November 2010 Volume 26, Number 13
New York State Medicaid Update
The official newsletter of the New York Medicaid Program
David A. Paterson, Governor
State of New York
Richard F. Daines, M.D. Commissioner
New York State DOH
Donna J. Frescatore, Medicaid Director & Deputy Commissioner
Office of Health Insurance Programs

In this issue....
POLICY AND BILLING GUIDANCE
ADDITIONAL INFORMATION/REMINDER:
PRESCRIBER'S INDIVIDUAL NATIONAL PROVIDER IDENTIFIER
(NPI) REQUIRED ON ALL PHARMACY CLAIM SUBMISSIONS
ANESTHESIA CODING CHANGES TO BEGIN 11/18/10
ANESTHESIA SUPERVISION BILLING AND PAYMENT UPDATE
MEDICAID PAYMENT TO LABORATORIES FOR HEPATITIS C VIRUS QUANTITATIVE PCR TESTS
PHARMACY UDATES
17 ALPHA-HYDROXYPROGESTERONE CAPROATE (17P) FOR PREVENTION OF PRETERM DELIVERY
ALL PROVIDERS
ARE YOUR UNINSURED PATIENTS ELIGIBLE FOR THE NEW YORK BRIDGE PLAN?
IMPORTANT INFORMATION REGARDING ENROLLMENT AND MAINTENANCE FORMS
SMOKING CESSATION ADVERTISEMENT
PROVIDER DIRECTORY
Additional Information/Reminder:
Prescriber's Individual National Provider Identifier
(NPI) Required on All Pharmacy Claim Submissions
Return to Table of Contents
Attention Prescribers and Pharmacists:
Since September 1, 2008, New York Medicaid has required the submission of the prescriber's individual National Provider Identifier (NPI) on each pharmacy claim. This includes unlicensed residents, interns, and foreign physicians in training programs, even though they do not always meet the HIPAA definition of health care provider.
New York Medicaid will soon implement claims editing to enforce the submission of the prescriber's individual NPI on pharmacy claims. Once claims editing is implemented, pharmacy claims submitted with a prescriber's MMIS Provider ID number or profession code and license number will be denied for edit 02029 - "Missing Prescribing NPI".
Pharmacists: All pharmacy claims should include the prescriber's NPI in the Prescriber ID field (NCPDP field 411-DB) and a "01" in the Prescriber ID Qualifier field (NCPDP field 466-EZ).
Prescribers: New York State does not currently require that the NPI be printed on your official prescription forms. However, as noted above, the Prescriber's NPI is required for claim submissions from pharmacies to New York Medicaid. Providing your NPI on the official prescription forms, as well as in electronic prescriptions, will ensure that the dispensing pharmacy can efficiently meet claims submission requirements. You may include your NPI on prescription pads by one of the following methods.
Your NPI may already be imprinted on your prescription forms if you provided it to the New York State Official Prescription Program. If you have not yet provided your NPI, you may do so by sending an e-mail to narcotic@health.state.ny.us. Please include your name, state license number, and your individual NPI in the e-mail (organization NPI's will not be printed).
You may write or stamp your NPI number on the official prescription.
To apply for a NPI #, please contact the NPI registry at (800) 465-3203 or visit: https://nppes.cms.hhs.gov/NPPES/StaticForward.do?forward=static.npistart.
For questions relating to the New York State Official Prescription Program, please call (866) 811-7957, option 1. For pharmacy billing questions, please call (800) 343-9000.
ANESTHESIA CODING CHANGES TO BEGIN 11/18/10
Return to Table of Contents
New York Medicaid is pleased to announce the adoption of CPT-4 Anesthesia administration procedure codes. These codes, with a lead "zero", must be reported for anesthesia administration services beginning with dates of service on and after November 18, 2010. New Anesthesia Services Procedure Code and Fee Schedule sections within the Physician Provider Manual are available on the eMedNY Web site at: http://www.emedny.org/ProviderManuals/Physician/index.html.
Billing Instructions:
- Anesthesiologists must be enrolled with a specialty of 020 on their Enrollment file.
- Anesthesiologists were sent an initial order of the new version of the eMedNY 150003 paper claim form which accommodates billing in minutes. In the 'Days or Units' field, field 24I, please indicate maximum minutes total only.
- For electronic claims, Loop 2400 must be completed with either: the MJ (minutes) qualifier and units reported as minutes, or with the UN (units) qualifier and units reported as 15 minute units.
- For ePACES billing, ePACES users must use minutes on the Service Count option. This field will validate that the procedure code does have a leading 0 in order for minutes to be selected as an option by the ePACES user. No base units should be added by the provider as eMedNY will now add those during claims processing. Units will be left on the dropdown list for billing dates of service prior to 11/18/2010.
- Anesthesia Basic Value will be automatically calculated during processing: do not add basic value to maximum minutes total on the claim.
- Modifiers -47 and -AA are no longer payable when billing for dates of service on and after November 18, 2010. They are required for billing dates of service prior to November 18, 2010.
Please note: Providers who use a computer program to print information on paper claim forms will need to adjust the printing as the units field 24l has been expanded and the charges fields (24J, 24K and 24L) have been reduced in size.
For billing questions, please call the eMedNY Call Center at (800) 343-9000.
ANESTHESIA SUPERVISION BILLING AND
PAYMENT UPDATE
Return to Table of Contents
Effective January 1, 2011, New York Medicaid will provide reimbursement to teaching anesthesiologists, when
they are involved in concurrent procedures involving residents, Certified Registered Nurse Anesthetists (CRNAs)
or a combination of both. The teaching anesthesiologist will be reimbursed a percentage of the regular Medicaid
fee schedule rate, based on how many cases are being performed concurrently and whether a medical resident
or CRNA is involved in furnishing the services. This change in policy will require the addition of three new
modifiers, GC, QK and AD, which will determine payment.
Note: This change applies to all supervising/teaching anesthesiologists, whether employed by the hospital or a
private anesthesia group.
Presently, Medicaid reimburses teaching anesthesiologists when they are involved in a single procedure with a resident (100% of the amount paid for the service, when performed by the physician alone). Reimbursement is not provided for concurrent supervision of more than one resident. Likewise, Medicaid does not recognize CRNAs or reimburse anesthesiologists for supervision of CRNAs.
Medicaid is revising its policy to allow payment at the regular Medicaid fee schedule rate, if the teaching anesthesiologist is involved in the training of a resident in a single anesthesia case, two concurrent anesthesia cases involving residents, or a single case involving a resident that is concurrent to another case paid under the medical direction rules. This change will require the addition of the "GC" modifier (this service has been performed in part by a resident under the direction of a teaching physician). The "GC" modifier will apply to the single resident case or to each of the two concurrent resident cases.
Medicare's "teaching rules" would be applicable in these instances. They require that the teaching anesthesiologist be present during all critical or key portions of the anesthesia service or procedure, and that the teaching anesthesiologist (or another anesthesiologist with whom the teaching anesthesiologist has entered into an arrangement) is immediately available to furnish services during the entire procedure. The documentation in the patients' medical records must indicate the teaching physician's presence during all critical or key portions of the anesthesia procedure(s) and the immediate availability of another teaching anesthesiologist as necessary.
Medicaid policy is also being revised to allow teaching anesthesiologists to bill for medical direction of up to four concurrent procedures/cases involving qualified individuals, all of whom could be resident physicians, CRNAs or a combination of these individuals. This would involve the use of the "QK" modifier (medical direction of two, three or four concurrent anesthesia procedures involving qualified individuals). In such cases, a reduced rate of 50% would be applied (by the eMedNY claims processing system) to the Basic Value Units assigned to the specific anesthesia code (Note: Anesthesia Basic Value will be automatically calculated during processing and added to the maximum minutes reported on the claim.)
EXAMPLES INCLUDE:
- If the teaching anesthesiologist is involved in two mixed concurrent cases, that is, a single resident case concurrent to another case that does not involve a resident (but that involves a CRNA), reimbursement for the resident case will be paid at 100% (teaching rules - "GC " modifier). The case involving the CRNA ("QK" modifier) will be paid under the medical direction rules at 50% of the base value for that anesthesia service (plus time).
- If the teaching anesthesiologist is involved in two concurrent cases involving CRNAs, the "QK" modifier would be applied. Reimbursement to the teaching anesthesiologist would be at the medical direction rate of 50%.
- If the teaching anesthesiologist is involved in three or four cases involving residents, CRNAs or a combination of these individuals, all cases would be paid at the medical direction ("QK") rate of 50%.
- If the teaching anesthesiologist is involved in more than two cases, ALL involving residents, reimbursement would be 50% of the regular fee schedule rate for ALL cases. The provision to pay teaching anesthesiologists 100% is strictly limited to supervision of a maximum of two resident cases.
Teaching anesthesiologists involved in furnishing more than four procedures concurrently or performing other services while directing concurrent procedures, will be paid at the "medical supervision" rate of three base units and 1 time unit (60 minutes, total) per procedure. Such cases would be appended with the "AD" modifier (medical supervision by a physician: more than four concurrent anesthesia procedures).
A physician, who is concurrently directing the administration of anesthesia to up to four surgical patients, cannot ordinarily be involved in rendering additional services to other patients. However, there may be situations that do not substantially diminish the scope of control exercised by the anesthesiologist in directing the administration of anesthesia to the surgical patients. Examples include addressing an emergency of short duration in the immediate surgical area or administering an epidural or caudal anesthetic to ease labor pain, or periodic (rather than continuous) monitoring of an obstetrical patient. This does not constitute a separate service for the purpose of determining whether the medical direction criteria are met. It is expected that the medically-directing anesthesiologist is aware of the nature and type of services he or she is medically directing, and is personally responsible for determining whether his supervisory capacity would be diminished if he or she became involved in the performance of a another procedure of short duration for both cases. Note: As a reminder, these claims should continue to be billed on the eMedNY 150003 claim form or in the electronic 837P format.
THE DEFINITIONS/REQUIREMENTS OF "TEACHING RULES," "MEDICAL DIRECTION" AND "MEDICAL SUPERVISION" ARE AS FOLLOWS:
"Teaching rules" require that the teaching anesthesiologist be present for all critical or key portions of the case.
"Medical direction" requires that the following seven conditions be met. The physician must perform the following activities:
- Perform a pre-anesthesia examination and evaluation;
- Prescribe the anesthesia plan;
- Personally participate in the most demanding procedures of the anesthesia plan, including induction and emergence;
- Ensure that any procedures in the anesthesia plan that he or she does not perform are performed by a qualified anesthetist;
- Monitor the course of anesthesia administration at frequent intervals;
- Remain physically present and available for immediate diagnosis and treatment of emergencies; and
- Provide indicated post-anesthesia care.
"Medical supervision" is the term for medical direction of more than four concurrent anesthesia cases. It may also be used to bill for cases that start out as "medically directed," but in which the anesthesiologist becomes involved in other activities and is, therefore, unable to fulfill all seven requirements of medical direction.
Questions? Please call the eMedNY Call Center at (800) 343-9000.
MEDICAID PAYMENT TO LABORATORIES FOR HEPATITIS C
VIRUS QUANTITATIVE PCR TESTS
Return to Table of Contents
The American Association for the Study of Liver Disease's (AASLD) practice guidelines "Diagnosis, Management and Treatment of Hepatitis C: An Update" recommends HCV quantitative PCR testing be performed periodically throughout the course of treatment.
Please see: http://www.aasld.org/practiceguidelines/Pages/GuidelinesDevelopment.aspx.
Measuring the rate of viral clearance through the use of HCV quantitative PCR testing is essential in predicting the likelihood of a response to therapy, for determining the optimal duration of therapy, and as a stopping rule for patients with chronic hepatitis C. Measuring the viral load at specific points throughout the course of treatment is standard-of-care and has the benefit of limiting the exposure to HCV anti-viral therapy, thus potentially leading to reduced toxicity and a cost savings.
Recommendations indicate testing should occur at the following times during the course of HCV anti-viral therapy:
- Prior to starting HCV therapy
- At week four of therapy
- At week twelve of therapy
- At week 24 of therapy
- At week 48 of therapy
- 24 weeks following the end of therapy
Based on these clinical practice guidelines, the Medicaid program is updating its reimbursement policy for hepatitis C laboratory testing. Effective for dates of service on or after April 1, 2009:
- MMIS procedure code 87522 is to be used whenever a laboratory bills for a HCV quantitative viral load test. The maximum reimbursable amount for code 87522 is $59.20. The HCV viral load test (quantitative) is a covered service when clinically indicated, up to a maximum of six tests per 12-month period per patient.1
- Clinical laboratories, Designated AIDS Centers, hospital outpatient services, residential health care
facilities, and ordering practitioners are reminded of the following payment policies applicable to all
laboratory testing, including hepatitis C testing:
- Laboratories may not bill for tests performed when patients are hospitalized. Medicaid payment to the hospital includes all necessary laboratory services.
- Laboratories may not bill for tests performed for clinic patients when that clinic has contracted for laboratory tests. Medicaid payment to the clinic (hospital outpatient department or Diagnostic and Treatment Center) includes all necessary laboratory tests.
Questions? Please call the Bureau of Policy Development and Agency Relations at (518) 473-2160.
1AASLD guidelines emphasize hepatitis C treatment should be individualized and monitored closely. During the course of treatment, exceptions to these guidelines may warrant an additional test. As with all tests, full documentation and medical justification should be included in the medical record.
17 ALPHA-HYDROXYPROGESTERONE CAPROATE
(17P) FOR PREVENTION OF PRETERM DELIVERY
Return to Table of Contents
17 alpha-hydroxyprogesterone caproate (17P) is an injectable long-acting synthetic derivative of progesterone, administered for the prevention of preterm delivery in patients with a documented history of previous spontaneous preterm birth. 17P must be prepared by, and purchased from, a pharmacy with the ability to compound drugs.
This drug is covered under the Medicaid program as a physician-administered drug ONLY, and is not included in the Medicaid formulary file. Therefore, Medicaid managed care and Family Health Plus (FHPlus) plans are responsible for covering this medication for their enrollees. When administered to an enrollee of a managed care plan, reimbursement and documentation requirements are determined by the provider's contract with the managed care plan.
17P is billed by private physicians, nurse practitioners, nurse midwives and ordered ambulatory providers using procedure code J3490 Unclassified Drugs. 17P is not included in the Article 28 clinic APG. Under the Medicaid feefor- service program, reimbursement is "By Report" and the billing provider must submit a paper claim accompanied by an invoice showing the cost of purchase from the compounding pharmacy, NDCs used in compounding, and a report documenting medical need. To identify the drug for rebate purposes, the claim must include the NDC for the bulk powder used in compounding. For more information on billing physician administered drugs, please refer to the December 2008 Medicaid Update.
Effective January 1, 2011, rebate agreements with all manufacturers of bulk powders used to formulate the 17P compound will expire. The New York Medicaid program, and Medicaid managed care and FHPlus plans, will continue to cover 17P. A future communication will be published instructing Medicaid fee-for-service providers on new eMedNY billing procedures.
Questions? Contact the Bureau of Program Planning & Implementation at (518) 473-0122.
ARE YOUR UNINSURED PATIENTS ELIGIBLE FOR THE
NEW YORK BRIDGE PLAN?
Return to Table of Contents
In March 2010, Congress passed the health care reform law, the Patient Protection and Affordable Care Act. The law created the Pre-Existing Condition Insurance Plan (PCIP), a temporary program until January 2014 that makes coverage available for individuals who have:
New York City Hospitals:
- a pre-existing medical condition;
- not had insurance for six months;
- and are legal US residents.
In New York, the PCIP plan is the NY Bridge Plan, administered by GHI, an EmblemHealth company. The NY Bridge Plan is an Exclusive Provider Option (EPO), which means that enrollees must use doctors and health care providers who are in the GHI EPO network, except in cases of emergency or when care is not available through a participating provider. The NY Bridge Plan covers a broad range of health benefits, including primary and specialty care, hospital care, and prescription drugs. Eligibility is not based on income and the Plan does not charge a higher premium because of a pre-existing condition. Coverage for a pre-existing condition begins right away, with no waiting period.
Additional information on the NY Bridge Plan, including how to enroll, premium rates, qualifying pre-existing conditions, and answers to other frequently asked questions can be found at: http://www.ghi.com/nybridgeplan/index.html
The Website also provides brochures in English and Spanish, please see:
http://www.ghi.com/nybridgeplan/assets/nybridgeplan_brochure.pdf
http://www.ghi.com/nybridgeplan/assets/nybridgeapp_sp.pdf
Eligibility Specialists are available to answer questions and to offer enrollment assistance from 8:30 am to 5:30 pm, Monday through Friday at: 1-866-NY-EZ-APP (1-866-693-9277).
IMPORTANT INFORMATION REGARDING
ENROLLMENT AND MAINTENANCE FORMS
Return to Table of Contents
PROVIDERS ARE REMINDED TO USE THE MOST CURRENT ENROLLMENT AND MAINTENANCE FORMS
New enrollment applications or requests to change or amend information to a provider's file must be submitted using the most current forms available.
In an effort to improve Medicaid processes for providers, eMedNY is converting enrollment and maintenance forms so that they can be completed by keying in the information and then printing for signature (when required) and mailing. This process will reduce the rejection of illegible hand-written forms.
Visit www.eMedNY.org for the most current enrollment applications and maintenance forms.
Questions? Please contact the eMedNY Call Center at (800) 343-9000.
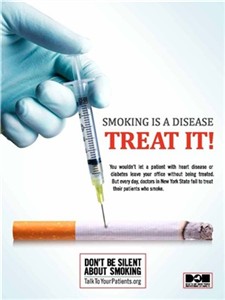
By providing counseling, pharmacotherapy, and referrals, you can double your patients' chances of successfully quitting. For more information, please visit www.talktoyourpatients.org or call the NY State Smokers' Quitline at 1-866-NY-QUITS (1-866-697-8487).
Do you suspect that a Medicaid provider or an enrollee has engaged in fraudulent activities?
Return to Table of Contents
Please Call: 1-877-87FRAUD or (212 417-4570)
Your call will remain confidential.
You can also complete a Complaint Form online at:
www.omig.state.ny.us

Provider Directory
Return to Table of Contents
Office of the Medicaid Inspector General:
http://www.omig.state.ny.us or call (518) 473-3782 with general
inquiries or 1-877-87FRAUD with suspected fraud complaints or allegations.
This contact information can also be used for Provider Self-Disclosures.
Questions about billing and performing MEVS transactions?
Please contact eMedNY Call Center at: (800) 343-9000.
Provider Training
To sign up for a provider seminar in your area, please enroll online at:
http://www.emedny.org/training/index.aspx
For individual training requests, call (800) 343-9000 or email: emednyproviderrelations@csc.com
Enrollee Eligibility
Call the Touchtone Telephone Verification System at any of the numbers below:
(800) 997-1111 (800) 225-3040 (800) 394-1234.
Address Change?
Questions should be directed to the eMedNY Call Center at: (800) 343-9000.
Fee-for-Service Providers
A change of address form is available at:
http://www.emedny.org/info/ProviderEnrollment/index.html
Rate-Based/Institutional Providers
A change of address form is available at:
http://www.emedny.org/info/ProviderEnrollment/index.html
Does your enrollment file need to be updated because you've experienced a change in ownership?
Fee-for-Service Providers please call (518) 402-7032
Rate-Based/Institutional Providers please call (518) 474-3575
Comments and Suggestions Regarding This Publication?
Please contact the editor, Kelli Kudlack, at:
medicaidupdate@health.state.ny.us
Medicaid Update is a monthly publication of the New York State Department of Health containing information regarding the care of those enrolled in the Medicaid Program.