New York State Medicaid Update - September 2024 Volume 40 - Number 10
In this issue …
- Policy and Billing
- Updated Licensure Threshold Guidance for Ambulatory Services
- Updated Medicaid Coverage of Mental Health Counseling by Licensed Clinical Social Workers and Licensed Master Social Workers Approved for Article 28 Outpatient Hospital Clinics and Free-Standing Diagnostic and Treatment Centers
- Blood Glucose Testing and Monitoring Changes
- Upcoming Changes to Billing Requirements for Professional Drug Claims
- All Providers
- Pharmacy
Information in gray boxes in this issue indicates material abridged but linked from the succinct interactive Portable Document Format (PDF) version.
Updated Licensure Threshold Guidance for Ambulatory Services
The New York State (NYS) Department of Health (DOH), NYS Office of Mental Health (OMH), NYS Office of Addiction Services and Supports (OASAS), and NYS Office for People with Developmental Disabilities (OPWDD) announced updates to "licensure thresholds," effective October 1, 2024. Licensure thresholds are the amount of physical, behavioral health or diagnostic and treatment services that can be delivered by a licensed provider without requiring another license, certification, or designation by a NYS oversight agency to provide those services.
Prior to this update*, providers that wished to offer ambulatory primary care, behavioral health services or diagnostic and treatment services above the established thresholds, were required to obtain an additional license, certification, or designation from more than one NYS agency. To increase access to integrated care for individuals with co-occurring needs and ease administrative burdens on providers, NYS DOH, NYS OMH, NYS OASAS, and NYS OPWDD have updated existing licensure thresholds as outlined below.
Guidance for Providers Under Updated Licensure Thresholds
Article 28 Provider Offering Ambulatory Behavioral Health Services and/or Diagnostic and Treatment Services
Article 28 providers who wish to offer integrated ambulatory services may deliver up to 30 percent of their total annual visits for mental health, addiction and/or diagnostic and treatment services without obtaining an Article 31 license from NYS OMH, an Article 32 certification from NYS OASAS, or Article 16 certification from NYS OPWDD. The majority of services provided in an Article 28 must be physical health services.
Behavioral Health Services Provider (Article 31 and Article 32) Offering Primary Care Services
NYS DOH has raised the licensure threshold for NYS OMH Mental Health Treatment and Rehabilitative Services (MHOTRS) programs licensed pursuant to of the Title 14 New York Codes, Rules, and Regulations (NYCRR) Part 599, and Article 32 providers certified pursuant to Title 14 NYCRR Part 822, to enable them to provide up to 30 percent of their total annual visits for primary care services, without obtaining an Article 28 license from NYS DOH. Medical services that occur throughout the NYS OASAS-bedded programs are not subject to the thresholds as outlined in guidance. The guidance will be effective for NYS OMH-licensed clinics providing primary care services, when the amendment to NYS OMH Part 599 regulations becomes effective, which is necessary to effectuate the changes outlined in this guidance. The amendment is anticipated to become effective in the near future.
Mental Health Services Provider (Article 31) Offering Addiction Services and Addiction Services Provider (Article 32) Offering Mental Health Services
NYS OMH-licensed and NYS OASAS-certified providers may continue to integrate mental health and addiction services for individuals with co-occurring conditions in accordance with NYS OMH and NYS OASAS regulations and guidance. Providers are not required to obtain an Integrated Outpatient Services (IOS) license, pursuant to Title 14 NYCRR Part 598 or Title 14 NYCRR Part 825, for this purpose and such services are not subject to any thresholds. The NYS agencies are working on additional guidance regarding integrated mental health and addiction services in NYS OMH and NYS OASAS settings.
I/DD Services Provider (Article 16) Offering Primary Care Services
NYS DOH has raised the licensure threshold for Article 16 clinic providers offering diagnostic and treatment services to people with I/DDs, as determined eligible by NYS OPWDD, to enable Article 16 clinic providers to provide up to 30 percent of their total annual visits for primary care services, without obtaining an Article 28 license from NYS DOH.
The following table illustrates the changes being made in this guidance:
| Licensure Thresholds Prior to October 1, 2024 |
Licensure Thresholds As of October 1, 2024 |
|||||||
|---|---|---|---|---|---|---|---|---|
| License Type | Diagnostic and Treatment Services1 | Primary Care | Mental Health | Addiction Services | Diagnostic and Treatment Services1 | Primary Care | Mental Health | Addiction Services |
| Article 16 | N/A | 20 percent | ** | ** | N/A | 30 percent | ** | ** |
| Article 28*** | 20 percent* | N/A | 30 percent | Zero percent | 30 percent* | N/A | 30 percent | 30 percent |
| Article 31 | ** | Five percent | N/A | ** | ** | 30 percent | N/A | ** |
| Article 32 | ** | Five percent | ** | N/A | ** | 30 percent | ** | N/A |
Billing
At this time, providers should continue billing for comprehensive services as is currently identified in their respective billing guidance. The NYS agencies are working to publish additional guidance and will notify providers and health care plans when this guidance is available, as well as whether there are any impacts to current billing practices. Providers should refer to the full Updated Licensure Threshold Guidance for Ambulatory Services for New York State Department of Health (DOH), Office of Mental Health (OMH), Office of Addiction Services and Supports (OASAS), and Office for People With Developmental Disabilities (OPWDD) programs. Please note: This guidance does not apply to IOS licensed providers, Delivery System Reform Incentive Payment (DSRIP) 3.a.i-approved providers, and comprehensive services that are already permissible under the license, certification, or designation of the provider and defined within NYS agency regulations.*
1. For I/DDs. In all circumstances, services that are already permissible (e.g., Health Monitoring Services in an Article 16, Article 31 or Article 32 setting) do not count against the threshold.;1
*Only in settings where less than 50 percent of the population served has an I/DD, as determined eligible by NYS OPWDD, and more than 30 percent of total services are diagnostic and treatment services for people with I/DDs.
**Providers can deliver integrated behavioral healthcare to individuals who meet the appropriate admission criteria, within scope and to the extent which staff have the necessary education, training, and experience.
***Notwithstanding the threshold allowances provided herein, the majority of services provided in an Article 28 must be physical health services.
NYS Agency Resources
Certification and Designation:
- NYS DOH "Certificate of Need (CON)" web page
- NYS OMH "Licensing" web page
- NYS OASAS "Program Certification" web page
- NYS OPWDD "Contact Us" web page, under the "Provider Inquiries - Regional Offices" tab
- NYS OPWDD "Article 16 Clinics" web page
Licensing Contact Information:
- NYS DOH - cons@health.ny.gov
- NYS OPWDD - clinic.services.information@opwdd.ny.gov
- NYS OASAS - picm@oasas.ny.gov
- NYS OMH Adult MHOTRS - omh.sm.adult-clinic@omh.ny.gov
- NYS OMH Children's MHOTRS - omhchildclinics@omh.ny.gov
Questions
Questions regarding this update should be directed to Tamara Glaser, Integrated Care Advisor for the NYS DOH Bureau of Adult Special Populations, at tamara.glaser@health.ny.gov.
Updated Medicaid Coverage of Mental Health Counseling by Licensed Clinical Social Workers and Licensed Master Social Workers Approved for Article 28 Outpatient Hospital Clinics and Free-Standing Diagnostic and Treatment Centers
Effectively immediately, for New York State (NYS) Medicaid fee-for-service (FFS) and Medicaid Managed Care (MMC) Plans, in accordance with changes to Public Health Law (PHL) §2807, mental health counseling provided by Licensed Clinical Social Workers (LCSWs) or Licensed Master Social Workers (LMSWs) rendered in Article 28 hospital outpatient department (OPD) clinics and free-standing diagnostic and treatment centers (D&TCs) will be expanded to include all ages and patient populations.
In an Article 28 clinic, there is no limit on the patient population that can receive treatment for services provided by Licensed Mental Health Counselors (LMHCs) or Licensed Marriage and Family Therapists (LMFTs). This expansion will allow LCSWs and LMSWs, in addition to LMHCs and LMFTs, to provide mental health counseling services within their scope of practice in an Article 28 clinic with no limitations on the patient population that can receive services in this setting. The Ambulatory Patient Group (APG) payment to the clinic includes the professional component for services rendered by a LCSW, LMSW, LMHC or LMFT; a professional claim cannot be billed.
For additional information pertaining to LCSW, LMSW, LMHC, and LMFT services, providers should refer to the Licensed Clinical Social Worker, Licensed Mental Health Counselor, and Licensed Marriage and Family Therapist Service Coverage article published in the December 2022 issue of the Medicaid Update.
Questions:
- NYS Medicaid FFS coverage and policy questions should be directed to the Office of Health Insurance Programs (OHIP) Division of Program Development and Management (DPDM) by telephone at (518) 473-2160 or by email at FFSMedicaidPolicy@health.ny.gov.
- MMC reimbursement, billing, and/or documentation requirement questions should be directed to the MMC Plan of the enrollee. MMC Plan contact information can be found in the eMedNY New York State Medicaid Program Information for All Providers - Managed Care Information document.
- NYS Medicaid FFS claims questions should be directed to the eMedNY Call Center at (800) 343-9000.
- NYS Medicaid FFS provider enrollment questions should be directed to eMedNY Provider Enrollment at (800) 343-9000.
Blood Glucose Testing and Monitoring Changes
As part of ongoing efforts to ensure optimal care for New York State (NYS) Medicaid members who require blood glucose testing, NYS Medicaid is making important changes to the coverage of blood glucose testing supplies, aligning with Medicare coverage criteria, which can be found in the Centers for Medicare & Medicaid Services (CMS) Medicare Coverage of Diabetes Supplies fact sheet. This update is designed to promote effective testing habits to support individuals managing their diabetes. Changes to the supply limits for test strips and lancets and the implications for pharmacies and healthcare providers, are explained below.
Overview of the New NYS Medicaid Policy
Effective October 1, 2024, the NYS Medicaid blood glucose testing supply coverage will align with Medicare policies. The new guidelines are as follows:
- NYS Medicaid members using insulin: Individuals requiring insulin for blood glucose management will be eligible to receive up to 300 test strips and 300 lancets every three months.
- NYS Medicaid members not using insulin: Individuals managing their diabetes without insulin will be eligible for an allowance up to 100 test strips and 100 lancets every three months.
Why This Change Matters
Simplifying Access: Aligning NYS Medicaid policies with the latest clinical guidelines simplifies the process for both pharmacies and physicians, ensuring that beneficiaries receive the supplies they need without unnecessary hurdles.
Pharmacies and Practitioners:
Key Actions: To facilitate a smooth transition to the updated policy, NYRx recommends the following actions for pharmacies and health care providers:
- Educate Patients: Patients with diabetes should be informed about their current testing habits. Pharmacy personnel and health care providers should take the initiative to communicate these changes during patient interactions.
- Promote Effective Monitoring: For patients not currently on an adequate testing regimen, pharmacy personnel and health care providers should encourage establishing a regular routine for blood glucose monitoring, emphasizing the importance of being proactive in managing their condition.
- Understand Claims Processing Limitations: NYRx edit "00710" (Procedure/Formulary Code Exceeds Service Limits), located on the NYRx, the Medicaid Pharmacy Program: Top Edit Resource, will be triggered for claims exceeding the above frequency limitations. Providers should verify the prescription directions for use and consult the prescriber, as necessary, on any changes. Frequency/Quantity/Duration amounts over the current criteria may be considered on a case-by-case basis for limited durations. An example of a medical exception to this limitation could be a patient with a diagnosis of gestational diabetes requiring more frequent monitoring for a period of time.
Reminders
NYS Medicaid policy requires practitioners to provide a valid International Classification of Diseases, Tenth Revision (ICD-10) on prescriptions for diabetic supplies. The ICD-10 must be submitted using the National Council for Prescription Drug Programs (NCPDP) D.0 claim format.
The following are the NCPDP fields utilized to report the ICD-10:
| NCPDP D.0 Claim Segment Field* | Value |
|---|---|
| 424-DO | ICD-10 code identifying diagnosis of the patient. Do not transmit the decimal point for ICD codes, decimal point is implied |
| 491-VE | Maximum count of "5" |
| 492-WE | Code qualifying the ‘Diagnosis Code' sent "02" = ICD-10 coding |
*The NCPDP D.0 Companion Guide can be found on the eMedNY "5010/D.0 Transaction Instructions" web page.
Questions and Additional Information:
- Additional information regarding the new policy changes can be found on the NYRx Preferred Diabetic Supply Program Resource.
- Providers should refer to the CMS Medicare Coverage Database (MCD) Glucose Monitor - Policy Article.
- NYRx coverage and policy questions should be directed to the Medicaid Pharmacy Unit by telephone at (518) 486-3209 or by email at NYRx@health.ny.gov.
- Billing and claims processing questions should be directed to the eMedNY Call Center at (800) 343-9000.
Upcoming Changes to Billing Requirements for Professional Drug Claims
Effective October 1, 2024, in preparation for changes per the 2024-25 enacted budget for the reimbursement of practitioner administered drugs (PADs), the New York State (NYS) Department of Health (DOH) only pends claims for manual pricing "BR" (By report) for unlisted drug codes. This applies to the following drug codes:
- "J3490" - Unclassified drugs
- "J3590" - Unclassified biologicals
- "J9999" - Not otherwise classified, antineoplastic drugs
- "J7999" - Compounded drug, not otherwise classified
The above drug codes will continue to be billed via paper claim on an Medical Assistance Health Insurance Claim Form (eMedNY 150003 form), and require the submission of a manufacturer invoice showing the acquisition cost of the drug administered, including all discounts, rebates, and incentives, per program policy.
All other PADs with an assigned J code may be billed via an electronic claim format (837P) for the following categories of service (COS) and with date of service (DOS) that is on or after October 1, 2024:
- Physician and Physician Group ("COS 0460" and "COS 0046") - Additional information can be found on the eMedNY "Physician Manual" web page.
- Nurse Practitioner ("COS 0469") - Additional information can be found in the eMedNY "Nurse Practitioner Manual" web page.
- Midwife ("COS 0525") - Additional information can be found on the eMedNY "Midwife Manual" web page.
- Free Standing or Hospital Based Ordered Ambulatory ("COS 0163" for Clinic Based and "COS 0282" for Hospital Based) - Additional information can be found on the eMedNY " Free Standing or Hospital Based Ordered Ambulatory Manual".
- Podiatry Services ("COS 0500") - Additional information can be found on the eMedNY "Podiatry Manual" web page.
Please note: The practitioner is expected to limit the NYS Medicaid claim amount to the actual invoice cost of the drug dosage administered and maintain that documentation.
Paper claims will still be accepted for all J codes and are required for reimbursement of claims that exceed unit maximums or frequency. Additionally, there are still requirements for additional clinical criteria to be met for certain drugs. To learn more about the additional clinical criteria, practitioners should visit the NYS DOH "New York State Medicaid Fee-for-Service Practitioner Administered Drug Policies and Billing Guidance" web page.
Practitioners should refer to the associated eMedNY provider manual web pages linked above, for additional program policy and billing guidance. Providers are encouraged to use electronic claims submission whenever allowed. These changes should ease practitioner burden by decreasing paper claim submission and associated invoice documentation for claims with a DOS on or after October 1, 2024. It also will have a positive effect on the timing of remittance, thus shortening the turnaround time for payment.
Questions and Additional Information:
- NYS Medicaid fee-for-service (FFS) drug coverage and policy questions should be directed to the Office of Health Insurance Programs (OHIP) Division of Program Development and Management (DPDM) by telephone at (518) 473-2160 or by email at FFSMedicaidPolicy@health.ny.gov.
- NYS Medicaid FFS billing/claim questions should be directed to the eMedNY Call Center at (800) 343-9000.
ePACES Self-Help Guides Available on eMedNY Website
Electronic Provider Assisted Claim Entry System (ePACES) self-help guides are available on the eMedNY website, by selecting "self help" in the upper right-hand corner of the web page. All provided resources have been created to assist ePACES users with a wide variety of topics including claim entry, eligibility determination, prior approval and claim status inquiry.
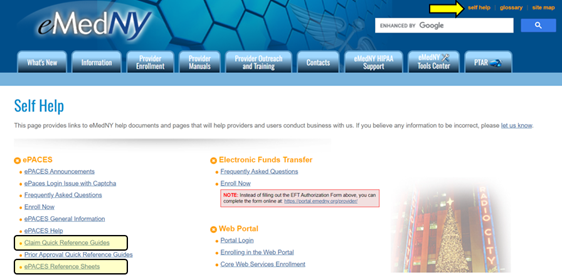
5010 ePACES Claim Reference Guides
5010 ePACES claim reference guides are available in Professional, Professional Real Time, Dental and Institutional formats, on the eMedNY "Claim Quick Reference Guides" web page. Guides include claim specific screen captures, descriptions of the individual claim entry fields and instructions on how to batch and submit completed claims.
ePACES Reference Sheets
ePACES reference sheets assist users with important features and functions in ePACES. ePACES reference sheets currently available include the following:
- ePACES - Building and Submitting Claim Batches
- ePACES - Claim Balancing
- ePACES - Claim Status Inquiry and Response
- ePACES - Prior Approval (PA)/Dispensing Validation System (DVS) Request
- ePACES - PA/DVS Response
- ePACES - PA/DVS Revise Cancel Quick Reference Guide
- ePACES - Obtaining a DVS for Durable Medical Equipment (DME)
- ePACES - Obtaining a DVS for Occupational, Physical and Speech Therapy in ePACES
- ePACES - Edit a Claim Function
- ePACES - Electronic Attachments for Dental Prior Approvals
- ePACES - Medicaid Eligibility Verification System (MEVS) Eligibility Request
- ePACES - MEVS Eligibility Response
- ePACES - Enhanced ePACES PA Inquiry
- ePACES - Enrollment
- ePACES - Enrollment Removing and Adding an Electronic/Paper Transmitter Identification Number (ETIN) (Submitter)
- ePACES - Finding, Editing and Deleting Claims
- ePACES - Replicating a Claim for a New Client
- ePACES - Support Files Provider, Other Payer and Submitter
- ePACES - Setting Up User Accounts
- ePACES - Voiding and Replacing Claims
- ePACES - Eligibility Request for School Supportive Health Services Program (SSHSP) and Voluntary Foster Care Agencies (VFCA) Providers
- ePACES - Out of State (OOS) Skilled Nursing Facility PA Requests/Responses
Questions
ePACES enrollment questions should be directed to the eMedNY Call Center at (800) 343-9000.
Expanded Reimbursement for Adverse Childhood Experiences Screening
This update expands the screening coverage previously published in the Reimbursement for Adverse Childhood Experiences Screening article published in the December 2023 issue of the Medicaid Update. Effective October 1, 2024, for New York State (NYS) Medicaid fee-for-service (FFS), and effective January 1, 2025, for Medicaid Managed Care (MMC), NYS Medicaid is expanding previously issued coverage for Adverse Childhood Experiences (ACEs) screening conducted in primary care settings for children and adolescents up to 21 years of age. This expansion includes adults, 21 years of age to 65 years of age. For adults, 21 years of age to 65 years of age, the screening is limited to once per lifetime. Please note: An annual ACEs screening will continue to be covered for children and adolescents up to 21 years of age, as determined appropriate and medically necessary.
ACEs are strongly related to brain development and a wide range of health problems throughout the lifetime of an individual. ACEs have been associated with chronic conditions in adulthood, such as obesity, cancer, depression, substance misuse as well as early mortality.
NYS Medicaid recommends integrating Positive Childhood Experiences (PCEs)/protective factors into ACEs screening for children and adults. PCEs are protective factors and can mitigate ACEs and promote resiliency. A critically important component of screening includes conversations with the NYS Medicaid member and their caregiver(s) to identify PCEs that can build resilience. PCEs include growing up with the support of adults (e.g., caregiver and/or other adults), at least one good friend, as well as a positive, predictable quality of life in childhood.
ACEs are categorized into three experience groups: abuse, neglect, and household challenges. These include emotional, physical, and sexual abuse; emotional and physical neglect; and household challenges that include a history of exposure to domestic violence, a family member with household substance use disorder, a family member with mental illness, an incarcerated household member, and/or parental separation or divorce.
ACEs screening should take place in the context of trauma-informed care to ensure a safe, empowering environment for the individual. According to Centers for Disease Control and Prevention (CDC) analysis, significant trauma is associated with substantial mental, physical, and social illness and disease. Trauma-informed care enables responsiveness to a history of specific ACEs of the individual by making the appropriate referrals to clinical services, such as mental health counseling, substance use treatment and care for social needs. Screening for ACEs is always voluntary, to minimize the risk of retraumatizing the individual. Parents/caregivers should complete the ACEs screening on behalf of children under 13 years of age.
Screening for ACEs can benefit adult patients by:
- improving clinical assessment, patient education, and treatment planning for chronic health conditions;
- helping providers and patients address behavioral pathways that lead to ACE-related health conditions; and
- validating and empowering patients, especially those who are pregnant or already parents, which may reduce intergenerational transmission of trauma and contribute to improved family health.
Eligible providers are licensed or unlicensed individuals under the supervision of a licensed provider, with training and experience using the screening tools and delivery of trauma-informed care. Providers conducting the screening must use a research-based screening tool to assess the history of exposure to adversity and factors that influence risk for associated negative outcomes of the individual. Providers and practice sites should consider which screening/assessment tool to use, who should administer the tool and how, and which NYS Medicaid members should be screened. NYS Medicaid also recommends integrating screening for protective factors as a component of ACEs screening. Suggested screening tools and guidance are shown below.
Specific ACEs do not need to be recorded; however, identification of the screening tool and positive or negative result must be documented. Following administration, the provider reviews the screen results along with the patient and parent/caregiver history. If the screen is determined to be positive for ACEs, based on provider discretion, the provider must consider the factors that influence the risk of the patient for associated negative outcomes, along with PCEs, and develop a treatment plan in partnership with the patient or parent/caregiver. Medical practices should ensure that they have the capacity to evaluate and treat children and adults who screen positive for ACEs before implementing standardized screening. Providers are expected to make referrals to appropriate resources, such as mental health providers or community-based organizations, for any needs identified or requested as the result of the screening.
ACEs Screening Tool Examples
Use of a research-based tool is required when screening for ACEs to be eligible for NYS Medicaid reimbursement. Health care practices should adopt the tool that meets the needs of their population and clinical workflow. Examples of recommended screening tools include:
- Modified ACEs questionnaire based on the original Centers for Disease Control and Prevention (CDC)-Kaiser Permanente ACEs study:
- Center for Health Care Strategies, Inc. (CHCH) Screening for Adverse Childhood Experiences and Trauma document
- ACEs Aware "Screening Tools" web page
- Part 1 of the Pediatric ACEs and Related Life Events Screener (PEARLS) - Child, intended for individuals zero years of age to 19 years of age, to be completed by the parent/caregiver or by the youth, based on the age of the patient.
- Adverse Childhood Experiences Questionnaire for Adults, intended for individuals 18 years of age to 65 years of age, to be completed by the patient.
- Behavioral Risk Factor Surveillance System (BRFSS) Adverse Childhood Experience (ACE) Module, intended for individuals 18 years of age to 65 years of age.
Billing
NYS Medicaid FFS:
- The supervising licensed provider or billing provider must be enrolled as a NYS Medicaid provider and obtain a National Provider Identifier (NPI).
- ACEs screening is reimbursed one time annually for NYS Medicaid members from birth up to 21 years of age.
- ACEs screening is reimbursed once per lifetime for NYS Medicaid members from 21 years of age to 65 years of age.
- Approved categories of service (COS) and providers:
- Physicians ("0460")
- Nurse Practitioners (NPs) ("0469")
- Ordered Ambulatory:
- Clinic ("0163")
- Hospital Outpatient Department (HOPD) ("0282")
- ACEs screening is included within the Prospective Payment System (PPS) primary care rate for Federally Qualified Health Centers (FQHCs).
- The U1 and U9 modifiers must appear consecutively, in this order on the claim line to identify the screening was performed as part of the ACEs screening.
| HCPCS Procedure Code | Modifiers | Description | Annual Allowance Per NYS Medicaid Member |
Reimbursement Rate |
|---|---|---|---|---|
| G9919 | U1 and U9 | ACEs screening was performed, and positive*, provision of recommendations is used for high-risk patients. | One annual screen for children and adolescents up to 21 years of age. One lifetime screen for adults 21 years of age to 65 years of age. |
$29.00 |
| G9920 | ACEs screening was performed and negative. |
*Clinician to determine if an ACEs screen is positive.
MMC Considerations
The billing instructions and fees listed in the chart are specific to NYS Medicaid FFS. For individuals enrolled in MMC, providers should refer to the MMC Plan of the enrollee for implementation details, reimbursement fees, and billing instructions.
Additional Resources:
- NYS Office of Children and Family Services (OCFS) "Adverse Childhood Experiences (ACEs)" web page
- CDC "About Adverse Childhood Experiences" web page
- CDC 2022 BRFSS Questionnaire (module 15, pages 95 through 98)
- ACEs Aware "Screening Tools" web page
- Project TEACH (Training and Education for the Advancement of Children's Health) is a statewide program that supports reproductive, primary care, and pediatric clinicians to deliver quality mental health care in NYS. Project TEACH strives to strengthen and support the delivery of care to children, families, and individuals who experience mental health concerns. Education, resources, and primary care provider consultations with child, adolescent, and maternal psychiatrists are available through the program.
- Project TEACH "About" web page
- Project TEACH "Provider Resources" web page
- For consultations with a child, adolescent, or maternal psychiatrist, providers should contact (855) 227-7272.
- Medicaid Update articles:
- Project TEACH Maternal Mental Health Services article published in the January 2023 issue of the Medicaid Update; and
- Understanding How Adverse Childhood Experiences Affect Patients' Health Across the Lifespan article published in November 2022 issue of the Medicaid Update.
Questions and Additional Information:
- NYS Medicaid FFS claim questions should be directed to the eMedNY Call Center at (800) 343-9000.
- NYS Medicaid FFS coverage and policy questions should be directed to the Office of Health Insurance Programs (OHIP) Division of Program Development and Management (DPDM) by telephone at (518) 473-2160 or by email at FFSMedicaidPolicy@health.ny.gov.
- MMC reimbursement, billing, and/or documentation requirement questions should be directed to the MMC Plan(s) of the enrollee. MMC Plan contact information can be found in the eMedNY New York State Medicaid Program Information for All Providers - Managed Care Information document.
Reminder: Sign Up for eMedNY Training Webinars
eMedNY offers various types of training webinars for providers and their billing staff, which can be accessed via computer and telephone (no travel is necessary). Valuable provider webinars offered include:
- ePACES for: Doula, Dental, Durable Medical Equipment Supplier (DME), Free-Standing and Hospital-Based Clinics, Institutional, Physician, Private Duty Nursing (PDN), Professional Real Time, Transportation and Vision.
- ePACES Dispensing Validation System (DVS) for DME
- eMedNY Website Review
- Medicaid Eligibility Verification System (MEVS)
- Medicaid Revalidation
- New Provider / New Biller
- Pharmacy - New Provider / New Biller
- Provider Enrollment Maintenance Portal - Practitioner
Webinar registration is fast and easy. To register and view the list of topics, descriptions and available session dates, providers should visit the eMedNY "Provider Training" web page. Providers are reminded to review the webinar descriptions carefully to identify the webinar(s) appropriate for their specific training needs.
Questions
Questions regarding training webinars should be directed to the eMedNY Call Center at (800) 343-9000.
Update to Medicaid Provider Enrollment Revalidation Requirement
In accordance with federal requirements, the revalidation process that was suspended during the public health emergency (PHE) was restarted. Revalidation dates that are published on the Medicaid Enrolled Provider Listing, and those appearing on provider files are estimated dates that may be subject to change based on factors such as a timing lag, updates made to an enrollment file, and the ability of New York State (NYS) to extend the revalidation date for certain providers. When required to revalidate, notification will always be mailed to the correspondence address of the provider that is on file, providing sufficient time to act. Therefore, providers are asked NOT to submit a revalidation package until notified to do so, as this can cause confusion and delays in processing all application types.
Once a revalidation has been submitted, eMedNY or NYS Department of Health (DOH) will contact the provider if more information is needed. Otherwise, nothing more is needed from the provider. Upon successful processing of the revalidation, the provider will be sent notification of such. Providers can continue to submit claims while the revalidation is awaiting processing.
Providers must ensure their enrollment file is kept up to date to receive important notifications about their enrollment. If an address update is needed, most practitioners can complete that update quickly and easily on the eMedNY "Provider Enrollment Maintenance Portal for Practitioners" web page. All other provider types should complete a Change of Address Form, provided on the eMedNY "Change of Address for Enrolled Providers" web page. Providers are asked to mail the form to eMedNY for processing. To determine if the provider type can submit transactions via the Maintenance Portal, providers should use the eMedNY "Provider Enrollment Portal COS/FORM Look Up Tool" web page.
Questions
Questions regarding the revalidation process should be directed to eMedNY Call Center at (800) 343-9000.
Medication Synchronization Program Implementation
Effective October 1, 2024, NYRx, the New York State (NYS) Medicaid Pharmacy program, accommodates a point-of-service (POS) indicator when refilling prescriptions for the purpose of Medication Synchronization. The Medication Synchronization program is designed to streamline the medication management process for NYS Medicaid members. Medication synchronization is intended to improve adherence to medication regimens by aligning prescription refills, so that maintenance medications and non-controlled substances are filled on the same day each month.
Medication Synchronization Program Overview
The Medication Synchronization program allows for the synchronization of multiple prescriptions, enabling patients to pick up their medications on a single day each month. This is particularly beneficial for patients who manage multiple conditions, reducing the number of trips to the pharmacy and improving adherence. Pharmacy providers should work with practitioners and patients to determine an effective begin date, to minimize excess supply.
Eligibility
The Medication Synchronization program should target patients in need of medication management of maintenance medications, with the same day supply. Controlled substances and medications when used for acute or short-term therapies, are ineligible for the Medication Synchronization program. Professional judgement should be utilized when determining a synchronization date, to limit excess supplies of medication. Per the NYS Department of Health NYRx the NY Medicaid Pharmacy Program - Pharmacy Manual Policy Guidelines, medication synchronization refills are not eligible for automatic refill.
Claim Submission
To facilitate this synchronization process, pharmacy providers should utilize value "61" (Synchronization Fill) in NCPDP field 420-DK (Submission Clarification Code) when processing claims for maintenance medications and non-controlled substances. This override will help align the dispensing of medications to the same refill date, making it easier for patients to manage their prescriptions. Pharmacy providers should be advised that the use of NCPDP field 420-DK (Submission Clarification Code) is subject to audit.
Limitation
All NYS Medicaid beneficiaries are eligible for one synchronization of a specific maintenance medication, per calendar year. This can be systematically applied by utilizing the claim submission process, as described above.
Questions and Additional Information:
- Claim processing questions should be directed to the eMedNY Call Center at (800-343-9000.
- NYRx coverage and policy questions should be directed to the Medicaid Pharmacy Unit by telephone at (518) 486-3209 or by email at NYRx@health.ny.gov.
Vaccine Billing Update for Pharmacies: Notice of Upcoming Transition
NYRx, the Medicaid Pharmacy program, will expand vaccine billing procedures during the 2024-25 flu season. This change includes the ability to bill by National Drug Code (NDC) for pharmacy categories of service (COS) "0441" and "0442", transitioning from the use of Current Procedural Terminology (CPT) and Healthcare Common Procedure Coding System (HCPCS) procedure codes.
How Transition Affects Pharmacy Providers
Billing Transition:
- All vaccine claims, when administered in pharmacy settings, will now utilize NDCs in addition to accommodating a single transaction to include administration fee. This change is in compliance with industry standards and new initiatives to modernize the billing process and enhance accuracy in vaccine administration record-keeping.
- Current billing procedures will be kept in place temporarily.
Understanding NDCs:
- NDCs are unique identifiers assigned to medications, including vaccines, that provide specific information about the product, such as the manufacturer, strength, and dosage form. This change will improve the ability to track vaccine distribution and utilization more effectively.
- Utilization of NDC for vaccine billing will standardize reimbursement rates, ensuring up-to-date fees.
Impacted Vaccines
This transition will apply to all pharmacist-administered vaccines. Additional detail can be found in the guides located on the NYS DOH "Pharmacists as Immunizers" web page. Current procedures for all other providers times will be unaffected.
Next Steps
NYRx is committed to making this transition as smooth as possible. To prepare for the update, NYRx encourages providers to review their software needs to accommodate the following NCPDP fields:
- All Pharmacy Providers: Use of NCPDP field 438-E3 (Incentive Amount Submitted) will be utilized for administration fees.
- Vaccines for Children (VFC)-Pharmacy Providers: Utilization of NCPDP field 423-DN: (Utilization of Basis of Cost Determination) value "15" (Free product or no associated cost).
Additional details will be made available in the coming weeks.
Questions and Additional Information
For questions and additional information regarding this policy, providers should contact NYRx by email at NYRx@health.ny.gov or by telephone at (518) 486-3209.
Reminder: NYRx Allows 90-Day Prescribing for Most Maintenance Medications and Over the Counter Drugs
NYRx, the Medicaid Pharmacy program, would like to remind stakeholders, including prescribers, pharmacies, NYS Medicaid members, and caregivers that 90-day supplies of most maintenance medications and over the counter (OTC) drugs are covered by NYRx. This benefit applies, but is not limited to, medications prescribed to treat hypertension, diabetes, cholesterol, depression, mild pain, asthma, and chronic obstructive pulmonary disease (COPD).
Ninety-day supplies offer numerous benefits:
- Patient benefits - Cost savings with fewer copays, convenience of fewer trips to the pharmacy, improved medication adherence, and reduced risk of missing refills.
- Prescriber benefits - Increased patient adherence equals easier monitoring, reduced administrative burden, increased patient satisfaction, and a more streamlined process for chronic disease management.
- Pharmacy benefits - Increased patient adherence, improved operational efficiency leading to more time for additional services such as immunizations, medication therapy management (MTM), and enhanced customer satisfaction, resulting in a stronger patient-pharmacy relationship.
Prescribers should consider writing for a 90-day supply and pharmacies should work with prescribers to switch to a 90-day supply once it is determined the patient is on a stable dose of a maintenance medication or OTC drug.
Questions and Additional Information
For questions and additional information regarding this policy, providers and prescribers should contact NYRx by email at NYRx@health.ny.gov or by telephone at (518) 486-3209.
NYRx, the Medicaid Pharmacy Program, Clinical Call Center Name Change
Effective October 1, 2024, Magellan Medicaid Administration, LLC. changed its name to Prime Therapeutics State Government Solutions, LLC. The vendor will continue to operate as the clinical call center for NYRx, the New York State (NYS) Medicaid Pharmacy program. The clinical call center handles all pharmacy prior authorization (PA) requests from NYS Medicaid providers. There are no changes to procedural operations or services provided.
The clinical call center hours and contact information remains the same. NYS Medicaid providers can continue to contact the clinical call center at (877) 309-9493 or visit the Magellan Medicaid Administration, LLC. "NYRx, the Medicaid Pharmacy Program" homepage. The clinical call center is available 24 hours per day, seven days per week. NYRx is updating the NYS Department of Health (DOH) web pages and resources to reflect the name change.
Questions
Questions regarding this change should be directed to the NYRx at NYRx@health.ny.gov.
Kathy Hochul
Governor
State of New York
James McDonald, M.D., M.P.H.
Commissioner
New York State Department of Health
Amir Bassiri
Medicaid Director
Office of Health Insurance Programs
The Medicaid Update is a monthly publication of the New York State Department of Health.