including the persons or entities responsible for completing actions;
- Describes the timelines and activities that New York will undertake to achieve the milestones; and
- Provides an overview of future plans to improve beneficiary access to SUD services and promote quality and safety standards.
Milestones
- Access to Critical Levels of Care for OUD and Other SUDs
New York offers a range of services at varying levels of intensity across a continuum of care because each type of treatment or level of care may be more or less effective depending on each beneficiary's individual clinical needs. To meet this milestone, New York's current SUD Medicaid treatment system includes coverage of the following:
- Screening, Brief Intervention and Referral to Treatment (SBIRT) Services
- Outpatient;
- Intensive Outpatient;
- Outpatient Rehabilitation
- Medication Assisted Treatment including Methadone Maintenance (medications, as well as counseling and other services, with sufficient provider capacity to meet the needs of Medicaid beneficiaries in the state);
- Ambulatory withdrawal management;
- Intensive LOCs in residential settings and withdrawal management;
- Intensive LOCs in inpatient hospital settings;
- Medically-managed and medically supervised withdrawal management;
- Residential Rehabilitative Services for Youth (RRSY); and
- Health Home for children and Adults with Serious Mental Illness, Serious Emotional Disturbance and Co-Occurring SUD.
This demonstration builds upon an extensive, existing array of New York Medicaid covered behavioral health (BH) services, including evidence-based services and will improve upon and enhance services that are currently covered only under non-Medicaid sources, including state funding and other federal funding.
New York Medicaid covers all ambulatory Level of Care for Alcohol and Drug Treatment Referral (LOCADTR) LOCs, as well as medication-assisted treatment (MAT), residential and inpatient services and withdrawal management. New York's Medicaid state Plan includes authority for a complete continuum of care as approved in state Plan Amendment (SPA) #16-0004, 91-0039, 91-0075, 09-0034, 19-0017, 19-0013, 19-0018, 06-61, and 08-39. The Demonstration will permit DOH to provide critical access to medically necessary SUD treatment services in the most appropriate setting for the member as part of a comprehensive continuum of SUD treatment services.
The demonstration would permit DOH to provide medically necessary medical and BH care (including co-occurring mental health [MH] and SUD treatment services) in the most appropriate setting for individuals receiving residential and inpatient SUD treatment services. This approach is designed address the demonstration goals detailed below under Hypothesis and Evaluation, including improving health care outcomes for individuals with SUD (reducing
hospital emergency department use and inpatient admissions, reducing hospital readmissions, and improving the rates of initiation, engagement and retention in treatment).
New York Medicaid currently covers adult SUD residential services under approved state Plan Amendment #16-004. However, the state has not yet implemented reintegration services under that state Plan. New York will begin reimbursing for reintegration services delivered by providers whose qualifications are consistent with LOCADTR, state regulations, and the already approved state Plan Amendment. Reintegration is a phase of care in residential treatment that correlated to
- in ASAM. People in this level of care benefit from ongoing rehabilitation and skill building to support recovery and move towards independent living. A reimbursement SPA will be submitted to update reimbursement methodologies.
The New York Office of Addiction Services and Supports (OASAS) directly operates 12 Addiction Treatment Centers and oversees over 1,600 addiction treatment programs. In addition, expanded regional programming including Centers of Treatment Innovation (COTIs), Open Access Centers and Recovery Community Centers, treat New Yorkers wherever they may be in their recovery journey.
Summary of All OASAS Services
| LOCATDR Service Description | NYCRR Title 14 | # of providers | # of facilities | # of beds / slots | Count Served Cohort CY2019 | Avg Length of Stay (days) for CY 2019 Cohort | Vacancie s as of 11/30/21 (Beds) | ASAM Level |
|---|---|---|---|---|---|---|---|---|
| Medically Managed Inpatient Detoxification | 816 | 17 | 18 | 350 | 32,079 | 3.7 | 120 | 4-WM |
| Medically Supervised Inpatient Detoxification | 816 | 23 | 26 | 703 | 32,769 | 4.1 | 318 | 3.7- WM |
| Inpatient Treatment | 818 | 62 | 65 | 2,492 | 49,553 | 15.7 | 354 | 3.7 |
| Residential Rehabilitation Services for Youth | 818 | 7 | 9 | 240 | 955 | 108.8 | 65 | 3.7 |
| Residential Services - Stabilization / Rehabilitation (w/o Reintegration) | 820 | 17 | 32 | 1,154 | 6,724 | 50.3 | 268 | 3.5 / 3.3 |
| Residential Services - Stabilization / Rehabilitation (with Reintegration) | 820 | 17 | 35 | 1,849 | 4,892 | 110.9 | 352 | 3.5/3.3/3.1 |
| Residential Services - Reintegration Only | 820 | 15 | 29 | 730 | 977 | 201.8 | 107 | 3.1 |
| Day Rehabilitation | 822 | 28 | 35 | NA | 6,977 | 117.7 | NA | 2.5 |
| Intensive Outpatient (Cohort Data is CY2021 Annualized) | 822 | 28 | 40 | NA | 387 | 185.4 | NA | 2.1 |
| Medically Supervised Outpatient Withdrawal | 822 | 10 | 10 | 259 | 2,981 | 12.4 | NA | 2-WM |
| Outpatient Clinic | 822 | 271 | 425 | NA | 158,158 | 185.4 | NA | 1 |
| Opioid Treatment Program | 822 | 56 | 103 | 40,886 | 54,976 | 481.2 | NA | 1 |
| Residential Services - Intensive Residential | 819 | 13 | 22 | 1,285 | 8,626 | 149.8 | 211 | Comparable to ASAM 3.3 |
| Residential Services - Community Residence | 819 | 38 | 50 | 1,021 | 4,860 | 155.7 | 98 | Comparable to ASAM 3.1 |
| Residential Services - Supportive Living | 819 | 22 | 27 | 659 | 1,965 | 209.2 | 159 | Comparable to ASAM 3.1 |
This demonstration is necessary to address critical unmet needs for residential SUD treatment that continue to exist despite significant improvements to the publicly-funded treatment delivery system outside of Medicaid. state-only funds and federal Substance Abuse and Mental Health Services Administration (SAMHSA) block grant funds are used to support some residential services for individuals enrolled in Medicaid.
Each residential program in the table above is certified to provide one or more of the phases of care based on population served, staffing, physical environment and expertise. Individuals are placed in the most appropriate phase of residential care and provided services that match that level. Programs are designated in the certification process to provide one or more of the phases.
Additional residential SUD services will be included under the Medicaid state Plan with this demonstration. This transition to Medicaid reimbursement of residential and inpatient IMD services will ensure access to a comprehensive, coordinated system of SUD care for children and adults in Medicaid. Most importantly, for some Medicaid-covered individuals in need of SUD treatment, there were limited options for residential community-based SUD treatment services.
The complete SUD benefit package includes support for evidence-based practices already implemented in the state, such as multi-systemic therapy (MST), Functional Family Therapy (FFT) and Multidimensional Family Therapy (MDFT) for children with SUD conditions. It also modernizes the SUD treatment benefit to include IMD levels of care that are currently outside of the benefit, but have always been a part of the treatment continuum that exists in LOCADTR criteria for outpatient, inpatient and residential treatment. Providers have been and continue to be trained using the most current edition of LOCADTR criteria to provide multi-dimensional assessments that inform placement and individualized treatment plans to increase the use of community-based and non-hospital residential programs and assure that inpatient hospitalizations are utilized appropriately for situations in which there is a need for safety, stabilization, or acute withdrawal management.
Below is a table that describes how New York meets Milestone 1 for Medicaid beneficiaries, including a variety of services at different levels of intensity across a continuum of care.
| Milestone Criteria | Current State | Future State | Summary of Actions Needed |
|---|---|---|---|
| Coverage of outpatient services | New York Medicaid covers SUD outpatient treatment services under the following sections of the Medicaid State Plan using the LOCADTR level of care criteria:
|
All LOCADTR levels are covered. | No further action needed |
| Coverage of intensive outpatient services | New York Medicaid covers SUD intensive outpatient treatment services, including partial hospitalization, under the following sections of the state Plan:
|
All LOCADTR levels are covered. | No further action needed |
| Coverage of MAT (medications as well as counseling and other services with sufficient provider capacity to meet needs of Medicaid beneficiaries in the state) | New York Medicaid covers MAT (for non-OUD and OUD) and associated counseling/services under the following sections of the state Plan:
|
All MAT is covered. | No further action needed |
| Coverage of intensive levels of care in residential and inpatient settings | New York Medicaid covers residential SUD in a non-hospital setting under the Rehabilitative Services Option. (Page Attachment 3.1-A 3b-37(v)-(viii)) New York Medicaid covers the following inpatient SUD treatment:
|
New York Medicaid enrollees do not have access to residential services under the LOCADTR LOC for Reintegration (similar to ASAM 3.1). Under this demonstration, the state will begin authorizing Medicaid coverage of this residential level of care delivered in IMDs as providers enroll in Medicaid. | Within 6 months, New York will authorize and begin to reimburse for Medicaid individuals to receive services for the LOCADTR LOC for Reintegration services provided in an IMD. The state anticipates 50 providers to enroll within the first year. |
| Coverage of medically supervised withdrawal management | New York Medicaid covers medically supervised withdrawal management in a hospital and non-hospital setting.
|
All LOCADTR levels are covered. | No further action needed |
- Use of Evidence-based, SUD-specific Patient Placement Criteria
New York has implemented the LOCADTR, which is evidence-based, SUD-specific patient placement criteria. New York Medicaid has adopted a complete array of SUD treatment services using a national placement criteria system (e.g., LOCADTR) or national provider standards. Specifically:
- Providers assess treatment needs based on SUD-specific, multi-dimensional assessment tools, linked to the ASAM Criteria; and
- Utilization management approaches are implemented to ensure that
- beneficiaries have access to SUD services at the appropriate level of care,
- interventions are appropriate for the diagnosis and level of care, and
- there is an independent process for reviewing placement in residential treatment settings.
Below, New York identifies how it requires all providers to use the LOCADTR evidence-based, SUD-specific placement criteria to provide treatment that reflects diverse patient needs and evidence-based clinical guidelines. This table includes current and intended actions and associated timelines needed to meet Milestone 2 (Use of evidence-based, SUD-specific patient placement criteria). This milestone has already been met.
| Milestone Criteria | Current State | Summary of Actions Needed |
|---|---|---|
| Implementation of requirement that providers assess treatment needs based on SUD-specific, multi-dimensional assessment tools that reflect evidence-based clinical treatment guidelines | New York providers are required to utilize assessments that are directly tied to the LOCATDR criteria for treatment planning. New York has implemented a universal training program for providers to assess treatment needs based on the LOCATDR's multi-dimensional tools and to base treatment needs on those assessments. New York requires all Medicaid SUD providers through regulation to use the for level of care (LOC) assessments using the LOCADTR, consistent with provider training. Under the regulations, providers are required to develop recommendations for placement in appropriate levels of care based on the LOCADTR and multi-dimensional assessments. |
No further action needed |
| Implementation of a utilization management approach such that (a) beneficiaries have access to SUD services at the appropriate level of care | Regardless of payor type, all providers are required to utilize the LOCADTR as the utilization management tool for all Medicaid SUD services, as well as the patient placement criteria to review residential placements using the LOCADTR placement criteria. New York has ensured that program standards are set for beneficiaries to have access to SUD services at the appropriate LOC based on the LOCADTR dimensions of care. New York already requires through MMCP contract language that for utilization management MMCPs use LOCADTR language consistent with provider training. All website, provider information and internal documentation are consistent with the LOCATR. OASAS has a website with a provider search function for Medicaid beneficiaries and providers at all LOCADTR LOCs. |
No further action needed |
| Implementation of a utilization management approach such that (b) interventions are appropriate for the diagnosis and level of care | Today, MMCPs and FFS providers utilize the LOCADTR to review utilization for ambulatory, residential care and inpatient hospital care. New York has developed program standards to ensure that providers' interventions are appropriate for the diagnosis and each LOCADTR LOC. All Medicaid websites, criteria, manuals, and provider standards will consistently refer to the latest ASAM edition. |
No further action needed |
| Implementation of a utilization management approach such that (c) there is an independent process for reviewing placement in residential treatment settings | The current Medicaid MMCPs already use the LOCADTR for residential and inpatient utilization review. MMCPs receive a copy of the LOCADTR report with clinical assessment information conducted by the provider. Plans have training on LOCADTR and complete LOCADTRs as necessary to independently review admissions. Oversight agency regulation of billing and certification requirements through 14 NYCRR Part 841, onsite chart reviews and general oversight of LOCADTR and placement as part of normal site review process. The placement criteria currently in use can be found at the following link. New York uses the LOCADTR for utilization review of Medicaid inpatient and residential placements. All website, provider information and internal documentation is consistent with the LOCADTR. Additionally, plans are prohibited by state law from requiring prior authorization for addiction services but conduct retrospective review to ensure services were clinically appropriate, consistent with LOCADTR. The current Medicaid MMCPs already use the LOCADTR for residential and inpatient utilization review. MMCPs receive a copy of the LOCADTR report with clinical assessment information conducted by the provider. Plans have training on LOCADTR and complete LOCADTRs as necessary to independently review admissions. Oversight agency regulation of billing and certification requirements through 14 NYCRR Part 841, onsite chart reviews and general oversight of LOCADTR and placement as part of normal site review process. The placement criteria currently in use can be found at the following link. New York uses the LOCADTR for utilization review of Medicaid inpatient and residential placements. All website, provider information and internal documentation is consistent with the LOCADTR. Additionally, plans are prohibited by state law from requiring prior authorization for addiction services, but can conduct retrospective review to ensure services were clinically appropriate, consistent with LOCADTR. |
No further action needed |
- Use of Nationally Recognized SUD-specific Program Standards to Set Provider Qualifications for Residential Treatment Facilities
Through this demonstration, New York will receive federal financial participation (FFP) for a continuum of SUD services, including services provided to Medicaid enrollees residing in residential treatment facilities that qualify as institutions for mental diseases (IMDs). To meet this milestone, New York will ensure that the following criteria are met:
- Implementation of residential treatment provider qualifications (in licensure requirements, policy manuals, managed care contracts that meet the LOCADTR criteria, which is a nationally recognized, SUD-specific program standards regarding the types of services, hours of clinical care and credentials of staff for residential treatment settings;
- Implementation of a state process for reviewing residential treatment providers to assure compliance with these standards; and
- Implementation of a requirement that residential treatment facilities offer MAT on-site or facilitate access off site.
OASAS regulations and Medicaid policy manuals contain standards consistent with LOCADTR criteria for residential programs, including requirements for the particular types of services, hours of clinical care and credentials of staff for residential treatment. The policies already include a requirement that residential treatment providers offer MAT onsite or facilitate access offsite with a MAT provider not associated with the residential treatment owner.10 New York will also continue to implement the process for initial certification and ongoing monitoring of residential treatment providers to ensure compliance with the state regulation requirements which are consistent with LOCADTR placement standards.
Below, New York already incorporates nationally recognized, SUD-specific LOCADTR program standards into their provider qualifications for residential treatment facilities through their regulations, policy manuals and other guidance to meet Milestone 3 (Use of Nationally Recognized SUD-specific Program Standards to Set Provider Qualifications for Residential Treatment Facilities).
| Milestone Criteria | Current State | Future State | Summary of Actions Needed |
|---|---|---|---|
| Implementation of residential treatment provider qualifications in licensure requirements, policy manuals, contracts, or other guidance. Qualification should meet program standards in the LOCADTR, which is a nationally recognized, SUD-specific program standards regarding, in particular, the types of services, hours of clinical care, and credentials of staff for residential treatment settings | OASAS regulations outline the types of services, hours of clinical care, and credentials of staff for residential treatment setting, which are consistent with the LOCADTR. Medicaid contracts reflect that residential providers must meet these requirements for residential programs, including requirements for the particular types of services, hours of clinical care and credentials of staff for residential treatment. 14 NYCRR 800.4; 14 NYCRR 810.7; 14 NYCRR 816; 14 NYCRR 817.3(d)(1); 14 NYCRR 818; 14 NYCRR 820 and 14 NYCRR 841. |
n/a | No additional action needed. |
| Implementation of a state process for reviewing residential treatment providers to ensure compliance with these standards | All SUD residential providers are licensed by the New York OASAS. All SUD residential providers are monitored and certified to provide the LOCADTR LOC for which the provider is enrolled in the Medicaid program. The monitoring of the providers includes a review of the facility's infrastructure, as well as how the infrastructure is applied to ensure compliance with the state standards consistent with the LOCADTR and state regulations supporting the LOCADTR. The monitoring includes initial certification, monitoring and recertification. Additional oversight activities as described in 14 NYCRR Part 810 may include unannounced site visits or provider contacts including but not limited to: interim performance reviews, focused or targeted reviews, facility evaluations, fiscal audit or reviews, corrective action plan monitoring, cursory on-site visits, and/or accreditation surveys completed by nationally recognized accrediting organizations. |
New York will continue to implement the process for initial certification and ongoing monitoring of residential treatment providers to ensure compliance with the state regulation requirements which are consistent with LOCADTR placement standards. | No additional action needed. |
| Implementation of requirement that residential treatment facilities offer MAT onsite or facilitate access off-site | New York has in place a regulatory requirement that residential treatment facilities offer multiple versions of MAT on-site or facilitate access off-site (14 NYCRR 817.3(d)(1) and 14 NYCRR 800.4) All residential treatment providers offer at least one version of MAT on-site or facilitates access off-site. | None needed – New York currently meets criteria. | No additional action needed – New York currently meets criteria. |
- Sufficient Provider Capacity at Critical Levels of Care including for Medication Assisted Treatment for OUD
To meet this milestone, New York will complete an assessment of the availability of providers enrolled in Medicaid and accepting new patients in the critical levels of care listed in Milestone
- This assessment will determine the availability of treatment for Medicaid beneficiaries in each of these LOCs, as well as availability of MAT and medically supervised withdrawal management, throughout the state. This assessment will identify gaps in availability of services for beneficiaries in the critical LOCs and develop plans for enhancement of capacity based on assessments of provider availability.
To ensure there is necessary information regarding access to outpatient providers, OASAS maintains a website that is updated regularly. This report, which can be found at the following link https://webapps.oasas.ny.gov/providerDirectory/. The state also maintains a toll-free number called the HOPEline at 1-877-8-HOPENY where operators provide three referrals to assessment services in a caller's area.
The state maintains a treatment availability dashboard for outpatient and bedded programs as well that can be accessed here. This dashboard allows the state to monitor capacity of all SUD treatment providers including MAT. It also allows New York residents to search for an open slot in a treatment program in their area. The treatment availability dashboard displays treatment programs with real-time availability for particular areas.
New York currently contracts for 98,835 adult SUD residential treatment beds across 214 providers. All but 5,712 of these certified SUD residential, withdrawal management and inpatient SUD treatment service providers have more than 17 beds and meet the definition of an IMD. See the table below for the number of beds and providers providing each non-Medicaid residential level of care in New York.
| LOCATDR Service Description | NYCRR Title 14 | # of Providers | # of Facilities | # of beds/ slots | Count Served Cohort CY2019 | Avg Length of Stay (days) for CY 2019 Cohort | Vacanciesas of 11/30/21 (Beds) | ASAM Level |
|---|---|---|---|---|---|---|---|---|
| Medically Supervised Inpatient Detoxification | 816 | 20 | 22 | 646 | 29,919 | 4.1 | 292 | 3.7-WM |
| Inpatient Treatment | 818 | 28 | 31 | 1,589 | 30,938 | 15.7 | 159 | 3.7 |
| Residential Services - Stabilization / Rehabilitation (w/o Reintegration) | 820 | 15 | 29 | 1,092 | 6,436 | 50.3 | 263 | 3.5 / 3.3 |
| Residential Services - Stabilization / Rehabilitation (with Reintegration) | 820 | 16 | 33 | 1,813 | 4,870 | 110.9 | 343 | 3.5/3.3/3.1 |
| Residential Services - Reintegration Only | 820 | 9 | 19 | 572 | 842 | 201.8 | 88 | 3.1 |
| TOTAL / AVG | 134 | 5,712 | 22.6 |
In NYS, more than 78,600 patients were prescribed at least one buprenorphine prescription for outpatient treatment of OUD in 2019. The crude rate of buprenorphine prescribing for OUD increased by 28.5 percent from 314.8 per 100,000 population in 2016 to 404.5 per 100,000 in 2019. The rate was more than two times higher in NYS excluding NYC than that for NYC during 2016-2019.
The NYSDOH Buprenorphine Access Initiative began in July 2016 with the goal of increasing the number of healthcare practitioners certified to prescribe buprenorphine and thus, increase the number of patients receiving buprenorphine. In 2019 DOH AIDS Institute implemented a statewide AIDS Institute Provider Directory which includes a directory of buprenorphine prescribers. This website allows individuals to search for prescribers in their area by zip code and distance they are willing to travel. Coupled with clarifications done by DOH AIDS Institute and NYS education department a significant increase in waived buprenorphine providers in NYS has occurred. Based upon the DEA record of waived buprenorphine providers in NYS, there has been an increase of 1,182 providers in 2018, with a total of 5,174 at the end of 2018 (Table 1b).
| 2017 | 2018 | 2019 | |
|---|---|---|---|
| MD/DO-30 patients | 2,716 | 3,302 | 4,190 |
| MD/DO-100 patients | 672 | 742 | 762 |
| MD/DO-275 patients | 236 | 280 | 318 |
| NP-30 patients | 287 | 567 | 928 |
| NP-100 patients | N/A* | 69 | 143 |
| NP-275 patients | N/A* | N/A* | 18 |
| PA-30 patients | 81 | 185 | 282 |
| PA-100 patients | N/A* | 29 | 62 |
| PA-275 patients | N/A* | N/A* | 8 |
| Total providers | 3,992 | 5,174 | 6,711 |
* Note: NP/PAs could not prescribe in NYS until May 2017
In NYS, the crude rate of patients who received at least one buprenorphine prescription for OUD increased between 2016 (314.8 per 100,000 population) and 2019 (404.5 per 100,000), representing a 29 percent increase (Figure 50). The rate was more than two times higher in NYS excluding NYC than in NYC during 2016-2019. It is encouraging that more qualified practitioners have completed the required training and have received their SAMHSA DATA 2000 waiver and DEA X-designation so that they have the capacity to prescribe buprenorphine for the treatment of OUD. These qualified practitioners include physicians, Nurse Practitioners (NPs), Physician Assistants (PAs), Clinical Nurse Specialists (CNSs), Licensed Midwifes (LMs) and are in various settings increasing access for this life-saving medication.
The table below summarizes the current and future actions, including associated timelines, to meet Milestone 4 (Sufficient Provider Capacity at Critical Levels of Care including for Medication Assisted Treatment). This milestone will be met within 12 months of Demonstration approval. Note: It is necessary to ensure the complete implementation of the new service array in Medicaid prior to the capacity assessment being conducted.
The anticipated penetration rate and geographic distributions of providers at each LOC is noted where available.
| Milestone Criteria | Current State | Future State | Summary of Actions Needed |
|---|---|---|---|
Completion of assessment of the availability of providers enrolled in Medicaid and accepting new patients in the following critical levels of care throughout the state including those that offer MAT:
|
The state maintains a treatment availability dashboard for outpatient and bedded programs as well that can be accessed here. This dashboard allows the state to monitor capacity of all SUD treatment providers including MAT. It also allows New York residents to search for an open slot in a treatment program in their area. The treatment availability dashboard displays treatment programs with real-time availability for all regions across the state. | New York will examine the potential to enhance access monitoring reporting under the Demonstration, including the provision of data related to Medicaid enrolled providers accepting new patients. This initiative will leverage the current dashboard for ongoing access monitoring and recruitment and enrollment of new facilities as needed. |
OASAS will work with NYS DOH to complete an assessment of providers accepting new patients (within 1 year of demonstration approval). |
- Implementation of Comprehensive Treatment and Prevention Strategies to Address Opioid Misuse and OUD
To meet this milestone, New York will ensure that the following criteria are met:
- Continue efforts to increase utilization and improve functionality of the NYS Prescription Monitoring Program
- Continue efforts to expand interstate PMP data sharing and PMP-EHR integration.
- Provide reference to relevant opioid prescribing guidelines along with other interventions such as practitioner-focused training programs, to prevent and/or reduce prescription drug misuse
- Expanded coverage of and access to naloxone for overdose reversal
Part of New York State Department of Health's (NYSDOH) efforts to address the opioid and prescription medication crisis includes several mandates that are focused on the practitioner's role in prevention or risk reduction. NYSDOH requires practitioners who prescribe controlled substances to consult the NYS PMP Registry when writing prescriptions for Schedule II, III, and IV controlled substances. The data that populates the registry (dispensing data for Schedule II, III, IV, and V controlled substance prescriptions) is required to be submitted to New York state within 24 hours of dispensing. NYSDOH has also limited the initial prescribing of opioids for acute pain to no more than a seven-day supply of any schedule II, III, or IV opioid, within the scope of a practitioner's professional opinion or discretion. In July 2016, New York state limited the initial prescribing of opioids for acute pain to no more than a 7-day supply.11 As a result, opioid prescriptions for more than a 7-day supply decreased steadily, from 28.7 percent in the first quarter of 2017 to 15.3 percent in the fourth quarter of 2019.12
Additionally, NYSDOH has required by mandate that practitioners who treat humans and have a DEA registration number to prescribe controlled substances, as well as medical residents who prescribe controlled substances under a facility DEA registration number, must complete at least three hours of course work in pain management, palliative care, and addiction. These efforts, in addition to referral to relevant opioid prescribing guidelines assist practitioners in engaging in informed prescribing practices and improves their ability to recognize areas of concern related to patient patterns of behavior.
Attachment A describes the state's plans for enhancing its health IT infrastructure to improve the NYS Prescription Monitoring Program (PMP) as part of the state's efforts to address SUD.
| Milestone Criteria | Current State | Future State | Summary of Actions Needed |
|---|---|---|---|
| Implementation of opioid prescribing guidelines along with other interventions to prevent opioid misuse | Centers for Medicare & Medicaid Services (CMS) issued guidance to the states in 2019 related to implementation of the Medicaid Drug Utilization Review (DUR) provisions that were included in Section 1004 of the Substance Use-Disorder Prevention that Promotes Opioid Recovery and Treatment for Patients and Communities Act, also referred to as the SUPPORT Act.13 New York has amended the Medicaid State Plan to reflect the new Drug Utilization Review provisions required in federal law. The NYRx program has implemented opioid clinical edits such as requiring prior authorization for the following:
|
NYSDOH (BNE and Office of Drug User Health) are currently working on revisions to the mandated prescriber training. This includes updating standards, guidance, language, and the addition of harm reduction concepts. | A revised version of the provider training will be completed in August 2023. |
| Expanded coverage of, and access to, naloxone for overdose reversal | NYS has taken a number of steps over the past decade to make naloxone more widely available, including: expanded efforts related to addressing opioid overdose through Article 33, Title 1 Section 3309. This multi-pronged approach focuses on building overdose response capacity within communities throughout the state. The core of this program is for community laypersons to be trained by organizations registered with the NYSDOH to administer naloxone (an opioid antagonist also known by the brand name Narcan) in the event of a suspected opioid overdose.
New York has a non-patient specific prescription for naloxone with pharmacy dispensing protocol appliable to all NYS registered pharmacists. Naloxone available to all addiction and mental health providers to use and distribute to communities that they serve through a direct order process. A naloxone copayment assistance program to cover up to $40 in prescription co-payments to minimize out of pocket expenses. Require pharmacies with 20 or more locations to have a non-patient specific prescription with an authorized health care professional or register as an opioid overdose prevention program. Scope of practice protections for obtaining, administering, and possession of naloxone for licensed individuals. Yearly co-prescribing requirements for patients prescribed an opioid. Establishment of guidelines for onsite opioid overdose response capacity in nightlife establishments. |
None needed – New York currently meets criteria. | None needed – New York currently meets criteria. |
| Implementation of strategies to increase utilization and improve functionality of prescription drug monitoring programs | Since 2012, New York state has required most prescribers to consult the NYS PMP Registry when writing prescriptions for Schedule II, III, and IV controlled substances. Establishing a duty to consult ensures practitioners have a fuller picture of their patient's controlled-substance history, which can inform treatment decisions, especially where practitioners recognize high risk patient behaviors. Additionally, NYS requires that data for all Schedule II, III, IV, and V controlled substance prescriptions dispensed by state-licensed pharmacies and dispensing practitioners be submitted to New York state within 24 hours. The requirement for data submission within 24 hours of dispensing makes helps to ensure that the data within the PMP registry is timely and accurate.
NYS OASAS by regulation and guidance, requires providers to educate about overdose prevention and must make Naloxone available to all patients, prospective patients. 14 NYCRR §800.6. Guidance can be found at this link. |
The Bureau of Narcotic Enforcement (BNE), within NYSDOH is working to enhance the NYS PMP Registry to improve utilization and functionality. BNE will continue to provide the MME calculator as resource for practitioners to identify patients who may benefit from closer monitoring, reduction or tapering of opioids, prescribing of naloxone, or other measures to reduce risk of overdose. BNE is currently working on project to redesign the PMP Registry patient search landing page. The enhancements will include an indicator that notes the type of medication prescribed (Opioid, Benzodiazepine, or Stimulant), whether the prescription is current, a highly visual summary dashboard that notes the number of pharmacies or practitioners visited by the patient in the past 90 days, and how many prescriptions are present for Opioid, Benzodiazepine, or Stimulant to assist the practitioner in avoiding overlapping prescriptions that could lead to overdose. Ultimately these visual indicators will aid practitioners in identifying patient risk behaviors and assist in identifying patients who may benefit from closer monitoring, reduction or tapering of opioids, prescribing of naloxone, or other measures to reduce risk of overdose. BNE continues to identify new states with which to develop data sharing agreements and will continue to explore the capacity of the RxCheck hub to further interstate interoperability. The PMP-EHR integration pilot project has demonstrated proof of concept and BNE is working to expand the number of sites engaged in PMP-EHR integration. BNE is exploring multiple options to meet this goal. NYSDOH (BNE and Office of Drug User Health) are currently working on revisions to the mandated prescriber training. This includes updating standards, guidance, language, and the addition of harm reduction concepts. |
BNE completed its technical build in March 2023 and released the new format in late May 2023. Within 6-9 months of release, BNE will conduct stakeholder engagement with PMP users to test system development and provide additional feedback regarding functionality. BNE continues to work with the Governance Board to aid in identification of state partners for interstate data sharing, as well as expand system knowledge to support NYSDOH's growth in the area of PMP-EHR integration. A revised version of the provider training will be completed in August 2023. |
- Improved Care Coordination and Transitions between Levels of Care
New York will implement policies to ensure residential and inpatient facilities link beneficiaries, especially those with OUD and other SUDs, with community-based services and supports following stays in these facilities. The table below outlines New York's current procedures for care coordination and transitions between LOCs to ensure seamless transitions of care and collaboration between services, including:
- Current content of specific policies to ensure these procedures;
- Specific plans to help beneficiaries attain or maintain a sufficient level of functioning outside of residential or inpatient facilities; and
- Current policies or plans to improve care coordination for co-occurring physical and mental health conditions.
New York has multiple interventions for coordinating the care of individuals with SUD and transitioning between LOCs including, but not limited to, facility credentialing, discharge, referral and transition requirements, and care management initiatives at DOH and OASAS. OASAS Providers utilize LOCADTR continuing care module to conduct ongoing assessments on the appropriateness of a level of care and to determine subsequent levels of care. OASAS has also utilized state Opioid Response dollars to support regional networks designed to improve successful transitions between residential and outpatient settings. Additionally grant funding has been utilized to support transportation initiatives which assist individuals with making successful connections to care.
Under the demonstration, New York will utilize the health home model and strengthen the transition management component for SUD populations between LOCs. DOH and OASAS will create a clear delineation of responsibility for improved coordination and transitions between LOCs to ensure individuals receive appropriate follow-up care following residential treatment.
In addition, under the demonstration, in order to ensure improved care coordination and transitions between LOCs, New York will also monitor access and healthcare outcome measures by demographic information, including race and ethnicity. In addition, New York intends to implement coverage of enhanced individualized care coordination for individuals with SUD that is designed to identify, prevent, and address health inequities and challenges related to social determinants of health. New York state will evaluate the use of peers and other care connection mechanisms to ensure improved care coordination and overall health outcomes for individuals in care.
This milestone will be met within 12 to 24 months of demonstration approval.
| Milestone Criteria | Current State | Future State | Summary of Actions Needed |
|---|---|---|---|
| Implementation of policies to ensure residential and inpatient facilities link beneficiaries with community-based services and supports following stays in these facilities. Additional policies to ensure coordination of care for cooccurring physical and mental health conditions |
New York has multiple interventions for coordinating the care of individuals with SUD and transitioning them between LOCs, including, but not limited to, facility credentialing, discharge planning requirements (including but not limited to needed referrals for services and medication continuation if appropriate, appointment times/dates) and care management initiatives with MCCPs. Service coordination in all ASAM LOCs is required. Service coordination, includes, but is not limited to, provider-specific and LOC-specific activities that enhance and improve linking members between Medicaid treatment services and enhance and improve the likelihood of engagement in treatment. |
Under the demonstration, OASAS will include all levels of services, including those over 16 beds in both managed care and fee for service environments. This will allow service recipients to obtain the full continuum of services as they progress in their recovery without interruption and will improve coordination and transitions between LOCs to ensure that individuals receive services and supports following stays in facilities and are retained in care. This will be done through increased clinical guidance and technical assistance, as well as data monitoring. There will also be increased case management staff/discharge planning staff as providers transition into the requirements of Part 820 regulations for service delivery and receive technical assistance and trainings/guidance from state Agency staff. 14 NYCRR Part 820 provides the staffing, programmatic and clinical requirements for the operation of a community based residential program providing stabilization, rehabilitation or reintegration services. MCCPs will be responsible for all residential levels of care which will allow them to coordinate services through an entire episode of care and provide care management. Providers will have an increased capacity to provide care management due to increase in care management staffing to better follow individuals to the next level of care or for a period post-discharge to ensure that linkages have been made. |
OASAS will improve discharge planning and transition planning in the residential and ambulatory LOCs using LOCADTR standards within 12 months of Demonstration approval. To improve care coordination, OASAS will provide technical assistance, engage in ongoing review and updating of guidance as issues are identified. OASAS will also work with providers as they transition to 820 service delivery mechanism around staffing and programming to meet regulatory standards and program guidance that has been issued. These actions will be completed on an as needed basis and do not require statutory revision. Future state will be achieved by implementing existing regulatory requirements that increase staff responsible for coordinating care and improving transitions to community services, including transitional planning. The state will also provide additional technical assistance to MCCPs on 820 reintegration level of care decisions within LOCADTR to ensure plans and providers are using the tool to fidelity. |
Section II - Implementation Plan Administration
Please provide the contact information for the state's point of contact for the Implementation plan.
Name and Title: Pat Lincourt, Associate Commissioner Email Address: Pat.Lincourt@oasas.ny.gov
Section III - Implementation Plan Relevant Documents
Please provide any additional documentation or information that the state deems relevant to successful execution of the implementation plan.
Attachment A: Template for Substance Use Disorder Health Information Technology Plan
Attachment A Section I.
As a component of Milestone 5, Implementation of Strategies to Increase Utilization and Improve Functionality of PDMPs, in SMDL 17-003, states with approved Section 1115 Substance Use Disorder (SUD) demonstrations are generally required to submit a SUD Health Information Technology (IT) Plan as described in the Special Terms and Conditions (STCs) for these demonstrations within 90 days of demonstration approval. The SUD Health IT Plan will be a section within the state's SUD Implementation Plan Protocol and, as such, the state may not claim federal financial participation for services provided in Institute for Mental Disease until the SUD Health IT Plan has been approved by CMS.
In the event that the state believes it has already made sufficient progress with regards to the health IT programmatic goals described in the STCs (i.e., PMP functionalities, PMP query capabilities, supporting prescribing clinicians with using and checking the PMP, and master patient index and identity management), it must provide an assurance to that effect via the assessment and plan below (see Table 1, "Current State"). SUD Demonstration Milestone 5.0, Specification 3: Implementation of Strategies to Increase Utilization and Improve Functionality of PMP
The specific milestones to be achieved by developing and implementing a Health IT Plan that can be used to address SUD include:
- Enhancing the health IT functionality to support PMP interoperability and integration.
- Enhancing and/or supporting clinicians in their usage of the state's PMP through improved functionality, education, and prescribing guidelines.
The state should provide CMS with an analysis of the current status of its health IT infrastructure "ecosystem" to assess its readiness to support PMP interoperability. Once completed, the analysis will serve as the basis for the health IT functionalities to be addressed over the course of the demonstration
– or the assurance described above.
The Health IT Plan should detail the current and planned future state for each functionality/capability/support – and specific actions and a timeline to be completed over the course of the demonstration – to address needed enhancements. In addition to completing the summary table below, the state may provide additional information for each Health IT/PMP milestone criteria to further describe its plan.
Table 1. State Health IT/ PDMP Assessment and Plan
| Milestone Criteria | Current State | Future State | Summary of Actions Needed |
|---|---|---|---|
5. Implementation of comprehensive treatment and prevention strategies to address Opioid Abuse and Opioid Use Disorder, that is:
|
Provide an overview of current PDMP capabilities, health IT functionalities to support the PDMP and supports to enhance clinicians' use of the state's health IT functionality to achieve the goals of the PDMP. | Provide an overview of plans for enhancing the state's PDMP, related enhancements to its health IT functionalities and related enhancements to support clinicians' use of the health IT functionality to achieve the goals of the PDMP | Specify a list of action items needed to be completed to meet the Health Information Include timeframe for completion of each action item |
| PDMP Functionalities | |||
| Enhancing and/or supporting clinicians in their usage of the state's PMP through improved functionality. |
|
Within the next two-years (2022-23) BNE plans to incorporate two phases of revisions into the PMP Registry patient search landing page. These enhancements are intended to enhance the functionality and usability of the PMP Registry. These will include an indicator that notes the type of medication prescribed (Opioid, Benzodiazepine, or Stimulant), whether the prescription is current, a highly visual summary dashboard that notes the number of pharmacies or practitioners visited by the practitioner in the past 30 days, and how many prescriptions are present for Opioids, Benzodiazepines, or Stimulants to assist the practitioner in avoiding overlapping prescriptions that could lead to overdose. Ultimately these visual indicators will aid practitioners in identifying patient risk behaviors and assist in identifying patients who may benefit from closer monitoring, reduction or tapering of opioids, prescribing of naloxone, or other measures to reduce risk of overdose. |
Through combined support from NYSDOH and the CDC funded Overdose Data to Action Grant, BNE will work with NYS ITS to build out the technical architecture. BNE plans to conduct stakeholder engagement with PMP users to test system functionality and provide additional feedback regarding functionality. |
| Enhancing and/or supporting clinicians in their usage of the state's PMP through education. |
|
BNE is working on an additional training series for pharmacists and dispensing vendors related to data submission to the PMP Registry and error correction to ensure the timeliness and accuracy of PMP data. Training development will be ongoing for the next two years. BNE is currently updating the mandated Opioid Prescriber Education training, with a target for completion within the next year. |
This work is scheduled and continues on a routine basis. It requires meetings with internal BNE partners. This work is being done in collaboration with the NYSDOH Office for Drug User Health and the State University of New York (SUNY) at Buffalo (UB). Scheduled work group meetings will be held to review and revise content and provide feedback to UB. |
| Enhanced interstate data sharing. |
|
BNE continues to identify new states with which to develop data sharing agreements and will continue to explore the capacity of the RxCheck hub to further interstate interoperability. | BNE continues to work with the Governance Board to aid in identification of state partners for interstate data sharing, as well as expand system knowledge to support NYSDOH's growth in the area of PMP-EHR integration. BNE will work with the VA and their integration vendor to ensure NYSDOH receives appropriate audit files in order for BNE to meet their responsibility in monitoring PMP access and use. |
| PMP-EHR Integration. Enhanced clinical workflow for prescribers and other state and federal stakeholders. |
|
The PMP-EHR integration pilot project had demonstrated proof of concept and BNE is working to expand the number of sites engaged in PMP-EHR integration. BNE is exploring multiple options to meet this goal. | BNE continues to work with the Governance Board to aid in identification of state partners for interstate data sharing, as well as expand system knowledge to support NYSDOH's growth in the area of PMP-EHR integration. |
| Enhanced connectivity between the state's PDMP and any statewide, regional or local health information exchange. | In previous years BNE explored PMP data sharing using health information exchanges (HIE) through the Regional Health Information Organizations (RHIOS) in NYS. At the time the RHIOs were not compatible with NYS security requirements. This resulted in NYSDOH exploring PMP-EHR integration, rather than data sharing through HIE. Currently, BNE is not supporting PMP data integration through HIE, though there is potential to revisit this in the future. | Potential exploration of the feasibility of PMP data sharing through HIE. | Potential exploration of the feasibility of PMP data sharing through HIE. |
| Use of PDMP – Supporting Clinicians with Changing Office Workflows / Business Processes | |||
| Develop enhanced provider workflow/business processes to better support clinicians in accessing the PMP prior to prescribing an opioid or other controlled substance to address the issues which follow | BNE, within the NYSDOH has demonstrated capacity to integrate PMP data into a healthcare system's EHRs BNE has initiated the process for EHR integration with the US Department of Veterans Affairs (VA). In previous years BNE explored PMP data sharing using health information exchanges (HIE) through the Regional Health Information Organizations (RHIOS) in NYS. At the time the RHIOs were not compatible with NYS security requirements. This resulted in NYSDOH exploring PMP-EHR integration, rather than data sharing through HIE. Currently, BNE is not supporting PMP data integration through HIE, though BNE is exploring the feasibility to revisit this in the future. |
The PMP-EHR integration pilot project had demonstrated proof of concept and BNE is working to expand the number of sites engaged in PMP-EHR integration. BNE is exploring multiple options to meet this goal, including the use of RxCheck as a method for supporting PMP-EHR integration. BNE is looking at the potential feasibility of revisiting PMP data sharing through HIEs. |
BNE will partner with federal and state partners through the Governance Board membership to identify additional options for expanding NYSDOH's PMP-EHR integration project. There is potential for NYSDOH to revisit the potential for integration through HEIs, but this is not a current active project. |
| Develop enhanced supports for clinician review of the patients' history of controlled substance prescriptions provided through the PDMP — prior to the issuance of an opioid prescription | The Bureau of Narcotic Enforcement (BNE), within NYSDOH is working to enhance the NYS PMP Registry to improve utilization and functionality. In 2021 NYS implemented a Morphine Milligram Equivalents (MME) calculator. Calculating the Total Daily MMEs of opioids helps practitioners to identify patients who may benefit from closer monitoring, reduction or tapering of opioids, prescribing of naloxone, or other measures to reduce risk of overdose. | Within the next two-year (2022-23) BNE plans to incorporate two phases of revisions into the PMP Registry patient search landing page. These will include an indicator that notes the type of medication prescribed (Opioid, Benzodiazepine, or Stimulant), whether the prescription is current, a highly visual summary dashboard that notes the number of pharmacies or practitioners visited by the practitioner in the past 30 days, and how many prescriptions are present for Opioids, Benzodiazepines, or Stimulants to assist the practitioner in avoiding overlapping prescriptions that could lead to overdose. Ultimately these visual indicators will aid practitioners in identifying patient risk behaviors and assist in identifying patients who may benefit from closer monitoring, reduction or tapering of opioids, prescribing of naloxone, or other measures to reduce risk of overdose. | BNE will work with NYS ITS to build out the technical architecture. BNE will conduct stakeholder engagement with PMP users to test system development and provide additional feedback regarding functionality. |
| Master Patient Index / Identity Management | |||
| Enhance the master patient index (or master data management service, etc.) in support of SUD care delivery. | The NYS PMP is not currently using a master patient index. The PMP is primarily used as one of many tools to support clinical decision making and is not currently used for tracking purposes. | If there is a future role for the NYS PMP it will need to be identified in collaboration with the Bureau of Narcotic Enforcement. | If there is a future role for the NYS PMP it will need to be identified in collaboration with the Bureau of Narcotic Enforcement. |
| Using PMP Data to aid in efforts to manage Medicaid payments for opioids | |||
| Leverage the above functionalities/ capabilities/ supports (in concert with any other state health IT, technical assistance or workflow effort) to provide support tools for practitioners to minimize the risk of inappropriate opioid overprescribing which can aid in management of efforts to mitigate inappropriate opioid payments by Medicaid inappropriately pay for opioids | Basic and advanced functionality of PMP allows practitioners to have an additional tool for their clinical decision making related to controlled substance providing. NYS Law related to 7-day supply also serves as a mechanism to decrease overprescribing. Practices can use Automated at Point-of-Service for Medicaid FFS to limit initial opioid prescriptions for a 7-day supply consistent with NYS Law. | Understanding where PMP data, NYS laws, and federal guidance, in collaboration with Medicaid health IT systems can work together to inform prescribing practices. | |
ATTACHMENT I
SUD Monitoring Protocol (Reserved)
ATTACHMENT J
HRSN Implementation Plan (Reserved)
ATTACHMENT K
Assessment of Beneficiary Eligibility and Needs, Infrastructure Planning, and Provider Qualifications for HRSN Services Protocol
ATTACHMENT L
Medicaid Hospital Global Budget Initiative Implementation Protocol (Reserved)
ATTACHMENT M
Provider Rate Increase Attestation Table (Reserved)
ATTACHMENT N
Approved List of DSHPs
| Program | Description | DSHP-Eligible Expenditures |
|---|---|---|
| Area Health Education Centers (AHEC) | The New York State Area Health Education Center (NYS AHEC) System is a workforce development initiative whose mission is to increase the diversity of qualified healthcare professionals by recruiting and training individuals of all races and ethnicities, with a special emphasis on medically underserved areas in both rural and urban communities. | $8,800,000 |
| Doctors Across New York (DANY) Diversity in Medicine | The DANY Diversity In Medicine program provides financial assistance to help train a diverse medical workforce in New York state. | $6,220,000 |
| DANY Physician Loan Repayment and Practice Support | Doctors Across New York (DANY) provides financial assistance to help train and place physicians in underserved communities in a variety of settings and specialties to care for New York's diverse population. | $54,420,000 |
| Health Care Workforce Bonus (HWB) Program | Front line health care and mental hygiene practitioners, technicians, assistants, and aides earning less than $125,000 annually, who provide hands on health or care services to individuals. | $766,998,088 |
| Health Workforce Retraining (Increase Training Capacity) | Grant funding for eligible organizations that seek to train or retrain health industry workers for new or emerging positions in the health care delivery system. transitions, reduce avoidable hospital readmissions and emergency room visits. | $28,186,550 |
| Nurses Across New York (NANY) | The NANY initiative is designed to help train and place nurses (RNs and LPNs) in underserved communities, in a variety of settings and specialties, to care for New York's diverse population. | $12,000,000 |
| Vital Access Providers Assurance Program (VAPAP) | The VAPAP program provides state-only support for facilities in severe financial distress to enable these facilities to maintain operations and provision of vital services while they implement longer-term solutions to achieve sustainable health care service delivery. | $2,404,793,968 |
| Alzheimer's Caregiver Support | Designed to support caregivers and people with dementia in the community using evidence-based strategies. Takes a two-pronged, systems approach to the investment—both focusing on community support while also equipping the medical system to provide early diagnoses, quality care management, and linkages to community services. | $105,468,000 |
| Cancer Services | The Cancer Services Program (CSP) provides breast, cervical and colorectal cancer screenings and diagnostic services at no cost to people who live in New York state, lack health insurance or have health insurance with a cost share that may prevent a person from obtaining screening and/or diagnostic services, and meet income eligibility/age requirements. | $89,300,000 |
| CSEA Buy-in | Grants to Civil Service Employee Association (CSEA) Local 1000, AFL-CIO to reduce the cost of providing health insurance, dental and vision benefits to covered child care providers. | $13,200,000 |
| Elderly Pharmaceutical Insurance Coverage (EPIC) | The Elderly Pharmaceutical Insurance Coverage Program provides secondary prescription drug coverage to Medicare-eligible individuals, assisting with drug costs after any Medicare Part D deductible is met and Part D premiums for low income individuals. | $250,068,000 |
| End of AIDS | Funding for Ending the Epidemic supports a range of activities, including but not limited to services delivered through contracts with providers, local health departments, community-based organizations, and a review agent; educational and awareness activities; enhanced surveillance; medications for uninsured persons; and expenses associated with linkage and retention collaboratives. | $60,000,000 |
| Expanded In-home Services for the Elderly (EISEP) | EISEP services include non-medical in-home services such as housekeeping, personal care, respite, case management, and related services (such as emergency response systems). EISEP services support and supplement informal care provided by clients' families. Clients are required to share the cost of services, based on income. These costs are determined by a sliding scale and range from no-cost to full-cost. | $20,000,000 |
| MLTC Ombudsman | ICAN (Independent Consumer Advocacy Network) is a group of nonprofit advocacy organizations, independent of the New York State Department of Health or any health insurance plan, which can: Answer Medicaid enrollee questions and give advice about MLTC plans for people who receive Medicaid or Medicare and long-term care; Solve problems between an enrollee's plan and providers (for example doctors, hospitals, and pharmacist); and Help enrollees file a complaint or appeal. | $20,000,000 |
| Newborn Screening | Newborn screening refers to medical tests, the majority of which are genetic, performed to identify babies with certain disorders, which without intervention, may permanently impact newborns and their families. Early recognition and treatment of most of these disorders leads to a better outcome for the newborn. The Newborn Screening Program's goal is to help affected babies live as long and normal of a life as possible. The Newborn Screening Program effectively identifies babies with certain disorders and is required for all newborns born in New York state unless the parents confirm, in writing, that they have a religious objection. | $38,941,504 |
| NY Connects | NY Connects is a locally based No Wrong Door (NWD) system that provides one stop access to free, objective, comprehensive information and assistance on long term services and supports for people of all ages or with any type of disability. The NY Connects NWD System is administered through a collaboration between the Area Agencies on Aging (AAAs), Local Departments of Social Services (LDSS), and six regionally contracted Independent Living Centers (ILCs). | $95,600,000 |
| Obesity - Diabetes Prevention Programs | The Department of Health works with many partners and contractors to develop and implement a range of obesity prevention programs in community, child care, school and heath care settings. | $23,880,000 |
| Supportive Housing Initiative | The Supportive Housing Initiative seeks to ensure that Medicaid members have proper housing that promotes a healthy environment and lifestyle as a social determinant of health. These resources utilize innovative housing program models to provide support services. | $163,212,000 |
| Tobacco Control | The Department through the Bureau of Tobacco Control administers the state's comprehensive Tobacco Control Program to reduce illness, disability, and death related to commercial tobacco use and secondhand smoke exposure, and to alleviate social and economic inequities caused by tobacco use. The program uses an evidence-based, policy-driven, and population-level approach to tobacco control and prevention with a commitment to promote health equity among populations disproportionately impacted by tobacco marketing and use. The Tobacco Control Program's efforts and actions have contributed to record-low youth and adult smoking rates in New York state. | $162,576,000 |
| Total Allowable DSHP-Eligible Expenditures | $4,323,664,110 | |
| Total DSHP Cap. The state must not claim more than $3,981,442,500 of DSHP. | $3,981,442,500 | |
ATTACHMENT O
DSHP Claiming Protocol (Reserved)
ATTACHMENT P
Monitoring Protocol for Other Policies (Reserved)
ATTACHMENT Q
DSHP Sustainability Plan (Reserved)
_______________________________
1. See SMD #17-003 RE: Strategies to Address the Opioid Epidemic. 1
2 Medically needy refers to those who have the option of spousal impoverishment budgeting, including post eligibility when it is more beneficial. Medically needy is defined as an individual who is not eligible for, or in receipt of public assistance or SSI (or the state supplement), because his/her income and/or resources are in excess of cash assistance standards, but who has insufficient income and/or resources to meet the cost of his/her necessary medical and remedial care (42 CFR 435.320 (aged), 435.322 (blind) and 435.324 (disabled)). 2
3 All beneficiary protections apply to MMMC, MLTC and HARPs, unless otherwise noted in STC 5 3
4 Throughout these STCs, the term "Health Home," unless otherwise noted, only refers to Health Homes approved under section 1945 of the Act and consistent with approved NY Health Home state plan benefits for Health Homes SPA for IDD, Health Homes SPA for children, and/or Health Home SPA for Chronic Medical and SSI Health Home program. 4
5 Prescription drug monitoring programs (PDMP) are electronic databases that track controlled substance prescriptions in states. PDMPs can provide health authorities timely information about prescribing and patient behaviors that contribute to the "opioid" epidemic and facilitate a nimble and targeted response. 5
6 Ibid. 6
7 Demographic and HRSN data should include all of the following categories: race, ethnicity, primary language, disability status, sexual orientation, gender identity, and health-related social needs. 7
8 For a description of CMS's current policies related to budget neutrality for Medicaid demonstration projects authorized under section 1115(a) of the Act, see State Medicaid Director Letter #18-009. 8
9. 42 CFR §431.420(a)(2) provides that states must comply with the terms and conditions of the agreement between the Secretary (or designee) and the state to implement a demonstration project, and §431.420(b)(1) states that the terms and conditions will provide that the state will perform periodic reviews of the implementation of the demonstration. CMS's current approach is to include language in STCs requiring, as a condition of demonstration approval, that states provide, as part of their periodic reviews, regular reports of the actual costs which are subject to the budget neutrality limit. CMS has obtained Office of Management and Budget (OMB) approval of the monitoring tool under the Paperwork Reduction Act (OMB Control No. 0938 - 1148) and in states agree to use the tool as a condition of demonstration approval. 9
10 14 NYCRR 817.3(d)(1) and 14 NYCRR 800.4 10
11 New York State Public Health Law Article 33 Section 3331 (5).https://www.nysenate.gov/legislation/laws/PBH/3331 11
12 New York State Opioid Annual Report 2020. https://www.health.ny.gov/statistics/opioid/data/pdf/nys_opioid_annual_report_2020.pdf 12
13 CMS Informational Bulletin: https://www.hhs.gov/guidance/sites/default/files/hhs-guidance-documents/cib080519-1004_64.pdf 13
14 Good Samaritan Law was enacted as Chapter 154 of 2011; Publicly available brochure can be found at: https://www.health.ny.gov/publications/0139.pdf 14
15 Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain - United States, 2016. MMWR Recomm Rep 2016;65(No. RR-1):1-49. DOI: http://dx.doi.org/10.15585/mmwr.rr6501e1 15
Follow Us