Open Doors Transition Center
The Open Doors Transition Center helps people living in nursing homes and intermediate care facilities to explore options for living and receiving services in the community. Open Doors is a project of the Money Follows the Person (MFP) program. Skilled transition specialists help you navigate the transition planning process and work with staff in the facility and in the community to assist you with setting up services in the community.
Anyone can make a referral to the Open Doors Transition Center!
For more information or to make a referral to Open Doors:
- Phone: 1-844-545-7108
- Email: secq@ilny.org
- Fax: 1-518-465-4625
- Open Doors Website (ilny.us)
Who can receive Open Doors assistance?
Adults aged 18 years or older who have:
- ✓ Medicaid coverage for at least one day of care in the facility
- ✓ Lived in a nursing home, hospital, or intermediate care facility for at least 60 days
- ✓ Needs that can be met in the community with home and community-based services
- ✓ A desire to move to a home in the community, such as a house, apartment, or small group home providing residence for four people or less
- ✓ A physical or developmental disability, traumatic brain injury, or who are elderly (including those elderly with mental health needs)
- ✓ Consented to participate
For more information about MFP and Open Doors, view this 2017 webcast: The Money Follows the Person Program: Facilitating Return to Community-based Settings
MFP participants are linked to Medicaid funded home and community-based services following their transition to the community.
The Open Doors Transition Center
| Transition Supports | Description |
|---|---|
| Transition Assistance | Provides information on community living and facilitates transition planning.
The Open Doors Transition Center consists of a network of 24 local transition centers throughout New York State. Working with nursing home and intermediate care facility staff, and home and community-based services providers, transition specialists assist participants to identify and access supports, benefits, and services in the community. Open Doors serves as a bridge between facility discharge planning and coordination and delivery of medical and supportive services in the community. |
| Peer Support | Supports participants considering transition.
Peers are people who have lived in institutional settings and then moved to home and community-based settings, and who have received services and support where they live. Peers visit and talk to Open Doors participants in nursing homes and intermediate care facilities to share their life experiences living independently in the community. Peers provide support during the transition process and can assist with community integration. Peers who are military veterans and family peers are also available to offer support. Peer support is available during the transition process and up to 60 days after discharge. |
| Education & Outreach | Provides information about community transition to nursing homes statewide.
Education and outreach staff provide targeted education to all nursing homes throughout New York State regarding the Minimum Data Set Section Q, the referral process to the Local Contact Agency, and the availability of community supports. These presentations include helpful information on transition center referral, assistance, and collaboration, and how these activities support compliance with the Olmstead decision. Presentations about Open Doors are also provided to many other referral sources such as community-based service providers, Ombuds staff, managed care plan staff, and others. |
| Good Neighbor Project | Provides informal support to participants.
The Good Neighbor project helps participants who do not have informal supports such as family and friends to support them in the community after they leave a nursing home or intermediate care facility. Good Neighbors can help fill crucial gaps in participants' informal support networks to enable participants to move from the facility to the community. |
| Communication Support | Supports independence and participation in transition planning.
To support participation in the transition planning process, participants may be able to receive an Open Doors mobile phone with pre-paid minutes and a short-term data plan to help them communicate with their transition specialist, community service providers, and informal supports during the transition planning process. |
| Person-Centered Planning Coaching | Builds skills for self-advocacy in service planning.
The federal Home and Community Based Services Final Rule supports participants to have full access to the benefits of community living and receive services in the most integrated settings. Person-centered planning coaching teaches Open Doors participants skills to improve self-advocacy during the person-centered planning process. This service is offered post-discharge to individuals who have transitioned to and are receiving services in the community. |
| Food Security | Provides grocery cards to address food insecurity upon discharge.
Grocery cards are available to participants identified as being at risk for food insecurity during the first month after discharge from the facility as a bridge to more permanent solutions. |
Participant Age Community Transitions with Open Doors in 2023
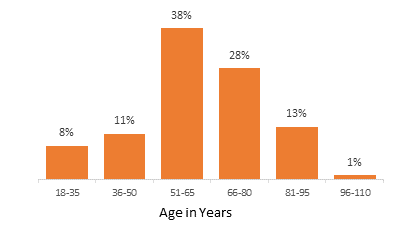
| Age range | Percentage |
|---|---|
| 18-35 | 8% |
| 36-50 | 11% |
| 51-65 | 38% |
| 66-80 | 28% |
| 81-95 | 13% |
| 96-110 | 1% |
Target Population Served Community Transitions with Open Doors in 2023
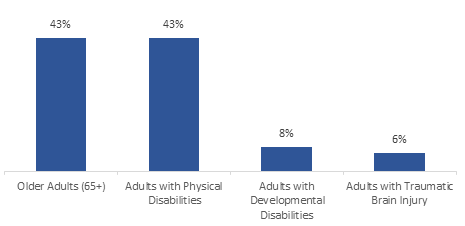
| Target Population | Percentage |
|---|---|
| Older Adults (65+) | 43% |
| Adults with Physical Disabilities | 43% |
| Adults with Developmental Disabilities | 8% |
| Adults with Traumatic Brain Injury | 6% |
Medicaid Home and Community Based Services Community Transitions with Open Doors in 2023
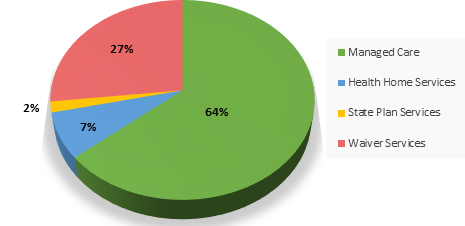
| Partner Programs | Percentage |
|---|---|
| Managed Care | 64% |
| Waiver Services | 27% |
| Health Home Services | 7% |
| State Plan Services | 2% |
Download the Open Doors brochure here:
This project is supported by the Centers for Medicare and Medicaid Services (CMS) of the U.S. Department of Health and Human Services (HHS) as part of a financial assistance award that is 100% funded by CMS/HHS. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by CMS/HHS, or the U.S. Government.
