F-SHRP 2012 Annual Report
- Report is also available in Portable Document Format (PDF, 317KB)
Federal-State Health Reform Partnership
Section 1115 Quarterly Report
Demonstration Year: 6 (10/1/2011 - 9/30/2012)
Federal Fiscal Quarter: 4 (07-01-2012 - 09/30/2012)
I. Introduction
On September 29, 2006, New York State received Centers for Medicare and Medicaid Services (CMS) approval to join in a partnership to reform and restructure the State´s health care delivery system. To accomplish the reform and restructuring, CMS approved a new five-year 1115 demonstration entitled, Federal-State Health Reform Partnership (F-SHRP). The waiver was effective October 1, 2006 through September 30, 2011. On March 31, 2011, CMS approved a three year extension of the F-SHRP Demonstration for the period April 1, 2011 through March 31, 2014. An amendment to the F-SHRP waiver, approved on July 29, 2011 provided authority to mandatorily enroll participants in the Recipient Restriction Program, one of the recommendations of the Governor´s Medicaid Redesign Team (MRT). CMS approved three waiver amendments on September 30, 2011, March 30, 2012 and August 31, 2012 incorporating additional changes resulting from recommendations of the MRT.
Under F-SHRP, the federal government will invest up to $1.5 billion over the life of the Demonstration in agreed upon reform initiatives. The primary focus of these initiatives is to promote the efficient operations of the State´s health care system; consolidate and right-size the State´s health care system by reducing excess capacity in the acute care system; shift emphasis in long-term care from institutional-based to community-based settings; expand the use of e-prescribing; foster the implementation of electronic medical records and regional health information organizations; and expand ambulatory and primary care services.
In accordance with Section VII, paragraphs 32 and 33 of the Special Terms and Conditions (STCs), this annual report documents program accomplishments, project status, health reform initiatives, quantitative and case study findings, evaluation findings, utilization data and policy/administrative complexities during the fifth year of the Demonstration (10/01/2011 - 9/30/2012) and includes significant Demonstration activities during the fourth quarter of the Demonstration year (7/1/12 - 9/30/12).
II. Accomplishments
In Demonstration Year 6 (DY6), New York State made significant progress toward achieving the F-SHRP goals of reforming the health care delivery system and expanding Medicaid managed care.
- Mandatory enrollment of Supplemental Security Income (SSI) and SSI-related individuals has been implemented in 53 counties and New York City.
- The number of SSI and SSI-related individuals enrolled in Medicaid managed care increased to 341,739 (79% of eligibles) as of September 2012.
III. Enrollment
Fourth Quarter
| Population Groups | Current Enrollees | # Voluntary Disenrollments | # Involuntary Disenrollments |
|---|---|---|---|
| Population 1 – TANF Child under 1 through 20 ("new" MC enrollment) | 79,261 | 1,329 | 3,781 |
| Population 2 – TANF Adults aged 21–64 ("new" MC enrollment) | 29,603 | 617 | 1,982 |
| Population 3 – Disabled Adults and Children 0–64 ("old" voluntary MC enrollment) | 66,827 | 2,151 | 412 |
| Population 4 – Disabled Adults and Children 0–64 ("new" MC enrollment) | 227,887 | 7,810 | 2,056 |
| Population 5 – Aged or Disabled Elderly ("old" voluntary MC enrollment) | 4,457 | 506 | 81 |
| Population 6 – Aged or Disabled Elderly ("new" MC enrollment) | 42,568 | 3,074 | 663 |
Demonstration Year Voluntary Disenrollment
| Population Groups | 1st Quarter | 2nd Quarter | 3rd Quarter | 4th Quarter | FFY 2011 Total |
|---|---|---|---|---|---|
| Population 1 – TANF Child under 1 through 20 ("new" MC enrollment) | 1,317 | 1,365 | 1,479 | 1,329 | 5,490 |
| Population 2 – TANF Adults aged 21–64 ("new" MC enrollment) | 549 | 542 | 649 | 617 | 2,357 |
| Population 3 – Disabled Adults and Children 0-64 ("old" voluntary MC enrollment) | 1,252 | 1,697 | 3,024 | 2,151 | 8,124 |
| Population 4 – Disabled Adults and Children 0–64 ("new" MC enrollment) | 6,966 | 9,155 | 9,825 | 7,810 | 33,756 |
| Population 5 – Aged or Disabled Elderly ("old" voluntary MC enrollment) | 596 | 634 | 733 | 506 | 2,469 |
| Population 6 – Aged or Disabled Elderly ("new" MC enrollment) | 2,797 | 2,901 | 3,223 | 3,074 | 11,995 |
Demonstration Year Involuntary Disenrollment
| Population Groups | 1st Quarter | 2nd Quarter | 3rd Quarter | 4th Quarter | FFY 2011 Total |
|---|---|---|---|---|---|
| Population 1 – TANF Child under 1 through 20 ("new" MC enrollment) | 3,927 | 3,352 | 3,630 | 3,781 | 14,690 |
| Population 2 – TANF Adults aged 21–64 ("new" MC enrollment) | 2,038 | 1,770 | 1,783 | 1,982 | 7,573 |
| Population 3 – Disabled Adults and Children 0-64 ("old" voluntary MC enrollment) | 454 | 442 | 994 | 412 | 2,302 |
| Population 4 – Disabled Adults and Children 0–64 ("new" MC enrollment) | 1,807 | 1,857 | 2,142 | 2,056 | 7,862 |
| Population 5 – Aged or Disabled Elderly ("old" voluntary MC enrollment) | 59 | 66 | 189 | 81 | 395 |
| Population 6 – Aged or Disabled Elderly ("new" MC enrollment) | 532 | 594 | 684 | 663 | 2,473 |
F-SHRP Waiver - Voluntary and Involuntary Disenrollment
| Voluntary Disenrollments | |
|---|---|
| Total # Voluntary Disenrollments in current Demonstration Year1 | 64,191 |
Reasons for voluntary disenrollments include: enrollment in another plan, approved enrollee request to qualify as either exempt or excluded, relocation to residence outside county of enrollment and Local Departments of Social Services (LDSS) approval to disenroll based upon good cause.
| Involuntary Disenrollments | |
|---|---|
| Total # Involuntary Disenrollments in current Demonstration Year1 | 35,295 |
Reasons for involuntary disenrollments include: loss of Medicaid eligibility, eligibility transfers between Family Health Plus (FHPlus) and Medicaid, inappropriate enrollment or death.
__________________________________
1. Demonstration year to date: 10/01/2011 - 03/31/2012 1
IV. F-SHRP Waiver
- F-SHRP Waiver Amendments
Three waiver amendments provided authorization for the State to implement initiatives of the Governor's Medicaid Redesign Team (MRT), which was tasked with redesigning the provision of Medicaid services to contain costs, create efficiencies and improve the quality of care provided to Medicaid beneficiaries. Approved initiatives implemented during the demonstration year included:- For 2011 implementation: 1) thirty day choice window for existing Medicaid beneficiaries to choose a managed care plan; 2) six month limitation on the exemption period for beneficiaries with a chronic illness; and, 3) mandatory enrollment of several populations who were previously excluded or exempt from enrolling in managed care.
- For April 2012 implementation: elimination of exclusions and exemptions for, 1) infants under 6 months of age born disabled or under 1200 grams; 2) individuals with End Stage Renal Disease (ESRD); and, 3) homeless individuals.
- For September/October 2012 implementation: 1) elimination of exemption for "look-alike" populations, i.e., individuals with characteristics and needs similar to those receiving services through certain 1915c waivers and those in an Intermediate Care Facility for the Developmentally Disabled (ICF/DD); 2) mandatory enrollment of individuals in need of community based long term care services in managed long term care programs; and, 3) housing disregard for single individuals who were living in a nursing home willing to enroll in managed long term care programs.
- Twelve Month Continuous Coverage
In 2007, revisions were made to Chapter 58 of the New York State Social Services Law to provide continuous coverage for certain Medicaid beneficiaries and FHPlus enrollees for a period of twelve months from the date of initial eligibility and subsequent redetermination of eligibility. This proposal will provide stability and continuity of coverage and care to adults in the same way that it has for children on Medicaid. The Department is in the process of developing and implementing systems and program changes and anticipates an effective date of November 1, 2012.
V. Operational/Policy Developments/Issues
As part of the F-SHRP demonstration, the Department expanded mandatory managed care enrollment to 14 counties with managed care capacity and to SSI and SSI-related Medicaid beneficiaries statewide.
- Mandatory Enrollment of the SSI Population
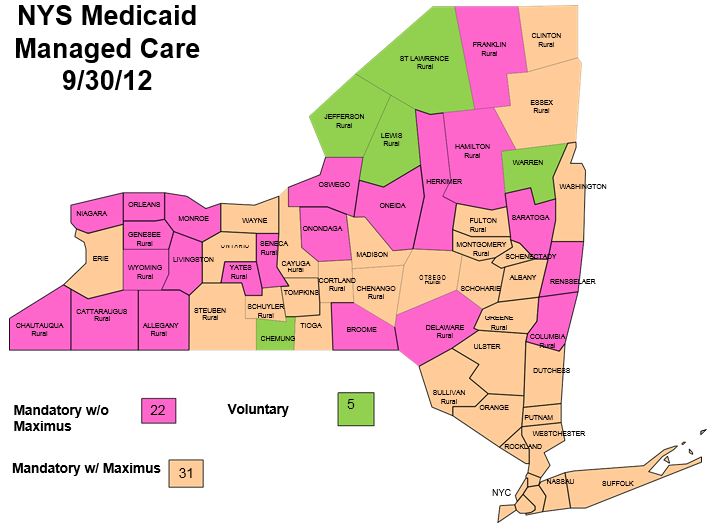
Medicaid managed care is mandatory in 53 New York State counties and New York City, while five counties operate voluntary programs. During the demonstration year, six counties implemented mandatory programs. The remaining five counties in New York State are scheduled to begin mandatory programs in the fall of 2012, marking the statewide implementation of mandatory Medicaid managed care. See Attachment 1: NYS Medicaid Managed Care Map. - Health Plans
Changes to Certificates of Authority - There were no changes to Certificates of Authority this quarter.
VI. Consumer Issues
- Complaints
Medicaid managed care plans reported a total of 734 complaints and action appeals from their SSI enrollees. This compares to 605 SSI complaints and action appeals from last quarter. Transportation was the most common complaint category, accounting for 20% of all SSI complaints.
Medicaid Advantage plans reported a total of 6 complaints and actions appeals.
VII. Successful Achievement of Milestones
- Employer Sponsored Health Insurance (ESHI) Initiative
Family Health Plus (FHPlus) Premium Assistance Program
The FHPlus Premium Assistance Program (PAP) for individuals who are eligible for FHPlus and have access to cost effective health insurance went into effect on January 1, 2008. Total enrollment as of June 30, 2012 is 3,080 individuals.
In November 2011, the 1199SEIU Home Care Workers union began offering employer sponsored health insurance to its members. The coverage was determined to be qualified and cost effective ESHI. This has increased the total number of ESHI enrollees during the quarter.Enrollment in ESHI
Through FHPlus PAPNew Enrollment
07/01/12-09/30/12Total Enrollment
September 30, 2012FHPlus Adults with children 54 584 FHPlus Adults without children 274 2,254 Total 328 2,981
Age group for reporting Quarter
07/01/12-09/30/12Number of Enrollees 19-44 2514 45-64 467 - Family Health Plus Buy-in Program
Development Activities
The United Federation of Teachers (UFT) contracted with New York State to provide up to 2,500 of their 25,000 child care providers with access to health insurance through the FHPlus Employer Buy-In. UFT will partner with the Health Insurance Plan of Greater New York to provide a network of services to their members. The child care workers are licensed and registered home based child care providers in New York City and provide services to low-income families. During the demonstration year, a total of 707 unsubsidized UFT members were enrolled into the FHPlus Buy-In Program. For child care workers who are eligible for Medicaid or Family Health Plus, the premium will be paid through the State.
Civil Service Employees Association (CSEA) also received legislative authority and appropriations to provide health insurance coverage through the FHPlus Employer Buy-In Program. CSEA is actively seeking a plan to provide coverage to their member population.
FidelisCare, present in almost every county of the State, is seeking to contract with a vendor, U.S. Fire and Unified Life, to provide family planning services so that FidelisCare can participate in the FHPlus Employer Buy-in program. As a Catholic health plan, FidelisCare does not provide these services. U.S. Fire and Unified Life are working with the State to complete the necessary steps to be approved as a vendor for family planning with FidelisCare for the FHPlus Employer Buy-In program.
The Department continues to receive inquiries from small employers about the FHPlus Buy-in Program. However, many of these inquiries are from counties where there is no health insurance plan participation.
Information on the FHPlus Employer Buy-in program for both managed care plans and potential employers is available on the Department website.
VIII. HEAL NY
During the quarter, the following events and activities occurred within the Health Care Efficiency and Affordability Law for New Yorkers (HEAL NY) grant program.
- Phase 1: Health Information Technology ($52.9 million)
In May 2006, 26 awards were announced. All awardees have fully-executed contracts (one MOU) in place with the Department. Most of the 26 contract projects were completed with 16 fully spent. One contract is still active and two were projects cancelled due to project issues. We are in the process of repurposing any unclaimed funds. - Phase 2: Capital Restructuring Initiatives ($267.7 million)
In November 2006, 53 awards were announced. Contracts were executed for 47 capital restructuring projects. Forty contract projects were completed, 12 were not completed (awards were either withdrawn or rescinded) and one is still active. We are in the process of repurposing any unclaimed funds. - Phase 3: Health Information Technology ($52.8 million)
The Department rebid the $53 million in Phase 3 HEAL-NY funds for health information technology projects as part of Phase 5.
Phase 4: Berger Implementation ($550 million)
Between September 2007 and September 2008, 49 awards were announced in four rounds. Of the 49 grant contracts, the status is as follows: 47 have been approved; one has been developed and is under review; and, one award will not go to contract due to lack of progress. Forty projects have completed their expenditures. We are in the process of repurposing any unclaimed funds. - Phase 5: Health Information Technology: Advancing Interoperability and Community Wide Electronic Health Record Adoption ($105 million)
In April 2008, 19 awards were announced. All of these contracts have been fully executed and are being managed by the Office of Health Information Technology. Sixteen projects have completed their expenditures. - Phase 6: Primary Care Infrastructure ($100 million)
In September 2008, 79 awards were announced. Seventy three contracts are fully executed. The remaining six contracts are under review at the Office of State Comptroller (OSC) or the Department. Forty-four projects have completed their expenditures. - Phase 7: Capital Restructuring Initiatives #2 ($150 million)
In September 2008, 26 awards were announced. Twenty four contracts were fully executed. One award was declined and another contract was rescinded due to significant changes to the scope of the contract. Fourteen projects have completed their expenditures. We are in the process of repurposing any unclaimed funds. - Phase 8: Residential Health Care Facility (RHCF) Rightsizing Demonstration Program ($30 million).
In September 2008, ten awards were announced. Contracts are being developed in the HEAL NY unit in conjunction with the Office of Long Term Care. All contracts were fully executed, but one was rescinded for lack of progress. Four projects have completed their expenditures. We are in the process of repurposing any unclaimed funds. - Phase 9: Local Health Planning Initiatives ($7 million)
In February 2009, a total of 18 awards were announced. Contracts were developed in the Workforce Development Unit and the Office of Rural Health. All contracts have been fully executed. Fourteen contracts have completed their expenditures. We are in the process of repurposing any unclaimed funds. - Phase 10: Health Information Technology - Improving Care Coordination and Management through a Patient Centered Medical Home Model Supported by an Interoperable Health Information Infrastructure ($60 million)
In September 2009, nine awards were announced. All of the contracts are fully executed and are being managed by the Office of Health Information Technology. One project is completed. - Phase 11: Capital Restructuring Initiatives #3 ($175 million)
In September 2009, 25 awards were announced. Of these, 23 contracts are fully executed. One facility, Saint Vincent's Catholic Medical Center has closed and will never go to contract. The remaining contract is in the Department review process. Four projects are fully expended. We are in the process of repurposing any unclaimed funds. - Phase 12: Alternative Long Term Care Initiatives ($175 million)
In September 2009, 19 awards were announced. All contracts have been fully executed. Six contracts are fully expended. We are in the process of repurposing any unclaimed funds. - Phase 13: Primary Care Initiatives
This pool of grant money was initially intended for primary care, but subsequently a decision was made not to issue an Request for Grant Applications (RGA) for that purpose. No grants were ever made under Phase 13. - Phase 14: Discretionary Awards
Finger Lakes Health System: On June 3, 2008, $1,000,000 was awarded to the Department to support local health planning activities. This project has been completed.
Queens Expanding Access Grants: On February 17, 2009, a $15,950,000 grant was awarded to nine facilities in the New York City borough of Queens. The purpose of this grant is to address the public health need associated with the closures of St. John's Queens and Mary Immaculate Hospitals and St. Dominic's Health Center. Funding will be used to restore adequate access to primary care, inpatient care and emergency services. All contracts are fully executed. Four projects have completed their expenditures.
Oswego Health: On May 19, 2009, $17.8 million was awarded to support the operation of a diagnosis and treatment urgent care center at the site of the former A. L. Lee Hospital in Fulton, New York. This contract has been developed but is not fully executed. An additional $8.34 million was awarded to Oswego Hospital on September 4, 2009. This award is for primary care in Oswego County, particularly Central Square. This contract is fully executed.
Health Care Services In Queens: A RGA was issued on August 21, 2009 announcing the availability of $30 million for the support of health care services in Queens. Hospitals, diagnostic and treatment centers are eligible to apply, as are organizations eligible to apply for establishment as diagnostic and treatment centers. As of September 14, 2009, 25 applications had been received. Twelve awards totaling $30,052,135 were announced September 25, 2009. All contracts are fully executed. Four projects have completed their expenditures.
P14 Discretionary - Thirteen awards were made on September 30, 2009; eight to hospitals and clinics totaling $57,340,000 and five to long term care facilities totaling $29,343,798. An additional award of $500,000 was made to Finger Lakes Health System to support research and analysis of local health care services. Eleven contracts are fully executed and one award has been rescinded based on the facility's decision to not move forward with the project. Another project will not go forward due to closure of the facility. Four projects have completed their expenditures.
We are in the process of repurposing any unclaimed funds.
- Phase 15: Medicaid Transition Funding - ($50 million)
Seventy three applications were received by the May 24, 2010 deadline for submission. The selection of 17 award recipients was announced on September 2, 2010. Award letters to the awardees were mailed September 3, 2010. Funds will support capital projects which do the following: 1) help the financial viability of hospitals adversely affected by changes in Medicaid reimbursement enacted in the 2009-10 State Budget; and, 2) serve a large proportion of Medicaid beneficiaries and other underserved populations. Fifteen contracts are fully executed. Two projects have completed their expenditures. - Phase 16: Urgent Care in Greenwich Village- ($14 million)
Grants to support an urgent care facility and other health care services in Greenwich Village for patients displaced by the closure of St. Vincent's Catholic Medical Center were made to 5 facilities. Projects will include an urgent care center providing round-the-clock care, seven days a week, to the Greenwich Village community and expansion of services at four well-established clinics in the St. Vincent's service area. All five contracts are fully executed and two have completed their expenditures. - Phase 17: Health IT - Medical Home ($140 million)
New York State grants will provide fourteen awards to health care organizations within the State to improve the coordination of health care through the use of health information technology (IT) were announced September 10, 2010. The grants will support projects that continue to build health information technology infrastructure in New York State and include statewide collaborative and program evaluation components. Ten contracts are fully executed and are being managed by the Office of Health Information Technology. - Phase 18: Mental Health Mental Health Services - ($30 million)
In September 2010, grants were awarded to 19 hospitals and clinics across New York State totaling $38.5 million to improve the coordination and delivery of inpatient and outpatient mental health services. Fifteen contracts are fully executed. Three projects have completed their expenditures. - Phase 19: Facility Specific Discretionary Awards- ($200 million)
In September 2010, grants were awarded to 32 awards to health care facilities and agencies. An announcement for a continuous acceptance of applications for this series of grants remains posted to the Department of Health (DOH) website. One facility, Ira Davenport Memorial Hospital, declined their award. The remaining 31 contracts are fully executed. Ten projects have completed their expenditures. - Phase 20: Long Term Care Initiatives #2 - ($150 million)
In September 2010, grants were awarded to nine health care facilities and agencies in New York State to improve long-term care services and develop community-based alternatives to traditional nursing home care for older New Yorkers. All contracts are fully executed. - Phase 21 - Restructuring initiatives in Medicaid Redesign - ($450 million)
In November of 2011, the grant opportunity for $450 million under HEAL NY was announced. These funds represent the final major HEAL NY grants under New York State's existing Medicaid 1115 Waiver, which expires March 31, 2014.
In June 2012, grants totaling $301,280,229 were awarded to 40 hospitals and nursing homes. The Department of Health received a diverse group of applications from 99 facilities throughout the state. The awards were distributed equitably among the State's various health planning regions. The balance of the $450 million has been reserved to support additional, actionable projects, including, when developed, efforts to help develop a high-quality, financially secure and sustainable health system in Brooklyn.
Twenty four contracts have been executed and the rest are being developed and processed by the HEAL NY Unit. - All Active Contracts
Letters were sent to 200 plus HEAL grantees with active contracts letting them know that they only had until December 31, 2013 to submit final payment claims, instead of March 31, 2014. The date was moved up to allow claiming data to be entered into the new Statewide Financial System, and to ensure the proper claiming by DOH of federal funds by the end of HEAL/F-SHRP grant program.
IX. Financial, Budget Neutrality Development Issues
Budget Neutrality (BN) is a requirement of Section 1115 waivers which limits federal funding to the amount that would have occurred absent of the waiver. The analysis compares without waiver expenditure limits to with waiver expenditures.
The without waiver amount is an estimated amount for persons eligible for the waiver using the initial PMPMs trended forward by trends included in the terms and conditions times the eligibles. The with waiver amount is equal to the actual expenditures for eligibles. The cost before the waiver (without waiver) must also be greater than the with waiver to have budget neutrality.
There is no allowance for Safety Net or Family Health Plus (members without children) expenditures; these must be funded with the savings.
All persons eligible for the waiver are included in the BN formula whether or not they are enrolled in managed care.
BN is calculated over the entire demonstration, not for each year of the demonstration. BN is a fluid calculation; many changes impact BN. Recipients transitioned from Fee for Service (FFS) to the Managed Care (MC) demographic mix of waiver eligibles changes over time, service utilization trends change, health plan capitation payments change, Medicaid fee schedules change, additional populations are made eligible through waiver amendments.
The current savings for the 1115 waiver is $51B (estimated through the proposed extension 12/31/13). However, this amount is overstated since CMS requires the amounts to match the CMS64, which has some time frames with little or no lag, therefore, understating the with waiver amounts. The actual savings amount is closer to $35B.
- Quarterly Expenditure Report Using CMS-64 and Savings Estimate, Budget Neutrality and Savings Analysis (See Attachment 2)
- Designated State Health Programs (See Attachment 3)
- Reform Initiatives (See Attachment 4)
- Hospital and Nursing Home Data (See Attachment 5)
X. Other
- Integrated Programs
The Medicaid Advantage program allows dually eligible individuals to voluntarily enroll in an approved Medicare Advantage plan that also has a Medicaid managed care product to receive most of their Medicare and Medicaid benefits. As of November 2012, 9,009 individuals in 24 upstate counties and New York City were enrolled in 13 Medicaid Advantage plans. - Changes to Certificates of Authority:
No Changes. - Consumer Issues
Medicaid Advantage plans reported a total of 20 complaints and action appeals as of November 2012.
XI. Transition Plan Updates
There are no updates to the transition plan for this quarter. The Department continues to explore the necessary system and program changes needed to implement the Affordable Care Act.
Attachments
- Contact:
Mark Bertozzi
Director of Bureau of Administration
One Commerce Plaza
Albany, NY 12237
Phone: 518-473-5876
Fax: 518-473-5508
Submitted on: December 31, 2012
ATTACHMENT 2
New York State Partnership Plan
Projected 1115 Waiver Budget Neutrality Impact Through December 2013
| Budget Neutrality Cap (Without Waiver) | DY 1 - 11 (10/1/97 - 9/30/09) Projected | DY 12 (10/1/09-9/30/10) Actual | DY 13A 10/1/10-3/31/11) Projected | DY 13B (4/1/11-9/30/11) Projected | DY 14 (10/1/11-9/30/12) Projected | DY 15 (10/1/12-9/30/13) Projected | DY 16 (10/1/13-12/31/13) Projected | BIPA Extension (10/1/09 - 12/31/13) Projected | DY 1 - 15 (10/1/97 - 12/31/13) Projected |
|---|---|---|---|---|---|---|---|---|---|
| demonstration Group 1 - TANF Children under age 1 through 20 | $11,197,206,500 | $6,105,699,488 | $6,123,530,693 | $13,981,603,311 | $15,455,268,043 | $4,137,807,371 | $57,001,115,405 | ||
| Demonstration Group 2 - TANF Adults 21-64 | $4,511,421,595 | $2,467,348,368 | $2,454,367,076 | $5,635,908,331 | $6,224,033,160 | $1,663,421,971 | $22,956,500,500 | ||
| Demonstration Group 6 - FHP Adults w/Children | $1,878,516,641 | $1,043,047,420 | $1,061,365,979 | $2,344,366,724 | $2,609,395,833 | $713,869,831 | $9,650,562,428 | ||
| Demonstration Group 6A - FHP Adults w/Children @ 160% | $0 | $0 | $0 | $0 | $0 | $0 | $0 | ||
| Demonstration Group 8 - Family Planning Expansion | $5,140,241 | $10,702,271 | $11,139,306 | $2,897,896 | $29,879,714 | ||||
| W/O Waiver Total | $187,390,575,140 | $17,587,144,736 | $9,616,095,275 | $9,644,403,988 | $21,972,580,637 | $24,299,836,341 | $6,517,997,069 | $89,638,058,047 | $277,028,633,187 |
| Budget Neutrality Cap (With Waiver) | DY 1 - 11 (10/1/97 - 9/30/09) Projected | DY 12 (10/1/09-9/30/10) Actual | DY 13A 10/1/10-3/31/11) Projected | DY 13B (4/1/11-9/30/11) Projected | DY 14 (10/1/11-9/30/12) Projected | DY 15 (10/1/12-9/30/13) Projected | DY 16 (10/1/13-12/31/13) Projected | BIPA Extension (10/1/09 - 12/31/13) Projected | DY 1 - 14 (10/1/97 - 12/31/13) Projected |
|---|---|---|---|---|---|---|---|---|---|
| demonstration Group 1 - TANF Children under age 1 through 20 | $4,144,199,750 | $1,827,792,863 | $2,601,977,167 | $6,033,438,430 | $6,651,329,935 | $1,767,244,953 | $23,025,983,098 | ||
| Demonstration Group 2 - TANF Adults 21-64 | $2,619,299,634 | $1,159,889,284 | $1,487,941,873 | $3,497,627,598 | $3,860,574,983 | $1,028,253,292 | $13,653,586,664 | ||
| Demonstration Group 5 - Safety Net Adults | $4,024,374,518 | $1,864,361,807 | $3,400,994,019 | $8,410,811,517 | $10,144,634,210 | $2,690,451,564 | $30,535,627,635 | ||
| Demonstration Group 6 - FHP Adults w/Children up to 150% | $963,020,020 | $502,539,894 | $560,735,692 | $1,179,549,495 | $1,307,464,677 | $356,244,880 | $4,869,554,658 | ||
| Demonstration Group 7 - FHP Adults without Children up to 100% | $313,222,949 | $155,882,395 | $154,684,278 | $330,264,237 | $374,046,202 | $103,281,236 | $1,431,381,296 | ||
| Demonstration Group 6A - FHP Adults w/Children @ 160% | $0 | $0 | $0 | $0 | $0 | $0 | $0 | ||
| Demonstration Group 7A - FHP Adults without Children @ 160% | $0 | $0 | $0 | $0 | $0 | $0 | $0 | ||
| Demonstration Group 8 - Family Planning Expansion | $9,839,735 | $4,164,485 | $5,460,394 | $11,576,340 | $12,272,547 | $3,252,352 | $46,565,853 | ||
| Demonstration Group 9 - Home and Community Based Expansion (HCBS) | N/A | N/A | $3,699,108 | $3,699,108 | $3,699,108 | $924,777 | $12,022,101 | ||
| Demonstration Population 1: State Indigent Care Pool Direct Expenditures (ICP-Direct) | $2,600,000 | $14,650,000 | $13,700,000 | $3,400,000 | $34,350,000 | ||||
| Demonstration Population 2: Designated State Health Programs to Support Clinic Uncompensated Care Funding (ICP - DSHP) | $2,600,000 | $14,650,000 | $13,700,000 | $3,400,000 | $34,350,000 | ||||
| Demonstration Population 3: Designated State Health Programs to Support Medical Home Demonstration (DSHP - HMH Demo) | $0 | $133,400,000 | $133,300,000 | $33,300,000 | $300,000,000 | ||||
| Demonstration Population 4: Designated State Health Programs to Support Potentially Preventable Readmission Demonstration (DSHP - PPR Demo) | $0 | $5,000,000 | $6,700,000 | $1,600,000 | $13,300,000 | ||||
| With Waiver Total | $151,007,816,586 | $12,073,956,605 | $5,514,630,728 | $8,220,692,530 | $19,634,666,726 | $22,521,421,662 | $5,991,353,054 | $73,956,721,305 | $224,964,537,890 |
| Expenditures (Over)/Under Cap | $36,382,758,554 | $5,513,188,131 | $4,101,464,547 | $1,423,711,458 | $2,337,913,911 | $1,778,414,679 | $526,644,016 | $15,681,336,742 | $52,064,095,296 |
New York State Partnership Plan
PMPM´s and Member Months
| WITHOUT WAIVER PMPMS | ||||||
|---|---|---|---|---|---|---|
| DY12 2009-2010 | DY13 2010-2011 (2 Qtrs) | DY13 2010-2011 (2 Qtrs) | DY14 2011-2012 | DY15 2012-2013 | DY16 2013-2014 (1 Qtr) | |
| TANF Kids | $585.99 | $624.67 | $624.67 | $665.90 | $709.85 | $756.70 |
| TANF Adults | $801.34 | $852.63 | $852.63 | $907.20 | $965.26 | $1,027.04 |
| FHPlus Adults with Children | $625.55 | $665.59 | $665.59 | $708.19 | $753.51 | $801.73 |
| Family Planning Expansion | $20.23 | $21.06 | $21.92 | $22.81 | ||
| WITH WAIVER PMPMS | ||||||
|---|---|---|---|---|---|---|
| DY12 2009-2010 | DY13 2010-2011 (2 Qtrs) | DY13 2010-2011 (2 Qtrs) | DY14 2011-2012 | DY15 2012-2013 | DY16 2013-2014 (1 Qtr) | |
| TANF Kids | $216.88 | $187.00 | $265.43 | $287.35 | $305.49 | $323.18 |
| TANF Adults | $465.25 | $400.82 | $516.90 | $563.01 | $598.72 | $634.87 |
| SN - Adults | $539.39 | $454.35 | $806.53 | $924.53 | $1,035.36 | $1,088.75 |
| FHPlus Adults with Children | $320.69 | $320.68 | $351.64 | $356.32 | $377.55 | $400.09 |
| FHPlus Adults without Children | $352.04 | $361.75 | $353.78 | $358.59 | $379.64 | $402.08 |
| Family Planning Expansion | $20.27 | $16.39 | $21.49 | $22.70 | $24.15 | $25.60 |
| MEMBER MONTHS | ||||||
|---|---|---|---|---|---|---|
| DY12 2009-2010 | DY13 2010-2011 (2 Qtrs) | DY13 2010-2011 (2 Qtrs) | DY14 2011-2012 | DY15 2012-2013 | DY16 2013-2014 (1 Qtr) | |
| TANF Kids | 19,108,187 | 9,774,280 | 9,802,825 | 20,996,551 | 21,772,583 | 5,468,227 |
| TANF Adults | 5,629,847 | 2,893,809 | 2,878,584 | 6,212,421 | 6,448,038 | 1,619,627 |
| SN - Adults | 7,460,970 | 4,103,355 | 4,216,837 | 9,097,365 | 9,798,142 | 2,471,136 |
| FHPlus Adults with Children | 3,002,984 | 1,567,102 | 1,594,624 | 3,310,364 | 3,462,988 | 890,412 |
| FHPlus Adults without Children | 889,734 | 430,909 | 437,231 | 921,016 | 985,257 | 456,870 |
| Family Planning Expansion | 485,446 | 254,090 | 254,090 | 508,180 | 508,180 | 127,045 |
New York State Department of Health
Federal-State Health Reform Partnership (F-SHRP)
Report of Reform Initiatives For the Period 07/1/12 - 09/30/12
| Awards Under FFY 2007 | ||||||
|---|---|---|---|---|---|---|
| Awards Made Prior Periods | Awards This Period | Total Awards to Date | Expenditures Prior Periods | Expenditures this Period | Expenditures to Date | |
| HEAL NY Phase 2 Restructuring | $230,831,661 | $230,831,661 | $187,236,215 | $1,173,306 | $188,409,521 | |
| Community Health Center Capital Program | $10,000,000 | $10,000,000 | $4,293,898 | $2,537,601 | $6,831,499 | |
| Displaced Worker Program | $12,614,885 | $12,614,885 | $11,618,214 | $11,618,214 | ||
| HEAL NY Phase 4: Implementation of Commission Mandates | $362,299,349 | $362,299,349 | $330,256,357 | $178,756 | $330,435,113 | |
| $615,745,895 | $0 | $615,745,895 | $533,404,684 | $3,889,663 | $537,294,347 | |
| Awards Under FFY 2008 | ||||||
|---|---|---|---|---|---|---|
| Awards Made Prior Periods | Awards This Period | Total Awards to Date | Expenditures Prior Periods | Expenditures this Period | Expenditures to Date | |
| HEAL NY Phase 4: Implementation of Commission Mandates | $187,700,651 | $187,700,651 | $178,862,344 | $374,217 | $179,236,561 | |
| HEAL NY Phase 5: Health IT | $104,944,003 | $104,944,003 | $102,196,641 | $102,196,641 | ||
| HEAL NY Phase 6: Primary Care Services | $99,885,522 | $99,885,522 | $71,592,272 | $3,760,197 | $75,352,469 | |
| HEAL NY Phase 7: Berger Lookalikes and coverage partners | $149,951,753 | $149,951,753 | $118,725,152 | $5,273,121 | $123,998,273 | |
| HEAL NY Phase 8: Nursing Home Rightsizing | $30,000,000 | $30,000,000 | $17,604,928 | $1,684,517 | $19,289,445 | |
| $572,481,929 | $0 | $572,481,929 | $488,981,337 | $11,092,051 | $500,073,389 | |
| Awards Under FFY 2009 | ||||||
|---|---|---|---|---|---|---|
| Awards Made Prior Periods | Awards This Period | Total Awards to Date | Expenditures Prior Periods | Expenditures this Period | Expenditures to Date | |
| HEAL NY Phase 10: Health IT | $99,914,713 | $99,914,713 | $40,373,152 | $6,798,578 | $47,171,730 | |
| HEAL NY Phase 11: Restructuring* | $174,343,776 | $174,343,776 | $54,290,228 | $8,513,034 | $62,803,263 | |
| HEAL NY Phase 12: Long Term Care* | $172,363,541 | $172,363,541 | $99,079,394 | $8,340,405 | $107,419,799 | |
| HEAL NY Phase 14(Q) - Targeted Hospitals, Queens | $15,950,000 | $15,950,000 | $15,011,782 | $15,011,782 | ||
| HEAL NY Phase 14(Q2) - Targeted Hospitals, Queens | $30,052,135 | $30,052,135 | $9,743,687 | $2,898,970 | $12,642,657 | |
| HEAL NY Phase 14(Os) - Targeted Hospitals, Oswego | $17,800,000 | $17,800,000 | $17,604,459 | $26,886 | $17,631,345 | |
| HEAL NY Phase 14(D) - Targeted Hospitals, Discretionary | $87,183,798 | $87,183,798 | $45,698,963 | $2,289,069 | $47,988,032 | |
| $597,607,963 | $0 | $597,607,963 | $281,801,666 | $28,866,942 | $310,668,608 | |
| Awards Under FFY 2010 | ||||||
|---|---|---|---|---|---|---|
| Awards Made Prior Periods | Awards This Period | Total Awards to Date | Expenditures Prior Periods | Expenditures this Period | Expenditures to Date | |
| HEAL NY Phase 15 - Medicaid Transition Funding | $49,927,203 | $49,927,203 | $11,710,832 | $2,533,921 | $14,244,754 | |
| HEAL NY Phase 16 - Ambulatory Care Lower Manhattan | $14,000,000 | $14,000,000 | $2,462,890 | $2,462,890 | ||
| HEAL NY Phase 17 - Health IT in Expanded Care Coordination | $138,575,701 | $138,575,701 | $28,931,425 | $3,540,558 | $32,471,983 | |
| HEAL NY Phase 18 - Mental Health Services | $38,501,949 | $38,501,949 | $9,375,376 | $502,410 | $9,877,786 | |
| HEAL NY Phase 19 - Facility Specific Reconfiguration | $200,181,491 | $200,181,491 | $104,220,874 | $15,484,335 | $119,705,209 | |
| HEAL NY Phase 20 - Long Term Care Initiatives #2 | $150,794,505 | $150,794,505 | $47,780,306 | $17,094,276 | $64,874,582 | |
| $591,980,849 | $0 | $591,980,849 | $204,481,703 | $39,155,501 | $243,637,204 | |
| Awards After FFY 2010 | ||||||
|---|---|---|---|---|---|---|
| Awards Made Prior Periods | Awards This Period | Total Awards to Date | Expenditures Prior Periods | Expenditures this Period | Expenditures to Date | |
| HEAL NY Phase CD - Commissioner´s Discretion (PHL Section 2818(6)) |
$8,957,680 | $8,957,680 | $0 | $3,600,000 | $3,600,000 | |
| HEAL NY Phase 21 - Restructuring Initiatives in Medicaid Redesign | $295,683,549 | $295,683,549 | $0 | $0 | ||
| $304,641,229 | $0 | $304,641,229 | $0 | $3,600,000 | $3,600,000 | |
| Awards Made Prior Periods | Awards This Period | Total Awards to Date | Expenditures Prior Periods | Expenditures this Period | Expenditures to Date | |
|---|---|---|---|---|---|---|
| Total All Health Reform Programs | $2,682,457,865 | $0 | $2,682,457,865 | $1,508,669,390 | $86,604,157 | $1,595,273,548 |
Signed: Date:
Name: Marybeth Hefner
Title: Director, Bureau of Accounts Management
Attachment IV
Federal-State Health Reform Partnership (F-SHRP)
Designated State Health Program Claim Sources
Demonstration Year 6 (October 1, 2011 - September 30, 2012)
Documented Cash Disbursements to Date
| Agency/Program | Claim Period | 1-3/12 QER | Total | |||||
|---|---|---|---|---|---|---|---|---|
| DOH | ||||||||
| AIDS Drug Assistance Program | 10-12/11 | $3,909,434 | $3,909,434 | |||||
| 1-3/12 | $0 | |||||||
| 4-6/12 | $0 | |||||||
| 7-9/12 | $0 | |||||||
| Healthy New York | 10-12/11 | $0 | ||||||
| 1-3/12 | $0 | |||||||
| 4-6/12 | $0 | |||||||
| 7-9/12 | $0 | |||||||
| Tobacco Control Program | 10-12/11 | $0 | ||||||
| 1-3/12 | $0 | |||||||
| 4-6/12 | $0 | |||||||
| 7-9/12 | $0 | |||||||
| Health Workforce Retraining | 10-12/11 | $0 | ||||||
| 1-3/12 | $0 | |||||||
| 4-6/12 | $0 | |||||||
| 7-9/12 | $0 | |||||||
| Recruitment and Retention of Healthcare Workers | 10-12/11 | $0 | ||||||
| 1-3/12 | $0 | |||||||
| 4-6/12 | $0 | |||||||
| 7-9/12 | $0 | |||||||
| Pay for Performance Demonstration | 10-12/11 | $0 | ||||||
| 1-3/12 | $0 | |||||||
| 4-6/12 | $0 | |||||||
| 7-9/12 | $0 | |||||||
| Telemedicine Demonstration | 10-12/11 | $0 | ||||||
| 1-3/12 | $0 | |||||||
| 4-6/12 | $0 | |||||||
| 7-9/12 | $0 | |||||||
| Early Intervention Services | 10-12/11 | $0 | ||||||
| 1-3/12 | $0 | |||||||
| 4-6/12 | $0 | |||||||
| 7-9/12 | $0 | |||||||
| SOFA | ||||||||
| Community Services for the Elderly | 10-12/11 | $0 | ||||||
| 1-3/12 | $0 | |||||||
| 4-6/12 | $0 | |||||||
| 7-9/12 | $0 | |||||||
| Expanded In-Home Services to the Elderly Program | 10-12/11 | $0 | ||||||
| 1-3/12 | $0 | |||||||
| 4-6/12 | $0 | |||||||
| 7-9/12 | $0 | |||||||
| OMRDD | ||||||||
| Residential and Community Support Services | 10-12/11 | $0 | ||||||
| 1-3/12 | $0 | |||||||
| 4-6/12 | $0 | |||||||
| 7-9/12 | $0 | |||||||
| OCFS | ||||||||
| Services to Special Education Children | 10-12/11 | $0 | ||||||
| 1-3/12 | $0 | |||||||
| 4-6/12 | $0 | |||||||
| 7-9/12 | $0 | |||||||
| Total | $3,909,434 | $0 | $0 | $0 | $0 | $0 | $3,909,434 | |
| Federal Share | $1,954,717 | $0 | $0 | $0 | $0 | $0 | ||
| Claims Reported to Date | $3,909,434 | $3,909,434 | $3,909,434 | $3,909,434 | $3,909,434 | $3,909,434 | ||
| Federal Share | $1,954,717 | $1,954,717 | $1,954,717 | $1,954,717 | $1,954,717 | $1,954,717 | ||
Attachment V
New York State Medicaid
Inpatient and Nursing Home Information
FFS Expenditures, Eligible Months, Days and Discharges
July 1, 2012 through September 30, 2012
| Q2: October 1, 2011 - March 31, 2012* | |||||
|---|---|---|---|---|---|
| Inpatient Hospital | Medicaid Expenditures | Medicaid Discharges | Medicaid Cost Per Discharges | Medicaid Member months | Discharges PMPY |
| Medicaid FFS | $ 1,480,003,858 | 134,329 | $ 11,018 | 6,334,606 | 0.25 |
| Managed Care** | $ 2,015,067,446 | 249,070 | $ 8,090 | 20,757,690 | 0.14 |
| Total Medicaid | $ 3,495,071,304 | 383,399 | $ 9,116 | 27,092,296 | 0.17 |
| Q2: October 1, 2011 - March 31, 2012* | |||||
|---|---|---|---|---|---|
| Nursing Home | Medicaid Expenditures | Medicaid Days | Medicaid Cost Per Day | Medicaid Member months | Days PMPY |
| Medicaid FFS | $ 3,094,986,211 | 14,539,252 | $ 213 | 6,334,606 | 27.54 |
| Managed Care** | $ 86,162,407 | 302,801 | $ 285 | 20,939,260 | 0.17 |
| Total Medicaid | $ 3,181,148,618 | 14,842,053 | $ 214 | 27,273,866 | 6.53 |
*For discharges paid through September 2012
**Managed care data includes an estimate for under-reporting of hospital encounter data
Managed care cost is a blended rate of plan paid claims and encounter proxy costs during the time period.
Managed care member months used for nursing home calculation include managed long-term care member months as the nursing home utilization for those members is in the managed care utilization.
Follow Us