Nursing Home Transition and Diversion (NHTD) Waiver and Traumatic Brain Injury (TBI) Waiver
Transition to Managed Care Workgroup Meeting
- Minutes also available in Portable Document Format (PDF)
August 24, 2015
Medicaid Redesign Background
- In 2011, Governor Andrew M. Cuomo established a Medicaid Redesign Team (MRT), which initiated significant reforms to the New York State (NYS) Medicaid program, including a critical initiative to provide "Care Management for All" by transitioning NYS´ Long Term Care recipients into managed care programs.
- The Care Management for All approach will improve benefit coordination, quality of care and patient outcomes over the full range of health care, including mental health, substance abuse and developmental disability and physical health care services.
- The MRT Action Plan which outlines the Care Management for All approach was included within the informational packet.
MRT Background
- On August 31, 2012, the Department of Health (DOH) received written approval from the Centers for Medicare and Medicaid Services (CMS) to move forward with Mandatory Managed Long Term Care (MLTC), which focuses on the transition of long term community based services into managed long term care models.
- The CMS approval was granted in phases to fully implement the transition and enrollment of individuals previously exempt or excluded from enrolling in Medicaid Managed Care (MMC) and Managed Long Term Care (MLTC) Plans.
NHTD/TBI Waivers
- 1915c Medicaid waivers are designed to provide services to a specific target population and there are two distinct waivers:
- Individuals between the age of 18–64 upon application that require nursing home level of care due to their traumatic brain injury (TBI) and
- Individuals between the age of 18–64 upon application that have a physical disability or who are 65 or older and require nursing home level of care (NHTD).
- Both waivers are managed locally through the same Regional Resource Development Centers but with different staff.
- Both waivers serve individuals residing in the community (diversions) or individuals residing in nursing homes that are seeking to move back to the community (transitions).
- Waiver services are not provided in nursing homes.
Waiver Eligibility Criteria
- The NHTD and TBI Medicaid waiver programs were developed based on the philosophy that individuals with disabilities, or seniors, may be successfully served and included in their surrounding communities. The individual is the primary decision maker and works in cooperation with care providers to develop a plan of services that promotes personal independence, greater community inclusion, self–reliance and participation in meaningful activities and services.
- The NHTD and TBI waiver eligibility criteria were included in the informational packet.
- The waiver programs provide a coordinated plan of care and services for individuals who would otherwise be medically eligible for placement in a nursing facility. The programs enable the state to provide participants with a number of supportive services not available under the State´s Plan for Medicaid services because the provision of waiver services is effective in preventing premature institutionalization of program participants and allows those who are at risk for nursing home placement to remain in the community.
- The waiver services were included in the informational packet.
What is Managed Care?
- Managed Care: a comprehensive and coordinated system of medical and health care service delivery encompassing ancillary services, as well as acute inpatient care.
- The Managed Care Organization (MCO) is responsible for assuring that enrollees have access to a comprehensive range of preventative, primary and specialty services.
- In a MCO, each Medicaid enrollee is linked to a Primary Care Provider (PCP).
- This PCP is responsible for the delivery of primary care and also coordinates and case manages most other necessary services.
- The PCP may be a specialist (SNP and HARP).
Managed Care and Waivers
- In keeping with this goal of Care Management for All, the state plans to transition the 1915c Home and Community Based Services (HCBS) Waivers, including NHTD and TBI waiver participants, into managed care programs.
- To receive long term care services, as well as to continue receiving current services received through the 1915c waiver, current participants will have to enroll into one of two managed care programs: MLTC or MMC.
- MLTC enrollees are individuals who are dual eligible (Medicaid and Medicare) and who are:
- Age 21 and older in need of community based long term care services for more than 120 days
- Effective 7/1/15 on a statewide basis, dual eligible Nursing Home residents who are age 21 and older and determined to need permanent Nursing Home placement must join a MLTC Plan
- Duals between 18 and 21 remain voluntary enrollment
- MMC enrollees are individuals with Medicaid only.
MLTC
- MLTC, also referred to as MRT #90, focuses on the transition of long term community based services into managed long term care plans to provide coordinated care for all and allow for a seamless supportive care delivery.
- MLTC seeks to help people who are chronically ill and who need health and long term care services stay in their homes and communities as long as possible
- The program is designed to be person–centered and integrate services and improve health outcomes for individuals in need of Long Term Services and Supports.
Types of MLTC Plans
- A MLTC Plan is a private health plan that provides Medicaid long term care benefits. As of January 1, 2015, enrollees have a choice of four MLTC Plans:
- Partially Capitated (Medicaid)
- Benefit package is long term care and ancillary services, including home care and unlimited nursing home care.
- Program for All–Inclusive Care for the Elderly (PACE) (Medicare and Medicaid)
- Benefit package includes all medically necessary services – primary, acute, and long term care.
- Medicaid Advantage Plus (MAP) (Medicare and Medicaid)
- Benefit package includes primary, acute, and long term care services (excludes specialized mental health services).
- Fully Integrated Duals Advantage (FIDA) (In downstate demonstration counties only)
- Benefit package includes Medicare Part A, Part B, and Part D (prescription medicines) and Medicaid services (home or nursing care and behavioral health services).
- Partially Capitated (Medicaid)
What is a Partial Plan?
- In a Partially Capitated Plan, an enrollee receives Medicaid services only:
- Nurses, home health aides, and physical therapists
- Personal Care: help with bathing, dressing, and grocery shopping
- Adult Day Health Care
- Social Day Care
- Nursing Home Care
- Specialty Health: audiology, dental, optometry, podiatry, and physical therapy
- Other services are available such as: home–delivered meals, personal emergency response services, and transportation to medical appointments.
- Medicare services: Continue with current coverage.
- A list of the covered services are contained within the informational packet.
What is a MAP Plan?
- In a MAP Plan, an enrollee receives both Medicaid and Medicare services from one Plan.
- The enrollee must use the Plan´s Medicare product and must choose a Primary Care Physician from the MAP Plan.
- In addition to the Partial services, a highlight of the Medicare services include:
- Doctor office visits
- Specialty care
- Clinic visits
- Hospital stays
- Mental health services
- X–ray and other radiology services
- Chiropractic care
- Medicare Part D drug benefits
- Ambulance services
What is a PACE Plan?
- A PACE Plan provides the enrollee with the same Medicaid and Medicare services through one Plan as MAP does, but the delivery of service is different.
- PACE health services are provided by a team that includes doctors, nurses, social workers, and others.
- The team of health care professionals help make health care decisions. The enrollee and family participate as the team develops and updates the plan of care and goals in the program.
- Enrollee has to be at least 55 years old to join PACE.
What is a FIDA Plan?
- A FIDA Plan provides certain dual eligible individuals (Medicaid and Medicare) with services through one fully–integrated managed care plan. Currently, available in New York City and Nassau County only.
- Each Participant must have an individualized care planning process using an Interdisciplinary Team (IDT) approach. Care will be person–centered, based on the Participant´s specific preferences and needs, and deliver services with respect to linguistic and cultural competence, and dignity.
- FIDA includes items and services currently covered by:
- Medicare
- Medicaid
- Behavioral health
- Wellness programs
- Prescription drugs
- NHTD and TBI Home and Community Based Waiver services
What is Mainstream Managed Care?
- Medicaid Managed Care provides Medicaid state plan benefits to enrollees through a managed care delivery system comprised of Managed Care Organizations (MCOs).
- Enrollment into an MCO is mandatory for eligible individuals, unless otherwise exempt or excluded.
- Medicaid eligibility must be first established by the New York State of Health (NYSoH) or the Local Departments of Social Services before enrolling into a MMC Plan.
- The MMC Plan is a comprehensive plan of services.
Medicaid Managed Care (MMC)
- A NYS–sponsored health insurance program for adults and children who have little or no income or who receive Supplemental Security Income (SSI).
- Authorized under Section 364–j of Social Services Law.
- NYS contracts with MCOs who then pay the participating provider directly for services.
- NYS pays the MCOs a capitated rate (per member/per month).
- Benefits consist of plan covered services and Medicaid fee–for–service (FFS) carve–outs.
- Very few carve–outs remain as these services were transitioned into MMC.
Exemptions
- Most Medicaid eligible individuals are required to enroll in a MMC Plan unless exempt or excluded.
- An exemption means that a consumer is not required to join a MMC Plan unless he or she so chooses. If a consumer is already enrolled in a MCO and applies for and receives an exemption, he or she will be disenrolled from the MCO.
- Exempt individuals can choose to enroll in a Plan or remain in FFS Medicaid:
- Person with chronic medical conditions with a non–participating physician – limited to a single 6 month exemption;
- Residents of long term chemical dependence treatment programs;
- Developmentally Disabled and other waivered individuals; and
- Native Americans.
What is Covered Under Medicaid Managed Care?
- Inpatient Hospital Services
- Emergency Services
- Physician Services/Nurse Practitioner Services/Midwifery Services
- Preventive Health Services
- General health education classes
- Smoking cessation
- Immunizations
- Laboratory Services
- Radiology Services
- Prescription/Non Prescription Drugs and Medical Supplies
- Home Health Services
- Behavioral Health (Mental Health and Substance Use)
- Dental
- Orthodontia
- Rehabilitation Services
- Physical Therapy
- Occupational Therapy
- Speech Therapy
- Durable Medical Equipment (DME)
- Vision Care
- Personal Care Services
- Consumer Directed Personal Assistance
- Hospice Services
- Family Planning
Receiving Care in a MLTC or MMC Plan
- Each enrollee that transitions to MLTC or MMC will have continuity of care under the enrollee´s pre–existing service plan for at least 90 days, or until a care assessment has been completed by the Plan, whichever is later.
- Each enrollee will have a:
- Person–centered plan of care, and
- Care Manager who will ask about service needs and assist the enrollee and family in developing a plan of care that meets the enrollees specific needs. The care manager also coordinates the delivery of services and outreaches to enrollee, at minimum, on a monthly basis.
DOH Complaints
- Enrollees and providers may file a complaint regarding managed care plans to DOH.
- DOH maintains toll free complaint lines for both MLTC and MMC enrollees:
- For MLTC: 1–866–712–7197 or mltccomplaints@health.ny.gov
- For MMC: 1–800–206–8125 or managedcarecomplaint@health.ny.gov
Enrollee Rights
- All MLTC/MMC enrollees must be informed of the Plan´s grievance and complaints systems.
- Enrollees can file a complaint or grievance with the Plan, either verbally or in writing.
- For a reduction, termination or suspension of service within the authorized period, the MLTC/MMC Plan will issue a Notice of Action, giving the enrollee the right to request a fair hearing and an internal appeal offering aid to continue.
- Enrollees can file an appeal for reconsideration of a Plan decision, there are two types of appeals: Expedited Appeal and Standard Appeal
- Enrollees can file a fair hearing through the Office of Temporary and Disability Assistance (OTDA) either verbally or in writing and request Aid to Continue in certain situations.
Participant Ombudsman – ICAN
- Additional safeguards exist, individuals can also call the Participant Ombudsman program, known as the Independent Consumer Advocacy Network (ICAN), which launched on December 1, 2014.
- ICAN provides Participants with direct assistance in navigating their coverage and in understanding and exercising their rights and responsibilities.
- ICAN serves MLTC and MMC enrollees who receive long term services and supports.
- The call center receives calls from the entire state and there are 60 locations throughout the state where individuals can get in–person assistance.
- ICAN can be reached by calling 1–844–614–8800 or online at: www.icannys.org.
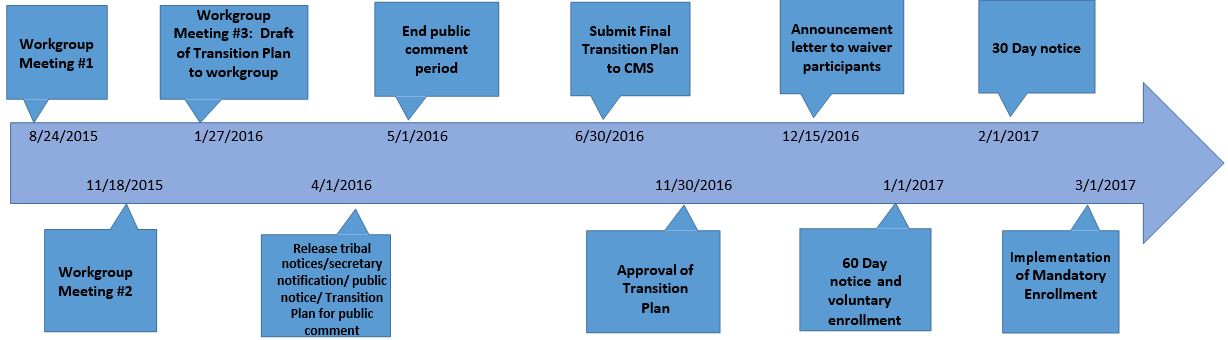
Draft NHTD/TBI Transition Timeline
Other Considerations
- Home and Community Based Services (HCBS) Settings Transition Plan
- 1115 Waiver Amendments
Follow Us