NYS Mainstream Medicaid Managed Care and School Based Health Center Billing Guidance
Note: Benefit Transition Date no sooner than April 1, 2026
- Billing Guidance is also available in Portable Document Format (PDF)
April 1, 2025 Implementation
April 2025 www.health.ny.gov/mrt Office of Health Insurance Programs
I. Introduction
II. Confidentiality
III. Billing and Payment of SBHC Services by Service Type
IV. Identification of SBHC Claims
Appendix A. Definitions
Office of Health Insurance Programs
NYS Mainstream Medicaid Managed Care and School-Based Health Center (SBHC) Billing Guidance
I. Introduction
This guide provides additional clarification for the general billing and payment guidance found in section VI. "SBHC Billing and Reimbursement" of the Department of Health (Department) publication entitled, Transition of School-Based Health Center Benefit and Population into MedicaidManaged Care. The guide is applicable to mainstream Medicaid Managed Care Plans (MMC) and HIV Special Needs Plans (HIV SNP) (herein referred to as MMCPs), for services provided to their enrollees by SBHC and SBHC-Dental (SBHC-D) operators.
II. Confidentiality
All MMCPs will ensure appropriate policies and procedures are in place to adhere to the Department's Policy for the Protection of Confidential Health Information for Minors Enrolled in NYS Medicaid Managed Care Plans.
III. Billing and Payment of SBHC Services by Service Type
A. Knowing Who to Bill for SBHC Services
For dental and behavioral health benefits managed by an MMCP through a sub-contractual relationship, the SBHC may be required to directly bill the subcontractor as indicated by the MMCP. Claim submission requirements may vary depending on the terms of contracts between MMCPs and SBHC operators.
B. Methods to Address Payment for the Transition Period
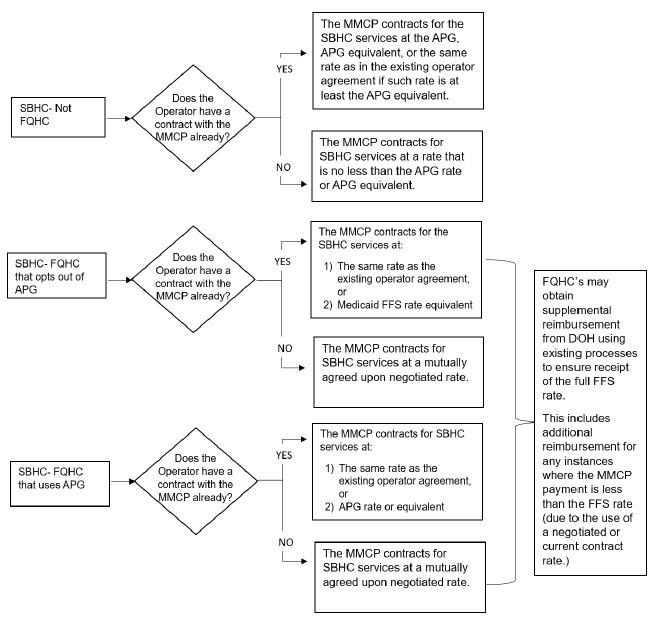
The Department intends that the transition of SBHC services to managed care be essentially cost neutral for the operators for a period of at least two (2) years following the transition effective date. To effectuate that goal, the Department requires the MMCP to reimburse the SBHC operators in accordance with how such operators would have been paid by the Medicaid fee-for-service (FFS) program. The claims and billing subgroup has identified that payment in accordance with Medicaid FFS rules can be fulfilled in a number of ways. The following is intended to illustrate the methods that satisfy the Department's intent as it relates to MMCP reimbursement for SBHC services, operated by Federally Qualified Health Centers (FQHCs) and non-FQHCs, and provide flexibility for SBHCs and MMCPs in order to avoid unnecessary systems configuration for both parties. Appendix A provides definitions of key terms used in this document.
IV. Identification of SBHC Claims
| Institutional Claim Identifiers | Paper (UB) | Electronic (837I) |
| Bill type | 089 | 089 |
| School Health Specific Rate Codes | Box 39 – Amount | L2300; HI01-5 |
| Professional Claim Identifiers* | Paper (1500) | Electronic (837P) |
| Place of Service | Value of 03, in Box 24 – B | Value of 03 in L2300; CLM05-1 |
*Billed only by hospital sponsored SBHCs when a physician service is performed in the visit.
V. General Claim Requirements
Every electronic claim submitted to an MMCP, regardless of payment methodology (i.e., Ambulatory Patient Group (APG) or Medicaid FFS/Prospective Payment System (PPS) rate), will require at least the following:
- Facility Claims
- Use of the 837i claim form;
- Bill type 089;
- Diagnosis code(s);
- Revenue code(s);
- Medicaid fee for service rate code(s);
- Valid procedure (current procedural terminology (CPT) and/or healthcare common procedure coding system (HCPCS)) code(s);
- Procedure code modifiers (as needed);
- Charge; and
- Unit(s) of service.
- Professional Claims (where applicable, see also Section IV.)
- Use of 837p claim form;
- Diagnosis code(s);
- Place of service;
- Valid procedure (CPT and HCPCs) code(s);
- Procedure code modifiers (as needed);
- Charge; and
- Units of service.
VI. SBHC APG & Rate Codes
SBHCs are to bill in accordance with the APG manual published by the Department. The table below is excerpted from the APG manual.
| Setting/Sponsor | Service | APG Visit Rate Code | APG Episode Rate Code |
|---|---|---|---|
| Hospital | School Based Health Center | 1444 | 1450 |
| Free ‐ Standing DTC | School Based Health Center | 1447 | 1453 |
Instructions for the submission of claims for Licensed Clinical Social Worker (LCSW), Licensed Masters Social Worker (LMSW), Licensed Mental Health Counselor (LMHC), and Licensed Marriage and Family Therapist (LMFT) services provided on the same day as other SBHC services are as follows:
| Rate Codes Established for SBHC Reimbursement for Mental Health Counseling when Provided by a LCSW/LMSW:1 | |
|---|---|
| Rate Code | Description |
| 3257 | SBHC-LCSW/LMSW service 20-30 minutes with patient |
| 3258 | SBHC-LCSW/LMSW service 45-50 minutes with patient |
| 3259 | SBHC-Family services LCSW/LMSW with or without patient present |
| Rate Codes Established for SBHC Reimbursement for Mental Health Counseling when Provided by a LMHC/LMFT:1 | |
|---|---|
| Rate Code | Description |
| 3260 | SBHC-LMHC/LMFT service 20-30 minutes with patient |
| 3261 | SBHC-LMHC/LMFT service 45-50 minutes with patient |
| 3262 | SBHC-Family services LMHC/LMFT with or without patient present |
For non-FQHCs and FQHCs that utilize APGs a separate mental health counseling claim must be submitted to the MMCP with the appropriate billing codes. The claim will pay at APG under a separate grouper rate.
FQHCs that do not utilize APGs should add mental health counseling service to the medical claim and submit it to the MMCP to pay at the FFS rate or contracted rate.
Vaccine Rate Codes (Administration Only):2
Influenza and pneumococcal vaccinations provided at SBHCs are billable using the non-APG rate codes below. Providers are to use the CPT code of the vaccine/toxoid administered with the appropriate rate code to be reimbursed for the administration of influenza and/or pneumococcal vaccines supplied by or available through the Vaccine for Children (VFC) program. No separate or additional vaccine administration CPT code is required.
| Vaccine Administration Rate Codes | |
|---|---|
| Rate Code | Description |
| 1381 | SBHC flu seasonal vaccines - administration only |
| 1383 | SBHC pneumococcal, vaccines - administration only |
SBHCs should bill all other vaccinations utilizing one of the APG rate codes listed above. The provider must append modifier SL to the CPT code of the vaccine/toxoid administered (indicating the administration of a vaccine supplied by or available through the VFC program or a vaccine supplied at no cost) to be reimbursed for the administration of the vaccine. Providers should refer to the NYS DOH "NYS APG Modifiers" web page, for current reimbursement rates when appending the modifier SL. No separate or additional vaccine administration CPT code is required.
Appendix A: Definitions
Fee-for-service is a Medicaid payment model where services are unbundled and paid for separately. Health care providers are paid for each service performed (i.e., office visits, laboratory tests, and procedures.)
Ambulatory Patient Groups (APGs) is an outpatient Medicaid payment system based upon an Enhanced Ambulatory Patient Group classification system. This system categorizes the amount and type of services across all ambulatory care settings (i.e., outpatient, ambulatory surgery, emergency room and diagnostic and treatment centers).
Prospective Payment System (PPS) is a system in which payment is made for primary health care and qualified preventive services based on a national rate adjusted to the location where services are provided. The national rate is a predetermined fixed amount.
___________________________
1. Medicaid Update; December 2022, Licensed Clinical Social Worker, Licensed Mental Health Counselor, and Licensed Marriage and Family Therapist Service Coverage. 1
2. Medicaid Update; October 2024, New York State Medicaid Fee-for-Service Coverage for Vaccinations Administered by Providers. 2
Follow Us