2020 Medicaid Managed Care Quality Incentive Report
A Report on the Medicaid Managed Care Quality Incentive Program in New York State
- Report also available in Portable Document Format (PDF)

QARR Report Series health.ny.gov
Table of Contents
Section 1: Background
New York's Medicaid Managed Care Quality Incentive Program began in early 2001. In 2002, the program was expanded to provide increased incentives for improvement. Plans became eligible to receive bonuses added to the premium based upon composite scores from quality measures and satisfaction measures. The bonus was later increased in 2005 to its current value. The Quality Incentive Program continues to evolve and includes new components and measures as well as a refined methodology to calculate current performance relative to peers.
The data sources used in the Quality Incentive Program include quality measures from the following sources:
- New York's Quality Assurance Reporting Requirements (QARR), which is largely comprised of National Committee for Quality Assurance (NCQA) Healthcare Effectiveness Data and Information Set (HEDIS®)
- State-specific performance measures
- Consumer Assessment of Healthcare Providers and Systems (CAHPS®)
- Prevention Quality Indicators using the Agency for Healthcare Research and Quality (AHRQ)
Rates of performance in Medicaid managed care have increased steadily over the last decade. New York State Medicaid plans have demonstrated a high level of care compared to national averages, and for many domains of care the gap in performance between commercial and Medicaid managed care has been decreasing since the Quality Incentive Program was implemented. The use of financial incentives has proven successful in engaging Medicaid managed care plans in developing infrastructure, programs, and resources to promote high quality care. Incorporating financial incentives that tie payment directly to quality is an important approach to improving the quality of care, holds health plans accountable for the care they provide, and rewards those who invest in processes that improve care. State Medicaid programs have steadily increased the use of financial incentives or pay-for-performance (P4P) mechanisms in their payment systems.
Currently, the Quality Incentive Program has a defined methodology to determine the percentage of the potential financial incentive that a plan receives. Plans earn up to 150 points from the categories of Quality of Care, Consumer Satisfaction, and Preventive Quality Indicators. Points are subtracted from the plan's total points if the plan had statements of deficiency in the Compliance category. A maximum of 20 points could be subtracted from the plan's total points for statements of deficiency associated with specific compliance areas. The plans total points out of the 150 points are normalized to a 100-point scale.
Summary of the current Quality Incentive structure components and possible points:
| Component | Number of Measures | Points | |
|---|---|---|---|
| Quality – QARR (HEDIS® and NYS-specific) | 30 measures | 100 points | |
| Satisfaction – CAHPS® Health Plan Survey | 3 measures | 20 points | |
| Prevention Quality Indicators | 2 measures | 20 points | |
| Total Points | 150 points | ||
| Compliance (Subtracted from Total) | 8 measures | Up to 20 points | |
| Final Score | Final points/150 | ||
* The number of measures per component may vary from year to year.
Plans are grouped into one of five tiers to determine the incentive award. The five tiers are based on the percentage of points earned by the plans and were set using the 2020 Quality Incentive scores. Plans must achieve or exceed the threshold for the respective tier to be eligible for their award. Incentive premium awards are impacted by enacted budget actions for SFY 2020-2021 and may change to meet program fiscal targets. The amount of the incentive award is determined by the Division of Finance and Rate Setting and subject to final approval from Division of Budget and the Center for Medicare and Medicaid Services (CMS).
A plan's performance in the Quality Incentive also affects the auto-assignment preference. Plans achieving Tier 1 - Tier 4 of the Quality Incentive award receive the quality preference in the auto-assignment algorithm. The quality preference in the algorithm directs a proportion of auto-assignees only to plans that qualified for the incentive. The quality preference for auto- assignment is not adjusted by the tier of the Quality Incentive award; rather all tiers other than Tier 5 receive the same quality preference and share in the distribution of auto-assignees equally. Score thresholds for each tier were consistent with thresholds used for the 2019 Quality Incentive.
The 2020 Quality Incentive awards become effective for capitation rates and for auto- assignment preference on April 1, 2021. Final revised capitation rates for the 2020 Quality Incentive will be sent separately from the Division of Finance and Rate Setting. If you have questions regarding the incentive premium award, please contact the Bureau of Acute & Managed Care Reimbursement at (518) 473-8822.
The Quality Incentive methodology aligns with the Department's efforts to reward comprehensive quality care. The improvement in results for Medicaid managed care has been impressive over the past ten years. The objective with the incentive methodology is to expand the scope of accountability and provide continued encouragement for improvement.
Section 2: Quality Incentive Components and Calculation Process – 2020 Methodology
In this section, a detailed description of the five Quality Incentive components and the calculation process are presented to explain how the points are assigned to each measure within each component.
The following five Quality Incentive components were used to determine the 2019 Quality Incentive results:
- Quality of Care: 2020 QARR results using 2019 data
- Consumer Satisfaction: The most recent CAHPS® survey for Adults in Medicaid, which was administered in fall 2019 and results released in reports dated May 2020
- Prevention Quality Indicators: Prevention Quality Overall Composite (PQI 90) and Pediatric Quality Overall Composite (PDI 90) using 2019 inpatient admissions
- Compliance: Regulatory compliance information from 2018 and 2019
Quality of Care Measures: (100 points possible)
The methodology for awarding points for quality measures in the 2020 Quality Incentive has changed slightly from the methodology used in the 2019 Incentive. Quality performance points were earned based on percentiles of the prior year performance for Medicaid managed care plans.
- The Quality Measures included align with the measures selected for the State's Value Based Payment arrangements. Quality measures from Primary Care, Mental Health, Substance Use, Maternity, Children's Health, and HIV will be included. This approach allows a comprehensive view of quality and aligns with other uses of the data for value- based purchasing. It also minimizes the impact of one problematic area in the overall performance of the plan. For some measures with more than one indicator, we use a weighted average method (see equation below) to average each measure's individual indicator rates and calculate a measure score.
Indicators with larger denominators contribute more to the scoring than indicators with smaller denominators. The table of Quality Measure Benchmarks included below identifies the measures with multiple indicators where the scores are calculated as weighted averages.
The weighted average equation is as follows: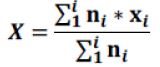
Where X is the final measure score that is the weighted average, xi is the indicator score, and is the indicator denominator. - The allotted 100 points for quality are distributed evenly for all measure scores, and for measures with more than one indicator, each measure score is counted as one measure. For example, if there are 30 measures in the quality section, each measure is worth up to 3.33 points.
- If a measure has less than 30 members in the denominator, we consider it to be Small Sample Size (SS), and we suppress those results. There is no reweighting for Small Sample Size. If plan results are SS, there is an overall reduction of quality points. For example, with 30 measures worth 3.33 points out of 100 possible points, if a plan only has 29 measures, each measure is worth 3.33 points but only out of 96.67 total points. The base is reduced by the maximum value for that one measure.
- The determination of the 50th, 75th, and 90th percentiles are based on the measurement year prior unless otherwise noted. Quality performance benchmarks used in the awarding of points are included in this report. To determine the plans achieving the percentiles, the results are rounded to two decimal points prior to the percentile determination.
- Plans are awarded 50 percent of possible points for a measure result at or above the 50th percentile, but less than the 75th percentile; 75 percent of possible points for a measure result at or above the 75th percentile, but less than the 90th percentile; and 100 percent of possible points for the measure at or above the 90th percentile.
- Trending determinations by measure are made by NYSDOH. Any Pay-for-Performance (P4P) measure that cannot be trended are awarded points on percentile benchmarks using data from the current measurement year, rather than the prior year.
- For measures reported using the hybrid methodology, either the HEDIS 2019 hybrid rates or HEDIS 2020 hybrid rate (whichever is higher) will be used for awarding points in the quality incentive. HEDIS 2019 benchmarks will be applied to these measures. Relevant measures are denoted in the table of benchmarks. No exceptions are being made for administrative rates which should be reported following HEDIS 2020 reporting requirements.
- Timeliness of Prenatal Care was not scored for the 2020 Quality Incentive and all plans base points were reduced to 96.97.
- Each plan's quality points are totaled and then divided by their base points. The resulting quality percentage points are normalized to 100. This normalization of the quality percentage points to 100 allows this section of the Quality Incentive to continue to retain a similar weight in the makeup of the overall scores.
Quality Measure Benchmarks for the 2020 Medicaid Quality Incentive
| Measure Name | 90th Percentile | 75th Percentile | 50th Percentile | Points Possible |
|---|---|---|---|---|
| Primary Care | ||||
| Antidepressant Medication Management | 46.33 | 46.18 | 45.33 | 3.33 |
| Asthma Medication Ratio | 67.03 | 65.90 | 63.62 | 3.33 |
| Breast Cancer Screening | 74.86 | 70.83 | 68.66 | 3.33 |
| Cervical Cancer Screening * | 75.72 | 73.97 | 72.13 | 3.33 |
| Chlamydia Screening in Women | 81.51 | 79.46 | 74.05 | 3.33 |
| Colorectal Cancer Screening * | 66.67 | 62.59 | 58.15 | 3.33 |
| Comprehensive Diabetes Screening: Eye Exam * | 71.78 | 69.34 | 65.21 | 3.33 |
| Comprehensive Diabetes Care: Poor Control * | 25.06 | 28.47 | 30.66 | 3.33 |
| Controlling High Blood Pressure * | 75.18 | 68.61 | 63.02 | 3.33 |
| Initiation and Engagement of Alcohol and Other Drug Abuse or Dependence Treatment | 37.53 | 33.92 | 31.66 | 3.33 |
| Medication Management for People with Asthma (Ages 5-64) | 54.57 | 54.13 | 50.20 | 3.33 |
| Statin Therapy for Patients with Cardiovascular Disease: Statin Adherence 80% | 74.47 | 70.72 | 67.02 | 3.33 |
| Use of Spirometry Testing in the Assessment and Diagnosis of COPD | 61.13 | 53.47 | 47.28 | 3.33 |
| Children's Health | ||||
| Annual Dental Visit: Ages 2-18 | 70.13 | 66.55 | 62.79 | 3.33 |
| Childhood Immunization: Combination 3 * | 83.45 | 81.51 | 78.11 | 3.33 |
| Immunizations for Adolescents: Combination 2 * | 53.53 | 43.55 | 40.15 | 3.33 |
| Well-Child Visits in the First 15 Months of Life: Five or More Visits | 88.30 | 85.90 | 83.01 | 3.33 |
| Well-Child Visits in the Third, Fourth, Fifth and Sixth Years of Life | 87.18 | 86.28 | 84.68 | 3.33 |
| Weight Assessment and Counseling for Nutrition and Physical Activity for Children/Adolescents * | 89.60 | 87.43 | 81.83 | 3.33 |
| Mental Health | ||||
| Adherence to Antipsychotic Medications for Individuals with Schizophrenia | 66.10 | 64.89 | 62.53 | 3.33 |
| Diabetes Screening for People with Schizophrenia or Bipolar Disorder Who Are Using Antipsychotic Medications | 85.45 | 82.67 | 80.84 | 3.33 |
| Follow-Up After Emergency Department Visit for Mental Illness: 7-day rate | 77.78 | 67.04 | 60.71 | 3.33 |
| Follow-Up After Hospitalization for Mental Illness: 7-day rate | 67.72 | 66.98 | 61.02 | 3.33 |
| Follow-Up Care for Children Prescribed ADHD Medication | 75.22 | 66.32 | 57.23 | 3.33 |
| Metabolic Monitoring for Children and Adolescents on Antipsychotics | 50.91 | 47.20 | 43.12 | 3.33 |
| Substance Use | ||||
| Follow-Up After Emergency Department Visit for Alcohol and Other Drug Abuse or Dependence: 7-day rate | 25.93 | 24.48 | 22.39 | 3.33 |
| Initiation of Pharmacotherapy Upon New Episode of Opioid Dependence | 41.45 | 40.15 | 35.78 | 3.33 |
| Maternity | ||||
| Timeliness of Prenatal Care | 95.38 | 91.00 | 88.81 | 0.00 |
| Postpartum Care | 84.43 | 82.48 | 80.29 | 3.33 |
| HIV | ||||
| Viral Load Suppression | 86.21 | 83.97 | 77.14 | 3.33 |
* HEDIS 2019 benchmarks will be applied to HEDIS 2019 or HEDIS 2020 health plan results (whichever is higher).
NA - Not applicable. Plans will be awarded points on the percentiles for this measure within the measurement year.
CAHPS Satisfaction Survey: (30 points possible)
Three CAHPS Experience of Care survey measures are included in the Quality Incentive. Thirty points are available and distributed based on whether a plan was at or above the statewide average for the most recent CAHPS survey. CAHPS is administered every year for Medicaid alternating adult and child surveys. For the 2020 Quality Incentive, the CAHPS scores from the survey conducted in fall 2019 with Adults in Medicaid were used. Plans were awarded points based on their scores within the measurement year. Plans earned ten points for measures with results significantly better than the statewide average, five points for measures with results not significantly different from the statewide average, and no points for measures with results significantly lower than the statewide average.
| CAHPS Measure | Statewide Average | Satisfaction Points |
|---|---|---|
| Rating of Health Plan | 75.90 | 10 points |
| Getting Care Needed | 81.34 | 10 points |
| Customer Service and Information | 87.14 | 10 points |
| Total | 30 points |
Prevention Quality Indicators (PQIs): (0 points)
The Prevention Quality Indicators (PQIs) and Pediatric Quality Indicators (PDIs) quantify hospital admissions that most likely could have been avoided through high-quality outpatient care. The PQI Composite measure (PQI 90) and the PDI Composite measure (PDI 90) are used in the 2020 Quality Incentive. To further align with the Agency for Healthcare Research and Quality (AHRQ), the prevention quality indicators are calculated as the number of admissions that met one of the prevention quality or pediatric quality indicators over the total number of people in the health plan. Plans are awarded points based on their risk adjusted rates within the measurement year. Results from the year prior cannot be used in the awarding of PQI/PDI points because of the risk adjustment methodology. Plans received 50 percent of possible points for a measure at or below the 50th percentile, but greater than the 25th percentile; 75 percent of possible points for a measure at or below the 25th percentile, but greater than the 10th percentile; and 100 percent of possible points for the measure at or below the 10th percentile.
| PQI | PQI Points |
|---|---|
| Adult Prevention Quality Overall Composite (PQI 90) | 10 points |
| Pediatric Quality Overall Composite (PDI 90) | 10 points |
| Total | 20 points |
Benchmarks for the 10th, 25th, and 50th percentiles for the PQI measures in the 2020 Quality Incentive:
| PQI Measures | 10th Percentile | 25th Percentile | 50th Percentile | Points Possible |
|---|---|---|---|---|
| Pediatric Quality Overall Composite (PDI 90) | 84.52 | 105.02 | 125.12 | 10 |
| Adult Prevention Quality Overall Composite (PQI 90) | 532.65 | 562.32 | 652.23 | 10 |
| Total Points | 20 | |||
Methodology used in calculating the PQI:
Data Source
Encounter data submitted by the managed care plans to the All Payer Database (APD) for inpatient hospitalizations where the patient was discharged in calendar year 2019 were used for this analysis. The patient had to be enrolled in the health plan for at least three months before the month of the hospital admission. AHRQ PQI version 2019 logic was used to assign PQI indicators to the hospitalizations. Members who were dually enrolled in Medicaid and Medicare at any time in the measurement year were removed.
Population
Health plan enrollment was determined as four months of continuous enrollment in a health plan. If a person was enrolled for more than four months in more than one health plan during the year, the member was counted in each health plan. The members enrolled in the plan were used to create the denominator for the PQI and PDI measures. Members who were dually enrolled in Medicaid and Medicare were removed.
Rate Calculation
Observed and risk adjusted rates per 100,000 enrollees were calculated for each plan for each of the two measures. The measures were risk adjusted by the patient's age group, gender, race/ethnicity, Medicaid aid category, and the enrollee's Clinical Risk Group (CRG) status from the previous year.
Compliance: (20 points for subtraction)
The Compliance section includes seven areas: Statements of deficiency (SOD) for the Medicaid Managed Care Operating Report (MMCOR), Quality Assurance Reporting Requirements, plan network, provider directory, member services, behavioral health parity, and claims payment and/or denials. The Quality Reporting Requirement area for 2020 includes submission requirements for Care Management data, Performance Improvement Project reports, performance matrices action plans, and focused clinical studies. In the 2020 Quality Incentive, points from issues with Compliance will be subtracted from the total points prior to calculating the final percentage scores. The number of points that may be subtracted is detailed below:
| Category | Measure Description | Timeframe | Points |
|---|---|---|---|
| Medicaid Managed Care Operating Report | Any SOD for timeliness, completeness, or failure to meet reserve requirements of MMCOR reports submitted for the measurement year (2019). | MMCOR reports submitted for 2019 | 4 points for any SOD timeliness, completeness, or failure to meet reserves. No more than 4 points will be removed for this category. |
| Any SOD for timeliness, completeness, or failure to meet reserve requirements of MMCOR reports submitted the year prior to the measurement year (2018). | MMCOR reports submitted for 2018 | ||
| Quality Reporting Requirements | Any SOD for failure to submit required complete quality data for Care Management (CMART) data and QARR data (includes the required member- level file and the birth file) by the established deadlines for the measurement year (2019). | Quality Reporting Requirements for 2019 data | 4 points for a SOD. No more than 4 points will be removed for this category. |
| Any SOD related to the Performance Improvement Projects or the quality performance matrix process. | Quality reporting requirements for 2019 | ||
| Any statement of deficiency related to a Focused Clinical Study (FCS). | FCS reporting requirements for 2019 | ||
| Plan Network | Any SOD issued for the measurement year (2019) for failure to manage access to care to maintain network with at least 75% compliance with required appointment timeframes based on the Access and Appointment Availability survey conducted for the department. | Access and Availability survey results for 2019 | 2 points for any SOD. No more than 2 points will be removed for this item in the category. |
| Any SOD for timeliness, incomplete, or inaccurate Provider Network Directory System (PNDS) or Panel Submission for measurement year (2019). | PNDS Quarterly submission for 2019 Panel Quarterly Submission for 2019 | ||
| Provider Directory | Any SOD for incomplete or inaccurate provider listings and/or failure to maintain at least 75% provider participation rate for the measurement year (2019). | Provider Directory Information and Participation results for 2019 | 2 points for any SOD for either directory information or for provider participation. No more than 2 points will be removed for this item in the category. |
| Member Services | Any SOD or statement of findings for member services during the measurement year (2019) for failure to: maintain a functional member services phone line; provide correct information to callers; provide specific information upon written request. | Member services for 2019 | 2 points for any SOD or statement of findings for any of the three- member service items. No more than 2 points will be removed for this category. |
| Behavioral Health Parity Reporting Requirement | Any SOD for timeliness, completeness, and/or accuracy or failure to meet requirements on Behavioral Health Parity reports submitted for the measurement year (2019). | Parity reports submitted for 2019 | 2 points for any SOD for timeliness, completeness or for accuracy. No more than 2 points will be removed for this category. |
| Claims Payment and/or Denials | Any statement of deficiency or statement of findings related to claims payment and/or denials issues for year (2019). | Claims payment and/or denials data for 2019 | 4 points for a statement of deficiency or statement of findings. No more than 4 points will be removed for this category. |
| Total | 20 points |
Quality Incentive Tiers:
Plans are grouped into one of five tiers to determine the incentive award. The five tiers are based on the percentage of points earned by the plans and were set using the 2017 Quality Incentive scores. The tiers are set without the addition of the bonus points and applied to the 2020 Quality Incentive.
| Tier | Range of Scores |
|---|---|
| Tier 1 | 100.00 – 80.09 |
| Tier 2 | 80.08 – 67.08 |
| Tier 3 | 67.07 – 49.10 |
| Tier 4 | 49.09 – 36.08 |
| Tier 5 | 36.07 – 0.00 |
Section 3: Quality Incentive Award Results
In 2020, the fifteen NYS Medicaid Managed Care plans were grouped into five tiers based on their Quality Incentive scores. The table below shows the tier assigned to each plan. The 2020 Quality Incentive awards become effective for capitation rates and for auto-assignment preference on April 1, 2021.
| MMC Quality Incentive 2020 Quality Points NORMALIZED to 100 based on highest score June 9, 2021 |
|||||||
|---|---|---|---|---|---|---|---|
| Incentive Premium Award (%) | Plan Name | Normalized Quality Points = Quality Points/Highest Score | Satisfaction Points (30 points possible) | PQI Points (20 points possible) | Compliance Points (20 points possibly subtracted) | Total Points | Percent (up to 100%) |
| Tier 1 | |||||||
| Tier 2 | MetroPlus Health Plan | 100 | 15 | 5 | 0 | 120 | 80 |
| Tier 2 | Healthfirst PHSP, Inc. | 92.96 | 15 | 5 | 0 | 112.96 | 75.31 |
| Tier 2 | Independent Health | 71.83 | 20 | 20 | 0 | 111.83 | 74.55 |
| Tier 2 | Fidelis Care New York, Inc. | 77.46 | 20 | 5 | 0 | 102.46 | 68.31 |
| Tier 2 | Empire BlueCross BlueShield HealthPlus | 78.87 | 15 | 8 | 0 | 101.37 | 67.58 |
| Tier 3 | MVP Health Care | 59.15 | 25 | 13 | 0 | 96.65 | 64.44 |
| Tier 3 | CDPHP | 63.38 | 25 | 10 | -2 | 96.38 | 64.25 |
| Tier 3 | HealthNow New York Inc. | 59.15 | 15 | 18 | -2 | 89.65 | 59.77 |
| Tier 3 | Affinity Health Plan | 76.06 | 15 | 0 | -4 | 87.06 | 58.04 |
| Tier 3 | Excellus BlueCross BlueShield | 61.97 | 20 | 0 | 0 | 81.97 | 54.65 |
| Tier 4 | HIP (EmblemHealth) | 61.97 | 15 | 0 | -4 | 72.97 | 48.65 |
| Tier 4 | YourCare Health Plan | 60.56 | 10 | 0 | -4 | 66.56 | 44.38 |
| Tier 4 | UnitedHealthcare Community Plan | 40.85 | 10 | 13 | 0 | 63.35 | 42.23 |
| Tier 4 | Molina Healthcare | 45.07 | 15 | 5 | -2 | 63.07 | 42.05 |
| Tier 5 | WellCare of New York | 30.99 | 15 | 10 | -2 | 53.99 | 35.99 |
* Incentive premium awards were impacted by enacted budget actions for SFY 20-21 and may change to meet program fiscal targets.
If you have questions regarding the incentive premium award, please contact the Bureau of Acute & Managed Care Reimbursement at (518) 473-8822.
We welcome suggestions and comments on this publication. Please contact us at:
Bureau of Quality Measurement and Evaluation
Office of Quality and Patient Safety
Empire State Plaza
Albany, New York 12237
Telephone: (518) 486-9012
Fax: (518) 486-6098
E-mail: nysqarr@health.ny.gov