UPDATE ON THE TRANSITION OF FFS COMMUNITY BASED LTC SERVICES TO MLTC MODEL
- Presentation is also available in Portable Document Format (PDF)
Margaret O. Willard
mow01@health.state.ny.us
NYS Department of Health
NYPWA Winter Conference 2013
Medicaid Redesign Team (MRT) #90
- Established by Governor Cuomo in January 2011, the Medicaid Redesign Team brought together stakeholders and experts from throughout the state to work cooperatively on reforming New York State´s health care system and improve the provision of care.
- MRT 90 focuses on the transition of long–term community–based services into managed long–term care models.
- In order to achieve this goal, strong partnerships have been forged between stakeholders, the Department of Health, NYC/HRA and the enrollment broker, NY MA Choice.
CMS APPROVAL
- On August 31, 2012, the Department received written approval from CMS to move forward with MRT #90 Initiative
- Approval was granted to fully implement the transition and enrollment of individuals requiring community–based long–term care into Managed Long Term Care Plans or Care Coordination Models
MANDATORY INITIATIVE
- The definition of community–based long–term care services includes:
- Personal Care Services
- Home Health Services
- Adult Day Health Care
- Private Duty Nursing
MANDATORY ENROLLMENT
- Mandatory enrollment in New York City began September 19th when the door was closed to new Personal Care Services Program referrals
- All new cases are referred by HRA to one of the following programs based on need and preference: New York Medicaid Choice; LTHHCP; NHTD; or TBI waivers (if eligible)
MANDATORY TARGET POPULATION
Who needs to enroll?
The 2011 Budget legislation requires that all dual eligibles who are:
- Age 21 and older and in need of community–based long–term care Services for more than 120 days must enroll in a Managed Long Term Care Plan or other Care Coordination Model.
- Duals between 18 and 21 remain voluntary
VOLUNTARY POPULATIONS
In addition to those who must enroll in a Managed Long Term Care Plan or Care Coordination Model, the following individuals may voluntarily enroll:
- Dual eligible, 18–21 in need of community–based long–term care services for over 120 days.
- Non–dual eligibles, age 18 and older assessed as nursing home eligible.
TYPES OF PLANS
A prospective enrollee has a choice of three Managed Long Term Care Plans:
- Partially Capitated Managed LTC (Medicaid)
Benefit package is long–term care and ancillary services including home care, unlimited nursing home care - Program of All–Inclusive Care for the Elderly (PACE) (Medicare and Medicaid)
Benefit package includes all medically necessary services – primary, acute and long–term care - Medicaid Advantage Plus (MAP) (Medicare and Medicaid)
Benefit package includes primary, acute and long–term care services (excludes some specialized mental health services).
SERVICES INCLUDED
- Audiology
- Dental Services
- Home Care including Nursing, Home Health Aide, Occupational, Physical and Speech Therapies
- Home Delivery and/or Meals in a Group Setting
- Durable Medical Equipment
- Medical and Surgical Supplies
- Non–Emergency Transportation
- Nursing Home Care
- Nutrition and Nutritional Supplements
- Optometry/Eyeglasses
- Personal Care (such as assistance with bathing, eating, dressing, etc.)
- Personal Emergency Response Services
- Podiatry
- Private Duty Nursing
- Prosthesis and Orthotics
- Outpatient Rehabilitation Therapies
- Respiratory Therapy
CONSUMER OUTREACH & EDUCATION–Mandatory Program
- Announcement Notice
- Mandatory Notice
- 60–day choice period begins with this notice
- 10–day Outreach Call
- 30– day Reminder Notice
- 45–day Reminder Notice (with outreach call)
Notices are available in English, Spanish, Russian and Chinese.
IMPLEMENTATION
- Beginning September 17, 2012 any New York City dual eligible consumer, aged 21 and over, newly requiring community–based long–term care of 120 days must enroll in a Managed Long Term Care plan to receive these services.
- HRA is no longer accepting referrals for the PCSP or CDPAP. LTHHCP and waivers continue to be a choice for consumers.
EXEMPTIONS AND EXCLUSIONS
- Mandatory enrollees may request to be exempt or excluded from joining a MLTC plan due to a specific circumstance or unique health care need.
- Enrollment Broker´s (New York Medicaid Choice– NYMC) Client Service Representatives (CSRs) educate enrollees about the exemption and exclusion process; explain the specific criteria that must be met and send the exemption or exclusion packet when appropriate.
- Approved applications:
- Individual will remain on FFS Medicaid
- Individual is automatically disenrolled
- NYMC will send the individual notification
- Denied applications:
- Individual will receive a notice informing them of the denial and fair hearing options
ENROLLING IN A MLTC PLAN
- NYMC can only process enrollments into Partial Plans for individuals who received mandatory notices.
- Calls from individuals requesting enrollment into a MAP or PACE plan will be “warm transferred” to the plan of choice.
- Plans will submit electronic enrollments to NYMC.
- NYMC will send a confirmation notice to the enrollee once the enrollment is accepted.
ENROLLEES WHO REQUIRE PCS
- Once an enrollee has chosen a plan, that plan will be responsible for assessing the enrollee and determining their eligibility for community–based long–term care.
- After the enrollee has been assessed for services and has agreed to enroll in a specific MLTC plan (signed an enrollment form), the plan will send the enrollment electronically to New York Medicaid Choice.
- Enrollments received by the 20th of the month at noon will be effective the first of the following month.
- Enrollments received after the 20th at noon will be enrolled effective the 1st of the next month.
TRANSITION of UNDERCARE POPULATION
- June 2012: New York County began process (announcement letters followed w/in 30 days with mandatory notification then 60 days to select plan)/ All boroughs by November 2012 then continue
- January 2013: initiate enrollment of PCS, CDPAP and ADHC in Suffolk, Nassau and Westchester counties. Initiate enrollment of ADHC in NYC.
- CHHA and PDN to be transitioned in the near future
- LTHHCP to be transitioned upon approval of 1915c HCBS waiver
SERVICE PLAN WILL CONTINUE for 60 DAYS
If a reduction in hours is proposed before authorization ends, must issue a Notice of Action
- Enrollee has right to appeal rights with aid continuing
- Fair hearing rights if appeal is adverse to enrollee
ENROLLEE RIGHTS
- A member can file a complaint or grievance. This can be done verbally or in writing.
- A member can file an appeal for reconsideration of a decision. There are two types of appeals:
- Expedited Appeal – responded to within 72 hours by telephone, fax or other available method. Written notification follows.
- Standard Appeal – responded to within 14 days. The plan must send written notice to the member within two (2) business days of the determination.
- A member can file for a Fair Hearing. This can be done verbally or in writing. The target timeframe for fair hearing resolution should be within 60 days of the request for the hearing.
MLTC ENROLLMENT
Statewide Enrollees in MLTC: 74,726 (As of 12/31/12)
- NYC: Partial Cap: 63,943, PACE 3131, Medicaid Advantage Plus: 2594 = 69,668
- ROS: Partial Cap: 3233, PACE 1463, Medicaid Advantage Plus: 362 = 5058
- TOTAL: Partial Cap: 67,176, PACE 4594, Medicaid Advantage Plus 2956 = 74,726
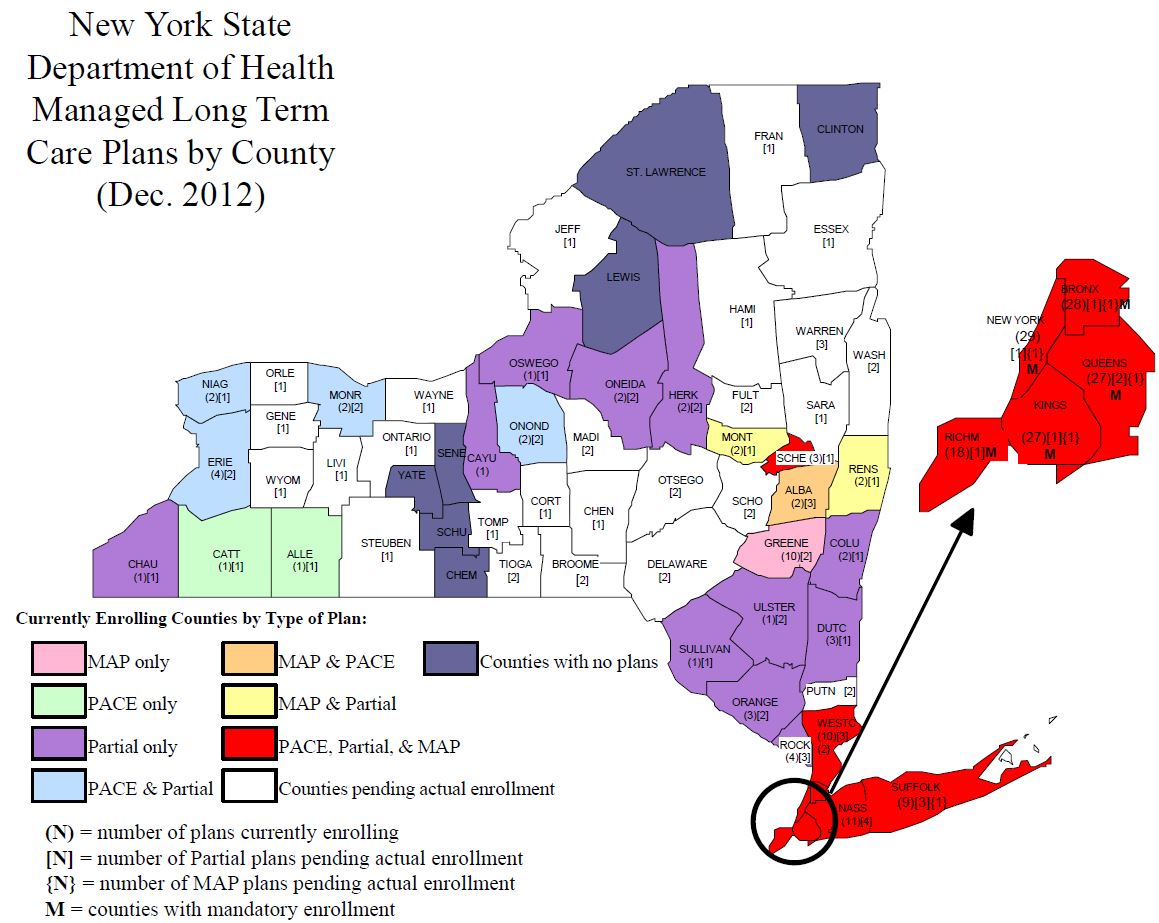
Number of Actively Enrolling Plans:
- Partial Caps: 22 (19 Serve NYC) PACE: 8 (2 Serve NYC) Medicaid Advantage Plus: 10 (10 Serve NYC)
MLTC APPLICATION STATUS
1/1/12 – 12/31/12
| Under Review/Pending Approval | Approved | |
|---|---|---|
| Full Certificate of Authority | 30 (29 partial cap; 1 CCM) | 5 (all partial cap) |
| Geographic Expansions (of currently operational plans) | 29 (21 partial cap; 4 PACE; 4 MAP) | 16 (13 partial cap; 1 PACE; 2 MAP) |
| New Line of Business (added to a currently operational plan) | 9* (7 partial cap; 2 Medicaid Advantage Plus) *One plan is adding both a partial and a MAP |
6 (4 partial cap; 2 Medicaid Advantage Plus) |
NEXT PHASES
As plan capacity is established, dually eligible community–based long–term care service recipients will be enrolled as follows:
- Phase III: Rockland and Orange Counties – Anticipated June 2013.
- Phase IV: Albany, Erie, Onondaga and Monroe Counties
– Anticipated December 2013. - Phase V: Other counties with capacity – Anticipated June 2014
FINAL PHASE
Phase VI: Previously excluded dual eligible groups contingent upon development of appropriate programs:
- Nursing Home Transition and Diversion waiver participants
- Traumatic Brain Injury waiver participants
- Assisted Living Program participants
ROLE OF HRA
- HRA is working with DOH and the MLTC plans to help ensure a smooth transition of the personal care population to a MLTC plan.
- HRA will continue to retain responsibilities for all aspects of Medicaid eligibility and renewal for individuals enrolled in the Managed Long Term Care Program.
Follow Us