May 2009 Volume 25, Number 6
New York State Medicaid Update
The official newsletter of the New York Medicaid Program
David A. Paterson, Governor
State of New York
Richard F. Daines, M.D. Commissioner
New York State Department of Health
Deborah Bachrach, Deputy Commissioner
Office of Health Insurance Programs
Dear Medicaid Provider,

Welcome to the May 2009 edition of the Medicaid Update. This month's issue features DME and Home Care policy and billing bulletins, pharmacy updates, and a notice to ambulance providers that effective July 1, 2009, they will be required to include procedure code modifiers on any submitted ambulance (category of service 0601) claim that contains certain procedure codes.
So that we may continue to keep you apprised of current Medicaid policy guidelines and bulletins, please notify us as soon as your contact information changes. Please send updated info to medicaidupdate@health.state.ny.us. It is the responsibility of each provider to alert Medicaid of any address or e-mail changes as soon as they occur. We thank you for your continued feedback.
In this issue....
POLICY AND BILLING GUIDANCE BULLETIN
DME Providers - Checking Beneficiary Eligibility? Look for Eligibility Response Exception Code NH
Home Care Providers - Billing Update
Providers Who Submit Batch Transactions
Ambulance Providers: Claim Modifiers Required Effective July 1, 2009
PHARMACY PROVIDERS
ALL PROVIDERS
Smoking Cessation Advertisement
Medicaid Provider Seminars
Provider Directory
Do you suspect that a Medicaid provider or an enrollee has engaged in fraudulent activities?
Return to Table of Contents
Call: 1-877-87FRAUD or (212 417-4570)
Your call will remain confidential.
You can also complete a Complaint Form online at:
www.omig.state.ny.us

PROVIDER MANUALS ARE AVAILABLE ONLINE
Your Provider Manual offers a wealth of information about Medicaid, as well as specific instructions on how to submit a claim for rendered services.
Provider Manuals can be accessed online at: http://www.emedny.org/ProviderManuals/index.html.
eMedNY also offers a FAQ section online at http://www.emedny.org/info/faq/index.html for providers seeking guidance on program requirements and updates.
NPI UPDATE: TO ENSURE PROMPT PROCESSING OF CLAIMS
PROVIDERS MUST USE NPI ON ALL BILLING TRANSACTIONS
Return to Table of Contents

On September 1, 2008, New York Medicaid implemented the National Provider Identifier (NPI) to process all submitted claims. We would like to thank all providers for their cooperation during this important transition process. The NPI implementation impacted all billing transactions (electronic and paper) submitted to New York Medicaid. Most providers have achieved compliance for claim submissions, however, this notice serves as an important reminder about compliance for the other types of transactions listed below:
- Claim Status Requests (Note: If a claim was submitted with only an NPI, the claim inquiry should be made with the submitted NPI. If both an NPI and MMIS ID were submitted on the claim then the claim inquiry must be made using the submitted MMIS ID);
- Eligibility Verifications including service authorizations and name search regardless of the method used, (touch-tone telephone, card-swipe terminals, batch, dial-up PC, CPU and ePACES);
- Prior Approval/Authorizations (PA) including dispensing validation system (DVS) and paper PA forms and PA change requests;
- Threshold Override Applications
- Provider Enrollment Applications and maintenance forms such as change of address forms;
- Electronic Request Forms such as Certifications for Billing, Electronic Remittance Requests, Electronic Funds Transfer Requests, etc.
We urge providers to fully examine their submissions for all transactions so that we may move to full NPI compliance. Failure to do so will result in future denials of these transactions.
We realize that some providers do not meet the HIPAA definition of a health care provider (i.e. personal care vendors, and non-emergency transportation providers) and will continue to submit their Medicaid IDs. Please contact the eMedNY Call Center at (800) 343-9000 with any questions regarding NPI compliance or visit http://www.eMedNY.org
Policy and Billing Guidance Bulletins
DME PROVIDERS - CHECKING BENEFICIARY ELIGIBILITY?
LOOK FOR ELIGIBILITY RESPONSE EXCEPTION CODE NH
Return to Table of Contents
Code NH identifies a beneficiary residing in a Nursing Home facility. The majority of the beneficiary's care, including durable medical equipment and supplies, is provided by the nursing home and is included in their Medicaid per diem rate. Only custom-made DME is reimbursed by fee-for-service Medicaid. Custom-made is defined as any durable medical equipment, orthopedic footwear, orthotics, or prosthetics fabricated solely for a particular Medicaid beneficiary from raw materials which cannot be readily changed to conform to another beneficiary's needs. These materials are used to create the item from patient measurements, tracing and patterns. Custom-made DME requires that the Medicaid beneficiary be measured and that the custom-made item be fabricated from these measurements. If you require additional information, please contact the Division of Provider Relations and Utilization Management at (800) 342-3005 (Option #1).
HOME CARE PROVIDERS - BILLING REQUIREMENTS UPDATE
Return to Table of Contents
The billing requirements set forth in the NYS Medicaid Provider Manuals for Home Health Services provided by Certified Home Health Agencies (CHHA), Long Term Home Health Care Programs (LTHHCP), and Private Duty Nursing (PDN) providers require that certain identifying information about ordering providers be submitted through paper and electronic billing submissions. CHHA and LTHHCP providers are subject to the instructions found on the UB-04 Form Locator Field #78. Instructions for PDN providers are found in Field #19C of the eMedNY paper forms #150001/150002. The electronic HIPAA compliant billing formats are subject to the same requirements as the paper claims. Provider Manuals are available online at http://www.eMedNY.org
Effective 90 days after the release of this Medicaid Update, a Billing Edit #00903 which will require completion of the ordering provider information fields on all home health care claims will be activated for the following categories of service (COS):

- 0260 (Home Health Agency Professional Services FS),
- 0284 (Hospital Services Home Care Program),
- 0386 (LTC HHA Prof. Services-NH Sponsored),
- 0388 (Long Term Home Health Care),
- 0521 (Nursing Service LPN),
- 0522 (Nursing Service RN),
- 0523 (Nursing Service Hospital Registry LPN), and
- 0524 (Nursing Service Hospital Registry RN).
Other COS codes may be added to this edit in the future. Once the edit is activated, any claim for service that does not include the required information in the relevant ordering provider field will be denied, and the billing provider must resubmit the required information to receive payment. The ordering provider should identify the practitioner who actually ordered the services being billed. Inaccurate information that is submitted to meet the edit requirements may result in future audit disallowances. Full compliance with this requirement will enable the State to verify the licensing of ordering practitioners and identify practitioners excluded or suspended from Medicare/Medicaid. Questions? Please call the eMedNY Call Center at (800) 343-9000.
PROVIDERS WHO SUBMIT BATCH TRANSACTIONS
Return to Table of Contents
Upon receipt of a batch transmission, eMedNY will return a series of response files to the submitter and communicate the status of the transactions. These files must be processed without delay so the submitter may identify any submission problems. Please visit the NYHIPAADESK FAQ section available on eMedNY at: http://www.emedny.org/hipaa/FAQs/index.html. There you will find a FAQ section entitled 'What Are the Response Files Sent by eMedNY." Questions regarding batch submissions and response files should be directed to the eMedNY Call Center at (800) 343-9000.
Policy and Billing Guidance
ATTENTION: AMBULANCE PROVIDERS
CLAIM MODIFIERS REQUIRED EFFECTIVE JULY 1, 2009
Return to Table of Contents
Effective July 1, 2009, all ambulance providers are required to include procedure code modifiers on submitted ambulance (category of service 0601) claims that include one of the following procedure codes:
| Procedure Code | Description |
|---|---|
| A0426 | Advanced Life Support, Non-emergency, Level 1 |
| A0427 | Advanced Life Support, Emergency, Level 1 |
| A0428 | Basic Life Support, Non-emergency (BLS) |
| A0429 | Basic Life Support, Emergency, (BLS Emergency) |
PLEASE NOTE: The modifier will not be required on the Prior Approval submitted for the service.
Claim submissions on and after July 1, 2009, will be rejected if the modifier is not included. Please follow the instructions below to ensure claims are submitted properly. Please see below for a listing of acceptable claim modifiers.
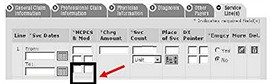
Claim Type - ePACES
INSTRUCTIONS: Enter the modifier in the modifier positions under the procedure code (HCPCS) entry.
New Claim - 837 Professional Real Time
Claim Type - Paper
Enter the modifier in the two digit space following the procedure code in Field 26.
Claim Type - Electronic 837 Professional
INSTRUCTIONS:
Enter the modifier in Loop 2400
Segment Name - Professional Services
Data Element - SV101-3
The 837 P CG is available at eMedNY.org for additional information.
Once effective, claims containing the procedure codes A0426, A0427, A0428, and A0429 that do not incorporate modifiers will be rejected. Similar to Medicare, for each base line item, the trip origin is reported by using a modifier in the first position and the destination is reported using a modifier in the second, as follows:
D = Diagnostic or therapeutic site other than P or H when these are used as origin codes
E = Residential, domiciliary, custodial facility (other than 1819 facility)
G = Hospital-based End-Stage Renal Disease (ESRD) facility
H = Hospital
I = Site of transfer (e.g. airport or helicopter pad) between modes of ambulance transport
J = Freestanding ESRD facility
N = Skilled nursing facility
P = Physician's office
R = Residence
S = Scene of accident or acute event
X = Intermediate stop at physician's office on way to hospital (destination code only)
R = Residence
S = Scene of accident or acute event
X = Intermediate stop at physician's office on way to hospital (destination code only).
CLAIM MODIFIERS REQUIRED EFFECTIVE JULY 1, 2009
Acceptable Ambulance Modifiers
Return to Table of Contents

| Origination/Destination | Modifier |
|---|---|
| DIAG THERA SITE NOT P OR H ORIG/RES,DOM,CUST FACIL | DE |
| DIAG THERA SITE NOT P OR H ORIG/HOSP BASE DIALYSIS | DG |
| DIAG THERA SITE NOT P OR H ORIG/HOSPITAL | DH |
| DIAG THERA SITE NOT P OR H ORIG/TRANS BETW AMB MOD | DI |
| DIAG THERA SITE NOT P OR H ORIG/NON-HOSP DIALYSIS | DJ |
| DIAG THERA SITE NOT P OR H ORIGIN CODES/SNF | DN |
| DIAG THERA SITE NOT P OR H ORIGIN CDS/PHYS OFFICE | DP |
| DIAG THERA SITE NOT P OR H ORIGIN CDS/RESIDENCE | DR |
| DIAG THERA SITE NOT P OR H ORIG/DEST INTERM STOP | DX |
| RES, DOM, CUST FAC (NOT 1819)/DIAG THERA NOT P OR H | ED |
| RES, DOM, CUST FAC (NOT 1819)/HOSP BASE DIALYSIS | EG |
| RES, DOM, CUST FACILTY(NOT 1819)/HOSPITAL | EH |
| RES, DOM, CUST FAC /SITE TRANS BETWEEN AMBUL MODES | EI |
| RES, DOM, CUST FAC (NOT 1819)/ NON-HOSP DIALYSIS | EJ |
| RES, DOM, CUST FAC (NOT 1819)/ SNF 1819 FACILITY | EN |
| RES, DOM, CUST FAC (NOT 1819)/ RESIDENCE | ER |
| RES, DOM, CUST FAC (NOT 1819)/DEST CD INTERM STOP | EX |
| HOSP DIALYSIS FAC/ORIG DIAG THER SITE NOT P OR H | GD |
| HOSP DIALYSIS FAC/RES, DOM, CUST FAC (NOT 1819) | GE |
| HOSP DIALYSIS FACILITY (HOSP RELATED)/ HOSPITAL | GH |
| HOSP DIALYSIS FAC/SITE OR TRANS BETW AMBUL MODES | GI |
| HOSP DIALYSIS FAC (HOSP RELATED)/SNF (1819 FAC) | GN |
| HOSP DIALYSIS FAC (HOSP RELATED)/PHYSICIANS OFFICE | GP |
| HOSP DIALYSIS FAC (HOSP REALTED)/RESIDENCE | GR |
| HOSP DIALYSIS FAC (HOSP RELATED)/DEST INTERM STOP | GX |
| HOSP/DIAG THERA SITE NOT P OR H USED AS ORIGIN CDS | HD |
| HOSP/RES, DOM, CUST FACILITY OTHER THAN 1819 FAC | HE |
| HOSPITAL/HOSP DIALYSIS FACILITY(HOSP OR HOSP RELAT) | HG |
| HOSPITAL/HOSPITAL | HH |
| HOSPITAL/SITE OF TRANS BETW MODES OF AMBUL TRANSP | HI |
| HOSPITAL/NON-HOSPITAL BASED DIALYSIS FACILITY | HJ |
| HOSPITAL/SKILLED NURSING FACILITY SNF (1819 FAC) | HN |
| NON-HOSP DIALYSIS FAC/RES, DOM, CUS FAC (NOT 1819) | JE |
| NON-HOSPITAL BASED DIALYSIS FACILITY/HOSPITAL | JH |
| NON-HOSP DIALYSIS FAC/SITE OF TRANS BETW MODES AMB | JI |
| HOSPITAL/PHYSICIAN'S OFFICE | HP |
| NON-HOSP BASED DIALYSIS FAC/SNF (1819 FACILITY) | JN |
| NON-HOSPITAL BASED DIALYSIS FACILITY/PHYSICIAN OFC | JP |
| NON-HOSPITAL BASED DIALYSIS FACILITY/RESIDENCE | JR |
| NON-HOSP DIALYSIS FAC/DEST CD INTERM STOP AT PHYS | JX |
| SNF (1819 FACILITY)/DIAG THERA ORIGIN(NOT P OR H) | ND |
| SNF (1819 FACILITY)/HOSP BASED DIALYSIS(HOSP RELAT | NG |
| SNF (1819 FACILITY)/HOSPITAL | NH |
| SNF (1819 FACILITY)/TRANS BETWEEN MODES OF AMBUL | NI |
| SNF (1819 FACILITY)/NON-HOSP BASED DIALYSIS FACIL | NJ |
| SNF (1819 FACILITY)/PHYSICIAN'S OFFICE | NP |
| SNF (1819 FACILITY)/RESIDENCE | NR |
| SNF (1819 FACILITY)/DEST CD INTERM STOP PHYS OFFIC | NX |
| PHYS OFFICE/DIAG THERA SITE ORIGIN CDS NOT P OR H | PD |
| PHYS OFFICE/RES, DOM, CUS FACILITY(NOT 1819 FACIL) | PE |
| PHYS OFFICE/HOSP BASED DIALYSIS FACILITY | PG |
| PHYSICIAN'S OFFICE/HOSPITAL | PH |
| PHYS OFC/SITE OF TRANS BETWE MODES OF AMBUL TRANSP | PI |
| PHYS OFFICE/NON-HOSPITAL BASED DIALYSIS FACILITY | PJ |
| PHYSICIAN'S OFFICE/SNF (1819 FACILITY) | PN |
| PHYSICIAN'S OFFICE/RESIDENCE | PR |
| RESIDENCE/DIAG THERA SITE ORIGIN CDS NOT P OR H | RD |
| RESIDENCE/HOSPITAL BASED DIALYSIS FACILITY | RG |
| RESIDENCE/HOSPITAL | RH |
| RESIDENCE/SITE OF TRANS BETWE MODES OF AMBUL TRANS | RI |
| RESIDENCE/NON-HOSPITAL BASED DIALYSIS FACILITY | RJ |
| RESIDENCE/SKILLED NURSINC FACILITY (SNF)(1819 FAC) | RN |
| RESIDENCE/DEST CD INTERM STOP AT PHYS OFF TO HOSP | RX |
| SCENE OF ACCIDENT ACUTE/DIAG THER ORIG NOT P OR H | SD |
| SCENE OF ACCIDENT ACUTE EVENT/HOSP BASED DIALYSIS | SG |
| SCENE OF ACCIDENT ACUTE EVENT/HOSPITAL | SH |
| SCENE OF ACCIDENT ACUTE/TRANS BETW MODES AMBUL TRA | SI |
| SCENE OF ACCIDENT OR ACUTE/NON-HOSP BASED DIALYSIS | SJ |
| SCENE OF ACCIDENT OR ACUTE EVENT/SNF (1819 FAC) | SN |
| SCENE OF ACCIDENT OR ACUTE EVENT/PHYSICIAN'S OFFIC | SP |
| DEST CD INTERM STOP AT PHYS OFC ON WAY TO HOSP | SX |
The instructions above appear on page 4 in the revised version of the Transportation Billing Guidelines Manual, located online at:
http://www.emedny.org/ProviderManuals/Transportation/index.html.
Billing questions? Please contact Computer Sciences Corporation at (800) 343-9000.
Policy questions? Please contact the Medicaid Transportation Unit at (518) 408-4825 or via e-mail at MedTrans@health.state.ny.us
Pharmacy Updates
PREFERRED DRUG PROGRAM UPDATE
Return to Table of Contents

The New York State Medicaid Pharmacy and Therapeutics (P&T) Committee recently expanded the Preferred Drug Program to include eight new drug classes. Prescriptions written on or after June 10, 2009, for non-preferred drugs in the following classes will require prior authorization:
- Antibiotics - Topical
- Antihistamines - Intranasal
- Anti-Virals - Topical
- Direct Renin Inhibitors
- Non-Ergot Dopamine Receptor Agonists
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDS) - Prescription
- Psoriasis Agents - Topical
- Skeletal Muscle Relaxants
To obtain prior authorization for non-preferred drugs, please contact the Call Center at (877) 309-9493 and follow the appropriate prompts. The most current Preferred Drug List (PDL), with a full listing of preferred and non-preferred drugs for each of the drug classes currently subject to the PDP is available for download at: https://newyork.fhsc.com/downloads/providers/NYRx_PDP_PDL.pdf
Additional information, such as a "Quick List" of only preferred drugs and updated prior authorization forms, is available at each of the following Websites: http://www.nyhealth.gov OR http://www.eMedNY.org OR https://newyork.fhsc.com
Remember: Preferred drugs do not require prior authorization!
For clinical concerns or preferred drug program questions, contact (877) 309-9493. For billing questions, contact (800) 343-9000. For Medicaid pharmacy policy and operations questions, contact (518) 486-3209.
All Providers
Don't Be Silent About Smoking
Return to Table of Contents
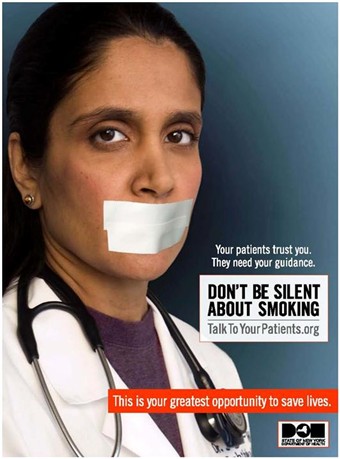
By providing counseling, pharmacotherapy, and referrals, you can double your patients' chances of successfully quitting. For more information, please visit www.talktoyourpatients.org or call the NY State Smokers' Quitline at 1-866-NY-QUITS (1-866-697-8487).

CSC offers Medicaid provider seminars
Return to Table of Contents
- Do you have billing questions?
- Are you new to Medicaid billing?
- Would you like to learn more about ePACES?
If you answered YES to any of these questions, you should consider registering for a Medicaid seminar. Computer Sciences Corporation (CSC) offers various types of seminars to providers and their billing staff. Many of the seminars planned for the upcoming months offer detailed information and instruction about Medicaid's Web-based billing and transaction program - ePACES.
ePACES is the electronic Provider Assisted Claim Entry System which allows enrolled providers to submit the following type of transactions:
- Claims
- Eligibility Verifications
- Utilization Threshold Service Authorizations
- Claim Status Requests
- Prior Approval Requests
Physicians, nurse practitioners and private duty nurses can even submit claims in "REAL-TIME" via ePACES. Real-time means that the claim is processed within seconds and professional providers can get the status of a real-time claim, including the paid amount without waiting for the remittance advice.
Fast and easy seminar registration, locations, and dates are available on the eMedNY Website at: http://www.emedny.org/training/index.aspx
Please review the seminar descriptions carefully to identify the seminar appropriate for your training requirements. Registration confirmation will instantly be sent to your e-mail address.
If you are unable to access the Internet to register, you may also request a list of seminars and registration information to be faxed to you through CSC-s Fax on Demand at (800) 370-5809.
Please request document 1002 for July - September seminar dates and 1003 for October - December seminar dates.
CSC Regional Representatives look forward to meeting with you at upcoming seminars!
Questions about registration? Please contact the eMedNY Call Center at (800) 343-9000.

Quick Reference Guide
Return to Table of Contents
Office of the Medicaid Inspector General: http://www.omig.state.ny.us (518) 473-3782
Questions about an Article?
Each article contains a contact number for further information, questions or comments.
Questions about billing and performing EMEVS transactions?
Please contact eMedNY Call Center at: (800) 343-9000.
Provider Training
To sign up for a provider seminar in your area, please enroll online at:
http://www.emedny.org/training/index.aspx
For individual training requests, call (800) 343-9000 or email: emednyproviderrelations@csc.com
Enrollee Eligibility
Call the Touchtone Telephone Verification System at any of the numbers below:
(800) 997-1111 (800) 225-3040 (800) 394-1234.
Address Change?
Questions should be directed to the eMedNY Call Center at: (800) 343-9000.
Fee-for-Service Providers
A change of address form is available at:
http://www.emedny.org/info/ProviderEnrollment/index.html
Rate-Based/Institutional Providers
A change of address form is available at:
http://www.emedny.org/info/ProviderEnrollment/index.html
Comments and Suggestions Regarding This Publication?
Please contact the editor, Kelli Kudlack, at:
medicaidupdate@health.state.ny.us
Medicaid Update is a monthly publication of the New York State Department of Health containing information regarding the care of those enrolled in the Medicaid Program.