Briefing on DSRIP and Mailing to Medicaid Members
October 2015
- Webinar is also available in Portable Document Format (PDF)
DSRIP
Delivery System Reform Incentive Payment Program
The Need for Change
´New York Has Fared Poorly on Several Measures of Avoidable Hospital Use and Costs´
– NYS Health Foundation, "Getting More Bang for the Buck: The Quality Question"
| New York State Ranked 50th for Potentially Avoidable Hospital Use and Cost of Care | |
|---|---|
| Hospital Admissions for pediatric asthma per 1000 children | 35 |
| Percent of adult asthmatics with ED or urgent care visit in past year | 31 |
| Percent of home health patients with a hospital admission | 49 |
| Hospital Care Intensity Index based on inpatient days and inpatient visits among Chronically Ill Medicare beneficiaries in the last 2 years of life | 50 |
SOURCE: Commonwealth Fund, October 2009 –"Aiming Higher: Results from a State Scorecard on Health System Performance, 2009"
MRT Waiver Amendment
- Medicaid Redesign Team convened January 2011 to develop an action plan to reshape Medicaid system to reduce avoidable costs and improve quality.
- In April 2014, Governor Andrew M. Cuomo announced that New York State and CMS finalized agreement on the MRT Waiver Amendment.
- Allows the state to reinvest $8 billion of the $17.1 billion in federal savings generated by MRT reforms.
- The MRT Waiver Amendment will:
- ✓ Transform the state´s Health Care System
- ✓ Bend the Medicaid Cost Curve
- ✓ Assure Access to Quality Care for all Medicaid members
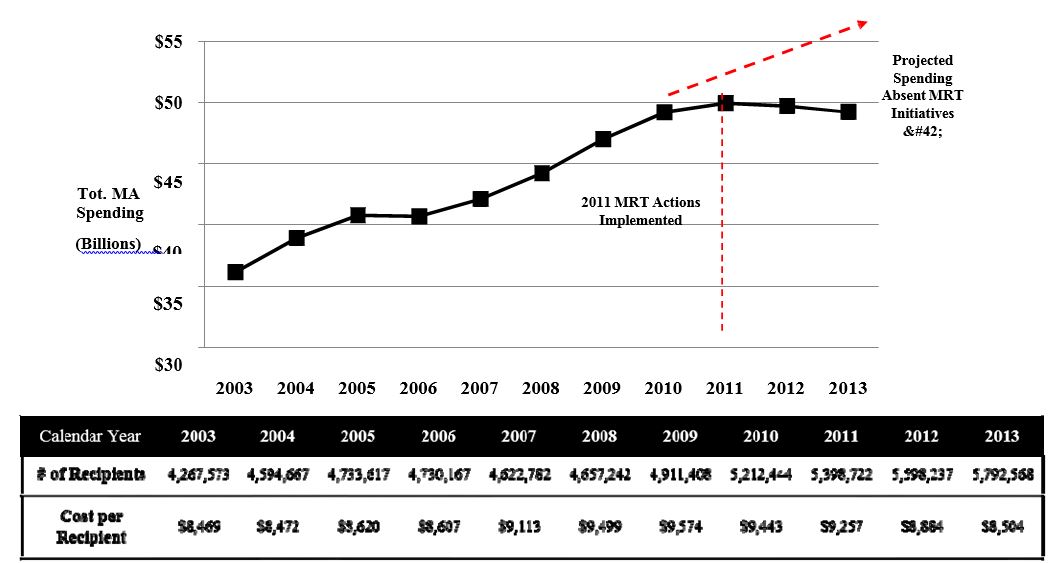
NYS Statewide Total Medicaid Spending (CY 2003 – 2013)
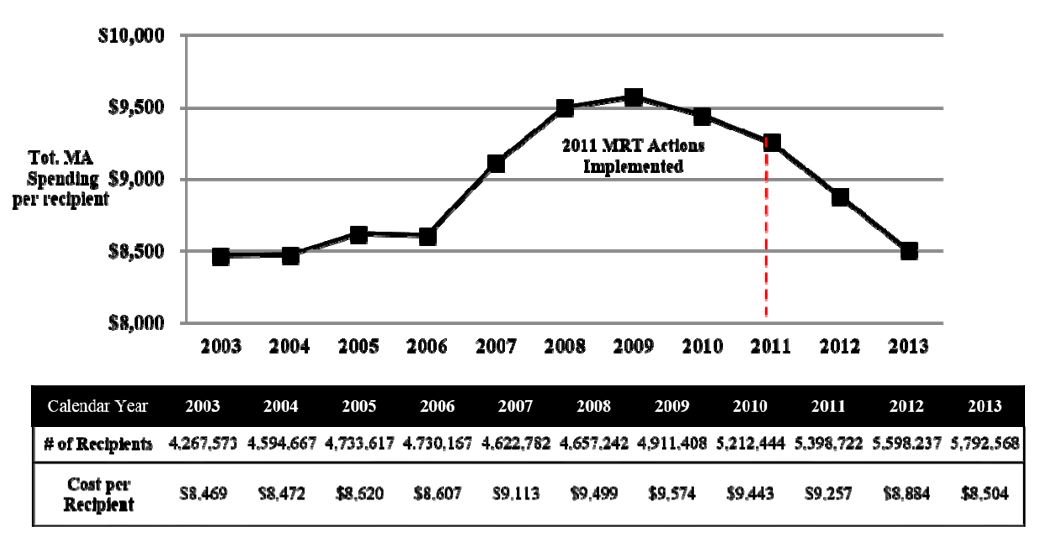
NYS Statewide Total Medicaid Spending per Recipient (CY 2003 – 2013)
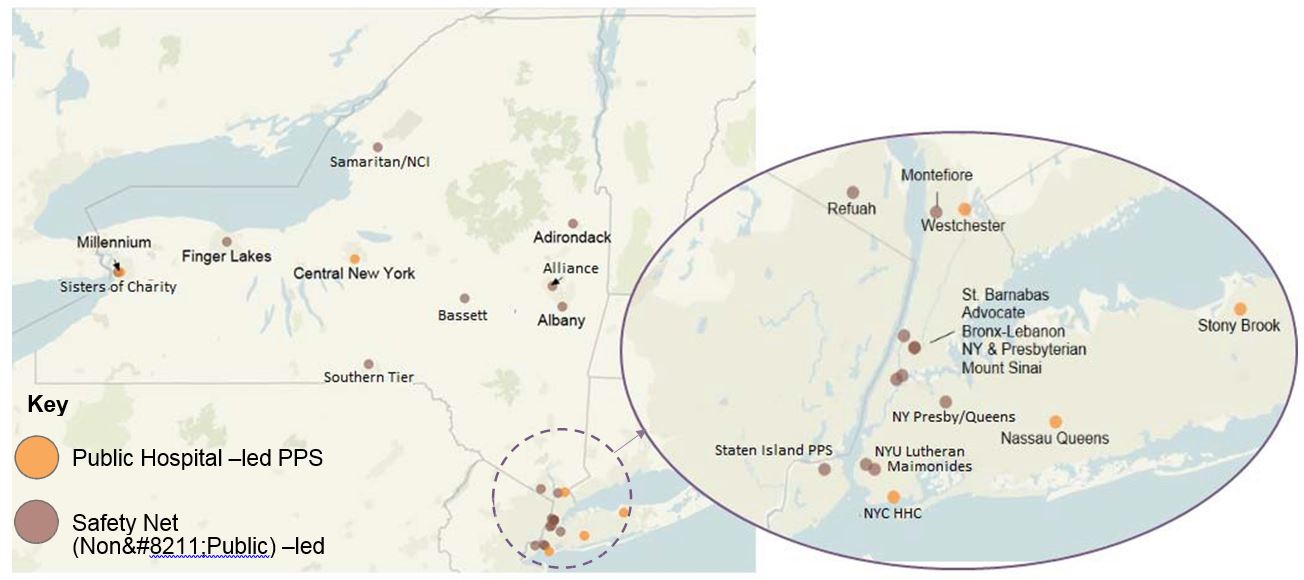
Performing Provider Systems (PPS): Local Partnerships to Transform the Delivery System
Partners should include:
- Hospitals
- Health Homes
- Skilled Nursing Facilities
- Clinics & FQHCs
- Behavioral Health Providers
- Home Care Agencies
- Other Key Stakeholders
Responsibilities must include:
- Community health care needs assessment based on multi–stakeholder input and objective data.
- Building and implementing a DSRIP Project Plan based upon the needs assessment in alignment with DSRIP strategies.
- Meeting and reporting on DSRIP Project Plan process and outcome milestones.
The 25 PPS in New York State
DSRIP Domain 3 – Sample Projects
| Domain 3: Clinical Improvement Projects | |
|---|---|
| A. | Behavioral Health |
| 3.a.i | Integration of primary care and behavioral health services |
| 3.a.ii | Behavioral health community crisis stabilization services |
| C. | Diabetes Care |
| 3.c.i | Evidence–based strategies for disease management in high risk/affected populations (adults only) |
| 3.c.ii | Implementation of evidence–based strategies to address chronic disease – primary and secondary prevention projects (adults only) |
| D. | Asthma |
| 3.d.i | Development of evidence–based medication adherence programs (MAP) in community settings – asthma medication |
| 3.d.ii | Expansion of asthma home–based self–management program |
| 3.d.iii | Implementation of evidence–based medicine guidelines for asthma management |
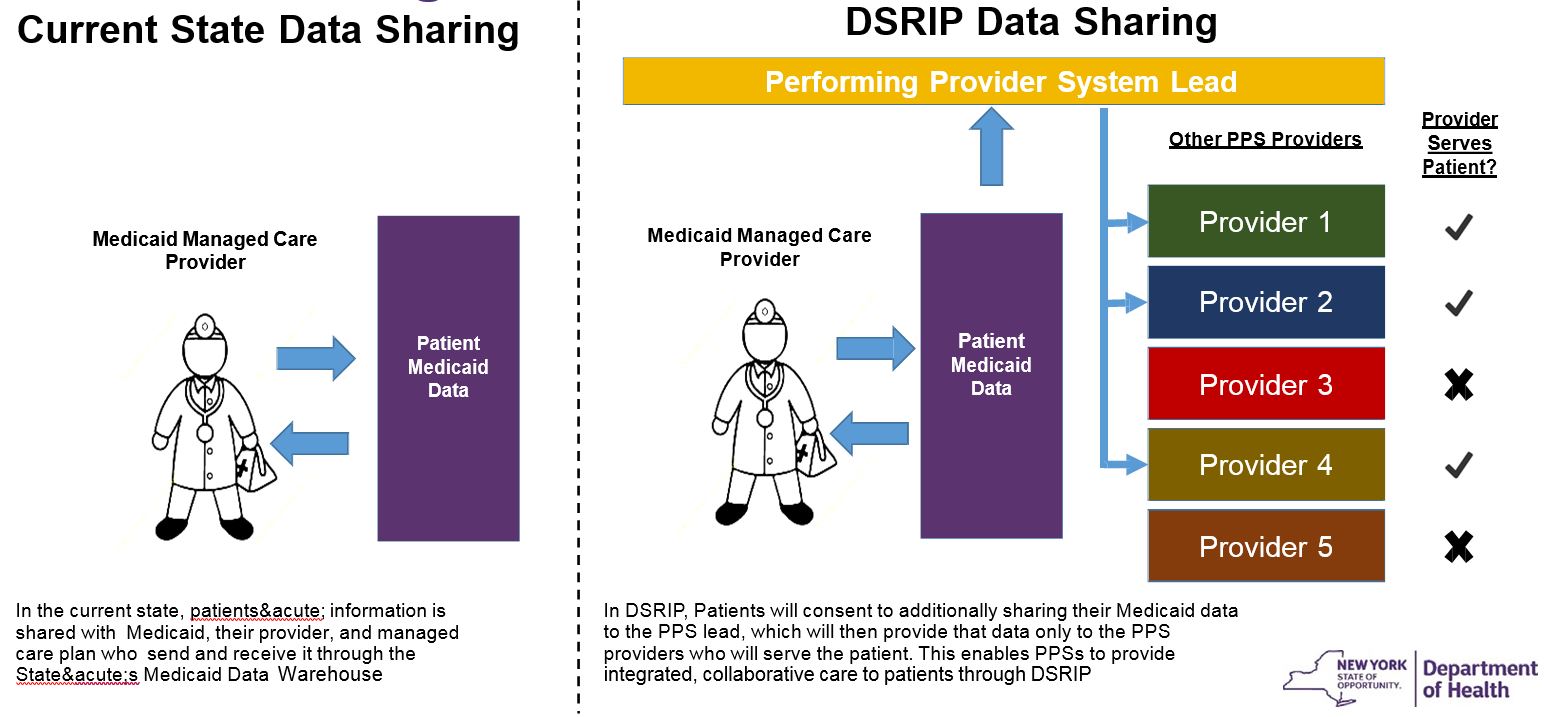
Medicaid Data Sharing
- State Medicaid data includes Personal Health Information (PHI):
- Medicaid member demographics
- Type of visit – office, Emergency Department, Inpatient
- Provider name
- Billing diagnoses (all alcohol and substance use information removed per federal law)
- Medicaid Members already consent to sharing their information when enrolling in Medicaid, and with managed care plans and providers for the purposes of clinical care, claims and quality review.
Key Foundation – Data Sharing
- Medicaid Member data is essential for PPS project implementation to identify patient populations for specific attention and outreach.
- PPSs have engaged providers and CBOs to conduct specific services such as outreach to non and low utilizing members and/or care management.
- Data sharing is key for effective collaboration between PPS and network partners in reaching and coordinating services to Medicaid members.
- The State has strict rules to protect Medicaid Member data and requires that any organization sharing or receiving Medicaid Member data from the Department adheres to federal and state data security protocols
Data Sharing – Current State vs. DSRIP
DSRIP Mailing to Medicaid Members
New York State Notice of Important Document
There is NO CHANGE to your MEDICAID.
Questions? Please call us at 1–855–329–8850 Monday – Friday 8:00 am – 8:00 pm, Saturday 9:00 am – 1:00 pm. If you need help in a language other than English, call 1–855–329–8850 and tell the Consumer Services Specialist. Help is free. TTY: 1–800–662–1220.
This letter is about a new program that New York State has started for our Medicaid members.
We know getting the health care you need is sometimes difficult. We want that to change. You should have a primary doctor. When you do not feel well, you should have a place to go besides an emergency room. We want you to know what health care you need and where to get it, so that you feel confident you can manage your health.
New York State Delivery System Reform Incentive Payment Program (DSRIP)
What is DSRIP?
The new program, the New York State "Delivery System Reform Incentive Payment Program" (DSRIP) will help you, your doctors and other health care providers work together better to serve your healthcare needs. DSRIP is a program in which doctors, clinics, hospitals, medical and community services in your area work together to build a better health care system. This will help you get better health care. These groups of providers are forming what is called a "Performing Provider System" (PPS). PPS providers have worked to understand what your community needs to improve health care. They are now planning how to meet those needs. To see the full list of PPS in your region and throughout the state, please visit the following website: (https://www.health.ny.gov/health_care/medicaid/redesign/dsrip/providers_professionals.htm) and look for "PPS Contact List" within the Introductory Information box.
Medicaid Member Mailing
- Introduce Members to DSRIP and State efforts on health care system change
- Advise Medicaid Members of potential benefits of DSRIP and to provide option to not have their data shared (opt–out) by calling Call Center or mailing opt–out form
- Mailing to be sent to all active Medicaid Members including dual eligibles
- Excluded from the mailing:
- Out–of–state addresses and
- Clients in non–Medicaid programs such as the Family Planning Benefit and Child Health Plus and those in partial Medicaid programs such as Emergency Services
- Dedicated DSRIP phone number (1–855–329–8850*) at the Medicaid Call Center to handle calls related to the DSRIP letter and the "opt out" process. Calls will be directed to language interpreters and staff trained on DSRIP FAQs.
Language and Accessibility
| ENGLISH | This is an important document. If you need help to understand it, please call 1‐855‐329‐8850. An interpreter will be provided free. |
| Español | Esto es un documento importante. Si necesitas ayuda en entenderlo, por favor llame al 1‐855‐329‐8850. Un intérprete será disponible gratuito. |
| 简 体字 | 这是一份重要文件。 如果您需要帮助理解此文件, 请打电话至 1‐855‐329‐8850 。 您会得到免 费翻译服务。 |
| 簡體字 | 这是一份重要文件。如果您需要幫助理解此文件,請打電話至 1‐855‐329‐8850 。 您会得到免費翻譯服務。 |
| Kreyól Ayisyen | Sa a se yon dokiman enpótan. Si ou bezwen éd pou konprann li, tanpri rele: 1‐855‐329‐8850. Y ap ba ou yon entéprét gratis. |
| Italiano | Il presente documento é importante. Per qualsiasi chiarimento puó chiamare il numero 1‐855‐329‐8850 . Un interprete sará disponibile gratuitamente. |
| 한국어 | 이것은 중요한 서류입니다. 도움이 필요하시면, 연락해 주십시오: 1‐855‐329‐8850 . 무료 통역이 제공됩니다. |
| Русский | Это важный документ. Если Вам нужна помощь для понимания этого документа, позвоните по телефону 1‐855‐329‐8850 . Переводчик предоставляется бесплатно. |
If you would like to view this letter in 18 point font, please visit the following website:
http://www.health.ny.gov/health_care/medicaid/redesign/dsrip/consumers.htm
What is "Opt Out"?
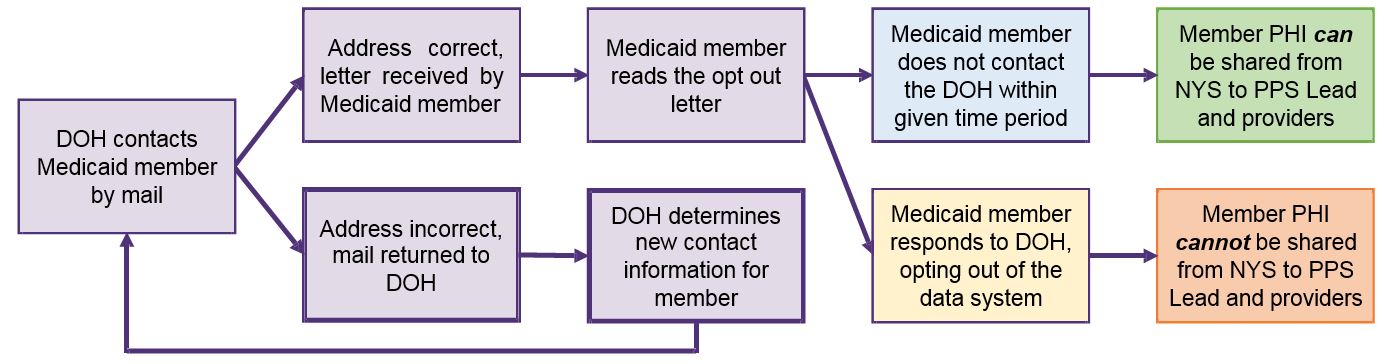
- NYS is modeling the DSRIP data consent process on the Medicare ACO model.
- Opt Out model: unless member formally opts–out of data sharing, their data will be shared.
- "Opt Out" means to NOT permit the sharing of any Medicaid data with the PPS.
- Until the Opt Out process is complete, the State supplied Medicaid data cannot be shared with the PPS partnering providers.
- The initial time period for Opting Out is 30 days from the receipt of the state mailing to return the "opt out" form or by calling the Medicaid Call center.
- The member who "opts out" will not have his/her Medicaid data shared with the PPS in subsequent files from the State.
- Members can opt out or opt in at any time by calling the Call Center or mailing the Opt– Out Form back.
- It can take up to 60 days to process the request to Opt Out or to Opt In and to notify the PPS of this change.
Opt–Out Process Flow
Phased Mailing and Timeline
- Phase I will be sent to 700,000 members in late October 2015. It will take place over a one–week period and targeted to Medicaid members state–wide who:
- Were eligible as of Sept 25
- Have claims for ambulatory sensitive conditions and avoidable ED/inpatient utilization
- Are HARP eligible
- Phase II will be sent to the remaining 5+ million members starting mid–February 2016
- Eligibility will be updated as of late January 2016
- Will be sorted by county and zip code and be statewide
- May take a month to send out all letters
- Ongoing letters and opt out forms to newly eligible
- Once the Phase I and Phase II is complete
- Will reoccur monthly
- Anticipate changes to Opt Out or Opt In within 60 days after approved eligibility
Mailing Timeline:
| Start | End | |
|---|---|---|
| Mailing Distribution | Thu 10/1/15 | Fri 10/23/15 |
| Opt Out Mailing Distribution | Mon 10/19/15 | Fri 10/23/15 |
| Medicaid Members Respond to mailing (30 days) | Mon 10/26/15 | Wed 11/25/15 |
| MAXIMUS Phone Support (Phase I) | Mon 10/26/15 | Wed 11/25/15 |
| General Phone Support Continues | Wed 11/25/15 | Sat 02/13/16 |
| PHASE 2 | Start | End |
| Opt Out Mailing Distribution (Phase II) | Mon 02/15/16 | Tues 03/15/16 |
| MAXIMUS Phone Support (Phase II + Ongoing) | Mon 02/15/16 | Ongoing |
The MAXIMUS phone line went live on October 16th
What if a Medicaid Member chooses NOT to allow this information to be shared?
- Medicaid members have the right to not have this personal protected health information shared with the local PPS by "opting out."
- Opting out means NYS will not share the Medicaid information with the local PPS about the Medicaid member´s previous care and treatment.
- Opting out means the PPS will not have Medicaid information about that member and may not be able to direct services to that member.
- Providers still share information with each other for patient treatment as they do today.
- All Medicaid members are still counted in State and PPS performance measures but data is not available at the opted out member level.
How Does This Impact Medicaid Members?
- 16–year–old John has severe asthma and has used ED 4 times in the last 6 months.
- 42–year–old Eduardo has chronic pain. He has been to the ED 9 times at 3 different hospitals in the last 6 months.
- Member has opted–out: Providers will treat the patients by utilizing resources they have at hand as they do today. They may or may not know about the other visits or other care received.
- Member´s data is shared: Data sharing would allow the PPS to identify the patients more quickly in a systematic way and alert providers. PPS may have a care manager or CHW reach the patients to ask about their needs for managing their conditions.
Summary of Key Information Points
- NYS launching new program called DSRIP for providers (PPS) to improve how care is provided to Medicaid members.
- To be able to implement the program effectively, NYS would like to share your Medicaid information with the PPS. The PPS may also share any necessary information with other partners in the PPS team to provide particular services.
- DSRIP will assume Medicaid members´ data can be shared. Your information will be shared with the PPS and its partners. By doing so, the PPS providers can do a better job coordinating your care and getting services to you.
- You have the right to opt out by mailing the form or calling the Call Center within 30 days after you receive the letter. Your information will not be shared with the PPS and its partners.
- The care you receive today will not change because you have decided to opt out.
Frequently Asked Questions
- What if I don´t receive a letter in the mail?
- If you don´t receive a letter, you may need to wait for the mailing to your area. If you do not receive a letter by March 15, 2016, please call 1–855–329–8850, Monday – Friday 8:00am – 8:00pm, Saturday 9:00am – 1:00pm.
- Can I change my mind?
- You can change your mind at any time about whether you want your information shared with other PPS providers or not
- Will my care change if I choose to opt out of data sharing?
- Your care will not change if you choose to opt out. To ensure you get all the benefits of the State´s efforts to improve how care is delivered, we encourage you to NOT opt out.
Medicaid Member Call Center
- There will be a dedicated DSRIP call center in order to answer questions beneficiaries may have regarding DSRIP in a timely manner. The call center will be open to Medicaid beneficiaries with DSRIP questions after October 16, 2015.
- The Center will have a dedicated DSRIP phone number (1–855–329–8850) to handle calls related to the DSRIP letter and the "opt out" process. Calls will be directed to language interpreters and staff trained on DSRIP FAQs.
- Reminder, the call center is available to Medicaid beneficiaries as a priority.
- CBOs, advocates, providers or PPS who have programmatic or policy questions should be using the dsrip@health.ny.gov with the subject line: Opt Out
Thank You!
DSRIP e–mail:
dsrip@health.ny.gov
Follow Us