2018 Medicaid Managed Care Quality Incentive Report
A Report on the Medicaid Managed Care Quality Incentive Program In New York State
- Report also available in Portable Document Format (PDF)

health.ny.gov
Table of Contents
Section 1: Background
New York's Medicaid Managed Care Quality Incentive Program began in early 2001. In 2002, the program was expanded to provide increased incentives for improvement. Plans became eligible to receive bonuses added to the premium based upon composite scores from quality measures and satisfaction measures. The bonus was later increased in 2005 to its current value. The Quality Incentive Program continues to evolve over the years and includes new components and measures as well as a refined methodology to calculate current performance relative to peers.
The data sources used in the Quality Incentive Program include quality measures from the following sources:
- New York's Quality Assurance Reporting Requirements (QARR), which is largely comprised of National Committee for Quality Assurance (NCQA) Healthcare Effectiveness Data and Information Set (HEDIS®)
- State-specific performance measures
- Consumer Assessment of Healthcare Providers and Systems (CAHPS®)
- Prevention Quality Indicators using the Agency for Healthcare Research and Quality (AHRQ)
Rates of performance in Medicaid managed care have increased steadily over the last decade. New York State Medicaid plans have demonstrated a high level of care compared to national averages, and for many domains of care the gap in performance between commercial and Medicaid managed care has been decreasing since the Quality Incentive Program was implemented. The use of financial incentives has proven successful in engaging Medicaid managed care plans in developing infrastructure, programs, and resources to promote high quality care. Incorporating financial incentives that tie payment directly to quality is an important approach to improving the quality of care and holds health plans accountable for the care they provide and rewards those who invest in processes that improve care. State Medicaid programs have steadily increased the use of financial incentives or pay-for-performance (P4P) mechanisms in their payment systems.
Currently, the Quality Incentive Program has a defined methodology to determine the percentage of the potential financial incentive that a plan receives. Plans earn up to 150 points from the categories of Quality of Care, Consumer Satisfaction, and Preventive Quality Indicators. Points are subtracted from the plan's total points if the plan had statements of deficiency in the Compliance category. A maximum of 20 points could be subtracted from the plan's total points for statements of deficiency associated with specific compliance areas. A plan can also earn up to 6 possible bonus points for an approved telehealth innovation plan. The plans total points out of the 150 points are normalized to a 100-point scale.
Summary of the current Quality Incentive structure components and possible points:
| Component | Measures * | Points |
|---|---|---|
| Quality – QARR (HEDIS® and NYS-specific) | 30 measures | 100 points |
| Satisfaction – CAHPS® Health Plan Survey | 3 measures | 30 points |
| Prevention Quality Indicators | 2 measures | 20 points |
| Total Points | 150 points | |
| Compliance (Subtracted from Total) | 6 measures | Up to 20 points |
| Bonus for Telehealth Innovation (Added to Total) | Up to 6 points | |
| Final Score | Final points/150 | |
* The number of measures per component may vary from year to year.
Plans are grouped into one of five tiers to determine the incentive award. The five tiers are based on the percentage of points earned by the plans and were set using the 2017 Quality Incentive scores (Attachment D). Plans must achieve or exceed the threshold for the respective tier to be eligible for their award. Incentive premium awards are impacted by enacted budget actions for SFY 19-20 and may change to meet program fiscal targets. The amount of the incentive award is determined by the Division of Finance and Rate Setting and subject to final approval from Division of Budget and the Center for Medicare and Medicaid Services (CMS).
Plans performance also affects the auto-assignment preference. Plans achieving Tier 1 - Tier 4 of the Quality Incentive award receive the quality preference in the auto-assignment algorithm. The quality preference in the algorithm directs a proportion of auto-assignees only to plans that qualified for the incentive. The quality preference for auto-assignment is not adjusted by the tier of the Quality Incentive award; rather all tiers other than Tier 5 receive the same quality preference and share in the distribution of auto-assignees equally.
The 2018 Quality Incentive awards become effective for capitation rates and for auto-assignment preference on April 1, 2019. Final revised capitation rates for plans that received the 2018 Quality Incentive will be sent separately from the Division of Finance and Rate Setting.
The Quality Incentive methodology aligns with the Department's efforts to reward comprehensive quality care. The improvement in results for Medicaid managed care has been impressive over the past ten years. The objective with the incentive methodology is to expand the scope of accountability and provide continued encouragement for improvement.
Section 2: Quality Incentive Components and Calculation Process – 2018 Methodology
In this section, a detailed description of the five Quality Incentive components and the calculation process are presented to explain how the points are assigned to each measure within each component.
The following five Quality Incentive components were used to determine the 2018 Quality Incentive results:
- Quality of Care: 2018 QARR results using 2017 data
- Consumer Satisfaction: The most recent CAHPS® survey for Adults in Medicaid, which was administered in fall 2017 and results released in reports dated March 2018
- Prevention Quality Indicators: Prevention Quality Overall Composite (PQI 90) and Pediatric Quality Overall Composite (PDI 90) using 2017 inpatient admissions
- Compliance: Regulatory compliance information from 2016 and 2017
- Bonus Points: Telehealth Innovation Plan (TIP)
Quality of Care Measures: (100 points possible)
The methodology for awarding points for quality measures in the 2018 Quality Incentive has changed slightly from the methodology used in the 2017 Incentive. Quality performance points were earned based on percentiles of the prior year performance for Medicaid Managed Care plans.
- The Quality Measures included align with the measures selected for the State's Value Based Payment arrangements. Quality measures from Total Care for the General Population (including Integrated Primary Care), Behavioral Health, Maternity, and HIV will be included. This approach allows a more comprehensive view of quality and aligns with other uses of the data for value-based purchasing. It also minimizes the impact of one problematic area in the overall performance of the plan. For some measures with more than one indicator, we will use a weighted average method (see equation below) to average each measure's individual indicator rates and calculate a measure score.
Indicators with larger denominators will contribute more to the scoring than indicators with smaller denominators. The attached list of measures identifies the measures with multiple indicators where the scores will be calculated as weighted averages.
The weighted average equation is as follows: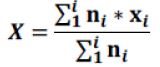
Where X is the final measure score that is the weighted average, xi is the indicator score, and is the indicator denominator. - The allotted 100 points for quality will be distributed evenly for all measure scores, and for measures with more than one indicator, each measure score will be counted as one measure. For example, if there are 30 measures in the quality section, each measure is worth up to 3.33 points.
- If a measure has less than 30 members in the denominator, we consider it to be Small Sample Size (SS), and we suppress those results. There will be no reweighting for Small Sample Size. If plan results are SS, there will be overall reduction of quality points. For example, with 30 measures worth 3.33 points out of 100 possible points, if a plan only has 29 measures each will be worth 3.33 points but only out of 96.67 total points. The base is reduced by the maximum value for that one measure.
- The determination of the 50th, 75th, and 90th percentiles will be based on the measurement year prior. Quality performance benchmarks to be used in the awarding of points are included in this report. To determine the plans achieving the percentiles, the results are rounded to two decimal points prior to the percentile determination.
- Trending determinations by measure are made by NYSDOH. Any Pay-for-Performance (P4P) measure that cannot be trended are awarded points on percentile benchmarks using data from the current measurement year, rather than the prior year.
- Plans are awarded 50 percent of possible points for a measure result at or above the 50th percentile, but less than the 75th percentile; 75 percent of possible points for a measure result at or above the 75th percentile, but less than the 90th percentile; and 100 percent of possible points for the measure at or above the 90th percentile.
- Each plan's quality points are totaled and then divided by their base points. The resulting quality percentage points are normalized to 100. This normalization of the quality percentage points to 100 allows this section of the Quality Incentive to continue to retain a similar weight in the makeup of the overall scores.
Quality Measure Benchmarks for the 2018 Medicaid Quality Incentive
| Quality Measure | Indicators | 90th Percentile | 75th Percentile | 50th Percentile | Points Possible |
|---|---|---|---|---|---|
| Annual Dental Visit | Ages 2-18 | 69.01 | 66.98 | 62.09 | 3.33 |
| Antidepressant Medication Management | Effective Acute Phase Treatment | 45.38 | 44.71 | 42.03 | 3.33 |
| Effective Continuation Phase Treatment | |||||
| Breast Cancer Screening | 73.10 | 70.80 | 68.04 | 3.33 | |
| Cervical Cancer Screening | 77.87 | 75.99 | 71.63 | 3.33 | |
| Chlamydia Screening | 16-20 years | 79.99 | 76.92 | 71.71 | 3.33 |
| 21-24 Years | |||||
| Childhood Immunization | Combination 3 | 83.21 | 81.86 | 77.13 | 3.33 |
| Colorectal Cancer Screening | 64.23 | 57.35 | 54.74 | 3.33 | |
| Comprehensive Diabetes Care | Received All Three Tests | 62.04 | 59.95 | 57.31 | 3.33 |
| Comprehensive Diabetes Care | HbA1C Control <8.0% | 61.07 | 57.42 | 55.07 | 3.33 |
| Controlling High Blood Pressure | 70.80 | 65.21 | 62.84 | 3.33 | |
| Flu Shots for Adults (CAHPS®) | 47.20 | 44.24 | 40.49 | 3.33 | |
| Immunization for Adolescents | Combination 2 | NT | NT | NT | 3.33 |
| Initiation and Engagement of Alcohol and other Drug Dependence Treatment | Initiation of AOD Treatment | NT | NT | NT | 3.33 |
| Engagement of AOD Treatment | |||||
| Medical Assistance with Tobacco Cessation (CAHPS®) | Advising Smokers and Tobacco Users to Quit | 66.83 | 65.09 | 63.49 | 3.33 |
| Discussing Cessation Medications | |||||
| Discussing Cessation Strategies | |||||
| Medication Management for People with Asthma (Ages 5-64) | 50% of Treatment Period Covered | 50.88 | 48.51 | 46.25 | 3.33 |
| 75% of Treatment Period Covered | |||||
| Statin Therapy for Patients with Cardiovascular Disease | Statin Adherence 80% | 69.57 | 66.25 | 63.64 | 3.33 |
| Use of Spirometry Testing in the Assessment and Diagnosis of COPD | 55.20 | 54.44 | 45.32 | 3.33 | |
| Weight Assessment and Counseling for Children and Adolescents | Body Mass Index (BMI) Percentile Documentation | 86.46 | 84.08 | 77.53 | 3.33 |
| Counseling for Nutrition | |||||
| Counseling for Physical Activity | |||||
| Well Child Visits in the First 15 Months – Five or more visits | 85.85 | 84.28 | 81.32 | 3.33 | |
| Well Child Visits in the 3rd, 4th, 5th and 6th Year | 87.28 | 85.04 | 82.77 | 3.33 | |
| Adherence to Antipsychotic Medications for Individuals with Schizophrenia | 67.69 | 63.49 | 60.90 | 3.33 | |
| Diabetes Screening for People with Schizophrenia or Bipolar Disorder Using Antipsychotic Medications | 83.26 | 82.54 | 80.93 | 3.33 | |
| Follow Up After Hospitalization for Mental Illness Within 7 Days | 7 Days | NT | NT | NT | 3.33 |
| Follow-up after Discharge from the Emergency Department for Mental Health- 7-day rate | 7 Days | NT | NT | NT | 3.33 |
| Follow Up After Hospitalization for Mental Illness- 7-day rate | 7 Days | NT | NT | NT | 3.33 |
| Follow Up for Children Newly Prescribed ADHD Medication | Initiation Phase | 69.55 | 69.13 | 60.95 | 3.33 |
| Continuation and Maintenance Phase | |||||
| Metabolic Monitoring for Children and Adolescents on Antipsychotics | 48.82 | 48.06 | 41.60 | 3.33 | |
| Timeliness of Prenatal Care | 92.94 | 90.02 | 88.67 | 3.33 | |
| Postpartum Care | 73.72 | 72.25 | 68.86 | 3.33 | |
| Viral Load Suppression | 83.97 | 83.41 | 76.81 | 3.33 | |
| Total Points | 100 | ||||
NT- Cannot trend data from previous year benchmarks. All plans receive the full points for measures labeled as NT.
Satisfaction Measures: (30 points)
This year's Quality Incentive incorporates satisfaction data from the state-sponsored CAHPS® survey for Adults in Medicaid, which was administered in fall 2017, and results released in reports dated March 2018. Thirty points (of the total 150) were assigned to the CAHPS® measures. To achieve 10 points for a measure, the plan's result for the measure must be significantly higher than the statewide average. Plan results that were not significantly different than the statewide average earn 5 points, and plan results that were significantly below the statewide average did not receive any points (zero points).
The CAHPS® measures included in the 2018 Quality Incentive:
| CAHPS Measure | Statewide Average |
Satisfaction Points |
|---|---|---|
| Rating of Health Plan | 76 | 10 |
| Getting Care Needed | 79 | 10 |
| Customer Service and Information | 86 | 10 |
| Total | 30 |
Prevention Quality Indicators (PQI) Measures (20 points)
The Prevention Quality Indicators (PQI) and Pediatric Quality Indicators (PDI) quantify hospital admissions that most likely could have been avoided through high-quality outpatient care. To align with the Delivery System Reform Incentive Payment Program (DSRIP), the PQI Composite measure (PQI 90) and the PDI Composite measure (PDI 90) are used in the 2018 Quality Incentive. To further align with the Agency for Healthcare Research and Quality (AHRQ), the prevention quality indicators will be calculated as the number of admissions that met one of the prevention quality or pediatric quality indicators over the total number of people in your health plan. Plans will be awarded points based on their risk adjusted rates. Plans will receive 50 percent of possible points for a measure at or below the 50th percentile, but greater than the 25th percentile, 75 percent of possible points for a measure at or below the 25th percentile, but greater than the 10th percentile and 100 percent of possible points for the measure at or below the 10th percentile. Plans received no points for a measure above the 50th percentile.
| PQI | 10th Percentile | 25th Percentile | 50th Percentile | PQI Points |
|---|---|---|---|---|
| Pediatric Quality Overall Composite (PDI 90) | 94.6 | 106.36 | 160.78 | 10 |
| Adult Prevention Quality Overall Composite (PQI 90) | 617.61 | 681.34 | 719.54 | 10 |
| Total Points | 20 |
Methodology used in calculating the PQI:
Data Source
Encounter data submitted by the managed care plans to the All Payer Database (APD) for inpatient hospitalizations where the patient was discharged in calendar year 2018 were used for this analysis. The patient had to be enrolled in the health plan for at least three months before the month of the hospital admission. AHRQ PQI version 2018 logic was used to assign PQI indicators to the hospitalizations. Members who were dually enrolled in Medicaid and Medicare at any time in the measurement year were removed.
Population
Health plan enrollment was determined as four months of continuous enrollment in a health plan. If a person was enrolled for more than four months in more than one health plan during the year, the member was counted in each health plan. The members enrolled in the plan were used to create the denominator for the PQI and PDI measures. Members who were dually enrolled in Medicaid and Medicare were removed.
Rate Calculation
Observed and risk adjusted rates per 100,000 enrollees were calculated for each plan for each of the two measures. The measures were risk adjusted by the patient's age group, gender, race/ethnicity, Medicaid aid category, and the enrollee's Clinical Risk Group (CRG) status from the previous year.
Compliance Measures: (20 points for subtraction)
The Compliance section includes six areas:
- Statements of deficiency for timely, complete, and/or accurate submissions of Encounter data
- Medicaid Managed Care Operating Report (MMCOR)
- Quality Assurance Reporting Requirements
- Plan network
- Provider directory
- Member services
The Quality Reporting Requirement area for 2018 includes submission requirements for Care Management data, Performance Improvement Project reports, and performance matrices action plans. In the 2018 Quality Incentive, points from issues with Compliance will be subtracted from the total points prior to calculating the final percentage scores.
Number of possible Compliance points subtracted.
| Category | Measure Description | Timeframe | Points |
|---|---|---|---|
| Encounter Data | Any statement of deficiency for timeliness or completeness of Encounter data submitted for the measurement year (2017). | Encounter data submitted for 2017 | 4 points for any statement of deficiency. No more than 4 points will be removed for this category. |
| Medicaid Managed Care Operating Report | Any statement of deficiency for timeliness, completeness, or failure to meet reserve requirements of MMCOR reports submitted for the measurement year (2017). | MMCOR reports submitted for 2017 | 4 points for any statement of deficiency for timeliness, completeness, accuracy, or failure to meet reserves. No more than 4 points will be removed for this category. |
| Any statement of deficiency for timeliness, completeness, or failure to meet reserve requirements of MMCOR reports submitted for the measurement year (2016). | MMCOR reports submitted for 2016 | ||
| Quality Reporting Requirements | Any statement of deficiency for failure to submit required complete quality data for Care Management (CMART) data and QARR data (includes the required member-level file and the birth file) by the established deadlines for the measurement year (2017). | Quality Reporting Requirements for 2017 data | 4 points for a statement of deficiency. No more than 4 points will be removed for this category. |
| Any statement of deficiency related to the Performance Improvement Projects or the quality performance matrix process. | Quality reporting requirements for 2017. | ||
| Plan Network | Any statement of deficiency issued for the measurement year (2017) for failure to manage access to care to maintain network with at least 75% compliance with required appointment timeframes based on the Access and Appointment Availability survey conducted for the department. | Access and Availability survey results for 2017 | 2 points for any statement of deficiency. No more than 2 points will be removed for this item in the category. |
| Provider Directory | Any statement of deficiency for incomplete or inaccurate provider listings and/or failure to maintain at least 75% provider participation rate for the measurement year (2017). | Provider Directory Information and Participation results for 2017 | 2 points for any statement of deficiency for either directory information or for provider participation. No more than 2 points will be removed for this item in the category. |
| Member Services | Any statement of deficiency or statement of findings for member services during the measurement year (2017) for failure to: maintain a functional member services phone line; provide correct information to callers; provide specific information upon written request. | Member services for 2017 | 4 points for any statement of deficiency or statement of findings for any of the three-member service items. No more than 4 points will be removed for this category. |
| Total | 20 points |
Bonus Points: (Up to 6 points added)
Telehealth Innovation Plan
Medicaid managed care plans who submit a Telehealth Innovation Plan (TIP) and "in lieu of services" (ILS) and receive DOH approval of their TIP request submission will earn five (5) bonus points for their annual Quality Incentive (Quality Incentive) award. An additional one (1) Quality Incentive bonus point will be earned if the submission demonstrates enhanced access to services and seeks to improve outcomes for women with high-risk pregnancies and/or children in their first 1000 days of life.
Quality Incentive Tiers:
Plans are grouped into one of five tiers to determine the incentive award. The five tiers are based on the percentage of points earned by the plans and were set using the 2017 Quality Incentive scores. The tiers were set without the addition of the bonus points and will be applied to the 2018 Quality Incentive and the 2019 Quality Incentive.
| Tier | Range of Scores |
|---|---|
| Tier 1 | 100.00 – 80.09 |
| Tier 2 | 80.08 – 67.08 |
| Tier 3 | 67.07 – 49.10 |
| Tier 4 | 49.09 – 36.08 |
| Tier 5 | 36.07 – 0.00 |
Section 3: Quality Incentive Award Results
In 2018, the fifteen NYS Medicaid Managed Care plans were grouped into five tiers based on their Quality Incentive scores. The table below shows the tier assigned to each plan. The 2018 Quality Incentive awards become effective for capitation rates and for auto-assignment preference on April 1, 2019.
| Incentive Tier | Plan Name | Normalized Quality Points = Quality Points/Highest Score | Satisfaction Points | PQI Points | Compliance Points | Bonus Points | Total Points | Percent |
|---|---|---|---|---|---|---|---|---|
| 100 points possible | 30 points possible | 20 points possible | 20 points possibly subtracted | 6 points possible | Up to 100% | |||
| Tier 1 | ||||||||
| Tier 2 | CDPHP | 66.29 | 30 | 20 | -4 | 6 | 118.29 | 78.86 |
| Tier 2 | MetroPlus Health Plan | 100.00 | 10 | 5 | -4 | 6 | 117.00 | 78.00 |
| Tier 2 | Fidelis Care New York, Inc. | 88.76 | 15 | 10 | -8 | 6 | 111.76 | 74.51 |
| Tier 2 | Healthfirst PHSP, Inc. | 97.75 | 10 | 0 | -4 | 6 | 109.75 | 73.17 |
| Tier 2 | Empire BlueCross BlueShield HealthPlus | 73.03 | 15 | 12.5 | -4 | 6 | 102.53 | 68.36 |
| Tier 2 | MVP Health Care | 61.80 | 30 | 12.5 | -8 | 6 | 102.30 | 68.20 |
| Tier 3 | Excellus BlueCross BlueShield | 74.16 | 15 | 5 | -8 | 6 | 92.16 | 61.44 |
| Tier 3 | Independent Health's MediSource | 67.42 | 20 | 0 | -4 | 6 | 89.42 | 59.61 |
| Tier 3 | HealthNow New York Inc. | 55.06 | 10 | 15 | -8 | 6 | 78.06 | 52.04 |
| Tier 3 | UnitedHealthcare Community Plan | 48.31 | 10 | 15 | -4 | 6 | 75.31 | 50.21 |
| Tier 3 | WellCare of New York | 57.30 | 15 | 5 | -8 | 6 | 75.30 | 50.20 |
| Tier 4 | Molina Healthcare | 39.33 | 15 | 10 | -4 | 6 | 66.33 | 44.22 |
| Tier 4 | Affinity Health Plan | 57.30 | 15 | 0 | -12 | 6 | 66.30 | 44.20 |
| Tier 4 | HIP (EmblemHealth) | 55.06 | 10 | 0 | -12 | 6 | 59.06 | 39.37 |
| Tier 4 | YourCare Health Plan | 49.44 | 15 | 0 | -12 | 6 | 58.44 | 38.96 |
| Tier 5 | ||||||||
*Incentive premium awards were impacted by enacted budget actions for SFY 19-20 and may change to meet program fiscal targets
If you have questions regarding the incentive premium award, please contact the Bureau of Acute & Managed Care Reimbursement at (518) 473-8822.
We welcome suggestions and comments on this publication. Please contact us at:
Bureau of Quality Measurement and Evaluation
Office of Quality and Patient Safety
Empire State Plaza
Albany, New York 12237
Telephone: (518) 486-9012
Fax: (518) 486-6098
E-mail: nysqarr@health.ny.gov