August 2009 Volume 25, Number 10
New York State Medicaid Update
The official newsletter of the New York Medicaid Program
David A. Paterson, Governor
State of New York
Richard F. Daines, M.D. Commissioner
New York State Department of Health
Deborah Bachrach, Deputy Commissioner
Office of Health Insurance Programs
In this issue....
Policy and Billing Guidance
Enhanced Medicare Cost Sharing for Certain Clinics
APG Policy Updates
APG Episode Payment Policy
APG Ancillary Services Payment Policy for Laboratory Tests
APG Ancillary Services Payment Policy for Radiology Services
APG Laboratory/Radiology Ancillary Service Compliance and Enforcement
Verifone POS Terminal Update
Local DSS and CMCM/TCM Providers
Improper Recording of Hospital MMIS # on Prescriptions
Bridge and Tunnel Toll Change
Pharmacy Updates
Preferred Drug Program Update
Providers Must Include NDC on Claim Transactions When Billing for Drugs
Provider Services
Medicaid Training Courses Offered
Smoking Cessation Advertisement
Quick Reference Guide
New York Medicaid to Implement Medicare Crossover System
Return to Table of Contents
New York Medicaid is currently implementing a claims crossover system that will accept electronic claims directly from the Medicare Coordination of Benefits Contractor (COBC) for Medicare beneficiaries also covered by New York Medicaid. Once implemented, Medicaid will issue reimbursements for coinsurance, deductibles, psychiatric reductions, and copayments to providers. Most providers will no longer need to submit a separate claim to New York Medicaid. They will simply submit them to Medicare and the COBC will forward them to New York Medicaid for processing. Please note that claims submitted by pharmacies for payment of the Part B drug coinsurance and deductible are excluded from the crossover system.
If a provider submits claims to Medicare with an NPI that is not enrolled with Medicaid, the claim will be denied and returned to Group Health Inc., (GHI), the Medicare contractor COBC responsible for submitting crossover claims to Medicaid on behalf of Medicare providers.
Providers who bill Medicare using an NPI that is not enrolled with Medicaid, must contact the NYS Medicaid Enrollment Unit at (800) 342-3005. Providers that receive electronic remittances (835) must ensure that they have designated a default ETIN on their file. The default ETIN will be used for sending electronic remittances for crossover claims, as well as remittances for submitted paper claims. If a default ETIN is not designated, all crossover claims will be reported on a paper remittance.
To designate a default ETIN, please complete the Electronic Remittance Request form available at: http://tiny.cc/BVE4N.
To designate an existing ETIN as the default ETIN please check the box in line 4 on the form in addition to lines 1, 2, and if applicable, line 3. The Medicare crossover system implementation is scheduled for December 2009. Please visit http://www.emedny.org for further details.
Policy and Billing Guidance
Enhanced Medicare Cost Sharing for Certain Clinics
Return to Table of Contents

Effective July 1, 2009, any Diagnostic and Treatment Center (D&TC) providing services to a Medicare beneficiary that is also covered by Medicaid (dually eligible) and identified with a Recipient Exception (R/E) Code 95 is entitled to receive the higher of the patient responsibility (Medicare deductible coinsurance) or the difference between the Medicaid rate of reimbursement minus the Medicare reimbursement. (Recipient Exception Code 95 is assigned by the Office of Mental Retardation and Developmental Disabilities to recipients who are developmentally disabled).
DOH Peer Group 41 providers that formerly received this enhanced cost sharing reimbursement for all dually eligible persons will now receive the enhanced payment only for those who are assigned R/E Code 95.
D&TC clinic providers can identify those individuals who have been assigned a R/E Code 95 through the usual Medicaid eligibility verification process.
Enhanced Medicare cost sharing for persons with R/E Code 95 is available for services billed under the following rate codes (visit based/episode based):
- 1407/1422 (Free-standing general clinic)
- 1428/1459 (Dental school)
- 1435/ 1425 (Mental Retardation/Developmentally Disabled/Traumatic Brain Injury (TBI) patient in freestanding general clinic) - Persons with TBI will not have R/E Code 95 on file and therefore will not be eligible for this enhanced cost-sharing.
Enhanced Medicare cost sharing does not apply to the following rate codes:
- 1400/1432 (Hospital outpatient department)
- 1401 (Hospital ambulatory surgery)
- 1402 (Emergency department)
- 1408 (Free-standing ambulatory surgery center)
- 1438/1456 (Free-standing renal clinic)
- 1444/1450 (School-based health clinic affiliated with hospital)
- 1447/1453 (School-based health clinic affiliated with diagnostic and treatment center)
The following clinics are also eligible for the higher of the patient responsibility (Medicare deductible coinsurance) or the difference between the Medicaid rate of reimbursement minus the Medicare reimbursement for services provided to all dually eligible recipients:
- Article 16 clinics;
- Clinics licensed by OMH that receive Comprehensive Medicaid Outpatient Programs (COPS) reimbursement; and,
- Federally Qualified Health Centers
Billing questions should be directed to the eMedNY Call Center at (800) 343-3000.
Policy questions should be directed to the Division of Financial Planning and Policy at (518) 473-2160.
Policy and Billing Guidance

APG Policy Updates
Update on APG Episode Payment Policy
Return to Table of Contents
Effective July 1, 2009, most ancillary laboratory or radiology services associated with a medical visit and/or a significant procedure billed under the APG payment methodology are the fiscal responsibility of the APG provider and must be included on the APG claim, even if the ancillary service is provided by an outside vendor or on a different date of service from the medical visit or significant procedure visit that generated the ancillary service.1
Consistent with this change, new rate codes have been issued by eMedNY to hospital OPDs (and will be issued to DT&C clinics upon APG implementation) which will enable the APG Grouper/ Pricer to recognize an episode of care as the basic unit of payment. With the episode of care as the basic unit of payment, the APG biller will not reassign the actual date of service for the ancillary lab or radiology service to correlate with the date of the medical visit or significant procedure that generated the ancillary service. An episode of care is defined as a medical visit and/or significant procedure that occurred on a single date of service and all the associated ancillary laboratory or radiology services, regardless of the provider or the dates of the ancillary services. The episode payment rate codes permit APG billers to include the actual dates of service at the line level for each lab and radiology ancillary service provided as part of the episode of care.
When using episode payment rate codes, APG billers must report the "from" and "to" date in the claim header to reflect the time span for the episode of care and the actual date of service for each service provided at the line level. All procedure codes associated with a medical or significant procedure visit should be reported on a single claim. If procedures from two different episodes of care are coded on the same claim unwarranted discounting or consolidation may occur resulting in underpayment to the APG biller.
Effective January 1, 2010, hospital OPDs and D&TCs clinic providers will be required to use episode of care rate codes. In the interim, APG billers may use either the appropriate visit based rate codes (1400 for OPD; 1407 for DT&C; 1435 for D&TC- MR/DD/TBI) or the appropriate new episode of care rate codes (1432 for OPD; 1422 for D&TC; 1425 for D&TC-MR/DD/TBI), but not both for the same visit. Visit based rated codes will be end-dated December 31, 2009, for all hospital OPDs and D&TC clinic providers. An episode rate code (1402) is already in effect for hospital emergency departments. New episode rate codes will not be issued for hospital-based or free-standing ambulatory surgery claims.
Between July 1, 2009, and August 31, 2009, if an episode claim (1432 rate code) has a time span in the header that overlaps with that of another episode claim for the same patient, the second claim will be denied and no payment will be made by eMedNY. An edit to correct this problem will be implemented by September 1, 2009.
This edit will result in use of only the "from" date in the header to identify duplicate claims. Any 1432 claims inappropriately denied as duplicate claims from July 1, 2009, through August 31, 2009, may be resubmitted by a hospital after September 1, 2009, once the new edit is in place. Similarly, if a claim with a 1400 rate code is improperly denied as a duplicate claim because of the dates used in the header of the claim, hospitals may also rebill these claims after September 1, 2009, once the new edit is in place.
Questions may be directed to the Division of Financial Planning and Policy at (518) 473-2160 or via e-mail at: apg@health.state.ny.us.
1Exceptions to the APG billing policy for ancillary laboratory and radiology services provided on behalf of clinic patients are identified at the end of Section 4.3 (p. 25) of the APG Provider Manual available at: http://www.health.state.ny.us/health_care/medicaid/rates/apg/docs/apg_provider_manual.
Policy and Billing Guidance

APG Ancillary Services Reimbursement Policy for Laboratory Tests
Return to Table of Contents
Under the APG reimbursement methodology, payment for laboratory services ordered by practitioners in Article 28 hospital-based clinics, diagnostic and treatment centers (D&TCs), and emergency departments is made to the Article 28 facility. When the patient receives laboratory tests from a laboratory other than one located on-site at the Article 28 facility, the facility is responsible for reimbursing the laboratory, even in the absence of a contractual relationship between the two parties. Unless specifically carved out of APGs,2 the laboratory may not directly bill Medicaid for laboratory tests related to an APG-reimbursed visit. It must bill the ordering facility.
Article 28 facilities are responsible for:
- notifying the ancillary lab provider that the ordered test (other than those specifically carved out of APGs) is part of a visit that is subject to APG reimbursement;
- instructing the ancillary lab provider that the ordering hospital facility should be billed for the ancillary service, and;
- reimbursing the ancillary lab provider for all ancillary procedures that were ordered as part of the hospital clinic/emergency room visit and provided to the patient.
Medicaid recommends that laboratories revise their requisition forms so that facility-based practitioners can advise the laboratory that the ordered tests/procedures are part of an Article 28 hospital outpatient clinic, D&TC or emergency department visit subject to APG reimbursement. Below is suggested wording for such notification:
Important: Check box if applicable:
[ ] Laboratory tests subject to APG reimbursement. These lab tests were provided as part of an APG visit and are billable to Medicaid only by the ordering facility. The laboratory provider is required to bill the ordering facility for these ancillary services and may not bill Medicaid directly. The facility is responsible for reimbursing the laboratory provider for the services provided for these patients.
Important: Check box if applicable
[ ] Laboratory tests not subject to APG reimbursement. The laboratory may bill these tests to Medicaid using the laboratory fee schedule.
Questions regarding the APG payment policy may be directed to the Division of Financial Planning and Policy at (518) 473-2160 or via e-mail at: apg@health.state.ny.us.
2 Exceptions to the APG billing policy for ancillary laboratory and radiology services provided on behalf of clinic patients are identified at the end of Section 4.3 (p. 25) of the APG Provider Manual available at http://www.health.state,ny.us/health_care/medicaid/rates/apg/docs/apg_provider_manual.
Policy and Billing Guidance

APG Ancillary Services Reimbursement Policy For Radiology Services
Return to Table of Contents
Under the APG payment methodology, the technical component of a radiology service ancillary to a hospital outpatient or emergency department or free-standing clinic visit is included in the APG payment to the hospital or clinic. The professional component of the radiology service is not included in the APG payment to the hospital or clinic; therefore, the radiologist reading the film may bill Medicaid directly, for professional services using the Medicaid fee schedule.
The Article 28 clinic is responsible for informing the radiology service provider that the technical component of a radiology service ordered for a clinic patient is ancillary to an APG visit and, therefore, should be billed to the clinic. Medicaid recommends that the clinic develop a cover form to accompany the radiology order that identifies the radiology service as an APG ancillary service and instructs the radiology vendor to bill the referring clinic for the technical component of the service.
Medicaid recommends that radiology departments revise their order forms so that facility-based practitioners can advise the clinic ordered tests/procedures that are part of a hospital clinic/emergency department visit and are subject to APG reimbursement. Below is suggested wording for such notification:
Important: Check box if applicable:
[ ] Radiology service is ancillary to a clinic visit subject to APG reimbursement. The radiology provider should bill the referring clinic for the technical component of the service. The radiology provider should bill the professional component of the service directly to eMedNY using the Medicaid fee schedule.
Questions regarding the APG payment policy may be directed to the Division of Financial Planning and Policy at (518) 473-2160 or via e-mail at: apg@health.state.ny.us.
Policy and Billing Guidance

APG Laboratory/Radiology Ancillary Service Compliance and Enforcement
Return to Table of Contents
The APG ancillary reimbursement policy changes the way Article 28 facilities, laboratories, and radiology providers do business with one another.
To assist providers in transitioning to the new billing system, the Office of Health Insurance Programs will produce reports that identify laboratory and radiology claims billed by ancillary service providers to Medicaid for patients for whom an APG Article 28 hospital outpatient/emergency department claim has also been reimbursed. Reports of duplicate claims for dates of service within the period July 1, 2009 through December 31, 2009 will be sent to both Article 28 hospital clinics and ancillary services providers starting at the end of November.
Article 28 hospital facilities and ancillary service providers are required to reconcile their billings to ensure that all APG related laboratory/radiology services have been appropriately reported on the facility APG claim. If an ancillary service provider finds that it has billed Medicaid for services that had been ordered by the Article 28 hospital outpatient department, diagnostic and treatment center, or emergency department and which are subject to APG reimbursement, it must void its Medicaid claim and re-bill the ordering facility. The Office of the Medicaid Inspector General (OMIG) will be informed if duplicative payment has occurred and has not been reconciled.
Once the APG payment methodology is implemented in Diagnostic and Treatment Centers, a similar process will be put in place for these facilities. Questions regarding APG reimbursement should be directed to the Division of Financial Planning and Policy at (518) 473-2160 or via e-mail at apg@health.state.ny.us.
Verifone POS Terminal May Not Function With Digital Telephone Service
If you are currently using a VeriFone POS Terminal (Omni 3750 or VX570 Point of Service (POS) device) to verify client eligibility or to request service authorizations, and are considering changing your telephone service, please be advised that the POS terminal may not function on a digital telephone line, such as an internet-based telephone service that uses Voiceover IP. The VeriFone POS Terminals will only support analog signals. (This only applies to an Omni 3750 or VX570 POS terminals purchased through CSC.)
Providers are responsible for verifying that their telephone service will support their VeriFone POS terminal. Please verify with your telephone provider prior to changing telephone services that your VeriFone will work on their service. Providers who are not mandated by DOH to use POS terminals may use ePACES to check eligibility or perform other transactions supported by the terminal. If you are interested in ordering a new VeriFone POS Terminal or enrolling in ePACES, please visit: http://www.emedny.org/selfhelp/pos/faq.html or http://www.emedny.org/selfhelp/epaces/faq.html. Please contact the eMedNY Call Center at (800) 343-9000 with any questions regarding the VeriFone POS Terminal or ePACES.
Local Social Service Districts and Providers of Comprehensive Medicaid Case Management (CMCM)/Targeted Case Management (TCM)
All Medicaid beneficiaries enrolled in a Comprehensive Medicaid Case Management (CMCM)/Targeted Case Management (TCM) program must be coded in WMS with a recipient/exception (R/E) Code 35. This code links the beneficiary with a specific CMCM/TCM provider and enables the provider to be reimbursed for case management services. The use of (R/E) Code 35 prevents Medicaid beneficiaries from being enrolled in more than one CMCM/TCM program at a time. System changes were made effective July 1, 2009, and resulted in strict implementation of the (R/E 35) edit. All local social service districts, OMRDD, OMH, and providers of CMCM/TCM must ensure proper enrollment of beneficiaries in CMCM/TCM programs with the (R/E) Code 35 in order to be reimbursed for CMCM/TCM services. For more details please refer to 18 NYCRR Section 505.16 and 89 ADM 29.
Improper Recording of Hospital MMIS # on Prescriptions
The Office of the Medicaid Inspector General (OMIG) recently identified that some unenrolled residents and hospital based physicians are improperly recording the hospital's MMIS number on prescriptions. When these prescriptions are processed for reimbursement, pharmacies are incorrectly recording the hospital's MMIS number as a physician's New York State license number. It is imperative that providers comply with the following directives which have been outlined in previous Medicaid Updates:
- (Medicaid Update - December 2003) - All prescriptions and fiscal orders written for Medicaid beneficiaries must bear the name, address, telephone number, profession, license number, or MMIS provider number, DEA number if applicable, and signature of the prescriber. In addition to the signature, the prescription or fiscal order must be imprinted or stamped legibly and conspicuously with the printed name of the prescriber who signed the prescription or fiscal order.
- (Medicaid Update - March 2004) - Prescribers must provide their NYS license number or MMIS provider numbers on all prescriptions written for Medicaid beneficiaries. When a prescription is written by an unlicensed intern or resident the supervising physician's MMIS number or State license number must be provided.
- (Medicaid Update - March 2004) - A facility MMIS number cannot be used to process pharmacy claims under Medicaid. If the prescriber's license number is not provided, pharmacists must contact the prescriber to obtain their license number or MMIS number, and to verify prescriber's identity.
Policy and Billing Guidance
Bridge and Tunnel Toll Change
Return to Table of Contents
The tolls charged by the New York City Metropolitan Transit Authority (MTA) to cross the bridges and tunnels that connect New York City were changed effective July 12, 2009. The new toll amounts for MTA-operated bridges and tunnels are reflected in the table below:
| Crossing | Toll Amount |
|---|---|
| Verrazano Narrows Bridge | $9.14 |
| Bronx-Whitestone Bridge, Brooklyn-Battery Tunnel, Queens Midtown Tunnel, Throgs Neck Bridge, and Triborough Bridge | $4.57 |
| Henry Hudson Bridge | $2.09 |
| Marine Markway-Gil Hodges Memorial Bridge, Cross Bay Veterans Memorial Bridge | $1.71 |
For dates of service on or after July 12, 2009, procedure codes NY117 (ambulette) and NY227 (livery) allow a maximum reimbursement of $9.14 per unit. However, providers should bill only the amount of the toll incurred.
Providers may seek Medicaid reimbursement for the appropriate E-Z Pass toll amount (as indicated in the table above) only if a toll was incurred while transporting a Medicaid enrollee in the vehicle across a bridge or tunnel. Only the E-Z Pass charge should be claimed.
If a vehicle is transporting more than one rider on the same trip, the provider may bill one unit per round trip crossing, not one unit per passenger.
Providers can enroll in the E-Z Pass program by calling (800) 333-TOLL, or online at: http://www.e-zpassny.com.
Questions? Please contact the Transportation Policy Unit at (518) 408-4825 or via e-mail to MedTrans@health.state.ny.us.
For billing questions, please call the eMedNY Call Center at (800) 343-9000.
Pharmacy Update
Preferred Drug Program Update
Return to Table of Contents

The New York State Medicaid Pharmacy and Therapeutics (P&T) Committee recently conducted a review of 21 drug classes subject to the Preferred Drug Program (PDP).
Effective August 19, 2009, prior authorization requirements changed for some drugs in the following four drug classes:
- Angiotensin Converting Enzyme Inhibitors (ACEIs)
- Bisphosphonates - Oral
- Corticosteroids - Inhaled
- Triglyceride Lowering Agents
To obtain prior authorization for non-preferred drugs, please contact the Call Center at (877) 309-9493 and follow the appropriate prompts. You will find the most current Preferred Drug List (PDL), with a full listing of preferred and non-preferred drugs for each of the drug classes currently subject to the PDP at:
https://newyork.fhsc.com/downloads/providers/NYRx_PDP_PDL.pdf
Additional information, such as a "Quick List" of only preferred drugs and updated prior authorization forms, is available at each of the following Websites:
http://www.nyhealth.gov or http://www.eMedNY.org or https://newyork.fhsc.com.
Preferred drugs do not require prior authorization (unless otherwise indicated on the PDL).
For clinical concerns or preferred drug program questions, contact (877) 309-9493. For billing questions, contact (800) 343-9000. For Medicaid pharmacy policy and operations questions, call (518) 486 -3209.
Pharmacy Update
Providers Must Include National Drug Code (NDC) on Medicaid Claim Transactions When Billing for Drugs
Return to Table of Contents
IMPORTANT NOTICE FOR PHYSICIANS, NURSE PRACTITIONERS, LICENSED MIDWIVES, AND ORDERED AMBULATORY PROVIDERS:
New York State Medicaid implemented the National Drug Code (NDC) billing requirements for billing physician administered drugs (J-codes) effective January 29, 2009. The NDC requirements apply to paper and electronic claims. The Department and its fiscal agent, Computer Sciences Corporation (CSC), have been percentage continue to submit claims without the NDC, NDC Unit of Measure, NDC Quantity, as well as J-code information.
REMINDER: Please make sure that claims for physician administered drugs include NDC monitoring the use of NDC on claims, and while information when billing. Failure to do so will result most providers are in compliance, a significant in claim denial.
Effective September 10, 2009, the Department will deny claims for physician administered drugs that do not include the appropriate NDC, NDC Unit of Measure, and NDC Quantity, except for drugs purchased through the 340B program and other products that are not deemed rebate eligible such as vaccines. Remember, the NDC found on the label of the drug administered must be the NDC submitted on the claim. Existing physician administered drug reporting requirements (using the Healthcare Common Procedure coding System- HCPCS) remain the same. Payment will continue to be based on HCPCS reporting information.
For additional information on billing physician administered drugs, please review the December 2008 Medicaid Update article or visit http://www.emedny.org to view the online Physician Manual150002 Billing Guidelines.
Please contact the eMedNY Call Center at (800) 343-9000 with any questions regarding this billing requirement.
Provider Services
Medicaid Training Seminars Offered
Return to Table of Contents
- Do you have billing questions?
- Are you new to Medicaid billing?
- Would you like to learn more about ePACES?
If you answered YES to any of these questions, you should consider registering for a Medicaid seminar. Computer Sciences Corporation (CSC) offers various types of seminars to providers and their billing staff. Many of the seminars planned for the upcoming months offer detailed information and instruction about Medicaid's Web-based billing and transaction program - ePACES.
ePACES is the electronic Provider Assisted Claim Entry System which allows enrolled providers to submit the following type of transactions:
- Claims
- Eligibility Verifications
- Utilization Threshold Service Authorizations
- Claim Status Requests
- Prior Approval Requests
Physicians, nurse practitioners and private duty nurses can even submit claims in "REAL-TIME" via ePACES. Real-time means that the claim is processed within seconds and professional providers can get the status of a real-time claim, including the paid amount without waiting for the remittance advice.
Fast and easy seminar registration, locations, and dates are available on the eMedNY Website at: http://www.emedny.org/training/index.aspx
Please review the seminar descriptions carefully to identify the seminar appropriate for your training requirements. Registration confirmation will instantly be sent to your e-mail address.
If you are unable to access the Internet to register, you may also request a list of seminars and registration information to be faxed to you through CSC-s Fax on Demand at (800) 370-5809.
Please note: Seminar schedule information is posted quarterly in CSC's Fax on Demand and Website at the beginning of each quarter. Please continue to check for updated information.
CSC Regional Representatives look forward to meeting with you at upcoming seminars!
Questions about registration? Please contact the eMedNY Call Center at (800) 343-9000.
Your Patients Are Listening
Return to Table of Contents
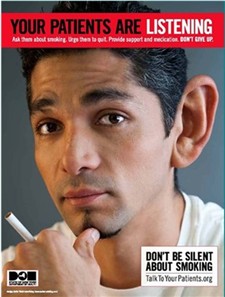
By providing counseling, pharmacotherapy, and referrals, you can double your patients' chances of successfully quitting. For more information, please visit www.talktoyourpatients.org or call the NY State Smokers' Quitline at 1-866-NY-QUITS (1-866-697-8487).
Do you suspect that a Medicaid provider or an enrollee has engaged in fraudulent activities?
Return to Table of Contents
Call: 1-877-87FRAUD or (212 417-4570)
Your call will remain confidential.
You can also complete a Complaint Form online at:
www.omig.state.ny.us

Quick Reference Guide
Return to Table of Contents
Office of the Medicaid Inspector General:
http://www.omig.state.ny.us or call (518) 473-3782 with general
inquiries or 1-877-87FRAUD with suspected fraud complaints or allegations.
Questions about billing and performing EMEVS transactions?
Please contact eMedNY Call Center at: (800) 343-9000.
Provider Training
To sign up for a provider seminar in your area, please enroll online at:
http://www.emedny.org/training/index.aspx
For individual training requests, call (800) 343-9000 or email: emednyproviderrelations@csc.com
Enrollee Eligibility
Call the Touchtone Telephone Verification System at any of the numbers below:
(800) 997-1111 (800) 225-3040 (800) 394-1234.
Address Change?
Questions should be directed to the eMedNY Call Center at: (800) 343-9000.
Fee-for-Service Providers
A change of address form is available at:
http://www.emedny.org/info/ProviderEnrollment/index.html
Rate-Based/Institutional Providers
A change of address form is available at:
http://www.emedny.org/info/ProviderEnrollment/index.html
Comments and Suggestions Regarding This Publication?
Please contact the editor, Kelli Kudlack, at:
medicaidupdate@health.state.ny.us
Medicaid Update is a monthly publication of the New York State Department of Health containing information regarding the care of those enrolled in the Medicaid Program.