42 CFR 438 Service Authorization and Appeals
MLTC: Partial Cap, MAP, Medicaid Advantage
- Presentation also available in Portable Document Format (PDF)
Bureau of Managed Long Term Care
Office of Health Insurance Programs
December 7, 2017
Welcome
- This presentation is for MLTC plans: Partial Cap and benefit determinations for MAP and Medicaid Advantage products
- Goals for today:
- Describe implementation steps related to full compliance with 42 CFR 438 for service authorization and appeal processes
- Highlight impacts of the 2016 Mega Rule on these processes
- Review appropriate use of the template notices
- Confirm the template notice approval process
Reminders
- This webinar is being recorded
- PLEASE:
- Type any questions into the Q & A box feature
- For plan specific or detailed questions, email MLTCmodelnotices@health.ny.gov
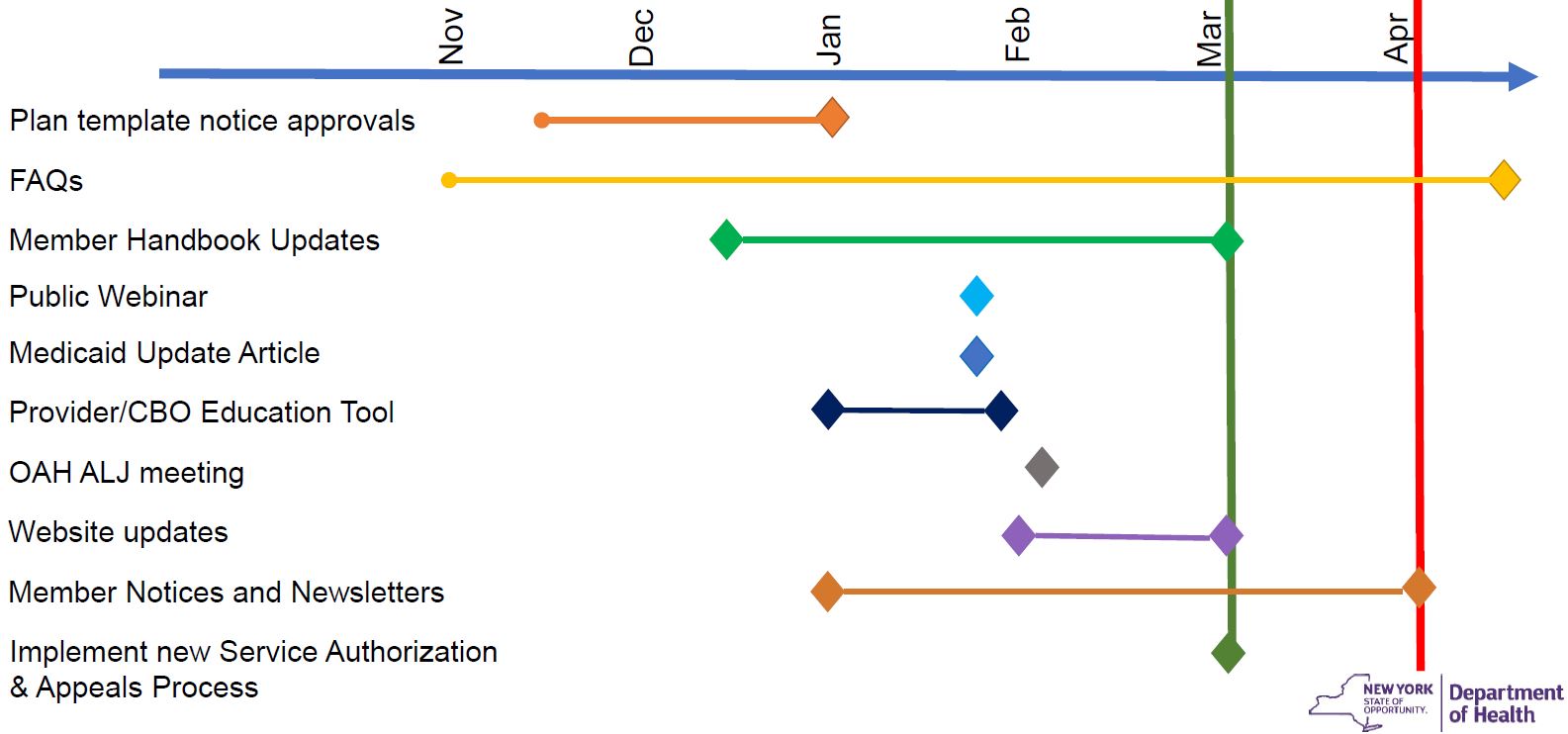
Implementation Timeline
Questions?
Are we speaking the same language?
| 42 CFR 438 | MLTC Model Contract | Template |
|---|---|---|
| Service Authorization Request | Services Authorization Request | You asked for [service] |
| Adverse Benefit Determination | Action | Decision to deny, reduce, suspend, stop |
| Notice of Adverse Benefit Determination | Notice of Action | Initial Adverse Determination |
| Appeal | Action Appeal | Plan Appeal |
| Notice of Appeal Resolution | Notice of Action Appeal Determination | Final Adverse Determination |
| Continuation of Benefits | Aid Continuing | Keep your services the same |
| External Medical Review | External Appeal | External Appeal |
| Grievance | Grievance | Complaint |
42 CFR 438 Impact on Service Authorizations and Appeals
| Changed Regulation: | Impact Summary: |
|---|---|
| 438.210(d)(2)(i) | Changes expedited authorization decision/notice timeframe to 72 hours subject to extension. This is a change from 3 business days |
| 438.402(c)(1)(i) 438.408(f)(1) Enrollee has to exhaust the internal appeal process prior to going to Fair Hearing |
Establishes the enrollees right to a Fair Hearing regarding an adverse benefit determination after receipt of notice under 438.408 (appeal resolution) that the adverse benefit determination has been upheld.
|
| 438.402(c)(1)(i)(A) 438.408(c)(3) 438.408(f)(1)(i) |
Defines ´deemed exhaustion´ – the enrollee has exhausted the plan´s appeal process if the notice and timing requirements of 438.408 (appeal resolution) have not been met and may request a fair hearing.
|
| 438.402(c)(1)(ii) | Adds requirement for enrollee´s written consent for representatives to request plan appeal, grievance or fair hearing on their behalf. Providers may request appeal, grievance or fair hearing but may not request Aid Continuing.
|
| 438.402(c)(2)(ii) | Requires appeals to be filed within 60 calendar days of the date on the Initial Adverse Determination |
| 438.404(b)(2) | Notices identify the right to request and receive, free of charge, copies of all sources of information relevant to the adverse determination
|
| 438.406(b)(5) Suggestion: Send case file with acknowledgement |
Requires provision of case file free of charge and sufficiently in advance of resolution timeframes for appeals to enrollee and representative.
|
| 438.408(b)(3) Change from 3 BD |
Changes expedited appeal determination/notice timeframe to 72 hours |
| 438.408(c)(2) | Plans must make reasonable efforts to give prompt oral notice of an extension and written notice within 2 calendar days |
| 438.408(f) Change from 60 days |
Provides enrollees 120 calendar days from the date of an adverse appeal resolution notice to request a fair hearing. |
| 438.420 We are going back to the process that was in place prior to July 2015 If member uses the Appeal form, AC should be provided unless the member checks the box indicating they don´t want it |
Provides enrollees the right to Aid Continuing upon timely filing of an appeal – 10–days of the notice of adverse benefit determination or by the effective date of the adverse benefit determination, whichever is later. Provides aid continuing without interruption if the enrollee requests a fair hearing within 10 days of the plan´s sending the written adverse appeal resolution notice.
|
| 438.424(a) | If the fair hearing decision reverses the plan´s adverse benefit determination, and the disputed services were not provided while the appeal and hearing were pending, the plan must authorize or provide the disputed services promptly and as expeditiously as the enrollee´s condition requires but no later than 72 hours from the date the plan receives the fair hearing decision. |
Standard MLTC Prior Authorizations and Appeals Process*
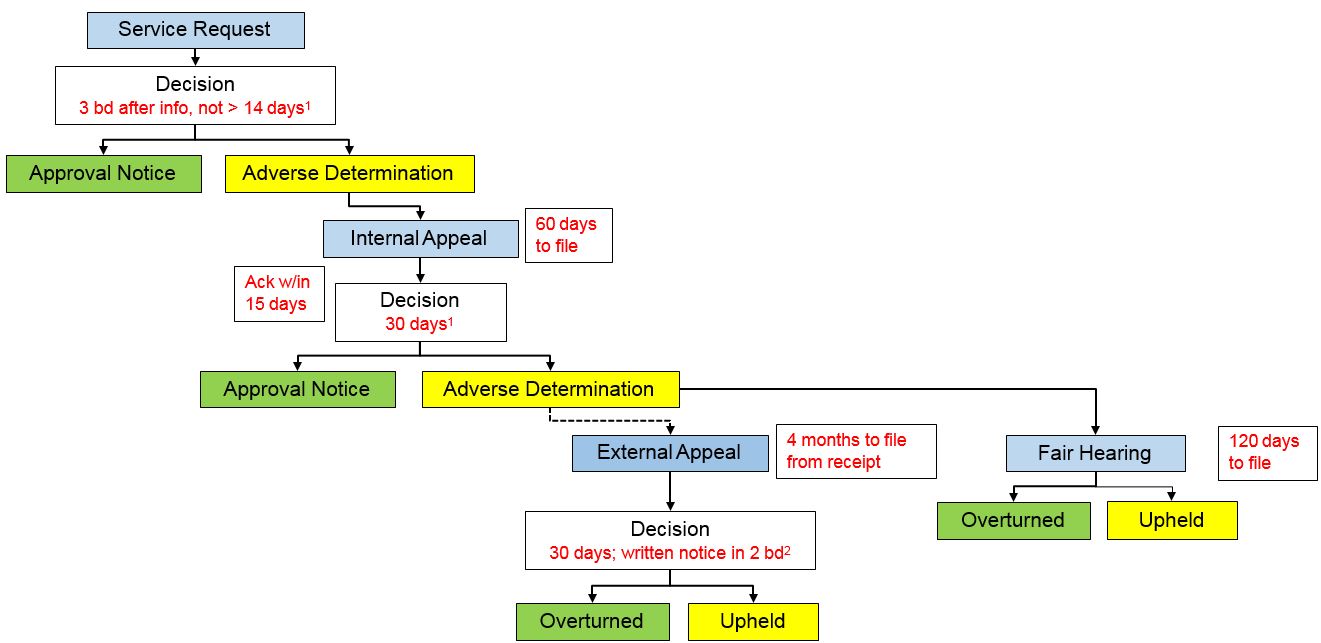
______________________________
1 possible extension of up to 14 days
2 possible extension of up to 5 bd
*Please see for NYS MLTC Service Authorization and Appeals Timeframe Comparison for more information
Standard MLTC Complaint Process*
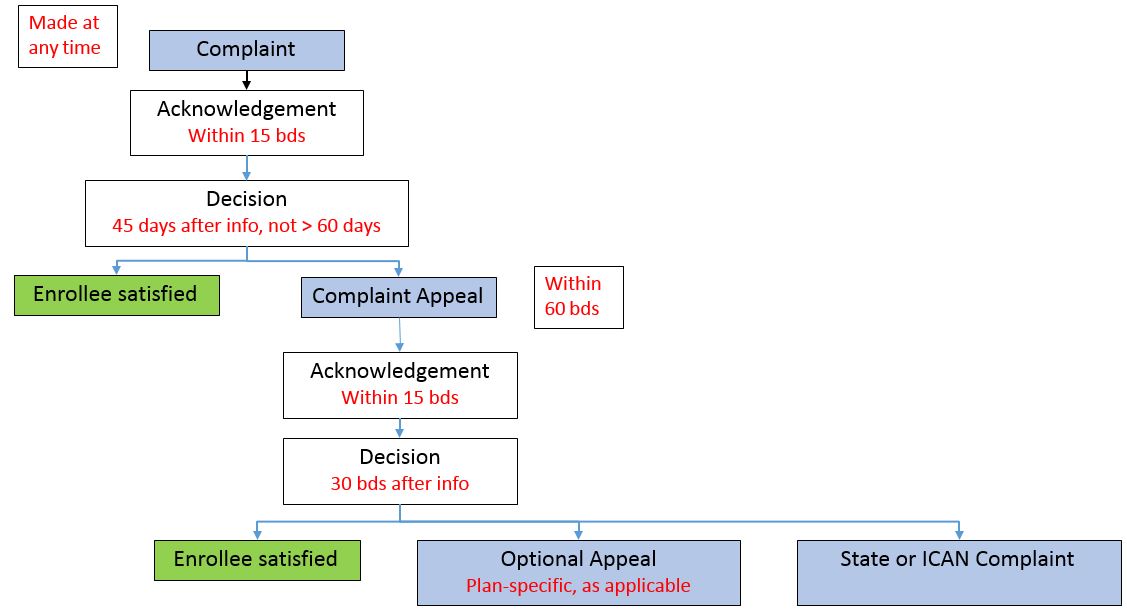
*Please see Grievances Timeframe Chart for more information
Questions?
Template Notices – Purpose and Use
- 42 CFR 438.10(c)(4)(ii) requires the use of model enrollee notices
- The State developed the template notices with significant input of the Service Authorization and Appeals Stakeholder Workgroup
- There are now eight model templates:
- Approval: approval of a services authorization request or whole overturn of an adverse benefit determination on appeal
- Extension: extension for more information during service authorization request review or appeal
- Initial Adverse Determination No AC: notice of adverse benefit determination
- Initial Adverse Determination With AC
- Final Adverse Determination No AC: adverse notice of appeal resolution (adverse benefit determination upheld in whole or in part)
- Final Adverse Determination With AC
- Complaint Resolution
- Complaint Appeal Resolution
- 2015 IAD combined all rights, with separate appeals attachment and fair hearing form to be used for any type of denial
- 2017 templates for IADs and FADs are split by decisions where the enrollee does or does not have a right to aid continuing.
- 2017 FADs are one notice – combined plan decision and Fair Hearing rights – no separate fair hearing form.
Notice Process and Timeframes
- New charts have been finalized indicating the blended time frames for compliance with PHL and 42 CFR 438 for service authorization requests, appeals, complaints and complaint appeals. Which we will be forwarding after presentation
- Plan policies and procedures must be updated to comply with the new timeframes
- New notices and exhaustion/AC processes may not be utilized prior to March 1, 2018. These apply to adverse benefit determination made on March 1, 2018 and thereafter.
- For enrollees who receive an action taken notice prior to March 1, 2018 and subsequently appeals or requests a fair hearing after March 1, 2018, the appeal or fair hearing will be considered timely and handled pursuant to the rights issued in the action notice (old rules).
- If the enrollee appeals, the plan´s appeal resolution will be the new FAD and the enrollee will receive the right to request a fair hearing within 120 days (new rules).
Template Notices – Clinical rationale/specific reason for denial
- During the stakeholder workgroup meeting 3, we reviewed poor clinical rationales and explored ways to improve noticing, including emphasis on plain language and reduction of extraneous information
- DOH restructured model notice templates placeholder language to improve the inclusion of all required elements for these decisions
Specific Denial Reason Requirements:
For benefit denials:- 4th–6th grade reading level
- Grounds for appeal must be easily identifiable
- Must include the specific service that is not covered
- For benefit coverage that is dependent on the enrollee´s condition, must include the specific benefit criteria that is not being met (e.g., dental, personal care, etc.)
- Examples:
- Family planning services are not covered under our benefit package. You may use your Medicaid card to obtain this service from any provider that accepts Medicaid.
- Root canals for tooth #18 (wisdom tooth) are not covered by Medicaid unless the tooth is needed to support a dental device or you need the tooth to be able to chew. You do not wear a dental device, and you have at least eight teeth in contact with each other and are able to chew without this tooth.
Out of Network (OON) IAD
For benefit denials:- 4th–6th grade reading level
- Grounds for appeal must be easily identifiable
- OON service denials for service that are not materially different must include a description of the service available in–network, why it is not materially different, and how to access the in–network service.
- OON referral denials for services requested based on the training and experience of a provider must include contact information for in–network providers available and able to provide the requested service.
Out–of–Network Example:
- OON Denial:
You requested outpatient physical therapy from Great PT Inc. You do not need to get these services outside of our network because we have providers who can give them to you. The in–network providers listed below are available to provide outpatient physical therapy and have the correct training and experience to meet your needs.
Dr. Smith
111 Main Street
New York, NY 10101
Phone: 212–555–5555
Dr. Brown
99 First Street
New York, NY 10001
Phone: 212–555–7777
Clinical Rationale Requirements:
- 4th– 6th grade reading level
- Grounds for appeal must be easily identifiable
- Must include for service request:
- the service requested;
- the enrollee´s condition;
- why the service was requested or how the service was intended to treat or improve the enrollee´s condition;
- the specific criteria that must be met for the service to be approved including the identification/ name of the criteria and a description of what is actually necessary to get the service approved;
- enrollee–specific information about why the decision was made including how the criteria was not met
- If this is a change to a service that has already been approved, the change to the enrollee´s condition impacting the level of care needed and when the change occurred must be included.
Updates to Specific Denial Reason/ Clinical Rationale Placeholders for LTSS
{INSERT IF THE DECISION IS ABOUT LTSS REQUEST FOR A NEW SERVICE OR FOR MORE OF A CURRENT SERVICE (CLINICAL OR ADMINISTRATIVE), OR DELETE THIS SEGMENT}
- The request for [service] was [denied] [partially approved]. This decision was based on:
- [Insert the criteria requirements and other information relied on to make the decision.].
- [Insert enrollee–specific details, including medical condition, social, or environmental circumstances that support the decision and illustrate how/why criteria for coverage was not met.].
{Note: The rationale must be sufficiently specific to enable the enrollee to determine the basis for appeal.}
Clinical Rationale for LTSS Service Request Example:
- The request for an increase in Personal Care Service from 24 hour live–in to 24 hour split shift (2x12) was denied. This decision was based on:
- 24 hour split shift of continuous personal care means the provision of care by more than one personal aide for more than 16 hours in a calendar day for a member who because of their medical condition needs assistance with toileting, walking, transferring, turning and positioning, or feeding, and needs assistance with such frequency that a live–in 24 hour personal care aide would be unlikely to obtain, on a regular basis, 5 hours daily of uninterrupted sleep during the aide´s 8 hour period of sleep.
- A sleep study was done 11/1/17. The member fell asleep at 11pm and woke up requesting to go to the bathroom at 5am. Member did not require turning or positioning at night. Current 24 hour live–in aide reported getting at least 5 hours of uninterrupted sleep per night.
- Therefore, the member´s needs are met with 24 hour live–in personal care aide.
Updates to Specific Clinical Rationale Placeholders for LTSS
{INSERT IF THE DECISION IS ABOUT LTSS STOPPAGES, REDUCTIONS, OR SUSPENSIONS (CLINICAL OR ADMINISTRATIVE), OR DELETE THIS SEGMENT}
- [Insert service] will be [stopped][reduced][suspended] because:
- [Indicate the change in medical condition, social, or environmental circumstances since the previous authorization was made.]
- [Indicate when the change occurred. Include the information and criteria relied on to make the decision.]
- You no longer meet the criteria for your current level of service because:
- [Describe why or how the change in medical condition, social, or environmental circumstances no longer meet the criteria for the previous authorization.]
{Note: The rationale must be sufficiently specific to enable the enrollee to determine the basis for appeal.}
Clinical Rationale LTSS Reduction Example:
- Your Level 2 Personal Care Services 4 hours per day, 5 days per week will be reduced to 2 hour per day, 5 days per week because:
- In March 2017 you fractured your hip, and your condition has since improved. You no longer need the same level of care with personal hygiene tasks and mobility.
- Your current services were approved based on your 3/15/17 UAS–NY results. At that time, you needed extensive assistance with both personal hygiene tasks and mobility. On 9/1/17, you had a UAS–NY completed. At this time, your needs show limited assistance with certain personal hygiene tasks and mobility.
- You no longer meet the criteria for your current level of service because:
- Based on your 9/1/17 assessment, you now only need some hands–on help for bathing and dressing. You now only need limited assistance when walking around your home and in the community.
- We are reducing your Personal Care Services because you do not need the level of service that was previously approved.
Questions?
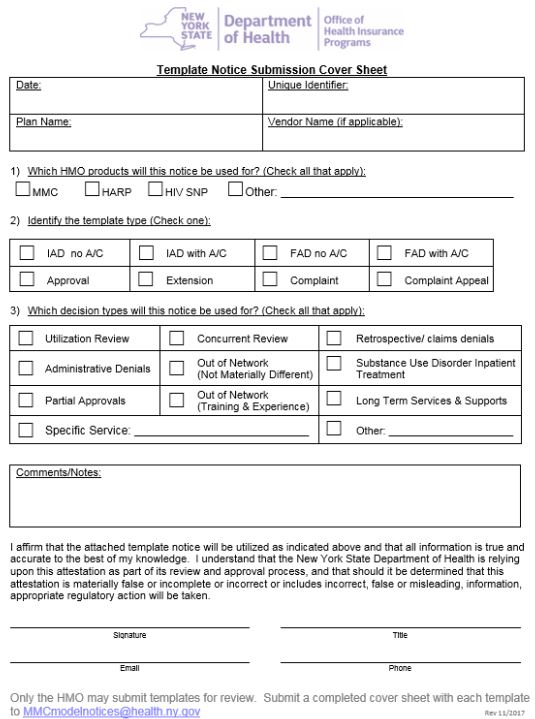
Template Approval Process
- All template notices must be submitted to the Department prior to use
- 2017 templates may not be used prior to May 1, 2018.
- Only MLTCs may submit templates for approval.
- A Notice Submission Cover Sheet must be submitted for EACH template
- A plan–created unique identifier must appear on the cover sheet and in the footer on each page of the template
- Plans are required to follow the model template language
- The Submission Cover Sheet identifies the intended purpose of each template
- Incomplete submissions will be returned
- Upon completion of the review, the plan will receive an approval or if revisions are needed, details highlighting needed changes.
Questions?
Next Steps
- Submit templates no later than December 15, 2017
- Additional guidance materials and FAQs will be provided
Thank You!
Please send comments or questions to: 438reg@health.ny.gov
Submit template notices or specific MLTC questions to: MLTCmodelnotices@health.ny.gov