January 2009
Volume 25, Number 1
New York State Medicaid Update
The official newsletter of the New York Medicaid Program
David A. Paterson, Governor
State of New York
Richard F. Daines, M.D. Commissioner
New York State Department of Health
Deborah Bachrach, Deputy Commissioner
Office of Health Insurance Programs
Dear Medicaid Provider,

Happy New Year! Welcome to the January 2009 edition of the Medicaid Update newsletter.
We want to hear from you!. Do you have news to share for future issues of the Medicaid Update? If you have a patient or office success story, a procedural or administrative tip or other information that might be of interest to your fellow providers, please e-mail us at: medicaidupdate@health.state.ny.us.
Please don't hesitate to contact us or you can visit us online at http://www.nyhealth.gov to learn more about our latest initiatives.
The Medicaid Update is a monthly publication of the New York State Department of Health and contains information regarding the care of those enrolled in the Medicaid program.
In this issue....

Policy and Billing Guidance
Ambulette providers are required to submit vehicle information
Attention ALP Providers
New York State Medicaid Inspector General Bureau of Investigations & Enforcement Ambulette Questionnaire
Hearing Aids Now Approved Through DVS
PHARMACY UPDATES
Preferred Drug Program Update
Family Health Plus Pharmacy Benefit Update
NEWS FOR ALL PROVIDERS
Important Change With Issuance of IRS Form 1099
Smoking Cessation
Provider Services
AMBULETTE PROVIDERS - 2009 SURVEY DUE 2/17/2009
Ambulette providers are required to submit vehicle information
Return to Table of Contents
Providers of Ambulette services are required to submit vehicle information on an annual basis in accordance with Title 18 NYCRR (New York Code, Rules and Regulations) 502.6(b).
All Ambulette providers must, during the month of January of each year, disclose to the department in writing, information concerning those vehicles currently owned or leased by the provider. The required information is outlined in the Ambulette Questionnaire.
An Ambulette provider that fails to disclose this information may have its participation in the medical assistance program terminated.
The form must be returned by February 17, 2009 to:
New York State Office of the Medicaid Inspector General
Investigations & Enforcement
Attn: 2009 Ambulette Survey
800 North Pearl St, Lower Level
Albany, New York 12204
Certified/Return Receipt mail is recommended. A copy of the form and proof of mailing should be retained for your records. In the event of non-receipt of the form by the Office of the Medicaid Inspector General, this proof will be used to validate compliance.
The Annual Ambulette Survey form is available on the OMIG Website under "Provider Compliance" at: http://www.omig.state.ny.us/data/images/stories/annual_ambulette_survey_for_2009.pdf.
Please Note: Failure to comply may result in the termination of enrollment as a Medicaid Provider.

Attention Providers
Return to Table of Contents
The contract between Assisted Living Programs (ALP - Category of Service 0267) and the local social services district requires ALPs to immediately notify the local district when one of their Medicaid clients enters a hospital to receive inpatient care.
Effective March 1, 2009, the Department of Health will edit ALP claims that are billed while the client is hospitalized. Any ALP claim that is denied will receive the following edit message: Edit 00760 (Duplicate Inpatient/Nursing Home, Clinic, Referred Ambulatory, DME, or Lab).
Questions regarding this change should be directed to the eMedNY Call Center at (800) 343-9000.

NEW YORK STATE MEDICAID INSPECTOR GENERAL
Bureau of Investigations & Enforcement
AMBULETTE QUESTIONNAIRE
Return to Table of Contents
Provider Information
PROVIDER NAME: _________________________________________________________________________________________________________________
ADDRESS:________________________________________________________________________________________________________________________
NEW YORK MEDICAID PROVIDER # ____________________________________________________________________________________________________
IF ADDITIONAL SPACE IS NEEDED, PROVIDE INFORMATION BY ATTACHMENT
General Information
Business phone number: (______)________________________Fax Number: (____)__________________________________________________________
Business Website: _______________________________________________________________________________________________________________
List any change in the business name and address if different from above:
__________________________________________________________________________________________________________________________
__________________________________________________________________________________________________________________________
IDENTIFY THE FOLLOWING PERSONNEL (PLEASE TYPE OR PRINT):
OWNER 1:___________________________________________________________________________________________________________________
OWNER 2: __________________________________________________________________________________________________________________
PRESIDENT: _________________________________________________________________________________________________________________
VICE PRESIDENT: ____________________________________________________________________________________________________________
SECRETARY: ________________________________________________________________________________________________________________
TREASURER:_________________________________________________________________________________________________________________
CHIEF EXECUTIVE OFFICER (CEO): ______________________________________________________________________________________________
General Questions
1. Does the business have more than one New York Medicaid provider number(s) or National Provider identifier (NPI) number?
Yes ? No ?
If yes, list the additional New York Medicaid provider/NPI number(s):
__________________________________________________________________________________________________________________
2. Do you, or any other owners/officers of the business, own or have an equity interest in other businesses that provide transportation services, whether a Medicaid provider or not?
Yes ? No ?
Please list these businesses by name and New York Medicaid provider/NPI number.
__________________________________________________________________________________________________________
3. Does the business operate from any location(s) other than the address listed above?
Yes ? No ?
If yes, identify the location(s):
________________________________________________________________________________________
4. Does the business have a Medicaid provider agreement in another state(s)?
Yes ? No ?
If yes, identify the state(s) and provider's name(s) and number(s):
_________________________________________________________________________________________________________
5. Approximately what percent of the business' customer population is Medicaid eligible?_________________________%
6. On average, how many Medicaid consumers does the business service per month? _________________________
7. Does the business have a service contract with a physician, group or nursing home, clinic, or hospital for the purpose of transporting Medicaid consumers?
Yes ? No ?
If yes, please attach a list of those physicians, group or nursing homes, clinics, or hospitals with which the business has service contracts.
8. Does ANY INDIVIDUAL employed (full or part time) by the company have (or has ever had) any other Medicaid provider number(s), whether currently active or inactive?
Yes ? No ?
If yes, identity the provider name(s) and number(s):
PROVIDER NAME: _____________________________________________ PROVIDER NUMBER: ____________________
PROVIDER NAME: _____________________________________________ PROVIDER NUMBER: ____________________
PROVIDER NAME: _____________________________________________ PROVIDER NUMBER: ____________________
PROVIDER NAME: _____________________________________________ PROVIDER NUMBER: ____________________
PROVIDER NAME: _____________________________________________ PROVIDER NUMBER: ____________________
9. Does the business have a contract with any Medicaid managed care programs?
Yes ? No ?
If yes, identify the names of the programs and the length of the contract:
______________________________________________________________________________________________________________________________________________________________
_________________________________________________________________________________________________________________________________________________________________
Record Keeping
1. List all transport records that are used any business day for the purpose of logging in and tracking the transports:
_________________________________________________________________________________________________
_________________________________________________________________________________________________
_________________________________________________________________________________________________
________________________________________________________________________________________________
_________________________________________________________________________________________________
_________________________________________________________________________________________________
2. Who is responsible for filing and maintaining the transport records? List name(s) and titles:
________________________________________________________________________________________________
_________________________________________________________________________________________________
Identify below (or attach) a list detailing any/all abbreviations or coding which are used in the records:
_________________________________________________________________________________________________
_________________________________________________________________________________________________
3. Where are your business records and supporting documentation for Medicaid claims stored/maintained?
________________________________________________________________________________________________
_________________________________________________________________________________________________
4. Are you keeping all records and documents necessary to substantiate transportation services for which Medicaid reimbursement is sought for at least six (6) years, as required by NYCRR 517.3 (b)
Yes ? No ?
Vehicles
1. Indicate the total number of vehicles currently in operation: Ambulette: ___________
2. Are the transport vehicles housed at or dispatched from another location(s)?
Yes ? No ?
If yes, identify the location(s):
_________________________________________________________________________________________________
________________________________________________________________________________________________
_________________________________________________________________________________________________
_________________________________________________________________________________________________
Medicaid Policy Updates
1. Does the business have internet access to Medicaid policy updates via the eMedNY Website?
http://www.emedny.org/ProviderManuals/Transportation/index.html
Yes ? No ?
2. Are you familiar with all the requirements set forth in the transportation provider manual?
http://www.emedny.org/ProviderManuals/Transportation/index.html
Yes ? No ?
If no, please explain:
_________________________________________________________________________________________________
_________________________________________________________________________________________________
________________________________________________________________________________________________
_________________________________________________________________________________________________
3. Are you aware that in order for an ambulette transport to be covered by Medicaid, the individual being transported must actually be rendered personal assistance as defined by the manual?
http://www.emedny.org/ProviderManuals/Transportation/index.html
Yes ? No ?
If yes, when did you become aware of this requirement? __________________________________________________
If no, please explain: _______________________________________________________________________________
_________________________________________________________________________________________________
4. Are you aware that in order for an ambulette transport to be covered by Medicaid, the individual being transported must be transported to or from a Medicaid covered service?
Yes ? No ?
If yes, when did you become aware of this requirement?
__________________________________________________
If no, please explain: _______________________________________________________________________________
_________________________________________________________________________________________________
5. Are you aware that in order for an ambulette transport to be covered by Medicaid, the individual being transported must be transported in an ambulette, licensed and approved as such by the New York State Department of Transportation/New York City Taxi and Limousine Commission (where applicable)?
Yes ? No ?
If yes, when did you become aware of this requirement? ______________________________________________________
If no, please explain: ___________________________________________________________________________________
_____________________________________________________________________________________________________
6. Are you aware that in order for an ambulette transport to be covered by Medicaid, you must have on file a Prior Approval signed by an ordering Practitioner covered under 18 NYCRR 505.10(c)(2),
for the individual being transported?
Yes ? No ?
If yes, when did you become aware of this requirement? ______________________________________________________
If no, please explain: ___________________________________________________________________________________
______________________________________________________________________________________________________
7. Are you aware that you are not permitted to seek Medicaid reimbursement for transportation services provided by another entity?
Yes ? No ?
If yes, when did you become aware of this requirement? ______________________________________________________
If no, please explain: ___________________________________________________________________________________
_____________________________________________________________________________________________________
8. Are you aware that the use and services of any vehicles and/or drivers leased from another transportation company must be leased from a transportation company that is enrolled as a provider in the Medicaid program?
Yes ? No ?
If yes, when did you become aware of this requirement? ______________________________________________________
If no, please explain: ___________________________________________________________________________________
_____________________________________________________________________________________________________
Billing and Fees
1. Did the business use an outside billing company to submit invoices to CSC?
Yes ? No ?
a. If yes, identify the billing company name, address, New York Medicaid provider/NPI number, and the contract period:
__________________________________________________________________
b. If no, identify the individual(s) in the business who completed the invoices submitted to CSC:
Name: _____________________________ Title: ________________________
Name: _____________________________ Title: ________________________
c. Identify the individual(s) who assigned the billing codes:
Name: _____________________________ Title: ________________________
Name: _____________________________ Title: ________________________
2. What Medicaid billing codes does your company utilize? Please list all the codes and a description of each code.
Code: __________ ______________________________________________________
Code: __________ ______________________________________________________
Code: __________ ______________________________________________________
Code: __________ ______________________________________________________
Prepared by (Name/Title)
___________________________________________ Date____________
Signature of Owner #1 ____________________________________________ Date____________
Signature of Owner #2 ____________________________________________ Date_____________

DAYS OPEN AND HOURS OF OPERATION
S ____ M _____ T _____ W _____ TH ____ F _____ S _____
List All Vehicles
| Check One | |||||
| DMV Plate Number | Vehicle Identification Number (VIN#) | Passenger Capacity | Owned | Leased | Leased from |
NYS DOT OPERATING CERTIFICATE #_________________________________________
Policy and Billing Guidance
Hearing aids are now approved through DVS
Return to Table of Contents
Effective September 1, 2008, prior authorization for all hearing aids for children and adults may now be obtained through the automated electronic Dispensing Validation System (DVS). A DVS request is submitted in "real time," which means that the status of the request will be available by the end of the DVS session. Speech and hearing centers, hearing aid vendors and dispensing audiologists must obtain an electronic DVS number prior to providing a hearing aid and must report it on the claim for payment to be made.
Prior approval requests for hearing aids received after March 1, 2009, will be rejected with the message, "Invalid Access Method," if a provider does not use DVS. Providers receiving a service limit rejection through DVS may submit a DVS override through the prior approval process with medical documentation attached as to why the service limits need to be overridden.
Ordering and dispensing providers
The actual provider identification number of the qualified ordering provider must be entered in the ordering provider identification field on prior authorizations and claims. Licensed audiologists, physicians and nurse practitioners are qualified to order hearing aids. No facility or center provider identification numbers are allowed in the ordering provider field due to HIPAA/NPI requirements.
Reporting and Technical Information
A hearing aid DVS authorization will be granted for an approved period of service of 180 days, and can be cancelled by the provider within 90 days of the authorization date. For monaural aids, the left (LT) or right (RT) modifier must be reported on the DVS request and claim. Binaural aids do not require a modifier.
Providers may use one of two methods to obtain a DVS prior authorization number:
- Medicaid Eligibility Verification System (MEVS) card swipe terminal, the VeriFone Omni 3750 (instructions for use are available at:
( ); http://www.emedny.org/ProviderManuals/AllProviders/Omni_3750_Supplemental_Guide/1_3/Omni3750_Supplemental_Guide.html
or - e-PACES free personal computer software instructions are available at: (http://www.emedny.org/HIPAA/SupportDocs/ePACES.html).
Questions? For additional information and assistance with obtaining a DVS or to obtain eMedNY Prior Approval Request Form 283202 (paper form) for DVS overrides, please contact Computer Sciences Corporation (CSC) at (800) 343-9000.
Instructions on prior approval submission are available at: http://www.emedny.org/ProviderManuals/HearingAid/PDFS/HearingAid_PA_Guidelines.pdf
For information regarding general Medicaid coverage of hearing aids or a specific prior approval submission, please call the Medical Prior Approval Bureau at (800) 342-3005, Option # 1.
Effective February 18, 2009
Preferred Drug Program Update
Return to Table of Contents
The New York State Medicaid Pharmacy and Therapeutics (P&T) Committee recently conducted a review of 11 drug classes subject to the Preferred Drug Program (PDP). Effective February 18, 2009, prior authorization requirements will change for some drugs in the following two drug classes:
- Anticholinergics - Inhaled
- Beta2 Adrenergic Agents - Inhaled Short Acting
In addition to these changes, the PDP is also expanding to include two new drug classes. Prescriptions written on or after February 18, 2009, for drugs in the following classes will be subject to the PDP:
- Dipeptidyl Peptidase-4 (DPP-4) Inhibitors
- Multiple Sclerosis Agents
To obtain prior authorization for non-preferred drugs, please call the pharmacy prior authorization clinical call center at (877) 309-9493 and follow the appropriate prompts.
Following is the most up-to-date Preferred Drug List (PDL), with a full listing of preferred and non-preferred drugs for each of the drug classes currently subject to the PDP: https://newyork.fhsc.com/downloads/providers/NYRx_PDP_PDL.pdf
Additional information, such as a "Quick List" of only preferred drugs and updated prior authorization forms, is available at each of the following Websites:
http://www.nyhealth.gov or http://www.eMedNY.org or https://newyork.fhsc.com

Remember: Preferred drugs do not require prior authorization!
For clinical concerns or preferred drug program questions, contact (877) 309-9493.
For billing questions, contact (800) 343-9000.
For Medicaid pharmacy policy and operations questions, call (518) 486 -3209.
Pharmacy Update
Family Health Plus Pharmacy Benefit
Return to Table of Contents
As of October 1, 2008, the pharmacy benefit for Family Health Plus managed care enrollees is "carved-out" of the managed care plan benefit package and is administered by Medicaid as a fee-for-service benefit. Family Health Plus enrollees were issued a Medicaid Benefit Identification Card to obtain their pharmacy benefit.
Family Health Plus enrollees must use their Medicaid Benefit Identification Card to obtain pharmacy services.
If enrollees were already using a Medicaid Card to obtain other benefits, they can use the same card to access their pharmacy benefits. If an enrollee did not receive a card, they should contact their local Department of Social Services or in New York City, contact HRA, and request an ID card.
The Family Health Plus pharmacy benefit includes:
- Prescription drugs
- Insulin and diabetic supplies currently covered as a pharmacy benefit by Medicaid (e.g., insulin syringes, blood glucose test strips, lancets, alcohol swabs)
- Smoking cessation agents, including OTC products
- Select OTC medications covered on the Medicaid Preferred Drug List (Prilosec OTC, loratadine, Zyrtec) and OTC vitamins currently covered by Medicaid
- Hearing aid batteries
- Enteral formulae
Prescriptions for Family Health Plus enrollees are subject to all Medicaid program requirements.
Providers may need to obtain prior authorization from Medicaid for certain prescription drugs through the following initiatives:
- the Clinical Drug Review Program (CDRP),
- the Preferred Drug Program (PDP),
- the Mandatory Generic Drug Program (MGDP).
Information on these programs is available at https://newyork.fhsc.com or through the Clinical Call Center at (877) 309-9493.
Prior authorization for enteral formula must be obtained through the automated voice interactive telephone system at (866) 211-1736.
- Drug co-payments for Family Health Plus enrollees did not change. Co-payments remain at $6.00 for brand-name drugs, $3.00 for generic drugs, $1.00 for diabetic supplies, hearing aid batteries and enteral formulae, and $0.50 for covered over-the-counter drugs. For more information, refer to the April 2006 Medicaid Update, "Family Health Plus Co-payment Information."
- With the exception of controlled substances, prescriptions must be filled within 60 days and are valid for 6 months from original prescription date with up to 5 refills.
- Drugs administered in the physician's office (J-Code drugs) remain in the managed care benefit package and should continue to be billed to the enrollee's Family Health Plus managed care plan.
Questions? Contact Medicaid Pharmacy Policy & Operations staff at (518) 486-3209.

APG Bulletin Update
Important Change with issuance of IRS Form 1099
Return to Table of Contents
Computer Sciences Corporation (CSC), the eMedNY contractor for the Department of Health (DOH), issues IRS (Internal Revenue Service) Form 1099 to providers at the beginning of each year for the previous year's Medicaid payments.
In previous years, a 1099 would be issued for each Medicaid Provider Number. Beginning in January 2009, however, 1099s will be issued by taxpayer identification number (TIN). Therefore, if multiple provider identifiers (Medicaid Provider Numbers or National Provider Identifiers) share a common TIN, only one 1099 will be issued.
As with previous years, please note that the IRS 1099 amount is not based on the date of the checks; rather, it is based on the date the checks were released to providers.
Due to the two-week check lag between the date of the check and the date the check is issued, the IRS 1099 amount will not correspond to the sum of all checks issued for your provider identification number during the calendar year.
The IRS 1099 that will be issued for the year 2008 will include the following:
- Check dated 12/17/07 (Cycle 1582) released on 01/02/2008 through,
- Check dated 12/15/08 (Cycle 1634) released 12/31/08.
Additionally, in order for group practice providers to direct Medicaid payments to a group identification number and corresponding IRS 1099, providers are reminded that they must submit the group identification number in the appropriate field on the claim (paper or electronic).
Claims that do not have the group identification number entered will cause payment to go to the individual provider and his/her IRS 1099. Please note that 1099s are not issued to providers whose yearly payments are less than $600.00.
IRS 1099s for the year 2008 will be mailed no later than January 31, 2009.
Questions? Please contact the eMedNY Call Center at (800) 343-9000.
Smoking Cessation
Return to Table of Contents
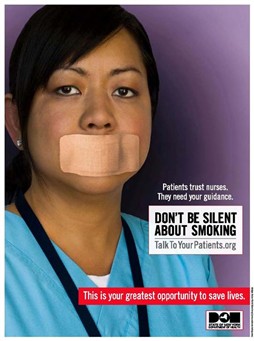
By providing counseling, pharmacotherapy, and referrals, you can double your patients' chances of successfully quitting.
For more information, visit http://www.talktoyourpatients.org or call the NY State Smokers' Quitline at 1-866-NY-QUITS (1-866-697-8487).
Do you suspect that a Medicaid provider or an enrollee has engaged in fraudulent activities?
Return to Table of Contents
Call: 1-877-87FRAUD (212 417-4570)
Your call will remain confidential.
You can also complete a Complaint Form online at:
www.omig.state.ny.us

PROVIDER SERVICES
Return to Table of Contents
Missing Issues?
The Medicaid Update, indexed by subject area, can be accessed online at:
http://www.nyhealth.gov/health_care/medicaid/program/update/main.htm
Office of the Medicaid Inspector General: http://www.omig.state.ny.us (518) 473-3782
Questions about an Article?
Each article contains a contact number for further information, questions or comments.
Questions about billing and performing EMEVS transactions?
Please contact eMedNY Call Center at: (800) 343-9000.
Provider Training
To sign up for a provider seminar in your area, please enroll online at:
http://www.emedny.org/training/index.aspx
For individual training requests, call (800) 343-9000 or email: emednyproviderrelations@csc.com
Enrollee Eligibility
Call the Touchtone Telephone Verification System at any of the numbers below:
(800) 997-1111 (800) 225-3040 (800) 394-1234.
Address Change?
Questions should be directed to the eMedNY Call Center at: (800) 343-9000.
Fee-for-Service Providers
A change of address form is available at:
http://www.emedny.org/info/ProviderEnrollment/index.html
Rate-Based/Institutional Providers
A change of address form is available at:
http://www.emedny.org/info/ProviderEnrollment/index.html
Comments and Suggestions Regarding This Publication?
Please contact the editor, Kelli Kudlack, at:
medicaidupdate@health.state.ny.us
Medicaid Update is a monthly publication of the New York State Department of Health containing information regarding the care of those enrolled in the Medicaid Program.