Written comment submitted pre and post meeting
- Comments is also available in Portable Document Format (PDF)
Alliance
FOR BETTER HEALTH
June 19, 2018
Subject: 1115 Public Forum Comment
Submitted to the Department of Health
Brooke McConnell
Vice President, Community Relations & Strategy Alliance for Better Health
Thank you for the opportunity to provide feedback on New York´ s 1115 waiver program.
Alliance for Better Health Background
Alliance for Better Health Participating Performance System (PPS) was established to participate in New York St at e´ s Delivery System Reform Incentive Payment (DSRIP) program. We serve over 190,000 Medicaid and uninsured members across Albany, Fulton, Montgomery, Rensselaer, Schenectady, and Saratoga counties. We drive a dynamic collaborative of over 2,000 providers and Community–Based Organizations (CBO).
Commitment to Health Equity
Our vision is health equity. We are driving toward a united and collaborative care delivery community, transforming care to improve the health of the most underserved.
Comments on Future of NYS 1115 Waiver Program
We believe there is an opportunity for NY State to build on the pioneering PPS work to date. PPS activities have served as the foundation for collaboration. Alliance is exploring a sustainability plan to continue our community–based efforts and transition to a business model that integrates social services and social determinant agencies with traditional medical models. Short –term objectives will focus on infrastructure that strengthens t h e CBO network. Our long term vision is to establish a foundation of activities to pursue risk–sharing or other value–based payment agreements and develop services that are responsive to neighborhood –level needs.
DOH should continue encouraging community–based services and social determinants of health use. Funding should pass–through to providers and agencies engaging in these activities.
It is imperative that DOH establish a nimble regulatory structure to support innovation in health delivery. There needs to be a mechanism to align regulatory relief and modernization that enables services, integration, and convergence across all silos.
We also believe workforce development and training must be prioritized as the State pursues delivery transformation and policy efforts. Needs extend beyond traditional care models and require s efforts that teach clinicians and direct care workforce about population health and social determinants. Regulatory flexibility and barriers to sharing staff in areas of workforce short ages should also be explored.
You have our commitment to work with you in the continued design of groundbreaking programs here in our region and across the state.
Thank you for your consideration.
403 Fulton St 2nd fl.
Troy, NY 12180
518.701.2200
www.abhealth.us
From: John Harper
Sent: Sunday, June 17, 2018 10:31 AM
To: doh.sm.1115Waivers <1115waivers@health.ny.gov>
Subject: Public Comment
COMMENT FOR 1115 WAIVER: IT IS CRITICAL TO STAND IN OPPOSITION TO THE TRUMP ADMINISTRATION´S REVISED CRITERIA TO IMPOSE WORK REQUIREMENTS AS A CONDITION OF ELIGIBILITY FOR MEDICAID RECIPIENTS EVEN UNDER THE GUISE OF "COMMUNITY ENGAGEMENT" FOR THE FOLLOWING REASONS:
>Medicaid should be seen as a health care benefit. Tying eligibility to work or Community Engagement requirements does not necessarily promote health.
>Working at minimum wage could make some people financially ineligible for Medicaid.
>Work requirements would require paying for the staff and systems to track work verification and exemptions.
>Because of complex documentation and administrative processes, some eligible individuals could lose coverage. There is a real risk of eligible people losing coverage due to their inability to navigate these processes, miscommunication, or other breakdowns in the administrative process. People with disabilities may have challenges navigating the system to obtain an exemption for which they qualify and end up losing coverage.
>Increased documentation requirements shift Medicaid from a health insurance program for low–income individuals and families back to one that operates under welfare rules. CMS´s work requirement waiver guidance explicitly supports alignment of Medicaid with SNAP or TANF welfare reporting and policies.
>The CMS guidance is explicit that states will be required to describe strategies to assist beneficiaries in meeting work requirements but may not use federal Medicaid funds for supportive services to help people overcome barriers to work.
John Harper SYSTEMS ADVOCATE INDEPENDENT LIVING INC.
441 WEST MAIN STREET
MIDDLETOWN, NEW YORK 10940
From: Cole, Michael
Sent: Monday, June 18, 2018 12:45 PM
To: doh.sm.1115Waivers <1115waivers@health.ny.gov>
Subject: Comments
I offer my comments from the perspective of a behavioral health provider and an Article 41 LGU DCS. Many positive changes have occurred since the launch of these initiatives. Behavioral health has reached out beyond its service silos to a greater extent than before, has an evolving understanding of both the volume vs value based models of payment, and the need for all partners to thrive for any one provider to thrive (both related to improved population health and Medicaid sustainability.
A few comments. concerns to consider as we move further along:
- The perception persists that DSRIP funding is a hospital bail out– with the "fox minding the hen house". If our aim is to bolster existing CBOs capacity rather that creating new community service capacity based out of the large hospital systems, DSRIP is not effective. The cost curve can most effectively be "bent", by increasing the EHR, CQI, Medicaid billing and inter‐operability capacity of the existing small and mid–size non‐hospital CBOs.
- Coordination will need to be mandated among PPSs sharing a geographic and between those PPSs and the emerging BHCCs
- Standardization of software is needed.
- Recognition that the data entry demands (though well intended) are significantly reducing face to face time with our consumers.
Thank you,
Michael Cole
––
Michael W. Cole, LCSW
Director of Community Services
325 Columbia Street, Suite 300
Hudson, NY 12534
Helping Columbia County Residents Find Hope & Healing For Over 50 Years
Columbia County Mental Health has many support services at multiple locations with flexible hours.
Crisis services available daily and
Open Access Mon–Thurs 9am – 11am
at 325 Columbia Street in Hudson
Reach us at 518–828–9446
columbiacountymhc.com
or
Facebook
Healing Starts Here
From: Duffy, Christine
Sent: Tuesday, June 19, 2018 3:27 PM
To: doh.sm.1115Waivers <1115waivers@health.ny.gov>
Cc: Toto, Danielle; Fardella–Roveto, Elvira
Subject: 1115 Public Comment Forum
Per request for comments regarding the services to be provided under the new 1115 Waiver, please see attached, Request for Policy Consideration, pertaining to HCBS Palliative Care Services.
Thank you for any feedback you can provide.
Christine Duffy
Project Manager, Strategic Initiatives
St. Mary´s Healthcare System for Children
5 Dakota Drive, Suite 200
New Hyde Park, NY 11042
CONFIDENTIALITY NOTICE: This message and any attachments are solely for the intended recipient and may contain confidential information which is, or may be, legally privileged or otherwise protected by law from further disclosure. If you are not the intended recipient, any disclosure, copying, use or distribution of the information included in this email and any attachments is prohibited. If you have received this communication in error, please notify the sender via email, telephone or fax and immediately and permanently delete any copies of this email and any attachments.
St Mary´s Kids
Where big hearts help little patients
Statement of Issue
St. Mary´s Home Care was thrilled to receive designation as a Community Palliative Care Provider under the new HCBS waiver effective January 1, 2019. St. Mary´s has a long history of palliative care dating back to 1980. As New York´s largest and most experienced care provider for children with medical complexity, St. Mary´s wants to be there for our children and their families in any circumstance,
However, while we are very thankful for the opportunity that the HCBS waiver provides, we submit this letter in the hopes of resolving our concerns pertaining to the service rates that were published and released after we had submitted our application.
The draft rates proposed for downstate services and published on the DOH website are as follows:
| Service Offered | Downstate Rate |
|---|---|
| Bereavement Services | $47.66 |
| Massage Therapy | $57.29 |
| Expressive (Art, Play, Music) Therapy | $39.04 |
We were disappointed to learn that the rates forth above professional services were so low. They are insufficient compared to the rates currently paid for similar professional services offered by Certified Home Health Agencies. For example, a Professional Social Work visit conducted by St. Mary´s Home Care is reimbursed between $110 and $150 per visit, versus the $47.66 reimbursement given through the HBCS waiver.
ln addition; two other provisions of the waiver concern us. The first is the level of staff qualification required, which we feel may limit our efforts to find employees already trained in both palliative care and the medically fragile population. The second is the limitation on visits per patient that we can provide, which we worry may prove insufficient due to the medically complex nature of our children.
The Need for Palliative Care
- The Center to Advance Palliative Care, a reputable nationwide resource for the development and promotion of palliative care, defines palliative care as specialized medical care for people living with serious illness, focused on providing relief from the symptoms and stress of the illness. The majority of our patient population, being medically complex and medically fragile at early ages, can he considered to suffer from such.
- St. Mary´s is New York´s largest provider of pediatric care for the medically complex. Based on home care census data from 6/11/2018, St. Mary´s currently treats 931 patients between the eligible ages of Oto 21 years old. As 55% of New York´s medically fragile population is between ages Oto 21, each new referral stands to expand this population (Simpser, Edwin F et al.).
- Half of the population of medically complex families in the United States have paid out of pocket for health care, cut work hours or stopped working altogether in order to care for their child, and taken on financial problems to ensure their child´s health (Kuo, Dennis z et al.). Since part of palliative care´s role is to provide relief from the stress caused by illness, it can prove integral for families in dire straits.
- ln general, 15% of families with medically complex children have reported the loss of a child (Namkung, Eun Ha et al.). Palliative care´s role in bereavement can help these already stressed families find peace.
- In a study of ten mothers of medically complex children, nine reported signs of post–traumatic stress disorder (Pizur–Bamekow, K).
With these factors in mind, it is clear that the St. Mary´s population is one that is uniquely in need of palliative care. At the rates presented, we worry that we cannot provide the consistency and breadth of Care that these families need. Below is an assessment of risks that we foresee, both from our past experiences in palliative care and from the current state of the healthcare industry.
Risks Within Healthcare
- Our hospital unit has performed palliative care for nearly 40 years and pioneered pediatric palliative care efforts, a sign of both our dedication and the relatively unique niche of pediatric palliative care. This unique niche poses several challenges, as noted below.
- Our previous Community Palliative Care program won a Circle of Life award for innovation and a NYS DOH Recognition Award for best practice, yet still needed to disband due to insufficient grant funding. We do not want to risk the same happening to our patients on the HCBS waiver.
- The families we care for need the stability of care and services. Without sustainable rates, such stability is far less likely to be achieved.
- Below is the average of our contracted rates for physical therapy (a close analog to massage therapy) and social work compared to those provided in the waiver.
Contracted Average Waiver Rates Difference Social Work $111.14 $47.66 $63.48 Physical Therapy $111.83 $57.29 $54.54 - The draft rates proposed for the waivered palliative services are drastically reduced when compared to the established rates currently paid to CHHA therapists and social workers,
- Because of the broad spectrum of medically complex conditions that our patient population has, the length of time that our patients will be in need of our services can vary significantly between patients. Though we strive to make our patients´ need for our services as short–term as possible, each year there will most likely be some percentage of our patients that need palliative care visits beyond the current amount being allotted. We hope to expand the current allotted amount to ensure that this segment of our population is not at risk of being underserved.
Policy Consideration
- Increase reimbursement rates for the services to be provided in order for us to recruit and retain the appropriately credentialed workforce.
- Allow for more flexibility in the requirements for hiring professionals, allowing us to use our education and training expertise along with past palliative care experience.
- Allow for palliative care services to continue on a by–need basis, similar to the medical doctor ordering periods and insurance authorization periods that we currently use for visits.
Conclusion
We feel that these are the best ways of continuing to attract and cultivate the qualified, professional staff required for our palliative care program to thrive. Our population is underserved, medically fragile, and come with the unique challenges that pediatrics poses for palliative care. With appropriate funding and flexibility, we expect St. Mary ´ s will be able to provide palliative services to those on the waiver when they need it most.
Respectfully,
Edwin F. Simpser, Md
President & CEO
Sources
Kuo. Dennis Z., et al. " A National Profile of Caregiver Challenges of More–Complex Children with Special Health Care Needs." Advances in Pediatrics., U.S. National Library of Medicine, Nov. 2011, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3923457/.
Namkung, Eun Ha, et al. "The Relative Risk of Divorce in Parents of Children with Developmental Disabilities: Imp acts of Lifelong Parenting." Advances in Pediatrics., U.S. National Library of Medicine, Nov. 2015, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4624231/.
Pizur–Barnekow, K. "Maternal Health After the Birth of a Medically Complex Infant: Setting the Context for Evaluation of Co–Occupational Performance." American Journal of Occupational Therapy, vol. 64, no. 4, 2010, pp. 642–649., doi:10.5014/ajot.2010.08160.
Simpser, Edwin F, et al. "CHILDREN AND YOUNG ADULTS WITH MEDICAL FRAGILITY: A Population Needs Assessment."
From: Peter Caplan
Sent: Tuesday, June 19, 2018 2:01 PM
To: doh.sm.1115Waivers <1115waivers@health.ny.gov>
Subject: Re: 1115 Public Forum Comment" – telemedicine/telehealth
In the future, why not have a call–in number for those not able to attend in person but would like to ask a question or make a statement
Peter M. Caplan
Managing Consultant eHealth Systems & Solutions
www.pctelemedicine.com
From: Peg Graham
Sent: Friday, June 29, 2018 9:39 AM
To: doh.sm.1115Waivers <1115waivers@health.ny.gov>
Subject: Corrected Public Comment
I noticed a few typos in the comments I submitted yesterday. Please use this corrected version.
Thank you,
Peg Graham, MBA, MPH
CONFIDENTIALITY NOTICE: This e–mail message and any attachments are for the sole use of the intended recipient(s) and may contain confidential and/or privileged information. Unless you are the intended recipient, you are hereby notified that copying, forwarding, printing or otherwise disseminating the information contained in or attached to this e–mail is strictly prohibited. If you are not the intended recipient, please notify the sender by telephone, and immediately and permanently delete and destroy all copies and printouts of this e–mail message and/or attachments.
"1115 Public Forum Comment"
Submitted by Peg Graham, Family Caregiver
In support of a FUNCTIONAL INDEPENDENCE standard New York, New York
June 26, 2018
On behalf of the family caregiver community, this public comment requests NYS to change the standard used to determine coverage of Durable Medical Equipment (DME) by 1115 waiver plans.
As the health system moves towards value–based purchasing arrangements, the rules surrounding procurement of DME continue to be bureaucratically driven, a cost–containment exercise without regard to the negative impact on beneficiaries. (SMD# 17–006 RE: Limit on Federal Financial Participation for Durable Medical Equipment in Medicaid).
We ask NYS to promote insurer coverage of DME that optimizes the capacity of beneficiaries to function at the level of their individual "healthiest self," especially those whose aging includes mobility–related disabilities. Such a "Functional Independence" standard is likely to result in a Return on Investment that aligns with the goals of the 1115 waiver: improving access, quality and cost effectiveness of health services for the poorest and most at risk residents.
EFFECTS OF THE CURRENT "MEDICAL NECESSITY" COVERAGE STANDARD
"[Generally] Medicaid will pay for medical equipment when it is determined to be medically necessary, cost effective and meet their strict definition of what is durable medical equipment. Most states define DME as ´equipment that can withstand repeated use, is primarily used to serve a medical purpose, is appropriate for home use and is not useful to a person without an illness or injury.´ ´Cost–effective´ usually means that Medicaid will pay for the most basic level of equipment only." Source: American Elder Care Research Organization, Paying for Senior Care website
This standard, in place for decades, has led to outdated DME designs that are NOT up to the challenge ahead of NYS: a growing number of aging beneficiaries and a decreasing number of available caregivers. Take a moment to think about what this equipment is used to do:
"The elderly and frail elderly segment of the US population is growing, as is in–home hospice care. Staff work alone and transfer, bathe, and lift patients, often without safe patient handling (SPH) equipment. Home care staff work in an environment that is very unpredictable, and may include pets, clutter, crime, and lack of equipment and patient financial resources. The functional status of a patient can change frequently, and homes, varying from cabins in rural areas without plumbing to luxury high–rise apartments in large cities...
Yet, many acute–care clinicians and prayers continue to think about DME in a very dismissive way, never thinking about whether the "cheapest" model is helping either the care recipient or the caregiver, whether it is the paid workforce or an unpaid family member, to accomplish the mobility and self–care tasks so necessary to someone´s health status.
What is unique for home care is what is not found on a similar list of high risk tasks for hospital and nursing home assistants. Performing care alone when two caregivers are needed, working without lifting equipment and non–height adjustable beds...and working without rest breaks are more unique to home care." SOURCE: Capewell RA "Safe Patient Handling in Home Health Care: A Review of the Literature" Am. J. SPHM, 2011, pp, 25–34
Nowhere does the Medical Necessity standard consider if:
"...the patient will benefit from increased levels of comfort and even a more positive clinical outcome. Assisted and frequent mobility can amount to speedier and more fruitful recovery. The patient can achieve a higher level of fitness, be bathed and washed with ease, experience increased agility through muscle strengthening, increased blood flow and heart strength and an overall improvement in personal dignity.
" SOURCE: Weingarten for Lancman R Wright K Gottfried R "Safe Patient Handling in New York: Short Term Costs Yield Long Term Results," May 2011, pp. 6–7.
We recommend that this sensibility, which drives NYS´ safe patient handling expectations of hospitals and nursing homes, also inform homecare policies in our state.
AVOIDABLE INJURIES
In addition, the continued application of a Medical Necessity standard reflects an apparent acceptance of a high rate of injury among paid home health workers and family caregivers.
"Caregiving tasks such as transfers, lifts, bathing, dressing, and repositioning the care recipient place physical strain on the caregiver and may result in musculoskeletal injury such as back ache, muscle strain, and contusions. These effects are likely to be exacerbated among older caregivers with impaired vestibular function, limited motion due to arthritis, and weakness due to age–related changes in muscle mass."
"The risk of injury is further compounded by the home environments of the care recipient, which may include small spaces, crowded and cluttered rooms, and steep stairways."
"(T)he fact that paid home health aides as well as home care nursing and rehabilitation personnel sustain high rates of work–related musculoskeletal disorders suggests that this is likely to be a problem among family caregivers as well." Source: Schulz, R Eden J "Families Caring for an Aging America," National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board of Health Care Services; Committee on Family Caregiving for Older Adults, 2016 pp. 100–101
Disincentive to Innovate
Finally, manufacturers lack any incentive to bring new basic DME innovations to market. Contrast the experience of getting a wheelchair today with the advancements made in oxygen concentrators and sleep apnea machines. In the latter, where clinicians and health systems support innovation through a willingness to pay higher prices, there are all sorts of companies bringing new products to market. The medical benefits are appreciated by physicians, measuring the things that physicians value: these devices inherently meet the "medical necessity" standard.
BUT the same statement cannot be made when it comes to basic DME. Whether or not people have the right equipment to ambulate, to toilet, to dress – patients are referred to the internet to purchase such items over the internet to avoid the paperwork involved with DME coverage. The result? No incentive to go beyond the "cheapest" alternative, placing avoidable burdens on family caregivers and an overly–challenging work environment for paid staff.
LIKELY EFFECTS OF A "FUNCTIONAL INDEPENDENCE" COVERAGE STANDARD
Functional Level is included in federal efforts to standardize post–acute care outcomes, specifically including outcome measures for Mobility and Self–Care tasks. Consider the measures used in Section GG, which is being phased into all post–acute care settings, including skilled nursing facilities (SNFs), rehabilitation hospitals, long–term care hospitals and home health agencies (HHAs). Not yet finalized for HHAs, this approach will be required of SNFs effective October 2018.
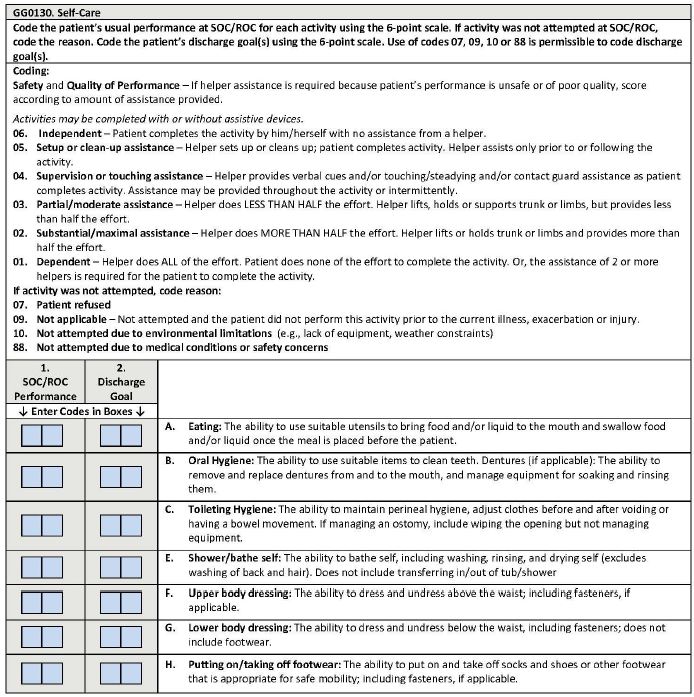
Note the emphasis on how much can be done, with or without personal assistance. This is a major opportunity to act in the interest of the care recipient and their families, of the paid workforce that takes on the challenge of helping those with mobility–related disabilities to live their healthiest lives.
At minimum, require plans to cover innovative equipment that can improve, or maintain, beneficiaries´ Section GG scores regardless of site of care (SNF, HHA, in–patient rehab or LTC Hospital). Support "Trials of N + 1" to allow for small usability and safety studies, growing slowly enough to support large enough Cost–Effectiveness studies that can justify expenditure for innovative products across larger populations. Please see "´N of 1´ Trials: Great News for Assistive Device Innovation" for more information about this approach.
The Return on Investment (ROI) of a "Functional Independence" standard can be estimated by modeling the potential for changes in the following, based on improvements in Section GG scores for beneficiaries with mobility–related disabilities:
- Hospital Readmissions/ED Visits,
- Provider Staff Recruitment and Retention Costs,
- Family Caregiver Burden;
- Injury Rates of Paid Workers and Family Caregivers;
- Patient Satisfaction Scores; and
- Provider Star Ratings
Thank you for your time and attention,
FULL DISCLOSURE: I came to appreciate the connection between family caregiving, equipment design and functional independence through my experience commercializing a SELF–Lift–&–Transfer Bedside Commode for older adult wheelchair users unable to safely access a flush toilet. I am currently conducting interviews with Subject Matter Experts for the TREAT Center´s Technical Assistance program, creating a summary report regarding health systems´ response to the needs of older adults aging with mobility–related disabilities.
Respectfully submitted,
Peg Grahm
From: Jennifer Muthig
Sent: Friday, June 29, 2018 2:18 PM
To: doh.sm.1115Waivers <1115waivers@health.ny.gov>
Subject: 1115 Public Forum Comment
Good afternoon,
Attached please find comments regarding the 1115 waiver. If you have any questions please do not hesitate to contact me, thank you.
MS National Multiple Sclerosis Society
June 29, 2018
Dear 1115 Waiver team:
Multiple sclerosis (MS) is an unpredictable, often disabling disease of the central nervous system that disrupts the flow of information within the brain, and between the brain and body. Symptoms vary from person to person and range from numbness and tingling, to walking difficulties, fatigue, dizziness, pain, depression, blindness and paralysis. The progress, severity and specific symptoms of MS in any one person cannot yet be predicted and while disease modifying therapies exist to assist with the symptoms to cure is known at this time.
When reviewing the work of the various components of the 1115 waiver programs there is a glaring omission: programs for people with physical disabilities. In fact, none of the DSRIP–PPSs in New York City have any members from organizations representing the needs of people with physical disabilities. Many other diagnosis types have been carved out because the needs of that population require special consideration to maximize their health outcomes, including HIV/AIDS, behavioral health and programs for children and families. People with physical disabilities are not represented on their own, instead they are lumped into managed long term care, assuming their care needs are similar to people who are elderly. While some of the needs of senior adults and people with physical disabilities may overlap, there are many significant differences that if addressed lead to healthier, more independent and more productive population or people with disabilities.
Managed care for people with mental and physical disabilities and chronic conditions such as Multiple Sclerosis (MS) must be based–to the maximum extent possible–on individual choice, person–centered planning, and consumer self–direction. This is particularly important for people with disabilities who are covered by Medicaid or are dually eligible for Medicaid and Medicare, especially when transition to managed care arrangements is mandated rather than voluntary.
The rumored closing of Independence Care System (ICS), the only managed care plan in New York State with a specialization in caring for people with disabilities, will dilute the expert services need by people who live with MS to live independently in their homes. Most skills are enhanced when you use them frequently and because ICS has a concentration of members with disabilities, it has allowed them to develop specialized programs to support the needs of people with physical disabilities, including specialized care management for people with Multiple Sclerosis. The high volume of people with MS and other physical disabilities has allowed ICS to develop a comprehensive understanding of the most prevalent conditions that occur for people with physical disabilities and create programs including a wheelchair evaluation, purchase and repair program, a wound care prevention program and a women´s health program that address the unique healthcare needs of people with physical disabilities.
People with physical disabilities in general, and people with Multiple Sclerosis in particular, need their care provided by people with a deep understanding of their condition. Because MS is a progressive neurological disease, a person´s condition can change rapidly and without caregivers that understand that fact, people with MS are more likely to end up hospitalized. People with physical disabilities are a high cost population and often times their community based services costs (i.e. homecare) are fixed because their disability is permanent. The population also is likely to experience secondary conditions that happen as a result of their disability that are highly predictive and preventable. For the population with MS, one such condition is Urinary Tract Infections (UTIs). A recent study (Oynhausen, 2014) showed that people with MS are who are underinsured often use the Emergency Department for the care of UTIs and are more likely to be admitted to the hospital for this treatment. This is a very costly way treat a common condition. Because ICS has 18 years of knowledge and experiences in working with people with MS, they developed interventions that help their members with MS to prevent UTIs including education to recognize the symptoms and supporting a relationship with a clinic that can respond quickly and provide the medications that can prevent Emergency Department usage and hospitalizations.
We urge New York State to use the 1115 waiver program to create a demonstration program for people with physical disabilities to lead the way in providing disability expert care in a fully integrated setting that could demonstrate both the positive health outcomes and cost savings that come when people with physical disabilities get the care they need from expert providers like Independence Care System so that those with live with MS can truly live their best lives possible and in their homes.
Thank you for your attention to this issue. If you have any questions or comments, please contact Director of Advocacy and Policy Jennifer Muthig.
Thank you,
Jennifer Muthig
Director of Policy & Advocacy
National Multiple Sclerosis Society
JOIN THE MOVEMENT®
1100 New York Ave. NW, Suite 440E, Washington D.C. 2005 tel. +1 202 408 1500 fax +1 202 408 0696 https://www.nationalMSociety.org/advocacy
Follow Us