Redesign Medicaid in New York State
Medicaid Redesign Team Update and Next Steps
- Update and Next Steps is also available in Portable Document Format (PDF, 842KB)
Significant Progress, Lots Still to Be Done
July 10, 2013
United Hospital Fund
Jason A. Helgerson, Medicaid Director
NYS Department of Health
Agenda
- MRT Implementation to Date
- Lowering Costs
- Improving Quality
- Looking Ahead to 2014 - Major Implementations
- Major Outstanding Policy Questions
- Q & A
MRT Implementation to Date
Are We Lowering Costs and Improving Outcomes?
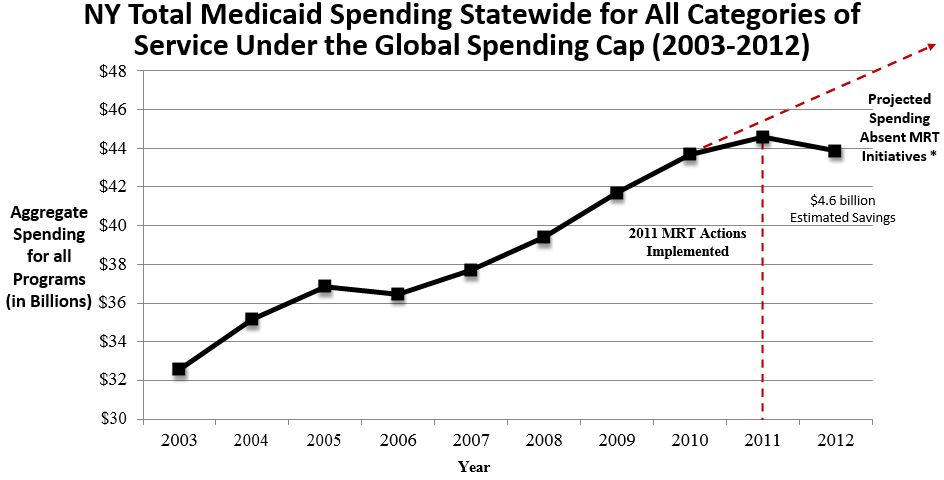
The MRT is Bending the Cost Curve
- Lowered total Medicaid spending by $4 billion in Year 1.
- Lived within the Global Spending Cap for two full years.
- Finished Year Two $200 million under the Global Spending Cap.
- Thanks to the MRT the state was able to absorb a $1.1 billion federal revenue loss due to a change in Medicaid financing for DD services.
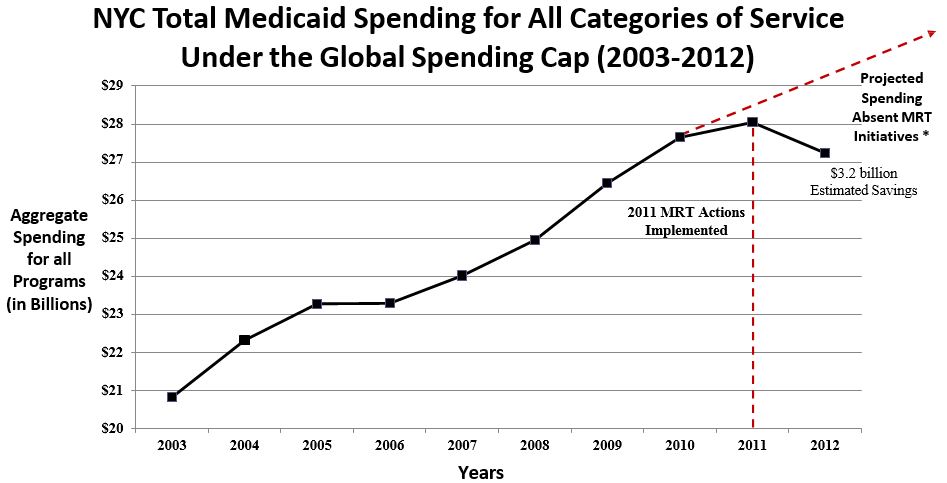
- Savings has been especially significant in New York City.
| 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | |
|---|---|---|---|---|---|---|---|---|---|---|
| # of Recipients | 4,266,535 | 4,593,566 | 4,732,563 | 4,729,166 | 4,621,909 | 4,656,354 | 4,910,511 | 5,211,511 | 5,396,521 | 5,578,143 |
| Cost per Recipient | $7,635 | $7,658 | $7,787 | $7,710 | $8,158 | $8,464 | $8,493 | $8,379 | $8,261 | $7,864 |
*Projected Spending Absent MRT Initiatives was derived by using the average annual growth rate between 2003 and 2010 of 4.28%.
| 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | |
|---|---|---|---|---|---|---|---|---|---|---|
| # of Recipients | 2,815,890 | 3,014,656 | 3,114,104 | 3,145,267 | 3,077,097 | 3,072,893 | 3,197,304 | 3,351,189 | 3,427,870 | 3,487,966 |
| Cost per Recipient | $7,397 | $7,406 | $7,477 | $7,406 | $7,807 | $8,121 | $8,272 | $8,251 | $8,183 | $7,810 |
* Projected Spending Absent MRT Initiatives was derived by using the average annual growth rate between 2003 and 2010 of 4.1%.
| 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | |
|---|---|---|---|---|---|---|---|---|---|---|
| # of Recipients | 181,960 | 181,971 | 183,181 | 185,591 | 185,409 | 185,067 | 188,207 | 192,207 | 194,912 | 193,062 |
| Cost per Recipient | $34,438 | $36,726 | $38,933 | $40,732 | $42,700 | $43,841 | $43,867 | $43,977 | $43,363 | $42,629 |
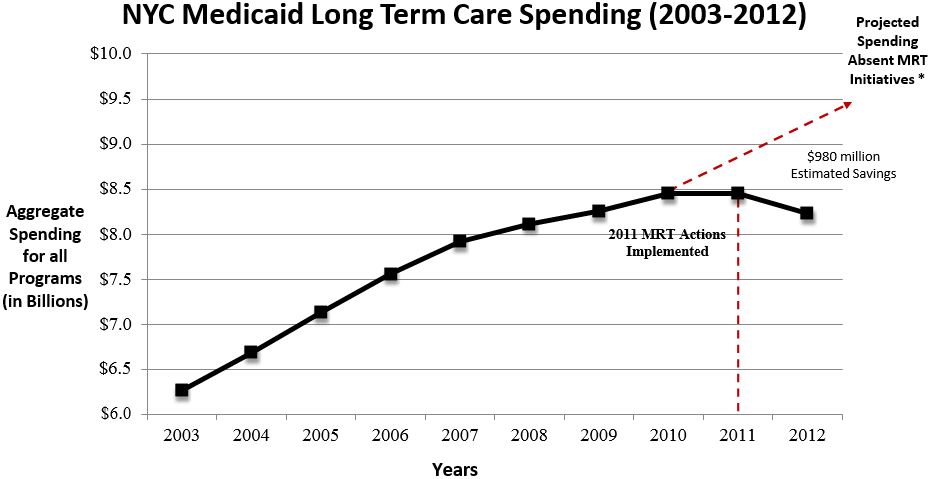
* Projected Spending Absent MRT Initiatives was derived by using the average annual growth rate between 2003 and 2010 of 4.4%.
MRT is Improving Patient Outcomes
NYS Managed Care Plans #2 in the Nation
Example #1
- National Committee for Quality Assurance (NCQA) analyzed New York´s Medicaid health care plans against 76 different quality measures.
- NYS plans are especially successful when it comes to offering the right type of care for common, costly diseases, for example:
- Diabetes;
- Childhood obesity;
- Smoking cessation;
- Follow-up care for the mentally ill.
- NCQA found that New York is a national leader, second only to Massachusetts.
Source: NCQA: http://www.ncqa.org/Newsroom/NYStateofHealthCare.aspx
Managed Long Term Care Improving Patient Outcomes
Example #2
- MRT 90, Mandatory Enrollment in MLTC Plans: Expands MLTC for Medicaid members who are also eligible for Medicare (dual eligibles) and currently receiving community-based long term care services.
- Benefit package includes home care, personal care, social supports, and transportation services. The costs of skilled nursing facility services are included in the capitation payment, providing a financial incentive for the plans to keep their members healthy and living in the community.
- MLTC enrollment has steadily increased over the past couple years:
- Enrollment has increased from approximately 10,000 in 2004 to nearly more than 100,00 as of May 2013;
- Number of plans has grown from 16 plans to more than 40 plans.
- MLTC is improving outcomes and the feedback is favorable.
- The New York State Department of Health 2012 Managed Long Term Care (MLTC) Report found that:
- the overall functional ability of 90 percent of MLTC enrollees has remained stable or improved;
- 85 percent of MLTC plan members rated their health plan as "good" or "excellent";
- 91 percent would recommend their plan to a friend, and
- Less than 2 percent of members are in nursing homes.
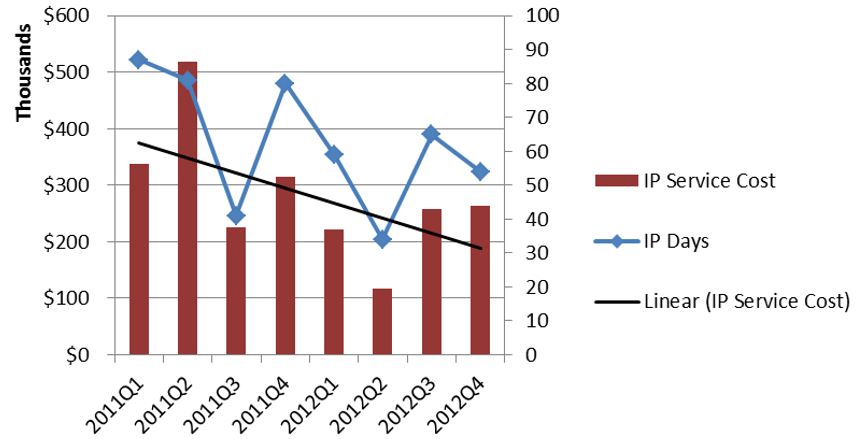
Health Homes Are Reducing Inpatient Utilization & ER Use
Example #3
- Health Homes are in their early days.
- Patients with little or no historic connection to traditional health care are benefiting the most.
- Preliminary results are for Phase 1 and Phase 2 counties.
Inpatient Service Cost for a Subset of Health Home Enrolled Members
Inpatient Services Utilization and Spending Dropping for Health Home Enrolled *
ER Service Cost for a Subset of Health Home Enrolled Members
Emergency Room Utilization and Spending Dropping for Health Home Enrolled *

* Includes individuals continuously enrolled in Medicaid with no case management services in calendar 2011 who enrolled in Health Home Services in the first six months of 2012. N = 194 individuals.
Looking Ahead to 2014: Major Implementations
Significant Implementations
- Affordable Care Act
- MRT Waiver Amendment
- FIDA Demonstration
- Behavioral Health Carve-in/HARP
Affordable Care Act (ACA)
ACA Implementation & Medicaid Administration Reform
- The Affordable Care Act (ACA) is a tremendous opportunity for New York State:
- 1 million New Yorkers will gain access to health insurance;
- Additional federal financing for Medicaid will help ensure program sustainability;
- Building a new health insurance exchange will allow the state to phase-out the out-of-date WMS eligibility system.
- New York will operate its own exchange and will use the launch of the exchange to also facilitate the state takeover of Medicaid administration from counties.
- State take-over will provide counties with mandate relief and create greater consistency in customer treatment across the state.
- Full state takeover will take five years to implement.
- Standing up the exchange by October 1, 2013 is a major challenge for DOH and our partners. Lots of work ahead!
MRT Waiver Amendment
MRT Waiver Amendment
- We currently have a waiver amendment pending with CMS that would allow us to reinvest $10 billion in MRT generated federal savings back into New York´s health care delivery system.
- The amendment is essential to both fully implement the MRT action plan as well as prepare for ACA implementation.
- The amendment, which requires federal approval, is a unique opportunity to address the underlying challenges facing NYS health care delivery:
- Lack of primary care;
- Weak health care safety net;
- Health disparities; and
- Transition challenges to managed care.
MRT Waiver Reinvestment Strategies
- Primary Care Expansion ($1.25 billion over the next five years).
- Health Home Development ($525 million over the next five years).
- New Care Models ($375 million over the next five years).
- Expand Vital Access/Safety Net Program ($1.5 billion over the next five years).
- Public Hospital Innovation ($1.5 billion over the next five years).
- Medicaid Supportive Housing ($750 million over the next five years).
- Long Term Transformation - Integration to Managed Care ($839.1 million over the next five years).
- Capital Stabilization for Safety Net Hospitals ($1.7 billion over the next five years).
- Hospital Transition ($520 million over the next five years).
- Ensuring the Health Workforce Meets the Needs in the New Era of Health Care Reform ($500 million over the next five years).
- Public Health Innovation ($395.3 million over the next five years).
- Regional Health Planning ($25 million on average annually over the next five years).
- MRT and Waiver Evaluation Program ($500 million over the next five years).
FIDA Demonstration
FIDA Demonstration
- A key step in the move to "care management for all" is the proposed Fully Integrated Dual Advantage (FIDA) demonstration project.
- Through this effort 170,000 dually eligible members (Medicaid and Medicare) will be enrolled into full-integrated managed care products.
- The enrollment process will rely on a "conversion in place" approach under which duals enrolled in MLTCP plans will see their Medicare benefit added to their managed care plan´s portfolio.
- Members will be able to opt-out of the Medicare managed care product.
Two Types of Plans:
- Primary FIDA - Dual eligibles, age 21 and over that require community-based long term care services for more than 120 days who are not residents of an OMH facility, and who are not receiving services from the OPWDD system.
- Geographic Service Area: Bronx, Kings, New York, Queens, Richmond, Nassau, Suffolk and Westchester Counties
- OPWDD FIDA - Dual eligibles, age 21 and over, who are not residents of an OMH facility, and who are receiving services from the OPWDD system
- Geographic Service Area: Statewide
Proposed Enrollment Process:
- In April 2014, begin accepting voluntary enrollments for individuals in need of community-based long-term care services greater than 120 days.
- In July 2014, begin process of passive enrollment notification for individuals in need of community-based long-term care services greater than 120 days.
- In October 2014, begin accepting voluntary enrollment for dual eligible individuals that have exhausted Medicare benefit in nursing homes.
- In January 2015, begin process of passive enrollment notification for dual eligible individuals that have exhausted Medicare benefit in nursing homes.
- This will be applicable to eligible individuals in the FIDA demonstration area.
- Eligible individuals can opt-out of passive enrollment.
- Enrollment broker will provide enrollment counseling and assistance.
Proposed Covered Benefits:
- NYSDOH is proposing to use the NY Medicaid definition of medical necessity for all services.
- Covered Services include services covered by the existing Medicare and Medicaid programs in New York in addition to Home and Community-Based waiver services.
- FIDA plans will have discretion to supplement covered services with non-covered services or items where so doing would address a Participant´s needs, as specified in the Participant´s Person-Centered Service Plan.
Status Update:
- The FIDA proposal has not yet been approved by CMS.
- NYSDOH is working with CMS on implementation funding for the first two years.
- NYSDOH is concurrently working with CMS on a Memorandum of Understanding (MOU) and anticipates that it will be completed in July 2013.
Behavioral Health Carve-In/ HARP
Behavioral Health Carve-In/ HARP
- Key MRT objective is to more effectively integrate physical and behavioral health services.
- Scope of project is broad with collaboration between and among DOH, OMH, OASAS, OCFS, NYC, stakeholders and local governmental units.
- Approximately 695,000 members impacted.
- $7B in Spend moved into Managed Care.
- Transition of BH Services will include BH State Plan Services, and specialized community-based services including Peer Support, Respite, Crisis and Employment.
- MRT guiding principles of the BH Design include:
- Person-Centered Care Management through Health Homes where eligible.
- Patient/Consumer Choice.
- Savings from unnecessary inpatient services will be reinvested into BH ambulatory and other community-based services
- Tracking of BH and Physical Health (PH) spending, and reinvestment of savings from unnecessary inpatient care into BH ambulatory and other community-based services.
- Address Unique needs of Children and Families.
- Center of Excellence Guidelines.
New York´s Design for Managed Behavioral Health for Adults (21 and older)
- Behavioral Health will be managed by:
- Special Needs Health and Recovery Plans (HARPs) for individuals with significant behavioral needs.
- Mainstream Managed Care Plans.
- Plans may operate services directly only if they meet rigorous standards.
- Plans that do not meet rigorous standards must partner with a BHO which meets standards.
- Children´s design is still under development.
MRT BHO/HARP Timeline
| MRT Milestone | Adult (NYC) | Adult (Rest of State) | Kids |
|---|---|---|---|
| Finalize program design | Spring 2013 | Spring 2013 | |
| Finalize BHO/HARP/MCO managed care contract requirements | Summer 2013 | Summer 2013 | |
| Post procurement on website for at least 30 days | Late Summer 2013 | Winter 2014 | |
| Select HARPs and Qualify Plans/BHOs for mainstream benefits | Winter 2013 | Summer 2014 | |
| Plans fully operational | Spring 2014 | Fall 2014 | Spring 2015 |
Major Outstanding Policy Questions
Question #1: How will the state share MRT savings with providers?
- MRT is beginning to really bend the cost curve.
- To many providers - Medicaid payments = Vital revenue.
- MRT created some mechanisms for sharing savings but as savings grow new, more systematic methods will be necessary.
Option #1: "Global" Shared Savings
- State captures shared savings by lowering managed care payments as costs decline.
- State then devises mechanisms to make either direct payments to providers or to require payments through managed care plans.
- Payments could be linked to both performance measures and to ensuring financial survival for vital access providers.
Option #2: Managed Care Shared Savings
- Require managed care organizations to develop plans for shared savings with their provider networks.
- The state would approve all plan shared savings agreements and ensure those agreements are enforced.
- Plans would be free to use "back end" shared savings agreements, sub-capitation and performance bonus payments as vehicles for sharing savings with providers.
- Model may be tested in the FIDA demonstration.
Question #2: How should Medicaid partner with the Exchange in health care purchasing?
- ACA implementation is a great opportunity to align incentives in public health care purchasing.
- Once the Exchange is "live" and stable DOH will look for ways to align payment policies so as to encourage better alignment of incentives in the delivery system.
- While this is a great opportunity the state will need to move forward carefully especially during the early years of the Exchange.
- In addition to the Exchange the state will need to look at additional partnerships with other payers across the state to see what kinds of multi-payer reform efforts are possible.
Question #3: How can Medicaid leverage advances in HIT to improve outcomes and lower costs?
- Universal adoption of electronic health records and the All Payers Claims Database create an opportunity for Medicaid to move performance measurement beyond the traditional HEDIS measures.
- If the state can collect population-wide health and public health outcome measures we have an opportunity to really focus plans on improving the overall health of the Medicaid population.
- This evolution will be especially important as more populations are added to Medicaid managed care over the next several years.
Questions?
Contact Information
We want to hear from you!
MRT website:
mrtwaiver@health.health.ny.gov
Subscribe to our listserv:
http://www.health.ny.gov/health_care/medicaid/redesign/listserv.htm
´Like´ the MRT on Facebook:
http://www.facebook.com/NewYorkMRT
Follow the MRT on Twitter:
@NewYorkMRT
Follow Us