New York State Medicaid Update - April 2019 Volume 35 - Number 5
In this issue …
- Pharmacy Update
- Policy and Billing Guidance
- All Providers
- Change to Physical Therapy Visit Limit
- Expedited Partner Therapy to Promote Sexual Health
- Important Reminder: Verify Member Eligibility
- Attention Submitters of 837 Batch Transactions: Provide Proper EDI Contact Information
- eMedNY Offers Medicaid Provider Training
- New York Medicaid EHR Incentive Program Update
Pharmacy Reminder: Emergency Contraceptive Coverage
Both prescription and over-the-counter (OTC) emergency contraception is a covered benefit for Medicaid fee-for-service (FFS) and Managed Care (MMC) members with pharmacy benefits. Pharmacies providing services to FFS and MMC members should be aware, prepared, and ready to bill FFS or MMC for these services for members. It is unacceptable to turn a member away due to a pharmacy's inexperience with billing this benefit or software issues with billing (see below).
In accordance with Title 18 of New York Codes, Rules and Regulations (NYCRR) §505.3, non-prescription (OTC) emergency contraceptive drugs can be obtained without a written order from a practitioner.
Effective March 1, 2017 per Federal Drug Administration (FDA) guidelines, New York State Medicaid has eliminated age restrictions when dispensing non-prescription emergency contraceptive drugs without a written order. Prescription-only emergency contraceptive drugs continue to require a prescription. Non-prescription emergency contraceptive drugs do not require a fiscal order or a prescription.
Medicaid Fee-for-Service Billing
When dispensing OTC emergency contraception products without a written/electronic/oral order, the prescriber identification field for pharmacy claims may be left blank and the claim will still be processed. Additionally, enter a value of "5" in the Prescription Origin Code field 419-DJ, and a value of "99999999" in the Serial Number field 454-EK to indicate pharmacy dispensing, per the "Matching Origin Codes" article in the July 2016 Medicaid Update. It is recommended that the pharmacy be familiar with this type of billing and, if necessary, contact the pharmacy software vendor to ensure Medicaid member access to this benefit.
Managed Care Plan Billing
For information on billing managed care plans for OTC emergency contraception for MMC members without a written order, please check with the individual managed care plan. Contact information for plans is available at: http://mmcdruginformation.nysdoh.suny.edu/. It is recommended that the pharmacy be familiar with the plans specific to the area and their billing requirements and, if necessary, contact the software vendor to ensure Medicaid member access to this benefit.
Reporting of the National Drug Code is Required for all Fee-for-Service Physician Administered Drugs
Effective April 1, 2019, to improve claims accuracy and completeness, an accurate National Drug Code (NDC) must be reported for all physician-administered drugs billed on the Institutional claim form, this includes drugs obtained at the 340B price indicated by the "UD" modifier. There will be no exceptions to this policy.
The eMedNY billing system will enforce this requirement effective July 1, 2019. This means that starting July 1, 2019, for any physician-administered drug billed under Ambulatory Patient Groups (APG) that does not include an accurate NDC, the line will not pay. Note, all APG fee schedule drugs will still require providers to code the number of units and acquisition cost for the claim line to pay.
Questions regarding Medicaid fee-for-service (FFS) policy should be directed to the Office of Health Insurance Programs, Division of Program Development and Management at(518) 473–2160 . Billing procedure questions should be directed to the eMedNY Call Center at 800-343-9000.
Change to Physical Therapy Visit Limit
Effective July 1, 2018, pursuant to enacted changes in Social Services Law SSL §365-a, the physical therapy visit limit for fee-for-service (FFS) and Medicaid Managed Care (MMC) was increased from 20 visits to 40 visits per member in a 12-month period. For Medicaid FFS enrollees, the 12-month benefit year begins on April 1st of each year and runs through March 31st of the following year. For MMC enrollees, the twelve-month benefit year is per calendar year, beginning January 1st of each year and runs through December 31st of the same year.
There has been no change to the occupational therapy and speech therapy benefits. Coverage of occupational and speech therapy will remain capped at 20 visits per therapy type each year. Certain Medicaid enrollees, settings, and circumstances are exempt from the visit limitations. These include:
- Children from birth to age 21 (until their 21st birthday)
- Individuals with developmental disabilities (members with restriction/exception code "95" on file)
- Individuals with a traumatic brain injury (TBI) (members with TBI* or restriction/exception code "81" on file)
- Individuals with both Medicare Part B and Medicaid (dually eligible) when the service is covered by Medicare
- Rehabilitation services received as a hospital inpatient
- Individuals receiving rehabilitation services in a nursing home in which they reside
- Rehabilitation services provided by a certified home health agency (CHHA)
*TBI as defined in Public Health Law Article 27-cc: § 2741. "Traumatic brain injury" means an acquired injury to the brain caused by an external physical force resulting in total or partial disability or impairment and shall include but not be limited to damage to the central nervous system from anoxic/hypoxic episodes or damage to the central nervous system from allergic conditions, toxic substances, and other acute medical/clinical incidents. Such term shall include, but not be limited to, open and closed brain injuries that may result in mild, moderate or severe impairments in one or more areas, including cognition, language, memory, attention, reasoning, abstract thinking, judgment, problem-solving, sensory perceptual and motor abilities, psycho-social behavior, physical functions, information processing, and speech. Such term shall not include progressive dementias and other mentally impairing conditions, depression and psychiatric disorders in which there is no known or obvious central nervous system damage, neurological, metabolic and other medical conditions of chronic, congenital or degenerative nature or brain injuries induced by birth trauma.
Reminders for Medicaid FFS Billing:
- Requirement to use modifiers: All providers submitting claims for physical, occupational, and speech therapy must use a procedure code modifier. The modifier identifies the therapy type and provides a mechanism for counting and matching. Without a modifier, the claim will be denied.
- "GN" – speech therapy service
- "GO" – occupational therapy service
- "GP" – physical therapy service
- Medicaid FFS utilizes the prior authorization (PA) mechanism to track therapy visits. A PA must be obtained for each therapy visit for enrollees not exempt from the limitation. The PA number must be included on the claim at the time of submission. If no PA number is on the claim and one is required, the claim will be denied. PA must be obtained through the PA/Dispensing Validation System (DVS). A unique PA number must be obtained through the DVS for each visit. The DVS operates on "real-time" and will give an immediate response to a request for PA. A DVS authorization does not guarantee payment. However, without a PA the claim will be denied. A request for a PA should be submitted before the provision of service. The request may be made after the date of the service and can be approved if the enrollee has not already been authorized for the maximum number of visits. A maximum of 20 prior authorization numbers will be issued for occupational therapy, 20 for speech therapy, and 40 for physical therapy. Further instructions on obtaining a DVS authorization number can be accessed online at: https://www.emedny.org/selfhelp/ePACES/ePACESRefSheets.aspx.
- Failing to obtain rehabilitation therapy PA prior to or on the date of service puts the provider's reimbursement at risk. It is important for the provider to know how many of the rehabilitation therapy visits an enrollee has already used because Medicaid will only pay for 20 occupational therapy visits, 20 speech therapy visits, and 40 physical therapy visits per benefit year for each member that is not exempt.
Additional information may be found in the Rehabilitation Services Manual online at: https://www.emedny.org/ProviderManuals/RehabilitationSrvcs/index.aspx. Policy questions for Medicaid FFS enrollees should be directed to the Office of Health Insurance Programs (OHIP) at (518) 473–2160 . Questions regarding MMC reimbursement and/or billing requirements should be directed to the enrollee's MMC plan. MMC benefit coverage questions should be directed to OHIP's Division of Health Plan Contracting and Oversight (DHPCO) at covques@health.ny.gov or (518) 473–1134.
Expedited Partner Therapy to Promote Sexual Health
Background
An important part of achieving sexual health is preventing sexually transmitted infections (STI). Chlamydia, a very common STI, is the most frequently reported communicable disease in New York State (NYS) with over 116,000 diagnoses last year. Chlamydia is a leading cause of pelvic inflammatory disease (PID), ectopic pregnancy, and infertility. Many people experience multiple episodes of chlamydia reinfection soon after treatment because they were reinfected by a partner who had an undiagnosed chlamydia infection. Recent data indicate that at least 12 percent of New Yorkers diagnosed with chlamydia are re-diagnosed with a new chlamydia infection within one year of treatment.
While the potential long-term consequences for untreated chlamydia can be serious, this STI is easily curable for most people. Expedited Partner Therapy (EPT) is the legal clinical practice of providing individuals with antibiotics (or a prescription for antibiotics) to deliver to their sexual partners as presumptive treatment for chlamydia, without completing a clinical assessment of those partners. The New York State Department of Health (NYSDOH) strongly encourages providers to utilize EPT. The Centers for Disease Control and Prevention (CDC), along with the American College of Obstetrics and Gynecology (ACOG), American Medical Association (AMA), American Bar Association, and Society for Adolescent Medicine are among several national professional organizations that recommend EPT as an effective and practical strategy for treating the sex partners of people diagnosed with chlamydia.1,2,3,4,5 Randomized controlled trials have found that this strategy decreases rates of chlamydia reinfection among index patients and increases the proportion of sex partner(s) reported to be treated for chlamydia.6,7
Important Information and Considerations:
- EPT for chlamydia is authorized under New York Codes, Rules, and Regulations (NYCRR) §23.5, of Title 10, and §2312 of NYS Public Health Law.8,9 Health care providers or pharmacists who administer EPT in accordance with this law are not subject to civil or criminal liability and will not be deemed to have engaged in professional misconduct as a result of this strategy.
- EPT prescriptions are currently waived from the NYS electronic prescription ("e-prescribe") mandate. A blanket waiver letter of the electronic prescribing requirements is available at: https://www.health.ny.gov/professionals/narcotic/electronic_prescribing/docs/2019-02-21_blanket_waiver_letter.pdf.
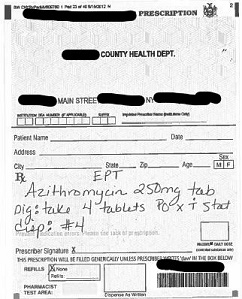
- Paper prescriptions may be used for EPT. Providers may order prescription pads at: https://www.health.ny.gov/forms/doh-250. If providing a paper prescription for EPT the prescription needs to include:
- The designation "EPT" must be written in the body of the prescription form above the name of the medication and dosage for all prescriptions issued.
- If the sex partner's name, address, and date of birth are not available, the written designation "EPT" shall be sufficient for the pharmacist to fill the prescription (see example image).
- If the name, address, and date of birth of the sex partner are available, this information should be written in the designated area of the prescription form.
- Medication costs for Medicaid patients are a covered service and may be billed to the Program by the dispensing pharmacy. Medication costs for the sex partner may be self-pay (paid by the person who picks up the prescription) or paid by the sex partner's health insurance. Alternatively, the provider may choose to directly dispense medications to both patients and partners at no cost instead of writing a prescription.
- EPT medication may be provided directly to the patient to deliver to their sex partner(s). This approach is preferred to a written prescription, especially for the adolescent population, because prescriptions may introduce barriers to accessing EPT such as transportation, cost, and/or confidentiality. Providing medication directly to the index patient may also be more convenient for providers.
- As stated in NYCRR §23.5, health education materials must accompany EPT (medication or prescription). EPT health education materials may be ordered from NYSDOH at: https://www.health.ny.gov/forms/order_forms/ept.htm.
- The New York City Department of Health and Mental Hygiene also produces EPT-related health education materials which are available at: https://www1.nyc.gov/site/doh/providers/health-topics/expedited-partner-therapy.page.
- Severe adverse reactions such as anaphylaxis are extremely rare with azithromycin. Milder side effects that may impact the success of treatment, including nausea and vomiting, occur in fewer than five percent of patients.10
- EPT should not be provided for any partner(s) when the patient with chlamydia is co-infected with gonorrhea, syphilis, and/or HIV. Treatment for chlamydia alone is not adequate to treat these other infections.
- EPT may not be clinically appropriate for every patient. For example, EPT is not recommended for gay, bisexual, and other men who have sex with men due to the lack of study data on EPT's effectiveness in this population and the risk of STI/HIV co-infection among partners.11
Additional EPT guidelines, resources, and information are available at: https://www.health.ny.gov/diseases/communicable/std/ept/index.htm.
References:
- Centers for Disease Control and Prevention. Expedited Partner Therapy in the Management of Sexually Diseases: Review and Guidance. https://www.cdc.gov/std/treatment/eptfinalreport2006.pdf. Published 2006. Accessed October 30, 2018.
- ACOG Committee Opinion No. 737. Obstet Gynecol. 2018;131(6). doi:10.1097/aog.0000000000002621.
- American Medical Association. Expedited partner therapy. In: Code of medical ethics of the American Medical Association: current opinions with annotations. 2014-2015 ed. Chicago (IL): AMA; 2015. p. 274-5.
- American Bar Association. Recommendation No. 116A. Adopted by the House of Delegates August 11-12, 2008. Chicago (IL): ABA; 2008. Available at: http://www.americanbar.org/content/dam/aba/directories/policy/2008_am_116a.authcheckdam.pdf. Retrieved October 30, 2018.
- Burstein GR, Eliscu A, Ford K, et al. Expedited Partner Therapy for adolescents diagnosed with chlamydia or gonorrhea: A position paper of the Society for Adolescent Medicine. J Adolesc Health. 2009;45(3):303-309. doi:10.1016/j.jadohealth.2009.05.010.
- Shiely F, Hayes K, Thomas KK, et al. Expedited Partner Therapy: A robust intervention. Sex Transm Dis. 2010:1. doi:10.1097/olq.0b013e3181e1a296.
- Golden MR, Whittington WL, Handsfield HH, et al. Effect of expedited treatment of sex partners on recurrent or persistent gonorrhea or chlamydial infection. N Engl J Med. 2005;352(7):676-685. doi:10.1056/nejmoa041681.
- New York State Codes, Rules, and Regulations Title 10, Section 23.5 - Expedited partner therapy for chlamydia trachomatis infection. Available at: https://regs.health.ny.gov/content/section-235-expedited-partner-therapy-chlamydia-trachomatis-infection.
- New York State Public Health Law Section 2312 — Expedited partner therapy for chlamydia trachomatis infection. Available at: http://public.leginfo.state.ny.us/lawssrch.cgi?NVLWO:.
- Rubinstein E. Comparative safety of the different macrolides. Int J Antimicrob Agents. 2001;18:71-76. doi:10.1016/s0924-8579(01)00397-1.
- Health.ny.gov. Expedited Partner Therapy Guidelines for Health Care Providers in NYS for Chlamydia trachomatis. Available at: https://www.health.ny.gov/diseases/communicable/std/ept/guidelines_for_providers.htm.
Important Reminder: Verify Member Eligibility
The Medicaid Eligibility Verification System (MEVS) and Dispensing Validation System (DVS) enable providers to verify member eligibility prior to provision of services and obtain authorization for specific services covered under DVS. A member, also known as client or recipient, must present an official Common Benefit Identification Card (CBIC) to the provider when requesting services. The issuance of an Identification Card does not constitute full authorization for provision of medical services and supplies. The member's eligibility must be verified through eMedNY to confirm the member's eligibility for services and supplies. A provider not verifying eligibility prior to provision of services will risk the possibility of nonpayment for those services.
The verification process through eMedNY can be accessed using one of the following methods:
- Telephone verification process, Audio Response Unit (ARU).
- Other access methods:
- ePACES (Electronic Provider Assisted Claim Entry System);
- Central Processing Unit (CPU)-to-CPU link;
- eMedNY eXchange;
- dial-up FTP (File Transfer Protocol);
- File Transfer Service (FTS) using SOAP (Simple Object Access Protocol); and
- CORE Web Services.
Additional information regarding MEVS access methods is found at: https://www.emedny.org/ProviderManuals/5010/MEVS%20Quick%20Reference%20Guides/5010_MEVS_Methods.pdf.
The MEVS/DVS Provider Manual is located on the eMedNY website and provides information on the CBIC, access methods for verification, a description of eligibility benefit responses, definitions of exception codes, and a list of county/district office codes. The MEVS/DVS Provider manual can be found at: https://www.emedny.org/ProviderManuals/5010/MEVS/MEVS_DVS_Provider_Manual_(5010).pdf.
Questions regarding MEVS or DVS should be directed to the eMedNY Call Center at (800) 343–9000.
Attention Submitters of 837 Batch Transactions: Provide Proper EDI Contact Information
The Submitter Name and Submitter Electronic Data Interchange (EDI) contact information contained in the PER segment of Loop 1000A in all 837 X12 claims transactions is an important part of troubleshooting problem files. The purpose of this segment is to identify to the entity receiving the X12 transaction a contact that can remediate EDI-related file issues immediately.
It is important to review this detail regularly, to ensure that the PER segment is populated with valid, and current, contact details. This will ensure that there is minimal delay if a problem is identified with the submitted file and an outbound call or email is necessary. If your X12 transactions are being submitted by a service provider/software vendor, please share this information with them.
For X12 Implementation/Companion guide questions, X12 transaction support, and X12 testing, submitters can contact EDI/HIPAA (Health Insurance Portability and Accountability Act) Transaction Support at: emednyHIPAAsupport@csra.com. For operational issues, including batch submission errors, submitters should contact Tier 2 Operations at: emednyproviderservices@csra.com.
eMedNY Offers Medicaid Provider Training
Training is very valuable when:
- Providers are new to Medicaid billing
- Providers have billing questions
- Anyone is interested in learning more about ePACES
Providers who are new to Medicaid billing, have billing questions, or who are interested in learning more about ePACES should consider registering for Medicaid training. eMedNY offers various types of training to providers and their billing staff including seminars and webinars. Seminars are in-person training sessions with groups of providers and billing staff conducted at locations throughout New York State. Webinar training sessions are conducted online and offer providers the convenience of joining the meeting from their computer and telephone. Many of the training sessions planned for the upcoming months offer detailed information and instruction about Medicaid's web-based billing and transaction program ePACES.
The electronic Provider Assisted Claim Entry System (ePACES) allows enrolled providers the ability to submit the following types of transactions:
- Eligibility Verifications
- Claims
- Claim Status Requests
- DVS and Prior Approval Requests
Physicians, nurse practitioners, private duty nurses, and other providers using the professional format can even submit claims in "real-time" via ePACES. Real-time means that the claim is processed within seconds and professional providers can get the status of a real-time claim, including the paid amount, without waiting for the remittance advice. Training dates, locations, and fast and easy registration are available on the eMedNY website at: http://www.emedny.org/training/index.aspx.
The training descriptions should be reviewed carefully to identify the training that is appropriate for each provider's billing requirements. Webinar registration confirmation will be sent to the provider's email address. Questions related to webinar registration should be directed to the eMedNY Call Center at (800) 343–9000.
New York Medicaid EHR Incentive Program
Distribution to Eligible Professionals & Eligible Hospitals Since the Start of the Program in 2011*
| Number of Payments: | Distributed Funds: |
|---|---|
| 39,908 | $970,735,163 |
*As of 3/25/2019
The New York (NY) Medicaid Electronic Health Record (EHR) Incentive Program promotes the transition to EHRs by providing financial incentives to eligible professionals (EPs) and eligible hospitals (EHs). Providers who demonstrate Meaningful Use (MU) of their certified EHR technology (CEHRT) are leading the way towards interoperability, which is the ability of healthcare providers to exchange and use patient health records electronically. The goal is to increase patient involvement, reduce costs, and improve health outcomes.
General Announcements
2018 MEIPASS Opening Date
MEIPASS is not currently accepting attestations for Payment Year (PY) 2018 meaningful use. Announcements will be made when MEIPASS is ready to accept PY2018 attestations. Providers can sign up for the program LISTSERV to receive important announcements at: https://www.health.ny.gov/health_care/medicaid/redesign/ehr/listserv/index.htm.
Pre-validation
Individual and group EPs who have already determined their Medicaid Patient Volume (MPV) may utilize the pre-validation services offered by the NY Medicaid EHR Incentive Program. Pre-validation enables EPs to submit their data prior to attesting for preliminary review. Pre-validation prior to submitting the complete attestation may subsequently reduce the time of State review.
Please note: The NY Medicaid EHR Incentive Program is unable to review data until 90 days have passed from the end date of the 90-day MPV Reporting Period. This period is required to allow Medicaid claims to be processed and finalized. Therefore, providers initiating pre–validation with an MPV Reporting Period that ended within the last 90 days will receive notice from NY Medicaid Support about the inability to review the data. The NY Medicaid EHR Incentive Program recommends selecting an MPV Reporting Period using the prior calendar year method. This prevents the possibility of timing out of the twelve months prior to attestation method. The necessary forms for completion can be found as follows:
- Individual EPs – Pre-Validation: https://www.health.ny.gov/health_care/medicaid/redesign/ehr/repository/docs/ind_ep_pre_val.xlsx
- Group EPs – Pre-Validation: https://www.health.ny.gov/health_care/medicaid/redesign/ehr/repository/docs/grp_ep_pre_val.xlsx
For more information about Pre-Validation services, please contact hit@health.ny.gov.
2015 Edition CEHRT
Beginning in PY2019, EPs attesting to MU in the EHR Incentive Program are required to meet the measures for MU Stage 3 and must use a 2015 edition of CEHRT. Additional resources are available on the Office of the National Coordinator for Health Information Technology (ONC) website at: http://www.healthit.gov/how-do-i/providers. For more information and assistance, please contact the NY Medicaid EHR Incentive Program Support Team by phone at (877) 646–5410, Option 2, or via email at hit@health.ny.gov.
MU Measures
MU Stage 3 establishes eight objectives, each with its own required activity to demonstrate that the EP is meaningfully using CEHRT. Centers for Medicaid and Medicaid Services (CMS) calls these activities measures and EPs must either meet the measure(s) for each objective or show that they qualify for an exclusion to the measure(s). A list of the eight objectives can be found under the "Meaningful Use Measures" expandable header at: https://www.health.ny.gov/health_care/medicaid/redesign/ehr/2019_opt_stage3.htm.
Regional Extension Centers
New York State (NYS) Regional Extension Centers (RECs) offer free support to help providers achieve Meaningful Use of CEHRT. Support provided by NYS RECs includes but is not limited to: answers to questions regarding the program and requirements, assistance on selecting and using CEHRT, or help meeting program objectives. NYS RECs offer free assistance for all practices and providers located within New York.
RECs were established nationwide to assist primary care providers in the adoption and meaningful use of EHRs. RECs work to optimize the use of EHRs so that providers can become meaningful users, engage in new health care transformation and quality initiatives, and participate in payment delivery reform programs. NYS has two RECs that provide support services to healthcare providers as they navigate the EHR adoption process and achievement of MU.
New York City Regional Electronic Adoption Center for Health (NYC REACH)
NYC REACH offers support services to providers located inside the five boroughs of NYC. For more information, please visit the NYC REACH website at: https://www.nycreach.org. For questions related to NYC REACH, please call 1-347-396-4888 or email pcip@health.nyc.gov.
New York eHealth Collaborative (NYeC)
NYeC offers support services to providers located outside the five boroughs of NYC. For more information, please visit the NYeC website at: https://www.nyehealth.org. For questions related to NYeC, please call 1-646-619-6400 or email hapsinfo@nyehealth.org.
Please Complete the New York Medicaid EHR Incentive Program Customer Satisfaction Survey
Survey responses provide valuable feedback and assist the NY Medicaid EHR Incentive Program in:
- developing webinars on the Health Information Exchange and the Patient Portal;
- using the LISTSERV® to send messages that are relevant to EPs (please see details below to subscribe);
- updating the program web site for ease of use; and
- hosting targeted training webinars such as the Navigating the EHR Incentive Program Web site webinar to best assist providers.
The NY Medicaid EHR Incentive Program values provider insight. The survey can be found at: https://www.surveymonkey.com/r/NY_EHR.
Webinars and Q&A Sessions
A calendar with the date and times of each webinar listed below, as well registration information, can be found at:https://www.health.ny.gov/health_care/medicaid/redesign/ehr/calendar/.
EP Stage 3 Meaningful Use
This webinar provides guidance to EPs about the requirements to attest to MU Stage 3 for the NY Medicaid EHR Incentive Program. Topics covered include:
- Medicaid Eligibility Criteria
- Brief Overview of the CMS Regulations
- MU Objectives and Measures
- Clinical Quality Measures (CQM)
Register at: https://register.gotowebinar.com/rt/6268737294881481475.
Meaningful Use Public Health Reporting
This webinar will provide an in-depth review of the MU Modified Stage 2 and Stage 3 Public Health Reporting Objectives, which are available to EPs. The webinar will also include information on how EPs can meet the Public Health Reporting Objective.
Register at: https://register.gotowebinar.com/rt/8341393679052665603.
Security Risk Analysis (SRA)
This webinar provides guidance to EPs about the SRA requirements to meet MU Objective 1: Protect Patient Health Information. Topics covered include:
- MU Objective 1: Protect Patient Health Information
- SRA Toolkit
- Safety Measures to Consider
- Common Considerations and Creating an Action Plan
Register at: https://register.gotowebinar.com/rt/1873662764857368066.
Visit the Web Site
Additional information about the NY Medicaid EHR Incentive Program can be found at: https://www.health.ny.gov/ehr. Please use the links provided below to go directly to the web page for the following categories:
- Eligible Hospital Requirements
https://www.health.ny.gov/health_care/medicaid/redesign/ehr/eh.htm - Public Health Reporting Objective Information
https://www.health.ny.gov/health_care/medicaid/redesign/ehr/publichealth/ - Post-Payment Audit Guidance
https://www.health.ny.gov/health_care/medicaid/redesign/ehr/audit/ - Frequently Asked Questions (FAQs)
https://www.health.ny.gov/health_care/medicaid/redesign/ehr/faqs/phr.htm - Materials and Information – Document Repository
https://www.health.ny.gov/health_care/medicaid/redesign/ehr/repository/index.htm - Webinar Calendar
https://www.health.ny.gov/health_care/medicaid/redesign/ehr/calendar/ - Sign up to receive LISTSERV® messages
NY Medicaid EHR Incentive Program and Public Health Reporting Objective
https://www.health.ny.gov/health_care/medicaid/redesign/ehr/listserv/index.htm - Archives
https://www.health.ny.gov/health_care/medicaid/redesign/ehr/archives/ - Contact Information
https://www.health.ny.gov/health_care/medicaid/redesign/ehr/contact.htm
Questions
The EHR Incentive Program has a dedicated support team ready to assist. Please contact the program at: 1-877-646-5410 (Option 2) or via email at: hit@health.ny.gov.
The Medicaid Update is a monthly publication of the New York State Department of Health.
Andrew M. Cuomo
Governor
State of New York
Howard A. Zucker, M.D., J.D.
Commissioner
New York State Department of Health
Donna Frescatore
Medicaid Director
Office of Health Insurance Programs