New York State Medicaid Update - September 2016 Volume 32 - Number 9
In this issue …
- All Providers
- Policy and Billing Guidance
- Updated Requirements for Volunteer Driver Organizations: This Guidance Supersedes the Guidance Published in the March 2016 Medicaid Update
- New York State Medicaid Comprehensive Coverage and Promotion of Long Acting Reversible Contraception
- Long-Acting Reversible Contraception Carve-out for Federally Qualified Health Center Clinics
- End-Dating the Long Term Home Health Care Program (LTHHCP) Exception Code 30
- New York Medicaid Statewide Patient Centered Medical Home Program Incentive Payment Program Policy: Update on Retroactive Incentive Payments
- Enrollment of Newborns When the Mother is Enrolled in a Medicaid Managed Care Plan or a Health and Recovery Plan
- New York State Medicaid Expansion of Coverage for Surgical First Assistants
- New York State Medicaid Coverage Clarification of Ocular Tonometry
- Pharmacy Update
- Provider Directory
Introducing the Newly Redesigned CBIC Card: What Providers Need to Know (cover)
The New York State Common Benefit Identification Card (CBIC) has been redesigned with a new look!
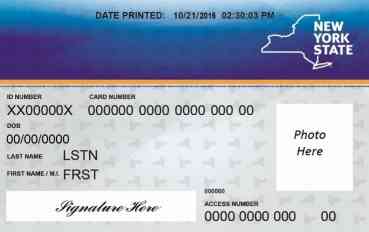
Effective August 1, 2016, the new Common Benefit Identification Card (CBIC) is available to Medicaid consumers who do not already have a card or need to request a replacement card.
Issuance of the new cards began at the two over-the-counter card issuance sites in New York City and mailed CBIC cards with the new design will begin statewide in late September 2016.
There will be no mass replacement of existing cards as a result of the new card design. Existing active blue and white cards with the current logo will continue to work throughout this transition and must be accepted by all Medicaid enrolled providers, including pharmacies, according to current procedures.
Reminder: It is unlawful to give, lend, sell, buy or offer inducements to obtain the use of a Medicaid enrollee's card.
Additional information on the new card design can be found at: www.otda.ny.gov/workingfamilies/ebt.asp
New York Medicaid EHR Incentive Program Update
The New York Medicaid Electronic Health Record (EHR) Incentive Program provides financial incentives to eligible professionals and hospitals to promote the transition to EHRs. Providers who practice using EHRs are in the forefront of improving quality, reducing costs and addressing health disparities. Since December 2011 over $783 million in incentive funds have been distributed within 24,271 payments to New York State Medicaid providers.
24,271
Payments
$783+
Million Paid
Are you eligible? For more information, visit www.emedny.org/meipass
Did you know?
2016 is the last year that eligible professionals (EPs) may begin participation in the New York Medicaid EHR Incentive Program. An EP may receive up to $63,750 over the course of six years, which includes a lump sum payment of $21,250 for the first participation year wherein the EP can demonstrate, adopt, implement, or upgrade to certified EHR technology. Thereafter, the EP may receive $8,500 for each of the remaining five years for demonstrating meaningful use. Visit https://ehrincentives.cms.gov/hitech/login.action to register for the program.
MEIPASS Availability
The New York Medicaid EHR Incentive Program Administrative Support Service (MEIPASS) is currently closed due to important maintenance being performed on the system for meaningful use attestations for payment year 2015 and beyond. It is anticipated that MEIPASS will reopen in early fourth quarter of calendar year 2016. Announcements will be made via LISTSERV and the program website regarding system availability and deadlines. Program support will continue to be available by phone at 877-646-5410.
Program Discussion
On August 23, 2016, the New York Medicaid EHR Incentive Program Support Team held a Town Hall meeting to provide important updates regarding the availability of MEIPASS, changes of the system, and preparations necessary to attest. This presentation was recorded and will be released to the public at a later date. If you were unable to attend this presentation and would like more information, please contact program support by phone at 877-646-5410 Option 2 or by email at hit@health.ny.gov.
Questions? Contact hit@health.ny.gov for program clarifications and details.
Updated Requirements for Volunteer Driver Organizations
This Guidance Supersedes the Guidance Published in the March 2016 Medicaid Update
The New York State Department of Health recognizes that volunteer drivers are a valuable component of the Medicaid Transportation Program, especially in transporting enrollees to necessary medical services in rural areas.
All volunteer driver organizations must be enrolled as Medicaid providers and can only assign trips to volunteer drivers who are affiliated with their organization.
Volunteer driver organizations are required to:
- Perform criminal background checks and driver's license verifications before assigning any Medicaid funded trips to a volunteer driver; and
- Ensure that all drivers maintain the appropriate vehicle liability insurance.
Volunteer drivers must:
- Maintain a valid license that is appropriate for the size and type of vehicle they are operating;
- Provide curb to curb transportation;
- Maintain all required records necessary to support a Medicaid transportation claim;
- Meet or exceed Medicaid quality standards (e.g., no smoking, vehicle cleanliness, etc.); and
- Maintain at least the minimum insurance requirements in accordance with the New York State Department of Motor Vehicles.
Vehicles used by volunteer drivers must:
- Have doors that are in working order;
- Be equipped with a working Global Positioning System (GPS);
- Pass the annual New York State Vehicle Safety and Emissions inspection; and
- Be retired at fifteen (15) years of age.
Questions may be referred to the Medicaid Transportation Unit at(518) 473–2160 or via email to MedTrans@health.ny.gov.
New York State Medicaid Comprehensive Coverage and Promotion of Long-Acting Reversible Contraception
The 2016-2017 New York State Executive Budget included an initiative for the comprehensive coverage and promotion of Long-Acting Reversible Contraception (LARC), including increasing access and improving education and outreach.
LARC methods include the intrauterine device (IUD) and the contraceptive implant. According to the American College of Obstetricians and Gynecologists, both methods are highly effective in preventing pregnancy and are reversible. In support of the initiative, Fee-For-Service (FFS) and Medicaid Managed Care (MMC) have implemented the following:
Fee-For-Service
- The Department of Health has obtained approval from the Centers for Medicare & Medicaid Services to allow the cost of LARC to be paid to Federally Qualified Health Centers (FQHCs) separately from the Prospective Payment System (PPS) rate. Reimbursement for actual acquisition cost of LARC is available retroactively to April 1, 2016. Please see the Long-Acting Reversible Contraception (LARC) Carve-out for Federally Qualified Health Center (FQHC) Clinics article in this edition of the Medicaid Update for billing guidelines.
- Medicaid FFS coverage and payment for post-partum LARC was separated from the inpatient APR-DRG reimbursement effective April 1, 2014. Please see the revised announcement, published on April 9, 2015, online at: https://www.emedny.org/listserv/Inpatient/Inpatient_Clarification_on_Reimbursement_for_LARC_Provided_as_an_Inpatient_Post-Partum_Svc_4-9-15.pdf. Effective May 1, 2014, MMC plans were encouraged to accommodate and promote coverage of LARC provided to women during their postpartum inpatient hospital stay.
Medicaid Managed Care
- Effective September 1, 2016, the Department of Health requires MMC plans to implement mechanisms to pay hospitals for immediate postpartum LARC separately from reimbursement for the inpatient stay.
Policy questions regarding Medicaid FFS may be directed to the Office of Health Insurance Programs, Division of Program Development and Management at(518) 473–2160 . Questions on billing or claims should be directed to the eMedNY call center at 1-800-343-9000. Questions regarding MMC reimbursement and/or documentation requirements should be directed to the enrollee's MMC plan.
Long-Acting Reversible Contraception Carve-out for Federally Qualified Health Center Clinics
The cost of Long-Acting Reversible Contraception (LARC) is being carved-out of the Federally Qualified Health Center (FQHC) prospective payment system (PPS) rates effective for dates of service on and after April 1, 2016. The LARC procedure codes in Table 1 may be billed to Medicaid Fee-For-Service (FFS) as an ordered ambulatory service on a separate claim from the clinic's PPS claim for the insertion of a device or removal and insertion of a new device.
A clinic designated as a FQHC must be enrolled in the Medicaid Program with the category of service of 0163 (ordered ambulatory diagnostic and treatment center) or 0282 (hospital based ordered ambulatory) in order to bill separately for the cost of the LARC. Call 1-800-343-9000 if you have questions about your clinic's enrolled category/categories of service.
Clinics contracting with a patient's Medicaid Managed Care (MMC) plan to provide intrauterine devices (IUDs) may not bill LARC as ordered ambulatory services under FFS. These clinics must bill the patient's Managed Care plan at rates negotiated with the plan.
Under the free access policy, when a MMC enrollee receives an IUD or implant from a qualified non-network clinic, the non-network provider bills Medicaid FFS at established rates and fees.
Members enrolled in a MMC plan that does not include family planning services in their benefit package (e.g., New York State Catholic Health Plan, dba Fidelis Care New York) can access these services, including purchase, insertion or removal of an IUD from a qualified Medicaid FFS provider who bills Medicaid FFS at established rates and fees.
| LARC Description | Procedure Code |
|---|---|
| Levonorgestrel-releasing intrauterine contraceptive system, 52 mg, 3 year duration (Liletta) | J7297 |
| Levonorgestrel-releasing intrauterine contraceptive system, 52 mg, 5 year duration (Mirena) | J7298 |
| Intrauterine copper contraceptive (ParaGard) | J7300 |
| Levonorgestrel-releasing intrauterine contraceptive system, 13.5 mg, 3 year duration (Skyla) | J7301 |
| Etonogestrel (contraceptive) implant system, including implant and supplies (Implanon or Nexplanon) | J7307 |
Medicaid FFS reimbursement for LARC is limited to the provider's acquisition cost by invoice. Providers must report the actual acquisition cost of the LARC in the charges field of the ordered ambulatory claim. Two separate claims will be required for submission - one for reimbursement of the clinic visit (PPS rate) and one for the LARC (acquisition cost). Claims for the LARC do not require submission of an invoice, although the invoice must be maintained by the provider for a period of six years for audit purposes. Please see article Reasonability Edits for Practitioner-Administered Drugs, published in the August 2015 Medicaid Update, for important claims processing rules.
Policy questions regarding Medicaid FFS may be directed to the Office of Health Insurance Programs, Division of Program Development and Management at(518) 473–2160 . Questions on Billing or Claims should be directed to the eMedNY call center at 1-800-343-9000. Questions regarding MMC reimbursement and/or documentation requirements should be directed to the enrollee's MMC plan.
End-Dating the Long Term Home Health Care Program (LTHHCP) Exception Code 30
As part of New York State's Medicaid Redesign Initiative (MRT 90), and with the approval of the Centers for Medicare and Medicaid Services, mandatory enrollment of LTHHCP participants into Mainstream Managed Care (MMC) or Managed Long Term Care (MLTC) began in 2013. At this time, all LTHHCP participants have transitioned to MMC, MLTC or other waiver programs. The program formally closed on May 27, 2016.
To promote continuity of care throughout the transition process, the Local Departments of Social Services were instructed to keep Exception Code 30 on file as this code identified individuals as LTHHCP participants and entitled to 90 days of community based long term care services and supports under the pre-existing service plan.
As more than 90 days have elapsed since the official closing of the program, the continuity period is over and there is no longer a need to maintain the Exception Code 30 on the individual case record. Therefore, Exception Code 30 was end-dated with an effective date of August 31, 2016 on all cases.
Questions may be directed to Vicki Rockefeller in the Bureau of Managed Long Term Care at(518) 474–5888 or email at vicki.rockefeller@health.ny.gov.
New York Medicaid Statewide Patient Centered Medical Home Program Incentive Payment Program Policy: Update on Retroactive Incentive Payments
Background:
The New York State Medicaid Statewide Patient Centered Medical Home (PCMH) Incentive Payment Program provides financial incentives to primary care practices who achieve PCMH recognition from the National Committee for Quality Assurance (NCQA). Payments are given as either per member per month (PMPM) capitation payments for Medicaid Managed Care (MMC) members or as an add-on payment for eligible claims billed for services provided to Medicaid Fee-For-Service (FFS) members. Rates for both PMPM payments and add-ons depend on a provider's NCQA recognition standard and level. For more information on the current established rates, please see the November 2015 Medicaid Update.
The first week of each month, the New York State Department of Health's Office of Health Insurance Programs (OHIP) posts the most recent list of PCMH-recognized practices and their providers to the Health Commerce System (HCS). The list contains the most recent PCMH recognition information the Department has on file from NCQA at that time. MMC plans use this list to identify which practices and providers in their networks are eligible to receive the PCMH incentive payments and the rate they should receive.
Due to the monthly schedule of data transmissions from NCQA to the Department of Health and from the Department of Health to HCS, it takes approximately 60 to 90 days after recognition is awarded for health plans to be notified of a new or changed recognition status. This lag has historically caused a two to three month delay in practices receiving PCMH incentive payments.
Policy Change:
Effective January 1, 2017, all MMC plans will be required to pay incentives for the New York State Medicaid Statewide PCMH Incentive Payment Program as of the month of PCMH recognition. This ensures incentives will be paid for every month of PCMH eligibility to practices and their providers. This may require plans to process retroactive payments to recognized practices and providers in their network when affected by this initial lag of information. Regardless of the NCQA recognition effective date, payments due to practices must account for the entire first month of their recognition, and should not be prorated.
MMC plans are required to distribute PCMH incentive payments to practices at least bi-annually, and MMC plans are encouraged to process on a more frequent basis if possible. Providers with questions regarding the frequency of payment for individual plans should contact their MMC plan representatives directly.
Finally, to ensure accurate incentive payments from both MMC plans and FFS Medicaid, providers must supply NCQA with the full address of the site's physical location, not a billing site address. The National Provider Identifier (NPI) for the group and the individual NPIs of practitioners working at the practice should be provided to NCQA to ensure payments are made accurately.
Questions regarding this policy change may be directed to pcmh@health.ny.gov. Questions regarding claim eligibility and/or billing guidance for Medicaid FFS claims should be directed to the eMedNY call center at 1-800-343-9000. For more information on how to achieve NCQA PCMH recognition, providers may contact NCQA at 1-888-275-7585 or visit the NCQA website at www.ncqa.org.
Enrollment of Newborns When the Mother is Enrolled in a Medicaid Managed Care Plan or a Health and Recovery Plan
Newborns born to women receiving medical assistance on the date of birth are automatically eligible for Medicaid for one year. If the mother is enrolled in a Medicaid Managed Care plan (MMCP), the newborn will be enrolled in the same plan from the date of birth. If the mother is enrolled in the Medicaid Managed Care Organization's Health and Recovery Plan (HARP), the newborn will be automatically enrolled in the sister mainstream Medicaid Managed Care product. The only exception to the automatic enrollment of a newborn into the same MMCP as the mother is when the newborn receives comprehensive third party health insurance (TPHI). In this case, the child will be disenrolled to Fee-For-Service (FFS) Medicaid.
What Pharmacies Need to Know:
When the mother of an infant presents the infant's Medicaid benefit card to the pharmacy to obtain a prescription for the infant, the pharmacy should recognize that the infant is guaranteed eligibility through the mother's MMCP or, if the mother is not enrolled in a MMCP, through Medicaid FFS. The pharmacist should ask the mother if she is enrolled in Medicaid FFS or Medicaid Managed Care to verify which insurance they should bill for the infant's prescription. If the mother of the infant is enrolled in Medicaid FFS, the pharmacist should bill Medicaid FFS for the infant's prescription. If the mother is enrolled in Medicaid Managed Care, the pharmacist should ask her to present her MMCP card, as the infant will be enrolled in the same MMCP. The claim should then be processed through the MMCP that the mother is associated with (after any available third party health insurance is billed). If the claim cannot be processed because the infant is not found in the MMCP's system, the pharmacist should contact the MMCP (not the plan's pharmacy benefits manager) to report the infant's information. The MMCP will add the information into the system to allow for an on-line adjudication. If the mother is enrolled in a MMCP, the pharmacy should NOT process the claim through the Medicaid FFS (eMedNY) system, as the infant's eligibility file may not be updated for plan enrollment, and the resulting erroneous payments will be subject to audit and recoupment.
Hospital Responsibilities:
Current State regulations require hospitals and all approved Medicaid providers to conduct a Medicaid eligibility verification (eMedNY) clearance on each presenting Medicaid recipient to determine Medicaid eligibility status and medical coverage. Under this policy, hospitals must also determine the newborn's managed care status by checking the mother's status on eMedNY. The hospital must check:
- Medicaid eligibility status;
- Medical coverage - Eligible PCP ; and
- MEVS eligibility responses no longer include the scope of services covered by the managed care plan. Providers must contact the health plan for this information, because MEVS eligibility responses no longer include scope of benefits information for managed care plans. Service type codes are used to identify carved-out services, where possible.
Providers must continue to determine whether the newborn and/or mother are enrolled in a MMCP. If either is enrolled and the service to be provided is covered by the MMCP, the provider should contact the plan before rendering service, except in an emergency.
Note: HARPs are MMCPs specifically for Medicaid recipients with significant behavioral health needs. Unlike other Medicaid Managed Care products, HARPs do not enroll individuals under 21 years of age. Newborns of HARP enrolled mothers will be automatically enrolled in the sister mainstream MMCP operated by the same Managed Care Organization. If the mother prefers to enroll the child in a plan other than the one in which the child is automatically enrolled, the child may be transferred to a different plan prospectively, at the mother's request.
For more information on newborn enrollment when a mother is enrolled in Medicaid managed care, please refer to the January 2013 Medicaid Update. Questions regarding Medicaid managed care may be referred to the Consolidated Call Center at(800) 541-2831 . Questions regarding Medicaid eligibility for newborns may be referred to the toll-free Newborn Helpline at(877) 463-7680 .
New York State Medicaid Expansion of Coverage for Surgical First Assistants
Pursuant to Social Services Law § 365-a (2) (cc), effective October 1, 2016 for Medicaid Fee-For-Service (FFS) and December 1, 2016 for Medicaid Managed Care (MMC), the New York State Medicaid program will recognize Registered Nurse First Assistants (RNFAs) and provide additional surgical assist reimbursement when appropriate.
An RNFA is a registered professional nurse who is certified in operating room nursing. The RNFA provides supportive and restorative patient care by performing as a first assistant at surgery under the direction of a licensed physician in accordance with scope of practice qualifications.
Physicians seeking to claim reimbursement that includes RNFA services must first verify that the procedure being performed allows for a non-physician surgical assistant per the Centers for Medicare and Medicaid Services guidelines at https://www.cms.gov/.
Claims for services that meet the above criteria should be billed by appending the “AS” modifier to the appropriate procedure code. Reimbursement for approved services will be made to the physician. Additional billing instructions can be found on eMedNY.org at the following link: https://www.emedny.org/ProviderManuals/Physician/PDFS/Physician%20Procedure%20Codes%20Sect5.pdf
Medicaid FFS policy questions may be directed to the Office of Health Insurance Programs' Division of Program Development and Management at(518) 473-2160 . Questions regarding MMC reimbursement and/or documentation requirements should be directed to the enrollee's MMC plan.
New York State Medicaid Coverage Clarification of Ocular Tonometry
The purpose of this article is to clarify New York State Medicaid's policy regarding coverage of ocular tonometry. Ocular tonometry is a method of measuring intraocular pressure for use in screening and diagnosing glaucoma. Medicaid considers the use of an ocular tonometer to be included in the reimbursement for an evaluation and management (E&M) visit. This policy applies to both Medicaid Fee-For-Service (FFS) and Medicaid Managed Care (MMC) Plans.
All providers are reminded to ensure that the services they are providing to patients fall within their scope of practice. Professional guidance on scope of practice can be found on the New York State Education Department's website at the following link: http://www.op.nysed.gov/prof/med/.
Medicaid FFS policy questions may be directed to the Office of Health Insurance Programs' Division of Program Development and Management at(518) 473-2160 . Questions regarding MMC reimbursement and/or documentation requirements should be directed to the enrollee's MMC plan.
Mosquito Repellent Coverage
Effective September 1, 2016, New York State Fee-For-Service (FFS) Medicaid provides coverage for mosquito repellent when prescribed to enrollees who intend to travel to, or return from a Centers for Disease Control and Prevention (CDC) recognized area of localized Zika transmission as reported here: http://www.cdc.gov/zika/geo/united-states.html. Medicaid Managed Care Plans are also required to cover mosquito repellent consistent with this guidance and must add covered mosquito repellents to their plan formularies as a covered over-the-counter product.
Currently, per the CDC, there are no known locally transmitted cases in New York State. To prevent the Zika virus from spreading, New York State FFS Medicaid will pay for mosquito repellent until the CDC states that there is no longer a risk./p>
Consistent with Medicaid policy for coverage of non-prescription items, a fiscal order, which includes all the same information contained on a prescription, is required. Fiscal orders should be written for one container (no refills). Some examples of covered items that have been evaluated for effectiveness by the U.S. Environmental Protection Agency, and approved for use by the CDC are listed below. Please note that this is not a comprehensive list of covered products. A full list of covered products can be found at: https://www.emedny.org/info/formfile.aspx.
Pharmacies may bill using the National Drug Codes (NDCs) provided, which have been derived by First Data Bank using the Universal Product Code (UPC).
| Drug Name | Package Size | NDC |
|---|---|---|
| OFF DEEP WOODS 25% SPRAY | 170 | 46500001842 |
| OFF DEEP WOODS DRY 25% SPRAY | 113 | 46500071764 |
| COLEMAN HIGH-DRY 25% REPEL SPRAY | 113 | 68093007514 |
| CUTTER BACKWOODS DRY 25% SPRAY | 113 | 71121096435 |
| CUTTER BACKWOODS 25% SPRAY | 170 | 71121096280 |
| REPEL SPORTSMEN 25% SPRAY | 184 | 11423094137 |
| NATRAPEL 20% SPRAY | 177 | 44224006878 |
Additional information regarding the Zika Virus can be found at: http://www.cdc.gov/zika/index.html and https://www.health.ny.gov/diseases/zika_virus/. CDC recommendations for travel care, including after travel care, can be found at: http://www.cdc.gov/zika/prevention/plan-for-travel.html.
IDNYC
IDNYC is New York City's government-issued photo identification card, available to all city residents aged 14 and older who provide proof of identity and residency. IDNYC is designed to meet State and federal standards of identity verification for people purchasing and accepting delivery of prescription medications and controlled substances purchased over the counter. A letter to familiarize pharmacies of the new card was recently mailed. More information can be found at www1.nyc.gov/site/idnyc/index.page.
Public Health Emergency Response Network Pharmacy Program (PHERN PP): A message from the New York City Health Department to community pharmacists in New York City!
As a community pharmacist, you are among the most accessible and trusted healthcare professionals in your community. We at the New York City Department of Health and Mental Hygiene (DOHMH) recognize that you serve a critical role not only in providing medications but also providing important health information to residents of your communities on a daily basis.
The New York City Department of Health is very interested in working with community pharmacists to support them in preparing for and recovering from disasters and other emergencies. However, we currently have no mechanism to communicate effectively with the more than 2,000 independent community pharmacies in New York City.
To address this gap, NYC DOHMH created the Public Health Emergency Response Network Pharmacy Program (PHERN PP), a simple application that allows New York City pharmacies to quickly and easily “register” and provide pharmacy contact and other service information. This information will assist us in engaging in a productive, reciprocal exchange of information that is essential for effective emergency preparedness and response, and will enable us to better support you and your important work ensuring the health and well-being of all New Yorkers.
The registration process is simple and should only take five minutes. Go to http://on.nyc.gov/phern and scroll down to select the PHERN Pharmacy Program. Questions about the program can be directed to Eric Medina, PHERN PP Coordinator, at PHERNPP@health.nyc.gov.
Thank you for supporting this important emergency preparedness initiative in NYC!
The Medicaid Update is a monthly publication of the New York State Department of Health.
Andrew M. Cuomo
Governor
State of New York
Howard A. Zucker, M.D., J.D.
Commissioner
New York State Department of Health
Jason A. Helgerson
Medicaid Director
Office of Health Insurance Programs
Provider Directory
Office of the Medicaid Inspector General:
For suspected fraud complaints/allegations, call 1-877-87FRAUD, (877) 873-7283, or visit www.omig.ny.gov.
Provider Manuals/Companion Guides, Enrollment Information/Forms/Training Schedules:
Please visit the eMedNY website at: www.emedny.org.
Providers wishing to listen to the current week's check/EFT amounts:
Please call (866) 307-5549 (available Thursday PM for one week for the current week's amount).
Do you have questions about billing and performing MEVS transactions?
Please call the eMedNY Call Center at (800) 343-9000.
Provider Training:
To sign up for a provider seminar in your area, please enroll online at: http://www.emedny.org/training/index.aspx. For individual training requests,call (800) 343-9000 or e-mail: emednyproviderrelations@csc.com.
Enrollee Eligibility:
Call the Touchtone Telephone Verification System at (800) 997-1111.
Medicaid Prescriber Education Program:
For current information on best practices in pharmacotherapy, please visit the following websites: http://www.health.ny.gov/health_care/medicaid/program/prescriber_education/presc-educationprog and
http://nypep.nysdoh.suny.edu/home
Need to change your address? Does your enrollment file need to be updated because you have experienced a change in ownership? Do you want to enroll another NPI? Did you receive a letter advising you to revalidate your enrollment?
Visit http://www.emedny.org/info/ProviderEnrollment/index.aspx and choose the link appropriate for you (e.g., physician, nursing home, dental group, etc.).
Medicaid Electronic Health Record Incentive Program questions?
Contact the New York Medicaid EHR Call Center at (877) 646-5410 for assistance.
Comments and Suggestions Regarding This Publication?
Please contact the editor, Amy Siegfried, at medicaidupdate@health.ny.gov