Delivery System Reform Incentive Payment (DSRIP)
Measure Specification and Reporting Manual
- Manual also available in Portable Document Format (PDF)
Measurement Year 5
JULY 18, 2019
DSRIP@HEALTH.NY.GOV
Table of Contents
I. Overview of Requirements
Throughout the five demonstration years, Performing Provider Systems (PPS) will report on progress and milestones and be evaluated using specific quality measures associated with their projects. This section describes the domains and the methodology for establishing goals and annual improvement increments that will be used to determine performance attainment in each demonstration year.
Domains
All DSRIP measures are organized into 4 Domains. The lead partner for each PPS will be required to report measures for all four domains as specified in the project plan. The project requirement details for Domain 1 are available from the Independent Assessor organization. Domain 2, 3 and 4 measures are described in this measure specification and reporting manual.
Domain 1 - Overall Project Progress
Domain 2 - System Transformation
Domain 3 - Clinical Improvement
Domain 4 - Population-wide
Reporting Requirements for Measures
In this document, there are two responsible parties noted for reporting requirements: 1) PPS - data reported by the PPS to the New York State Department of Health (NYS DOH); and 2) NYS DOH - NYS DOH data sources used to calculate measures.
II. Methodology for Establishing Performance Goals, Annual Improvement
Targets, and High Performance
Performance Goals
Performance goals are intended to reflect best performance expected in New York State and the performance goals are the same, consistently applied to all PPS each year. The performance goal for each measure will not be changed throughout the DSRIP demonstration. CMS suggested using the top decile as a mechanism for establishing performance goals. For measures where the goal is to reduce an outcome or occurrence and a lower result is desirable, the lower decile is used, and for measures where the goal is to increase the occurrence and a higher result is desirable, the upper decile is used.
Several sources were considered for establishing goals. National data (NCQA´s Quality Compass for Medicaid) top decile results were compared to NYS Medicaid managed care (MMC) results for 2013. The NYS MMC results exceeded the national data for the majority of the measures. The 2013 MMC data was used to calculate results for quality measures by zip code of the member´s residence (excluding members with dual eligibility). Zip codes with less than 30 in the denominator or eligible population were excluded, and the 90th percentile was determined for the performance goal. Two quality measures had a small number of zip codes with 30 enrollees for the measure, therefore the top decile of health plan data was used for the performance goal. Efficiency measures (i.e., potentially preventable admissions, readmissions and emergency room visits) are population-based measures that have a skewed distribution when examined by zip code. For these measures, the performance goals were established by using all PPS baseline results and reducing the best performing baseline result by 20% of the gap to the default goal, so that the performance goal will provide every PPS with a goal that moves beyond the best current performance.
If data for the measure was not available for 2013, the performance goal was set to a default of 100%/0% for use in the first measurement year. The performance goals for these measures have been reset using the first measurement year PPS results. The performance goals were established with the same methodology as above by using PPS results from measurement year 1 and reducing the best performing baseline result by 20% of the gap to the goal. All performance goals that have not been set using MY 1 results will be established with PPS results from MY 2. Performance goals using dually eligible members will be established using results from MY 3.
If the measure specifications are changed to the degree that prior results are not comparable, CMS and NYS DOH have established a process for resetting performance goals. Details about the process are in section VIII.
Annual Improvement Targets (AITs)
Annual improvement targets for measures for a PPS will be established using the methodology of reducing the gap to the goal by 10%. The most current PPS measurement year (MY) result will be used to determine the gap between the PPS result and the measure´s performance goal, and then 10% of that gap is added to the most current PPS result to set the annual improvement target for the current MY (baseline for Measurement Year 1 and so on). Each subsequent year will continue to be set with an improvement target using the most recent year´s result. This will account for smaller gains/losses in subsequent years as performance improves toward the goal or measurement ceiling. If a PPS result for a MY meets or exceeds the performance goal, then the annual improvement target and the high-performance target (where applicable) for the next MY will equal the performance goal. Information on how achievement values are determined using AIT and performance goals is contained in the Achievement Value Guide.
Figure 1.
PERFORMANCE GOAL, ANNUAL IMPROVEMENT AND HIGH PERFORMANCE
Follow Up after Hospitalization for Mental Illness - 30 Days
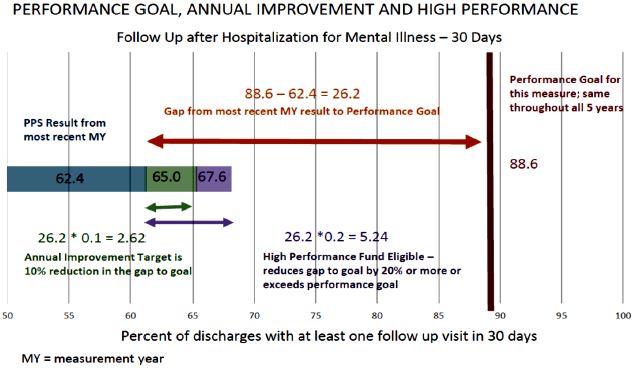
Percent of discharges with at least one follow-up visit in 30 days
As illustrated in Figure 1, the following example demonstrates the process for determining the annual improvement target (AIT):
| Process Step: Determine AIT | Description | Example |
|---|---|---|
| Establish gap amount | Goal - MY4 PPS´ result = gap | 88.6 - 62.4 = 26.2 |
| Calculate 10% of gap amount (increment) | Gap *.10 = increment | 26.2 * .10 = 2.62 |
| Set annual improvement target (AIT) by adding increment to PPS´ result | Increment + MY4 PPS´ result = MY5 AIT | 2.62 + 62.4 = 65.02 |
In this example, the annual improvement target for the PPS would be 65.02%, and the PPS result would need to meet or exceed that value to get the achievement value for payment for P4P measures. If the PPS´ result demonstrated a 20% reduction in the gap, and the measure is eligible for high-performance funds, the PPS would receive additional payment. Determining the AIT and high-performance is explained below:
| Process Step: Determine High Performance | Description | Example |
|---|---|---|
| Establish gap amount | Goal - MY4 PPS´ result = gap | 88.6 - 62.4 = 26.2 |
| Calculate 10% of gap amount (increment) | Gap *.10 = increment | 26.2 * .10 = 2.62 |
| Set annual improvement target (AIT) by adding increment to PPS´ result | Increment + MY4 PPS´ result = AIT | 2.62 + 62.4 = 65.02 |
| Evaluate high-performance (HP) using actual PPS performance for MY | (Increment*2) + MY4 PPS´ result = MY5 HPT OR higher than performance goal | 5.24 + 62.4 = 67.64 OR PPS > 88.6 |
The PPS result for MY5 is used to determine if the MY5 annual improvement target was met:
| Process Step: Determine next MY AIT | Description | Example |
|---|---|---|
| Determine MY5 PPS result (example provided here) | 66.38 | |
| Identify MY5 AIT | 65.02 | |
| Compare MY5 PPS result with MY5 AIT. Achievement Value awarded if MY5 PPS result is greater than or equal to MY5 AIT | 66.38 > 65.02 |
In this example, the MY5 annual improvement target was 65.02%. The MY5 PPS´ result (66.38%) exceeded the MY5 AIT so an AV would be awarded to the PPS for the measure.
High Performance Measures
Ten measures are part of the high-performance funds. These measures relate to avoidable hospitalizations, behavioral health and cardiovascular disease with the latter markers aligning with the nationwide Million Hearts Initiative on cardiac outcomes, in order to tackle the leading cause of mortality in New York State.
The ten measures eligible for high-performance are:A PPS can achieve high-performance through two methods: 1) achieving a reduction in gap to goal by 20% or more in any annual measurement year for a high-performance eligible measure; or 2) meeting or exceeding the measure´s performance goal for the measurement year for a high-performance eligible measure.
- Potentially Preventable Emergency Room Visits (All Population)
- Potentially Preventable Readmissions (All Population)
- Potentially Preventable Emergency Room Visits (BH Population)
- Antipsychotic Use in Persons with Dementia (SNF Long Stay Residents)
- Follow-up after Hospitalization for Mental Illness - Within 7 Days
- Follow-up after Hospitalization for Mental Illness - Within 30 Days
- Antidepressant Medication Management - Effective Acute Phase Treatment
- Antidepressant Medication Management - Effective continuation Phase Treatment
- Diabetes Monitoring for People with Diabetes and Schizophrenia
- Cardiovascular Monitoring for People with Cardiovascular Disease and Schizophrenia
- Controlling High Blood Pressure
- Medical Assistance with Smoking and Tobacco Use Cessation - Discussion of Cessation Strategies
Pay for Reporting (P4R) Measures
In cases where the measure type is Pay for Reporting (P4R), performing provider systems can earn incentive payment for successfully reporting the measures the PPS is responsible for reporting to NYS DOH within the timeframes for each MY. Measures that NYS DOH has the responsibility of reporting will be credited to the PPS in P4R situations.
Pay for Performance (P4P) Measures
In cases where the measure type is Pay for Performance (P4P), a PPS will receive achievement values for results that meet or exceed the annual improvement target or exceed the performance goal.
Improvement targets are determined based on a PPS´ previous annual performance in the measure and will be calculated by NYS DOH using the methodology described previously in this section.
If the denominator for a measure is less than 30 members or events, the data is considered too small to determine a statistically valid result; this is referred to as small cell size. Measure results with small cell size are not used for determining the achievement value for the measure. Prior to receiving the achievement value for the measure, PPS will need to have results for two consecutive years that are based on denominators greater than or equal to 30. For information about how these situations impact annual achievement value awards, see the Achievement Value Guide.
However, to provide PPS with as much information as possible, the results based on small cell size WILL be shared in PPS annual reports and used to create the AIT for the next measurement year so the PPS can understand current status.
III. Defining the Eligible Population for Performance Measurement
IMPORTANT NOTES:
- The eligible population is comprised of all members attributed to the PPS who qualify for the measure. The eligible population is NOT limited to people who have gone to providers or sites that are involved in project specific activities, or people residing in a specific county or area.
- Calculation of measure results are member-centric, evaluating each member for meeting criteria for the measure. The member is then attributed to the PPS as of the measurement time frame, such as end of the measurement year. Member eligibility information is evaluated for the measurement window, such as 12 months irrespective of PPS attribution.
- Members who are dually eligible (Medicare and Medicaid) will NOT be included in PPS measure results for claims-based measures for any measurement years
Note: Several measures currently include dual eligible members as the measure specifications do not require claim derived information. These measures include: Health Home enrollment measures (3 measures), Skilled Nursing Facility measures (Long-Stay Residents Depressive Symptoms and Antipsychotic Use for Persons with Dementia), and Hospital measures (ED for Uninsured and H-CAHPS).
Measure Eligible Population
Members are attributed to a specific PPS for performance measurement based on the qualifying services the members used, their assigned PCP or area of residence. In addition to the member´s attribution to a PPS, performance measures use specific criteria to determine eligibility for the measure.
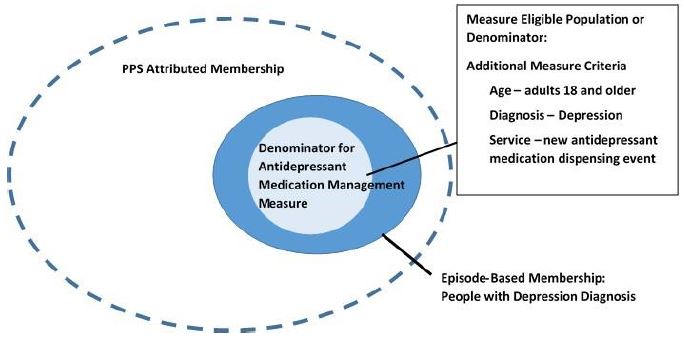
Measures are developed to capture the population for which a particular service is recommended; this is called the eligible population. To define the eligible population, measures often apply criteria such as age or diagnosis of a health condition to identify members in the eligible population. While some measures may apply to everyone in the PPS (population-based), others may capture a smaller group within the PPS membership that meet added measure specific criteria such as diagnosis of a health condition (episode- based).
For example, Figure 2 below shows how the PPS membership is narrowed to those with a diagnosis and then further to the measure´s eligible population or denominator for an episode-based measure, Antidepressant Medication Management.
Figure 2. Denominator Illustration
IV. Baseline Results for Project Approval - Completed
Specifically, with the exception of behavioral health Domain 3 measures (3.a.i - 3.a.v), if the performing provider system´s performance on the 2012 and 2013 data for the majority of the measures associated with a Domain 3 project was within 10 percentage points or 1.5 standard deviations to the performance goals, the project was not approved. If baseline PPS data was not available (such as measures requiring medical record data or survey responses), the PPS baseline result was assumed to be 0% for the purposes of approving projects. For example, if a project had seven associated measures, baseline PPS results were available for three of the measures and unavailable for four, the PPS would be approved as the majority of the measures (i.e. four of the seven) were not within 10 percentage points or 1.5 standard deviations.
In January 2015 all PPS passed the project approval test using available data.
V. Measure Reporting Schedule
Each measurement year will encompass twelve months, from July 1 of the year prior to June 30 of the reporting year. The reason for using a mid-year time period is to allow for a claim lag of six months so data will be as complete as possible when the PPS performance is calculated for the measurement year. Results for the measurement year will be finalized in January of the following year to allow for six-month run out of billing data. The DSRIP time frame for providing results to the Independent Assessor to make determinations of the MY award is in March of the year after the MY. Measures which require information from medical records or other data sources will be collected from the PPS. NYS DOH will provide the PPS with information about the eligible members, the required data elements and formats, and the file submission process (see Section IX, XI and Appendix B). Measures are required to be reported each year and will not be allowed to be rotated. The PPS will gather and report this information by December of the reporting year.
The following provides the timeline for activities in the measurement year (Table 1). This is illustrated in Figure 3.
Table 1 - Annual Measurement Cycle
Activity Time Frame Measurement Year 4 Begins July 1, 2017 Measurement Year 4 Ends June 30, 2018 Measurement Year 5 Begins July 1, 2018 NYS DOH sends samples for measures requiring medical record (MR) data for MY5 July 2018 NYS DOH and vendor pull sample frame and administer C&G CAHPS August - December 2018 MR abstraction conducted, validated and Member Detail File created August - February 2019 Completed Member Detail File sent to NYS DOH February 2019 NYS DOH calculates final results for MY3, including PPS´ Member Detail File information, C&G CAHPS, other non-claims-based data March 2019 PPS MY4 results and MY5 annual improvement targets released to PPS April 2019 Measurement Year 5 Ends June 30, 2019
Figure 3 - Annual Measurement Year Cycle Timeline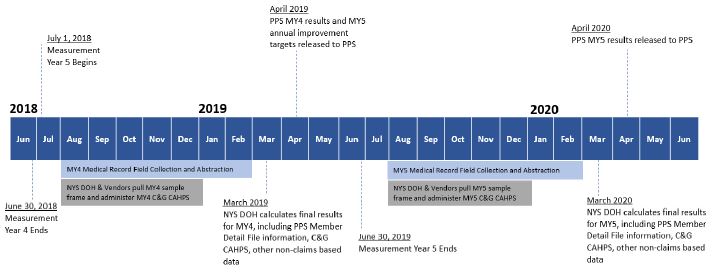
VI. Reporting Submission Process
Measures or reports indicated as ´PPS´ for reporting responsibility will be provided by the PPS. For several of the measures in Domain 3, the reporting responsibility is shared between the PPS and NYS DOH. The PPS reporting will be done through a member detail file. The information from the PPS member detail file will be incorporated into the final result calculation by NYS DOH. Table 2 lists the PPS reporting requirements for each Domain. Several requirements are specific to projects.
Table 2 - Performing Provider Systems Reporting Responsibilities
| Domain 1 | Domain 1 Measures will be reported through the MAPP system DSRIP Implementation Plan tool. PPS will report on progress towards, and completion of organizational milestones as well as project requirements. PPS will also report progress towards and achievement of project speed and scale commitments set forth in the application. |
| Domain 2 |
Patient Activation (Project 2.d.i)
|
| Domain 3 | PPS and NYS DOH shared - NYS DOH prepares sample and calculates final results; PPS provides Member Detail File for the following measures:
|
| Domain 4 | Domain 4 Measures are based on the NYS Prevention Agenda and will be calculated in accordance with NYS Prevention Agenda data source methodology located here. The measures will be calculated in alignment with PPS service areas where geographically limited data is available. Measures will be reported against NYS Prevention Agenda benchmarks, but achievement is based on reporting of applicable measures. |
VII. Resources for Technical Assistance
Several resources are available for collecting data for measures required to be calculated by the PPS. All of the resources can be requested by sending an email to dsrip@health.ny.gov:
- Measure specifications are available from the Measure Stewards for each measure. A number of measures are from the National Committee for Quality Assurance´s HEDIS® Technical Specifications (Volume 2) which is available for purchase. Some of the measure descriptions with some details are available on the National Quality Forum website (http://www.qualityforum.org/).
- The Independent Assessor Performance Facilitators can provide technical assistance in collection and use of performance data.
- The NYS DOH´s Office of Quality and Patient Safety (OQPS) staff can provide technical assistance for specifications or file layout.
- Technical specifications for all NYS-specific measures such as Screening for Clinical Depression and Follow up and Viral Load Suppression have been developed by OQPS (Appendix G).
- IPRO is available to help with any specification clarifications for medical record reviews.
VIII. Measure Descriptions, Specifications and Performance Goals
- Table 3. Domain 1 Measures
- Table 4. Additional Domain 1 Health Home Measures
- Table 5. Domain 2 Measures
- Table 6. Domain 3 Measures
- Table 7. Domain 4 Measures
Measure descriptions and information for Domain 1 measures are included in Table 3 and Table 4. Tables 5 and 6 contain information for the measures associated with Domains 2 and 3 respectively, including the projects associated with each measure. Table 7 contains the Prevention Agenda indicators associated with the Domain 4 Population-wide Strategy Implementation. Reporting responsibility is indicated for each measure. Measures identified as PPS´ responsibility will be obtained from information provided by the PPS. For several Domain 3 measures, responsibility is shared between NYS DOH and the PPS. The PPS will provide medical record review information in the member detail file which NYS DOH will incorporate into the final result calculation. Measures indicated as NYS DOH´s reporting responsibility will be calculated by NYS DOH and results will be provided to the PPS.
NYS DOH Measure Calculation Process
NYS DOH uses Medicaid claims and encounters as the basis for calculation of claims-based measures and identification of the eligible population for measures requiring medical record data. Programs used to calculate measure results have been developed using the measure steward specifications. Validation procedures for these programs included: review by external staff experienced in Healthcare Effectiveness Data and Information Set (HEDIS®) source code review, replication of Medicaid managed care submitted data produced from certified HEDIS® software results, and comparison of all Medicaid results from previous years. Medicaid transaction data for the measurement year (July 1 of previous year to June 30 of current year) will be considered finalized with the inclusion of the current year December billing information in the transaction systems, allowing a six-month run out of claims data.
Measure Retirement and Specification Modifications
The measures associated with the Domain 2 and 3 projects will be collected for all five years of the demonstration and specifications will be held consistent to the extent possible. Many of the measures used in DSRIP are currently used in CMS Medicaid quality core sets, as well as health plan reporting for Quality Assurance Reporting Requirements (QARR is NYS´ version of HEDIS®), and the measure steward is often a national organization. Situations may arise when the measure stewards retire or alter measure specifications to reflect changes in clinical care guidelines, treatment recommendations, or current health care practices. To align collection of data from all health care providers, the measure modifications may also be incorporated in DSRIP.
Measure Retirements
| Measure | Project | MY Retired | Replacement |
|---|---|---|---|
| Frequency of Ongoing Prenatal Care | 3.f.i | MY4 | None |
| Aspirin Use | 3.b.i - 3.b.ii | MY4 | None |
| Discussion of Risks and Benefits of Aspirin Use | 3.b.i - 3.b.ii | MY4 | None |
| PQI 13 - Angina without Procedure Admission Rate | 3.b.i - 3.b.ii | MY2 | PQI 8 - Heart Failure Admission Rate |
Objective
The objective is to maintain the achievement value awards for measures associated with projects throughout the DSRIP demonstration years. Measure definitions and specifications will be maintained consistently throughout the measurement years (2014-2019) to the greatest extent possible.
Guiding Principles
Should the measure steward retire or modify the specifications, we may accept and incorporate retirement or modifications to keep DSRIP measures relevant and meaningful to providers working to improve the quality of care. To that end, the guiding principles for the incorporation in DSRIP measures are as follows:
- Clinically relevant and meaningful quality measures reflecting recommended care and current health care practices; and
- Alignment and consistent use of measure specifications for DSRIP and core sets used by other programs in NYS, such as QARR, health homes or provider programs (e.g. incentives or Patient Centered Medical Home initiatives).
Determining Use in DSRIP
These two guiding principles are the key criteria for determining whether the retirement or modification will be incorporated into DSRIP. If clinical relevance is the reason for the recommended action by the measure steward, the modification will be incorporated into DSRIP. Clinically relevant, meaningful information will better engage providers in improvement activities by providing credible data for use in those activities.
Improvement of care is facilitated by coordinated efforts among units of health care delivery (practices, health plans). Measure alignment between PPS and other units facilitates coordination and comparability of results at various levels of health care delivery.
Process for Adjusting Performance Goals, Annual Improvement Targets and Achievement Values
Using the two guiding principles, decisions will be made regarding retirement or implementation of modifications. CMS will be notified of all decisions, including impact to performance goals, annual improvement targets and achievement values prior to the measurement year that the change is introduced.
When the decision is made to retire a measure or to implement a modification with a measure, the method of implementing the change and its impact to the performance goal (PG) and annual improvement target (AIT) will be dependent on four factors:
- Necessity of implementation (clinical relevance and alignment concern)
- Availability of replacement measure for retired measure
- Ability to implement change in a stratified fashion
- Ability to compare results with modification to previous results or to re-calculate previous results with modification
Necessity - If the genesis for the retirement or modification is not due to clinical relevance and the measure is not used in other programs, the retirement or modification will not be implemented for DSRIP.
Availability of replacement measure for retired measure - If there is a standardized measure with similar focus available for replacement for the retired measure, the new measure will be introduced at the beginning of the next measurement year. The new measure will be associated with the same achievement value as the retired measure. See Adjusting Performance Goals, Annual Improvement Targets and Achievement Values below for details on how data sources affect the continuity of the total achievement values.
Stratified implementation - If the modification can be applied in a stratified manner, meaning that the portion of the result used in DSRIP remains unchanged, this portion will be used for the improvement evaluation for the PPS in determining the achievement value award.
Comparability to Previous results - Retirement of a measure would not allow comparability to previous results. A measure result with the modification will be considered to not affect comparability if the change in the result with the modification is less than 10 percent change from the previous results without the modification, or no significant impact. Significant impact is determined if revised specifications alter the previous year´s overall results by more than a 10 percent change. The method to determine percent change is to:
- divide the previous result (pervious measurement year data with original specifications) by the new result (previous measurement year data if available or current measurement year data with revised specifications) and multiply the quotient by 100;
- then subtract 100 from the result for the percent change.
Percent Change = [(Previous Result/New Result) × 100] − 100
Adjusting Performance Goals, Annual Improvement Targets and Achievement Values - If the previous year´s result, compared to results with the changes implemented, is determined to have less than a 10 percent change, the performance goals, annual improvement targets and achievement values will not be affected in any manner.
If there is more than a 10 percent change or significant impact to the previous year´s result compared to results with the changed implemented, the performance goals and annual improvement targets will be re- established. If the data is available to re-calculate the previous year´s results with the modification, such as with claims-based measures, the revised result can be created using previous year´s claims. This would allow no interruption of achievement value awards. Non-claims-based measures would need to have data collection before the baseline data would be available. The first year´s results with the revised measure will be considered the baseline and will be used to set the performance goal and the annual improvement target for the next measurement year. In the interim year, when the baseline data is being collected, the achievement value will be retained in the project as pay-for-reporting (P4R) award.
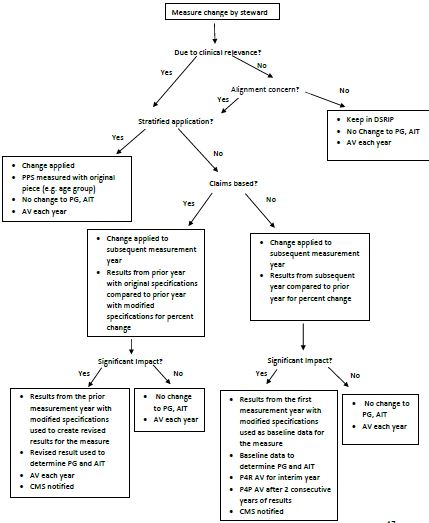
The decision process and any subsequent need for revising performance goals, annual improvement targets, and achievement values are described in two decision trees (Measure Retirement- Figure 4 and Measure Specification Modifications - Figure 5).
Annual achievement value (AV) awards are affected under two scenarios as shown in the two decision trees: in the case of measure retirement with no replacement and in the case of significant modification to non- claims-based measures. (Details regarding impact of available achievement values on annual payments are contained in the Achievement Value Guide).
Figure 4. Measure Retirement Decision Tree
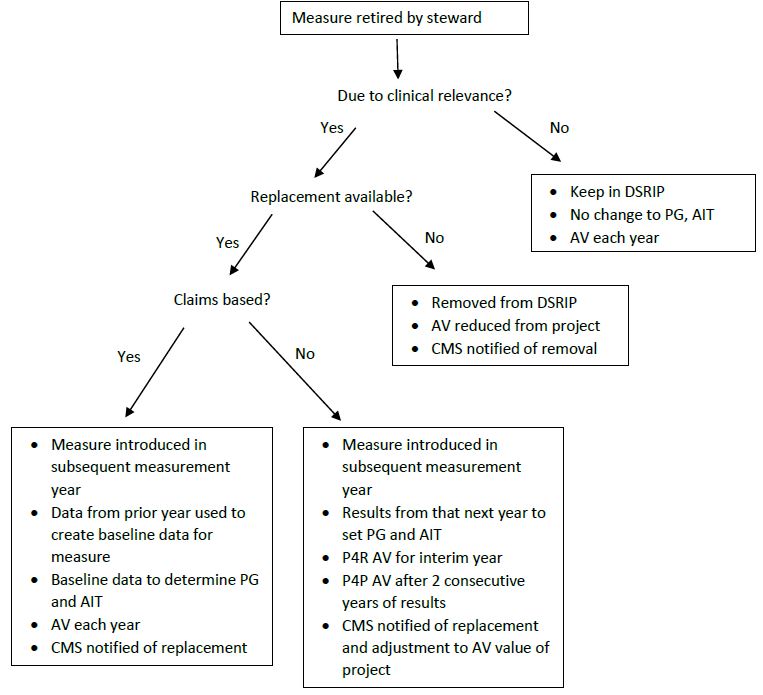
PG = Performance Goal
AIT = Annual Improvement Target
AV = Achievement Value
Figure 5. Measure Specification Modification Decision Tree
Common Scenarios
To demonstrate the process, several examples are provided. The examples described in this section are not intended to be inclusive of every situation which may arise, but address scenarios most likely to occur. If a new scenario arises during DSRIP, CMS and the NYS DOH will collaborate on the appropriate process to address the new scenario.
Scenario 1 - Measure specifications altered for reasons other than clinical relevance AND no alignment concern because measure is not in use in other levels of health care delivery in New York, such as health plan (QARR), meaningful use and health homes.
For example, a newer version of C&G CAHPS questionnaire is released with a modification in the response option schema for some questions. This could be done to echo new response options for other items in the survey version. The measure steward determines the modification is not based on validity of results and is not related to changes in clinical care recommendations.
Process decision: the original response option schema will be maintained to allow for consistent measurement. Maintaining measures specific to DSRIP will not introduce any confusion over the use of different measure versions within other levels of health care delivery.
Scenario 2 - Measure specifications altered for clinical relevance AND can be applied to DSRIP in a stratified fashion to allow consistent trending.
For example, if the upper age limit for a DSRIP measure was changed from 64 to 75 years, the specification modification could be applied in a manner that the original measure specifications would be maintained for consistency in trending. The PPS results for the measure could be stratified by age allowing consistent trending for the age group through age 64. The change in the age limit does not indicate an issue with relevance to the population through age 64.
Process decision: the measure specifications will be applied in a manner that allows for stratification of results so that the original specifications will be maintained to allow for consistent trending for evaluation of improvement. Stratified results would be provided; for example, results for the 65 to 75-year age group separately from the results for the other age group.
Scenario 3 - Measure specifications altered for clinical relevance AND cannot be applied to DSRIP in a fashion to allow consistent trending. Common examples are modifications to coding, medications, other technical adjustments, or criteria related to recommended clinical care or treatment guidelines.
For example, measure specifications are modified to update new Current Procedural Terminology (CPT) and Healthcare Common Procedure Coding System (HCPCS) codes which reflect recently added services relevant to the measure and allow more complete collection of the information.
Process decision: the modifications will be incorporated into the finalized version of the measure specification manual for the measurement year to allow for continued meaningful results of recommended quality care.
Scenario 4 - Measures which are retired by the measure steward because of changes in recommended quality care.
For example, the Cholesterol Management for Patients with Cardiovascular Conditions has been retired by NCQA due to recommendation changes regarding the LDL-c control level.
Process decision: the retirement will be incorporated.
Glossary for Measure Components
The terminology below is included in components for measures described in the tables below or in performance measurement procedures.
Achievement Value: The achievement value associated with the measure which the PPS will earn if associated criteria are met.
Annual Improvement Target (AIT): The result the PPS needs to meet or exceed to attain the achievement value for the measure for the measurement year. The annual improvement target is established using the PPS´ result from the previous measurement year. For example, the result for Measurement Year (MY) 1 is used to set the annual improvement target for MY 2 (see Section II).
Demonstration Year (DY): DYs are twelve-month calendar year periods beginning on April 1st and ending on March 31st for all 5 of the demonstration years. For example, DY1 begins on April 1, 2015 and ends March 31, 2016. The DY is different from the measurement year (see below).
Denominator: The members of the eligible population who meet the measure´s additional criteria (e.g. all adult patients with diabetes) and are included in the result calculation. Note: many measures include specific denominator inclusion and exclusion criteria.
High Performance Eligible: The indicator is displayed for measures which are eligible for high-performance funds.
Measure Eligible Population: Measures are developed to capture the population which is recommended for a particular service, called the eligible population. To define the eligible population, measures often have criteria such as age or diagnosis of a health condition to be included in the eligible population. While some measures may apply to everyone in the PPS (population-based), others may capture a smaller group within the PPS membership (episode-based). Population-based measures apply to the entire attributed PPS population over the measurement year. Episode-based measures are limited to only those members seen for that episode of care during the measurement year. Episode of care refers to all care provided over a measurement year for a specific condition (e.g. Diabetes - all diabetes care received in a defined time period for those members; HIV- all HIV care received in a defined time period for those members). Institutional-based measures apply to all people within the institution, such as nursing home measures.
Measure Reporting Responsibility: The collection process for each measure will be identified as calculated by the NYS DOH, or will be the responsibility of the PPS to collect or report. Measures that incorporate medical record data collected by the PPS with claims and encounters are shared responsibility of the PPS and NYS DOH. This will be detailed in Section IX in medical record guidelines.
Measure Name: The measure name or description is a brief statement of the measure. This will be used in the specifications, reporting templates and PPS reports containing results of the measures.
NQF Number: If the measure has a measure number from the National Quality Forum, whether currently endorsed or not, the number is included to facilitate access to more detailed specifications. Measures without an NQF number are listed as NA or Not Applicable.
Measure Status for DSRIP Payment: Pay for Performance (P4P) or Pay for Reporting (P4R). This designation specifies how the measure will be used for the purpose of DSRIP payment. Some measures are P4R throughout the entire demonstration period, while some measures also introduce a P4P achievement value in latter demonstration years (see tables 4 through 7).
Measure Achievement Value (AV): Several measures have more than one component. For such measures, the achievement value for the measure is proportioned among the components for a total AV of ‘1´ for the measure. This allows each measure to weigh equally in the overall achievement for a project.
Measurement Year (MY): A twelve-month period from July 1 of the previous year to June 30 of the current year.
Numerator: Description of criteria to determine compliance for the particular measure (e.g. all patients with an HbA1c test). Note: many measures include specific numerator inclusion and exclusion criteria.
Payment: The payment methodology for DYs is displayed.
Performance Goals (PG): Many of the measures in domain 2 and 3 will have performance goals established to represent the best performance expected in NYS. The goals are used in calculating the gap to goal for the annual improvement targets and high-performance targets, if applicable. This methodology used for establishing performance goals is described in Section II.
Specification Version: The version of the specifications used for the measure results is indicated, where applicable. When there are changes to the measure specifications, there can be differences with the NQF version. The indicated version of the measure steward´s specifications will be used.
Statewide Measure: The indicator is displayed for measures which are used to determine State performance for DSRIP. These measures are used to calculate state achievement of annual performance milestones in DY 3-5. The performance on these milestones can determine the amount of funding available to the program
Steward: Specifies the organization that maintains or administers the measure (e.g. National Committee for Quality Assurance (NCQA), Agency for Healthcare Research and Quality (AHRQ)). The measure steward should be referred to for detailed specifications. This manual provides high-level requirements for collection of the measures.
Calculation of Domain 1 Process Measures
Domain 1 measures are process measures and are based largely on milestone reporting and completion of milestones and project requirements, as well as measures specific to Health Homes in accordance with Attachment J. Domain 1 measures are broken into two categories: organizational measures and project measures. Domain 1 achievement values are assigned for each project for both organizational and project components.
Organizational measures include the following sections: Governance, Workforce Strategy, Financial Sustainability, and Cultural Competency and Health Literacy.
Project requirements are based on Domain 1 DSRIP Project Requirements Milestones & Metrics and are described in more detail in Appendix A.
Calculation of Achievement Values for Domain 1 metrics is described in Tables 3 and 4 below.
Calculation of Domain 4 Population Health Measures
Projects in Domain 4: Population-wide Strategy Implementation are aligned to the NYS Prevention Agenda and align with projects in Domain 3. Performing Provider Systems selected one or two projects from at least one of the four priority areas:
- Promote Mental Health and Prevent Substance Abuse;
- Prevent Chronic Disease;
- Prevent HIV/AIDS; and
- Promote Healthy Women, Infants and Children
The Prevention Agenda has established performance goals for each priority area and defined indicators to measure progress toward achieving these goals, including reductions in health disparities among racial, ethnic, and socioeconomic groups and persons with disabilities. These performance goals will be utilized to report on performance of PPS Domain 4 projects (payment is based on reporting only). The PPS are responsible for reporting on progress in implementing their selected strategies.
The New York State Prevention Agenda Dashboard allows for a visual presentation of the Prevention Agenda tracking indicator data at state and county levels. It will serve as a key source for monitoring progress made around the state with regard to meeting the Prevention Agenda 2018 objectives. The state dashboard homepage displays a quick view of the most current data for New York State and the Prevention Agenda 2018 objectives, many of which are Domain 4 Pay for Reporting measures. The most current data are compared to data from previous time periods to assess the annual progress for each indicator. Specific data source methodology can be located here. Results of indicators are not specific to Medicaid and are not from the same time frame as the DSRIP measurement year. The most currently available data for some indicators may represent past years.
For each Prevention Agenda priority area and focus area, measurable targets have been identified with outcome goals. Achievement values for Domain 4 measures are based on Pay for Reporting only, but progress towards these Prevention Agenda benchmarks will be calculated and monitored for reporting purposes. When possible, Domain 4 measures will be calculated according to PPS service areas, depending on the availability of county-specific data.
Data Sources for Domain 4 Projects
Domain 4 measures rely on data sources such as those listed below. Each project measure will be tracked and published electronically in yearly reports for the State and counties (where county data is available) as a Prevention Agenda (PA) Tracking Indicator.
- Asthma Surveillance Data
- Baseline Data - State and County Tracking Indicators for the Priority Areas
- Cancer Registry
- Community Health Indicator Reports
- County Health Indicators by Race/Ethnicity (CHIRE)
- County/ZIP Code Perinatal Data Profile
- Expanded (County Level) Behavioral Risk Factor Surveillance System
- Health Data NY GOV
- Hospital-Acquired Infection Reporting System
- Leading Causes of Death in New York State
- Medicaid Redesign Team Health Disparities Work Group Data and Information
- New York State Prevention Agenda Tracking Indicator Dashboard
- Prevention Quality Indicators (PQI)
- Report on Managed Care Plans Performance in New York State
- Sexually Transmitted Diseases Data and Statistics
- The New York State Pregnancy Risk Assessment Monitoring System (PRAMS)
- Vital Statistics (births, pregnancies, deaths)
Other External Data Sources
- America´s Health Rankings
- Behavioral Risk Factor Surveillance System - National and State Prevalence Data
- Children in the States Factsheets (Children´s Defense Fund)
- Chronic Disease Indicators - CDC
- County Health Rankings-Mobilizing Action Toward Community Health
- County Mental Health Profiles
- EpiQuery: NYC Interactive Health Data
- Governor´s Traffic Safety Committee
- Health Indicator Sortable Stats
- Health, United States, 2012 - In Brief
- Healthy People 2010
- Healthy People 2020
- Kids Well-being Indicator Clearinghouse (KWIC)
- National Center for Health Statistics
- New York State Data Center
- NYS School Report Cards, NYS DOE
- Pregnancy Risk Assessment Monitoring System (PRAMS) - CDC Ponder
- Prevention Risk Indicator Services Monitoring System (OASAS)
- U.S. Bureau of Labor Statistics
- U.S. Census Bureau
- Youth Risk Behavior Survey (YRBS)
Table 3. Domain 1 Measures
| Domain 1 Section | Metrics / Measurement Definition | AV Calculation Methodology | |
|---|---|---|---|
| Organizational Measures | |||
| Organizational - Governance | Finalize governance structure and sub-committee structure | One achievement value point for each project will be given for Governance based on demonstrated progress towards completion of milestones, completion of milestones by target dates specified by DOH or PPS, and ongoing reporting. * | |
| Establish a clinical governance structure, including clinical quality committees for each DSRIP project | |||
| Finalize bylaws and policies or Committee Guidelines where applicable | |||
| Establish governance structure reporting and monitoring processes | |||
| Organizational - Workforce Strategy | Workforce Strategy Budget Updates | One achievement value point for each project will be given for Workforce Strategy based on quarterly reporting, adherence to adjusted workforce spending commitments in each payment period, and sufficient explanation of any deviation from implementation plan projections. Workforce spending commitments have been adjusted according to the following: DY1: 80% of DY1 commitment DY2: 80% of total DY1 and DY2 commitment DY3: 85% of total DY1, DY2 and DY3 commitment DY4: 90% of total commitment DY5: 100% of total commitment Note that these are subject to change in future DSRIP periods. | |
| Workforce Staff Impact Analysis and Updates | |||
| New Hire Employment Analysis and Updates | |||
| Organizational - Financial Sustainability | Finalize PPS finance structure, including reporting structure | One achievement value point for each project will be given for Financial Sustainability based on demonstrated progress towards completion of milestones, completion of milestones by target dates specified by DOH or PPS, and ongoing reporting. * | |
| Perform network financial health current state assessment and develop financial sustainability strategy to address key issues | |||
| Finalize Compliance Plan consistent with New York State Social Services Law 363-d Administer a Value Based Payments (VBP) Needs Assessment (VNA) to the PPS network partners to identify opportunities to support the transition to VBP. | |||
| Develop a VBP support implementation plan to address the needs of the PPS network partners as identified in the VNA. | |||
| Develop partner engagement schedule for VBP education and trainings. | |||
| Cultural Competency and Health Literacy | Finalize cultural competency / health literacy strategy | One achievement value point for each project will be given for Cultural Competency / Health Literacy based on demonstrated progress towards completion of milestones, including completion of milestones by target dates specified by DOH or PPS, and ongoing reporting. * | |
| Develop a training strategy focused on addressing the drivers of health disparities (beyond the availability of language- appropriate material) | |||
| Project Measures | |||
| Quarterly Progress Reports | See Appendix A and Domain 1 DSRIP Project Requirements Milestones & Metrics guide. | One achievement value point for each project will be given for demonstrated progress towards completion or achievement of project metrics, for reporting of providers completing project requirements where applicable, and for additional required project reporting such as project budget, flow of funds, and health home P4R measures. | |
| Project Implementation Speed | Measure for evaluating performance against application commitments to speed of implementation of all project requirements. | One achievement value point following completion of project requirements by commitment date (see Appendix A for more details on completion of project requirements and applicable timeframes). | |
| Project System Change Implementation (DY2) | Measure for evaluating completion of major project system transformation requirements (See Appendix A). | One achievement value point for completion of project requirements classified as "Project System Changes". See Appendix A for more details. | |
| Patient Engagement Speed | Measure for evaluating performance against discounted application commitments to member engagement. | One achievement value point for engaging at least 80% of discounted active engagement commitments in DSRIP application for each payment period. Definitions of active engagement have been published under a separate protocol document to the DSRIP Website. | |
*Progress will be demonstrated through quarterly reporting. Independent Assessor will make final determination regarding whether or not PPS has achieved organizational milestones or demonstrated satisfactory progress towards completion.
Table 4. Additional Domain 1 Health Home Measures
| Measure Name | Numerator Description | Denominator Description | Performance Goal | Achievement Value | Reporting Responsibility | Payment: DY 1 through 5 |
|---|---|---|---|---|---|---|
| Health Home assigned/referred members in outreach or enrollment | Number of referred and assigned HH eligible members with at least one outreach or enrollment segment during the measurement year | Total number of referred and assigned HH eligible members in the Health Home Tracking System during the measurement year | NA - Pay for Reporting measure only | Reporting on this measure is required in order to earn project Quarterly Progress Report AV | NYS DOH | P4R |
| Health Home members who were in outreach/ enrollment who were enrolled during the measurement year | Number of HH members with at least one enrollment segment in the Health Home Tracking System during the measurement year | Total number HH eligible members with at least one outreach or enrollment segment of in the Health Home Tracking System during the measurement year | NA - Pay for Reporting measure only | Reporting on this measure is required in order to earn project Quarterly Progress Report AV | NYS DOH | P4R |
| Health Home enrolled members with a care plan during the measurement year | Number HH with a care plan update indicated in any of the four quarters of the measurement year | Total number HH eligible members with at least one segment of enrollment in the Health Home Tracking System during the measurement year | NA - Pay for Reporting measure only | Reporting on this measure is required in order to earn project Quarterly Progress Report AV | NYS DOH | P4R |
± A lower rate is desirable.
* High Performance Eligible measure.
# Statewide measure.
Table 5. Domain 2 Measures
| Measure Name | Steward and Specification Version | NQF # | Projects Associated with Measure | Numerator Description | Denominator Description | Performance Goal *High Performance eligible #Statewide measure | Achievement Value | Reporting Responsibility | Payment: DY 2 | Payment: DY 3 | Payment: DY 4 and 5 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Domain 2 - System Transformation | |||||||||||
| Potentially Preventable Emergency Room Visits ± | 3M | NA | 2.a.i - 2.a.v, 2.b.i - 2.b.ix, 2.c.i - 2.c.ii |
Number of preventable emergency visits as defined by revenue and CPT codes | Number of people (excludes those born during the measurement year) as of June 30 of measurement year | 6.50 per 100 Medicaid enrollees *High Perf Elig # SW measure | 1 if annual improvement target or performance goal met or exceeded | NYS DOH | P4R | P4P | P4P |
| Potentially Preventable Readmissions ± | 3M | NA | 2.a.i - 2.a.v, 2.b.i - 2.b.ix, 2.c.i - 2.c.ii |
Number of readmission chains (at risk admissions followed by one or more clinically related readmissions within 30 days of discharge) | Number of people as of June 30 of the measurement year | 180.66 per 100,000 Medicaid Enrollees *High Perf Elig # SW measure | 1 if annual improvement target or performance goal met or exceeded | NYS DOH | P4R | P4P | P4P |
| Prevention Quality Indicator # 90 (PQI 90 - Composite of all measures) +/- | AHRQ 7.0 | NA | 2.a.i - 2.a.v, 2.b.i - 2.b.ix, 2.c.i - 2.c.ii |
Number of discharges which were in the numerator of one of the adult prevention quality indicators | Number of people 18 years and older who were enrolled in Medicaid for at least one month as of June 30 of measurement year | 138.65 per 100,000 Medicaid Enrollees | 1 if annual improvement target or performance goal met or exceeded | NYS DOH | P4R | P4R | P4P |
| Pediatric Quality Indicator # 90 (Overall Composite) +/- | AHRQ 7.0 | NA | 2.a.i - 2.a.v, 2.b.i - 2.b.ix, 2.c.i - 2.c.ii |
Number of discharges which were in the numerator of one of the pediatric prevention quality indicators | Number of people 6 to 17 years who were enrolled in Medicaid for at least one month as of June 30 of measurement year | 30.24 per 100,000 Medicaid Enrollees # SW measure | 1 if annual improvement target or performance goal met or exceeded | NYS DOH | P4R | P4R | P4P |
| Percent of total Medicaid provider reimbursement received through sub- capitation or other forms of non-FFS reimbursement | NYS-specific | NA | 2.a.i - 2.a.v, 2.b.i - 2.b.ix, 2.c.i - 2.c.ii |
Dollars paid by MCO under value based arrangements | Total Dollars paid by MCOs | NA - Pay for Reporting measure only | 1 | NYS DOH | P4R | P4R | P4R |
| Meaningful Use Certified Providers who have a participating agreement See Appendix G for additional measure specifications |
NYS-specific | NA | 2.a.i - 2.a.v, 2.b.i - 2.b.ix, 2.c.i - 2.c.ii |
Number of eligible providers meeting meaningful use criteria, who have at least one participating agreement with a qualified entity (QE) | Number of eligible providers meeting meaningful use criteria in the PPS network | NA - Pay for Reporting measure only # SW measure | 0.5 | NYS DOH | P4R | P4R | P4R |
| Meaningful Use Certified Providers who conduct bidirectional exchange See Appendix G for additional measure specifications |
NYS-specific | NA | 2.a.i - 2.a.v, 2.b.i - 2.b.ix, 2.c.i - 2.c.ii |
Number of eligible providers meeting meaningful use criteria, who both 1) make data available and 2) access data using SHIN-NY with a QE | Number of eligible providers meeting meaningful use criteria in the PPS network | NA - Pay for Reporting measure only # SW measure | 0.5 | NYS DOH | P4R | P4R | P4R |
| Percent of PCP providers meeting PCMH (NCQA) or Advanced Primary Care (SHIP) standards See Appendix G for additional measure specifications |
NA | NA | 2.a.i - 2.a.v, 2.b.i - 2.b.ix, 2.c.i - 2.c.ii |
Number of PCP providers meeting PCMH Standards (all levels and any standard year) or Advanced Primary Care Standards | Number of PCP providers in the PPS network | NA - Pay for Reporting measure only # SW measure | 1 | NYS DOH | P4R | P4R | P4R |
| Primary Care - Usual Source of Care | 1351a_C&G CAHPS Adult Primary Care (version 3.0, Q2) | NA | 2.a.i - 2.a.v, 2.b.i - 2.b.ix, 2.c.i - 2.c.ii |
Percent of Reponses ´Yes´ | All Responses | 92.5% # SW measure | 0.5 if annual improvement target or performance goal met or exceeded | NYS DOH | P4R | P4P | P4P |
| Primary Care - Length of Relationship | 1351a_C&G CAHPS Adult Primary Care (version 3.0, Q3) | NA | 2.a.i - 2.a.v, 2.b.i - 2.b.ix, 2.c.i - 2.c.ii |
Percent of Responses at least ´1 year´ or longer | All Responses | 85.0% # SW measure | 0.5 if annual improvement target or performance goal met or exceeded | NYS DOH | P4R | P4P | P4P |
| Adult Access to Preventive or Ambulatory Care - 20 to 44 years | HEDIS® 2019 | NA | 2.a.i - 2.a.v, 2.b.i - 2.b.ix, 2.c.i - 2.c.ii |
Number of adults who had an ambulatory or preventive care visit during the measurement year | Number of adults ages 20 to 44 as of June 30 of the measurement year | 91.1% # SW measure | 0.33 if annual improvement target or performance goal met or exceeded | NYS DOH | P4R | P4P | P4P |
| Adult Access to Preventive or Ambulatory Care - 45 to 64 years | HEDIS® 2019 | NA | 2.a.i - 2.a.v, 2.b.i - 2.b.ix, 2.c.i - 2.c.ii |
Number of adults who had an ambulatory or preventive care visit during the measurement year | Number of adults ages 45 to 64 as of June 30 of the measurement year | 94.4% # SW measure | 0.33 if annual improvement target or performance goal met or exceeded | NYS DOH | P4R | P4P | P4P |
| Adult Access to Preventive or Ambulatory Care - 65 and older | HEDIS® 2019 | NA | 2.a.i - 2.a.v, 2.b.i - 2.b.ix, 2.c.i - 2.c.ii |
Number of adults who had an ambulatory or preventive care visit during the measurement year | Number of adults ages 65 and older as of June 30 of the measurement year | 94.4% # SW measure | 0.33 if annual improvement target or performance goal met or exceeded | NYS DOH | P4R | P4P | P4P |
| Children´s Access to Primary Care - 12 to 24 months | HEDIS® 2019 | NA | 2.a.i - 2.a.v, 2.b.i - 2.b.ix, 2.c.i - 2.c.ii |
Number of children who had a visit with a primary care provider during the measurement year | Number of children ages 12 to 24 months as of June 30 of the measurement year | 100.0% # SW measure | 0.25 if annual improvement target or performance goal met or exceeded | NYS DOH | P4R | P4P | P4P |
| Children´s Access to Primary Care - 25 months to 6 years | HEDIS® 2019 | NA | 2.a.i - 2.a.v, 2.b.i - 2.b.ix, 2.c.i - 2.c.ii |
Number of children who had a visit with a primary care provider during the measurement year | Number of children ages 25 months to 6 years as of June 30 of the measurement year | 98.4% # SW measure | 0.25 if annual improvement target or performance goal met or exceeded | NYS DOH | P4R | P4P | P4P |
| Children´s Access to Primary Care - 7 to 11 years | HEDIS® 2019 | NA | 2.a.i - 2.a.v, 2.b.i - 2.b.ix, 2.c.i - 2.c.ii |
Number of children who had a visit with a primary care provider during the measurement year or year prior | Number of children ages 7 to 11 years as of June 30 of the measurement year | 100.0% # SW measure | 0.25 if annual improvement target or performance goal met or exceeded | NYS DOH | P4R | P4P | P4P |
| Children´s Access to Primary Care - 12 to 19 years | HEDIS® 2019 | NA | 2.a.i - 2.a.v, 2.b.i - 2.b.ix, 2.c.i - 2.c.ii |
Number of children who had a visit with a primary care provider during the measurement year or year prior | Number of children ages 12 to 19 years as of June 30 of the measurement year | 98.8% # SW measure | 0.25 if annual improvement target or performance goal met or exceeded | NYS DOH | P4R | P4P | P4P |
| Getting Timely Appointments, Care and information | 1351a_C&G CAHPS Adult Primary Care (version 3.0, Q6, 8 and 10) | NA | 2.a.i - 2.a.v, 2.b.i - 2.b.ix, 2.c.i - 2.c.ii |
Number responses ´Usually´ or ´Always´ got appt for urgent care or routine care as soon as needed, and got answers the same day if called during the day | Number who answered they called for appointments or called for information | 92.5% # SW measure | 1 if annual improvement target or performance goal met or exceeded | NYS DOH | P4R | P4P | P4P |
| Medicaid Spending on ER and Inpatient Services ± See Appendix G for additional measure specifications | NYS-specific | NA | 2.a.i - 2.a.v, 2.b.i - 2.b.ix, 2.c.i - 2.c.ii |
Total spending on ER and IP services | Per member per month of members attributed to the PPS as of June of the measurement year | NA - Pay for Reporting measure only | 1 | NYS DOH | P4R | P4R | P4R |
| Medicaid spending on Primary Care and community based behavioral health care See Appendix G for additional measure specifications | NYS-specific | NA | 2.a.i - 2.a.v, 2.b.i - 2.b.ix, 2.c.i - 2.c.ii |
Total spending on Primary Care and Community Behavioral Health care as defined by MMCOR categories | Per member per month of members attributed to the PPS as of June of the measurement year | NA - Pay for Reporting measure only | 1 | NYS DOH | P4R | P4R | P4R |
| H-CAHPS - Care Transition CMS Data Set H_COMP_7_SA and H_COMP_7_A | H-CAHPS V13.0 (Q23, 24, and 25) |
NA | 2.a.i - 2.a.v, 2.b.i - 2.b.ix, 2.c.i - 2.c.ii |
Average of hospital specific results for the Care Transition composite using Strongly Agree and Agree responses | Hospitals with H-CAHPS participating in the PPS network | 97.0% | 1 if annual improvement target or performance goal met or exceeded | NYS DOH | P4R | P4P | P4P |
| Care Coordination | 1351a_C&G CAHPS Adult Primary Care (version 3.0, Q13, 22 and 24) |
NA | 2.a.i - 2.a.v, 2.b.i - 2.b.ix, 2.c.i - 2.c.ii |
Number responses ´Usually´ or ´Always´ that provider seemed to know important history, follow- up to give results from tests, and talked about all prescription medicines | All responses | 91.9% # SW measure | 1 if annual improvement target or performance goal met or exceeded | NYS DOH | P4R | P4P | P4P |
| PAM Score | Insignia -NYS Modifications | NA | 2.d.i | N/A | N/A | Performance based on difference between mean score of current and previous measurement year by cohort | Between 0-1 based on interval scale of performance | PPS | P4R | P4P | P4P |
| Non-use of primary and preventive care services ± See Appendix G for additional measure specifications | NYS-specific | NA | 2.d.i | The percentage of Medicaid members who do not have at least one claim with a preventive services CPT or equivalent code in the measurement year | The percentage of Medicaid members who do not have at least one claim with a preventive services CPT or equivalent code in the baseline measurement year | Ratio lower than 1 | 1 if ratio lower than 1 | NYS DOH | P4R | P4P | P4P |
| ED use by uninsured ± | NYS-specific with SPARCS | NA | 2.d.i | The percentage of ED visits which are self-pay payer typology only for all hospitals in the PPS network in the measurement year | The percentage of ED visits for self-pay payer typology only for all hospitals in the PPS network in the baseline measurement year | Ratio lower than 1 | 1 if ratio lower than 1 | NYS DOH | P4R | P4P | P4P |
| C&G CAHPS by PPS for uninsured | 1351a_C&G CAHPS Adult Primary Care (version 3.0) | NA | 2.d.i | Using the C&G CAHPS Survey, three composite measures and one rating measure: 1) Getting timely appointments, care, and information 2) How well providers (or doctors) communicate with patients 3) Helpful, courteous, and respectful office staff 4) Patients´ rating of the provider (or doctor) |
At least 30 (or more) completed survey responses | Ratio higher than 1 | 0.25 for each (total of 1 AV) if ratio higher than 1 (based on 30 or more completed surveys) | PPS | P4R | P4P | P4P |
± A lower rate is desirable.
* High Performance Eligible measure.
# Statewide measure.
Table 6. Domain 3 Measures
| Measure Name | Steward and Specification Version | NQF # | Projects Associated with Measure | Numerator Description | Denominator Description | Performance Goal *High Performance eligible #Statewide measure | Achievement Value | Reporting Responsibility | Payment: DY 2 | Payment: DY 3 | Payment: DY 4 and 5 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Domain 3 - Clinical Improvement Projects | |||||||||||
| Potentially Preventable Emergency Room Visits (for persons with BH diagnosis) ± The list of ICD-10 codes for the BH definition used in member attribution is available upon request from the Account Support Team | 3M | NA | 3.a.i - 3.a.iv | Number of preventable emergency room visits as defined by revenue and CPT codes | Number of people with a BH diagnosis (BH definition used in member attribution; excludes those born during the measurement year) as of June 30 of measurement year | 39.57 per 100 Medicaid enrollees with Behavioral Health Qualifying Service *High Perf Elig | 1 if annual improvement target or performance goal met or exceeded | NYS DOH | P4P | P4P | |
| Antidepressant Medication Management - Effective Acute Phase Treatment | HEDIS® 2019 | 0105 | 3.a.i - 3.a.iv | Number of people who remained on antidepressant medication during the entire 12-week acute treatment phase | Number of people 18 and older who were diagnosed with depression and treated with an antidepressant medication | 60.0% *High Perf Elig | 0.5 if annual improvement target or performance goal met or exceeded | NYS DOH | P4P | P4P | |
| Antidepressant Medication Management - Effective Continuation Phase Treatment | HEDIS® 2019 | 0105 | 3.a.i - 3.a.iv | Number of people who remained on antidepressant medication for at least six months | Number of people 18 and older who were diagnosed with depression and treated with an antidepressant medication | 43.5% *High Perf Elig | 0.5 if annual improvement target or performance goal met or exceeded | NYS DOH | P4P | P4P | |
| Diabetes Monitoring for People with Diabetes and Schizophrenia | HEDIS® 2019 | 1934 | 3.a.i - 3.a.iv | Number of people who had both an LDL-C test and an HbA1c test during the measurement year | Number of people, ages 18 to 64 years, with schizophrenia and diabetes | 89.8% *High Perf Elig | 1 if annual improvement target or performance goal met or exceeded | NYS DOH | P4P | P4P | |
| Diabetes Screening for People with Schizophrenia or Bipolar Disease who are Using Antipsychotic Medication | HEDIS® 2019 | 1932 | 3.a.i - 3.a.iv | Number of people who had a diabetes screening test during the measurement year | Number of people, ages 18 to 64 years, with schizophrenia or bipolar disorder, who were dispensed an antipsychotic medication | 89.0% | 1 if annual improvement target or performance goal met or exceeded | NYS DOH | P4P | P4P | |
| Cardiovascular Monitoring for People with Cardiovascular Disease and Schizophrenia | HEDIS® 2019 | 1933 | 3.a.i - 3.a.iv | Number of people who had an LDL-C test during the measurement year | Number of people, ages 18 to 64 years, with schizophrenia and cardiovascular disease | 92.2% (health plan data) *High Perf Elig | 1 if annual improvement target or performance goal met or exceeded | NYS DOH | P4P | P4P | |
| Follow-up care for Children Prescribed ADHD Medications - Initiation Phase | HEDIS® 2019 | 0108 | 3.a.i - 3.a.iv | Number of children who had one follow-up visit with a practitioner within the 30 days after starting the medication | Number of children, ages 6 to 12 years, who were newly prescribed ADHD medication | 72.3% | 0.5 if annual improvement target or performance goal met or exceeded | NYS DOH | P4R | P4P | |
| Follow-up care for Children Prescribed ADHD Medications - Continuation Phase | HEDIS® 2019 | 0108 | 3.a.i - 3.a.iv | Number of children who, in addition to the visit in the Initiation Phase, had at least 2 follow-up visits in the 9-month period after the initiation phase ended | Number of children, ages 6 to 12 years, who were newly prescribed ADHD medication and remained on the medication for 7 months | 78.7% (health plan data) | 0.5 if annual improvement target or performance goal met or exceeded | NYS DOH | P4R | P4P | |
| Follow-up after hospitalization for Mental Illness - within 7 days | HEDIS® 2018 (DSRIP will not be using HEDIS® 2019 for MY5 for this measure) | 0576 | 3.a.i - 3.a.iv | A follow-up visit with a mental health practitioner within 7 days after discharge. Do not include visits that occur on the date of discharge. | Number of discharges between the start of the measurement year to 30 days before the end of the measurement year for patients ages 6 years and older, who were hospitalized for treatment of selected mental health disorders | 78.3%*High Perf Elig | 0.5 if annual improvement target or performance goal met or exceeded | NYS DOH | P4P | P4P | |
| Follow-up after hospitalization for Mental Illness - within 30 days | HEDIS® 2018 ( DSRIP will not be using HEDIS® 2019 for MY5 for this measure ) | 0576 | 3.a.i - 3.a.iv | A follow-up visit with a mental health practitioner within 30 days after discharge. Do not include visits that occur on the date of discharge. | Number of discharges between the start of the measurement year to 30 days before the end of the measurement year for patients ages 6 years and older, who were hospitalized for mental health disorders treatment of selected | 93.4%*High Perf Elig | 0.5 if annual improvement target or performance goal met or exceeded | NYS DOH | P4P | P4P | |
| Screening for Clinical Depression and follow-up See Appendix G for additional measure specifications | NYS-specific | NA | 3.a.i - 3.a.iv | Number of people screened for clinical depression using a standardized depression screening tool, and if positive, with follow-up within 30 days | Number of people with a qualifying outpatient visit who are age 18 and older | 56.2% | 1 if annual improvement target or performance goal met or exceeded | PPS and NYS DOH | P4R | P4P | |
| Adherence to Antipsychotic Medications for People with Schizophrenia | HEDIS® 2019 | 1879 | 3.a.i - 3.a.iv | Number of people who remained on an antipsychotic medication for at least 80% of their treatment period | Number of people, ages 19 to 64 years, with schizophrenia who were dispensed at least 2 antipsychotic medications during the measurement year | 76.5% | 1 if annual improvement target or performance goal met or exceeded | NYS DOH | P4P | P4P | |
| Initiation of Alcohol and Other Drug Dependence Treatment (1 visit within 14 days) | HEDIS® 2019 | 0004 | 3.a.i - 3.a.iv | Number of people who initiated treatment through an inpatient AOD admission, outpatient visit, intensive outpatient encounter, or partial hospitalization within 14 days of the index episode | Number of people age 13 and older with a new episode of alcohol or other drug (AOD) dependence | 57.1% | 0.5 if annual improvement target or performance goal met or exceeded | NYS DOH | P4P | P4P | |
| Engagement of Alcohol and Other Drug Dependence Treatment (Initiation and 2 visits within 48 days) | HEDIS® 2019 | 0004 | 3.a.i - 3.a.iv | Number of people who initiated treatment AND who had two or more additional services with a diagnosis of AOD within 34 days of the initiation visit | Number of people age 13 and older with a new episode of alcohol or other drug (AOD) dependence | 28.3% | 0.5 if annual improvement target or performance goal met or exceeded | NYS DOH | P4P | P4P | |
| Antipsychotic Use for Persons with Dementia ± | Pharmacy Quality Alliance MDS 3.0 | NA | 3.a.v | Number of long stay residents with dementia who are persistently receiving an antipsychotic medication without evidence of a psychotic disorder or related condition | Number of days for long stay residents (101+ days) with two consecutive assessments and who have an active diagnosis of Alzheimer or dementia OR cognitive impairment. Persons with evidence of psychotic disorder or related condition are excluded | 6.9% *High Perf Elig | 1 if annual improvement target or performance goal met or exceeded | NYS DOH | P4P | P4P | |
| Percent of Long Stay Residents who have Depressive Symptoms ± | MDS 3.0 Measure #0690 | NA | 3.a.v | Residents with an assessment with either 1) the resident expressing little interest or pleasure, or feeling down or depressed or hopeless in half or more of the days over the last 2 weeks and a resident interview total severity score indicates the presence of depression; OR 2) staff assess resident demonstrates little interest or pleasure, or feeling down or depressed or hopeless in half or more of the days over the last 2 weeks and a staff assessment interview total severity score indicates the presence of depression | Long stay residents (101+ days) with an assessment | 0.16% | 1 if annual improvement target or performance goal met or exceeded | NYS DOH | P4P | P4P | |
| Prevention Quality Indicator # 7 (Hypertension Admission Rate) +/- | AHRQ 7.0 | 0276 | 3.b.i - 3.b.ii | Number of discharges with a principal diagnosis code of hypertension | Number of people 18 years and older who were enrolled in Medicaid for at least one month as of June 30 of measurement year | 3.49 per 100,000 Medicaid Enrollees | 1 if annual improvement target or performance goal met or exceeded | NYS DOH | P4R | P4P | |
| Prevention Quality Indicator # 8 (Heart Failure Admission Rate) +/- | AHRQ 7.0 | 0277 | 3.b.i - 3.b.ii | Number of discharges with a principal diagnosis code of heart failure | Number of people 18 years and older who were enrolled in Medicaid for at least one month as of June 30 of measurement year | 6.76per 100,000 Medicaid Enrollees | 1 if annual improvement target or performance goal met or exceeded | NYS DOH | P4R | P4P | |
| Statin Therapy for Patients with Cardiovascular Disease -Received Statin Therapy | HEDIS® 2019 | 3.b.i - 3.b.ii | Number of people who were dispensed at least one high or moderate- intensity statin medication | Number of males age 21 to 75 or females age 40 to 75 who have had an MI, CABG or PCI in the year prior or a diagnosis of ischemic vascular disease in both the measurement year and year prior | 100% | 0.5 if annual improvement target or performance goal met or exceeded | NYS DOH | P4R | P4P | ||
| Statin Therapy for Patients with Cardiovascular Disease - Statin Adherence 80% | HEDIS® 2019 | 3.b.i - 3.b.ii | Number of people who achieved a proportion of days covered of 80% for the treatment period | Number of males age 21 to 75 or females age 40 to 75 who have had an MI, CABG or PCI in the year prior or a diagnosis of ischemic vascular disease in both the measurement year and year prior AND who were dispensed at least one high or moderate-intensity statin medication. | 78.3% | 0.5 if annual improvement target or performance goal met or exceeded | NYS DOH | P4R | P4P | ||
| Controlling High Blood Pressure | HEDIS® 2018 (DSRIP will not be using HEDIS® 2019 for MY5 for this measure) | 0018 | 3.b.i - 3.b.ii, 3.h.i | Number of people whose blood pressure was adequately controlled as follows:
|
Number of people, ages 18 to 85 years, who have hypertension | 73.3% (2012 Data) *High Perf Elig | 1 if annual improvement target or performance goal met or exceeded | PPS and NYS DOH | P4R | P4P | |
| Medical Assistance with Smoking and Tobacco Use Cessation - Advised to Quit | HEDIS® 2019 (Volume 3 using CAHPS data) | 0027 | 3.b.i - 3.b.ii, 3.c.i - 3.c.ii, 3.e.i, 3.h.i | Number of responses ´Sometimes´, ´Usually´ or ´Always´ were advised to quit | Number of respondents, ages 18 years and older, who smoke or use tobacco some days or every day | 95.6% | 0.33 if annual improvement target or performance goal met or exceeded | NYS DOH | P4R | P4P | |
| Medical Assistance with Smoking and Tobacco Use Cessation - Discussed Cessation Medication | HEDIS® 2019 (Volume 3 using CAHPS data) | 0027 | 3.b.i - 3.b.ii, 3.c.i - 3.c.ii, 3.e.i, 3.h.i | Number of responses ´Sometimes´, ´Usually´ or ´Always´ discussed cessation medications | Number of respondents, ages 18 years and older, who smoke or use tobacco some days or every day | 83.9% | 0.33 if annual improvement target or performance goal met or exceeded | NYS DOH | P4R | P4P | |
| Medical Assistance with Smoking and Tobacco Use Cessation - Discussed Cessation Strategies | HEDIS® 2019 (Volume 3 using CAHPS data) | 0027 | 3.b.i - 3.b.ii, 3.c.i - 3.c.ii, 3.e.i, 3.h.i | Number of responses ´Sometimes´, ´Usually´ or ´Always´ discussed cessation methods or strategies | Number of respondents, ages 18 years and older, who smoke or use tobacco some days or every day | 75.3% *High Perf Elig | 0.33 if annual improvement target or performance goal met or exceeded | NYS DOH | P4R | P4P | |
| Flu Shots for Adults Ages 18 - 64 | HEDIS® 2019 (Volume 3 using CAHPS data) | 0039 | 3.b.i - 3.b.ii, 3.c.i - 3.c.ii, 3.h.i | Number of respondents who have had a flu shot | Number of respondents, ages 18 to 64 years | 63.4% | 1 if annual improvement target or performance goal met or exceeded | NYS DOH | P4R | P4P | |
| Health Literacy - Instructions Easy to Understand | 2357a_ C&G CAHPS Adult Supplement (QHL13) | NA | 3.b.i - 3.b.ii, 3.c.i - 3.c.ii | Number of responses ´Usually´ or ´Always´ that instructions for caring for condition were easy to understand | Number of respondents who answered they saw provider for an illness or condition and were given instructions | 98.8% | 0.33 if annual improvement target or performance goal met or exceeded | NYS DOH | P4R | P4P | |
| Health Literacy - Describing How to Follow Instructions | 2357a_ C&G CAHPS Adult Supplement (QHL14) | NA | 3.b.i - 3.b.ii, 3.c.i - 3.c.ii | Number of responses ´Usually´ or ´Always´ that provider asked patient to describe how the instruction would be followed | Number of respondents who answered they saw provider for an illness or condition and were given instructions | 89.7% | 0.33 if annual improvement target or performance goal met or exceeded | NYS DOH | P4R | P4P | |
| Health Literacy - Explained What to do if Illness Got Worse | 2357a_ C&G CAHPS Adult Supplement (QHL16) | NA | 3.b.i - 3.b.ii, 3.c.i - 3.c.ii | Number of responses ´Usually´ or ´Always´ that provider explained what to do if illness/condition got worse or came back | Number of respondents who answered they saw provider for an illness or condition | 94.1% | 0.33 if annual improvement target or performance goal met or exceeded | NYS DOH | P4R | P4P | |
| Prevention Quality Indicator # 1 (Diabetes Short-Term Complications Admission Rate) +/- | AHRQ 7.0 | 0272 | 3.c.i - 3.c.ii | Number of discharges with a principal diagnosis code of diabetes with short-term complications (ketoacidosis, hyperosmolarity, or coma) | Number of people 18 years and older who were enrolled in Medicaid for at least one month as of June 30 of measurement year | 16.91 per 100,000 Medicaid Enrollees | 1 if annual improvement target or performance goal met or exceeded | NYS DOH | P4R | P4P | |
| Comprehensive Diabetes screening - All Three Tests (HbA1c, dilated eye exam, and medical attention for nephropathy) | HEDIS® 2019 | 0055, 0062, 0057 | 3.c.i - 3.c.ii, 3.h.i | Number of people who received at least one of each of the following tests: HbA1c test, diabetes eye exam, and medical attention for nephropathy | Number of people ages 18 to 75 with diabetes | 64.6% | 1 if annual improvement target or performance goal met or exceeded | PPS and NYS DOH | P4R | P4P | |
| Comprehensive Diabetes Care: Hemoglobin A1c (HbA1c) Poor Control (>9.0%) ± | HEDIS® 2019 | 0059 | 3.c.i - 3.c.ii, 3.h.i | Number of people whose most recent HbA1c level indicated poor control (>9.0 percent), was missing or did not have a HbA1c test | Number of people ages 18 to 75 with diabetes | 23.2% | 1 if annual improvement target or performance goal met or exceeded | PPS and NYS DOH | P4R | P4P | |
| Prevention Quality Indicator # 15 (Asthma in Younger Adults Admission Rate) +/- | AHRQ 7.0 | 0283 | 3.d.i - 3.d.iii | Number of discharges with a principal diagnosis code of asthma | Number of people ages 18 to 39 who were enrolled in Medicaid for at least one month as of June 30 of the measurement year | 6.55per 100,000 Medicaid Enrollees | 1 if annual improvement target or performance goal met or exceeded | NYS DOH | P4R | P4P | |
| Pediatric Quality Indicator # 14 (Asthma Admission Rate) +/- | AHRQ 7.0 | 0728 | 3.d.i - 3.d.iii | Number of discharges with a principal diagnosis code of asthma | Number of people ages 2 to 17 who were enrolled in Medicaid for at least one month as of June 30 of the measurement year | 19.79per 100,000 Medicaid Enrollees | 1 if annual improvement target or performance goal met or exceeded | NYS DOH | P4R | P4P | |
| Asthma Medication Ratio (5 - 64 Years) | HEDIS® 2019 | 1800 | 3.d.i - 3.d.iii | Number of people with a ratio of controller medications to total asthma medications of 0.50 or greater during the measurement year | Number of people, ages 5 to 64 years, who were identified as having persistent asthma | 76.0% | 1 if annual improvement target or performance goal met or exceeded | NYS DOH | P4P | P4P | |
| Medication Management for People with Asthma (5 - 64 Years) - 50% of Treatment Days Covered | HEDIS® 2019 | 1799 | 3.d.i - 3.d.iii | Number of people who filled prescriptions for asthma controller medications during at least 50% of their treatment period | Number of people, ages 5 to 64 years, who were identified as having persistent asthma, and who received at least one controller medication | 68.6% | 0.5 if annual improvement target or performance goal met or exceeded | NYS DOH | P4P | P4P | |
| Medication Management for People with Asthma (5 - 64 Years) - 75% of Treatment Days Covered | HEDIS® 2019 | 1799 | 3.d.i - 3.d.iii | Number of people who filled prescriptions for asthma controller medications during at least 75% of their treatment period | Number of people, ages 5 to 64 years, who were identified as having persistent asthma, and who received at least one controller medication | 44.9% | 0.5 if annual improvement target or performance goal met or exceeded | NYS DOH | P4P | P4P | |
| HIV/AIDS Comprehensive Care: Engaged in Care See Appendix G for additional measure specifications | NYS-specific | NA | 3.e.i | Number of people who had two visits for primary care or HIV related care with at least one visit during each half of the past year | Number of people living with HIV/AIDS, ages 2 years and older | 91.8% | 1 if annual improvement target or performance goal met or exceeded | NYS DOH | P4P | P4P | |
| HIV/AIDS Comprehensive Care: Viral Load Monitoring See Appendix G for additional measure specifications | NYS-specific | NA | 3.e.i | Number of people who had two viral load tests performed with at least one test during each half of the past year | Number of people living with HIV/AIDS, ages 2 years and older | 82.7% | 1 if annual improvement target or performance goal met or exceeded | NYS DOH | P4P | P4P | |
| HIV/AIDS Comprehensive Care: Syphilis Screening See Appendix G for additional measure specifications | NYS-specific | NA | 3.e.i | Number of people who were screened for syphilis in the past year | Number of people living with HIV/AIDS, ages 19 years and older | 85.4% | 1 if annual improvement target or performance goal met or exceeded | NYS DOH | P4P | P4P | |
| Cervical Cancer Screening | HEDIS® 2019 | 0032 | 3.e.i | Number of women who had cervical cytology performed every 3 years or women, ages 30 to 64 years, who had cervical cytology/human papillomavirus (HPV) co- testing performed every 5 years | Number of women, ages 24 to 64 years | 83.9% | 1 if annual improvement target or performance goal met or exceeded | NYS DOH | P4R | P4P | |
| Chlamydia Screening (16 - 24 Years) | HEDIS® 2019 | 0033 | 3.e.i | Number of women who had at least one test for Chlamydia during the measurement year | Number of sexually active women, ages 16 to 24 | 80.0% | 1 if annual improvement target or performance goal met or exceeded | NYS DOH | P4P | P4P | |
| Viral Load Suppression See Appendix G for additional measure specifications | NYS-specific | NA | 3.e.i | Number of people whose most recent viral load result was below 200 copies | Number of people living with HIV/AIDS | 69.0% | 1 if annual improvement target or performance goal met or exceeded | PPS and NYS DOH | P4R | P4P | |
| Prevention Quality Indicator # 9 (Low Birth Weight Rate) +/- | AHRQ 7.0 | 0278 | 3.f.i | Number newborns with any diagnosis code for birth weight less than 2,500 grams | Number of newborns who were enrolled in Medicaid for at least one month as of June 30 of the measurement year | 25.12 per 1,000 newborns | 1 if annual improvement target or performance goal met or exceeded | NYS DOH | P4R | P4P | |
| Prenatal and Postpartum Care—Timeliness of Prenatal Care | HEDIS® 2019 | 1517 | 3.f.i | Number of women who had a prenatal care visit in their first trimester or within 42 days of enrollment in Medicaid | Number of women who gave birth in the last year | 93.9% | 0.5 if annual improvement target or performance goal met or exceeded | PPS and NYS DOH | P4R | P4P | |
| Prenatal and Postpartum Care—Postpartum Visits | HEDIS® 2019 | 1517 | 3.f.i | Number of women who had a postpartum care visit between 21 and 56 days after they gave birth | Number of women who gave birth in the last year | 81.6% | 0.5 if annual improvement target or performance goal met or exceeded | PPS and NYS DOH | P4R | P4P | |
| Well Care Visits in the first 15 months (5 or more Visits) | HEDIS® 2019 | 1392 | 3.f.i | Number of children who had five or more well- child visits with a primary care provider in their first 15 months of life | Number of children turning 15 months in the measurement year | 93.3% | 1 if annual improvement target or performance goal met or exceeded | NYS DOH | P4R | P4P | |
| Childhood Immunization Status (Combination 3 - 4313314) | HEDIS® 2019 | 0038 | 3.f.i | Number of children who were fully immunized (4 Diphtheria/Tetanus/Pert ussis, 3 Polio, 1 Measles/Mumps/Rubell a, 3 H Influenza type B, 3 Hepatitis B, 1 Varicella, and 4 pneumococca1) | Number of children turning age 2 in the measurement year | 88.4% | 1 if annual improvement target or performance goal met or exceeded | PPS and NYS DOH | P4R | P4P | |
| Lead Screening for Children | HEDIS® 2019 | NA | 3.f.i | Number of children who had their blood tested for lead poisoning at least once by their 2nd birthday | Number of children turning age 2 in the measurement year | 95.3% | 1 if annual improvement target or performance goal met or exceeded | PPS and NYS DOH | P4R | P4P | |
| Early Elective Deliveries (All inductions and cesarean sections that occur prior to onset of labor, occurring at or after 36 0/7 weeks and before 38 6/7 weeks gestation without documentation of listed maternal or fetal reason) ± | NYS Perinatal Quality Collaborative | NA | 3.f.i | Number of scheduled deliveries (i.e. All inductions and cesarean sections that occur prior to onset of labor) occurring at or after 36 0/7 weeks and before 38 6/7 weeks gestation without documentation of listed maternal or fetal reason | Number of scheduled deliveries (i.e. All inductions and cesarean sections that occur prior to onset of labor) occurring at or after 36 0/7 weeks and before 38 6/7 | NA - Pay for Reporting measure only | 1 | PPS | P4R | P4R | |
| Percentage of patients indicating need who were offered or provided an intervention for pain symptoms experienced during the past week | NA | NA | 3.g.i - 3.g.ii | Number of patients offered or provided an intervention for the question | Number of patients indicating need (responses of 2, 3, or 4 for the question) | Ratio greater than 1 | 1 if ratio greater than 1 | PPS | P4R | P4P | |
| Percentage of patients indicating need who were offered or provided an intervention for physical symptoms (other than pain) experienced during the past week | NA | NA | 3.g.i - 3.g.ii | Number of patients offered or provided an intervention for the question | Number of patients indicating need for one or more symptoms (responses of 2, 3, or 4 for the question) | Ratio greater than 1 | 1 if ratio greater than 1 | PPS | P4R | P4P | |
| Percentage of patients indicating need who were offered or provided an intervention for not feeling at peace during the past week | NA | NA | 3.g.i - 3.g.ii | Number of patients offered or provided an intervention for the question | Number of patients indicating need (responses of 2, 3, or 4 for the question) | Ratio greater than 1 | 1 if ratio greater than 1 | PPS | P4R | P4P | |
| Percentage of patients indicating need who were offered or provided an intervention for depressive feelings experienced during the past week | NA | NA | 3.g.i - 3.g.ii | Number of patients offered or provided an intervention for the question | Number of patients indicating need (responses of 2, 3, or 4 for the question) | Ratio greater than 1 | 1 if ratio greater than 1 | PPS | P4R | P4P | |
| Percentage of patients who were offered or provided an intervention when there was no advance directive in place | NA | NA | 3.g.i - 3.g.ii | Number of patients offered or provided an intervention for the question | Number of patients indicating need (response of 4 (None) for the question) | Ratio greater than 1 | 1 if ratio greater than 1 | PPS | P4R | P4P | |
| Annual Monitoring for Patients on Persistent Medications - ACE/ARB | HEDIS® 2019 | NA | 3.h.i | Number of people who had at least one blood test for potassium and a monitoring test for kidney function in the measurement year | Number of people, ages 18 and older, who received at least ACE inhibitors and/or ARBs a 180-day supply of | 95.4% | 1 if annual improvement target or performance goal met or exceeded | NYS DOH | P4R | P4P | |
± A lower rate is desirable.
* High Performance Eligible measure.
# Statewide measure.
Table 7. Domain 4 Measures
| Measure Name | Data Source | Projects Associated with Measure | Numerator Description | Denominator Description | Achievement Value | Reporting Responsibility | Payment: DY 2 through 5 |
|---|---|---|---|---|---|---|---|
| Percentage of premature death (before age 65 years) | NYS DOH Vital Statistics | 4.a.i - 4.a.iii, 4.b.i - 4.b.ii, 4.c.i - 4.c.iv, 4.d.i |
Number of people who died before age 65 in the measurement period | Number of deaths in the measurement period | Pay for Reporting measure only | NYS DOH | P4R |
| Percentage of premature death (before age 65 years) - Ratio of Black non-Hispanics to White non-Hispanics | NYS DOH Vital Statistics | 4.a.i - 4.a.iii, 4.b.i - 4.b.ii, 4.c.i - 4.c.iv, 4.d.i |
Percentage of Black non-Hispanics who died before age 65 | Percentage of White non- Hispanics who died before age 65 | Pay for Reporting measure only | NYS DOH | P4R |
| Percentage of premature death (before age 65 years) - Ratio of Hispanics to White non- Hispanics | NYS DOH Vital Statistics | 4.a.i - 4.a.iii, 4.b.i - 4.b.ii, 4.c.i - 4.c.iv, 4.d.i |
Percentage of Hispanics who died before age 65 | Percentage of White non- Hispanics who died before age 65 | Pay for Reporting measure only | NYS DOH | P4R |
| Age-adjusted preventable hospitalizations rate per 10,000 - Aged 18+ years | SPARCS | 4.a.i - 4.a.iii, 4.b.i - 4.b.ii, 4.c.i - 4.c.iv, 4.d.i |
Number of preventable hospitalizations for people age 18 or older | Number of people age 18 or older | Pay for Reporting measure only | NYS DOH | P4R |
| Age-adjusted preventable hospitalizations rate per 10,000 - Aged 18+ years - Ratio of Black non-Hispanics to White non- Hispanics | SPARCS | 4.a.i - 4.a.iii, 4.b.i - 4.b.ii, 4.c.i - 4.c.iv, 4.d.i |
Rate of preventable hospitalizations for Black non-Hispanics age 18 or older | Rate of preventable hospitalizations for White non-Hispanics age 18 or older | Pay for Reporting measure only | NYS DOH | P4R |
| Age-adjusted preventable hospitalizations rate per 10,000 - Aged 18+ years - Ratio of Hispanics to White non- Hispanics | SPARCS | 4.a.i - 4.a.iii, 4.b.i - 4.b.ii, 4.c.i - 4.c.iv, 4.d.i |
Rate of preventable hospitalizations for Hispanics age 18 or older | Rate of preventable hospitalizations for White non-Hispanics age 18 or older | Pay for Reporting measure only | NYS DOH | P4R |
| Percentage of adults with health insurance - Aged 18-64 years | US Census | 4.a.i - 4.a.iii, 4.b.i - 4.b.ii, 4.c.i - 4.c.iv, 4.d.i |
Number of respondents age 18-64 who reported that they had health insurance coverage | Number of people age 18-64 | Pay for Reporting measure only | NYS DOH | P4R |
| Age-adjusted percentage of adults who have a regular health care provider - Aged 18+ years | eBRFSS | 4.a.i - 4.a.iii, 4.b.i - 4.b.ii, 4.c.i - 4.c.iv, 4.d.i |
Number of respondents age 18 or older who reported that they had a regular health care provider | Number of people age 18 or older | Pay for Reporting measure only | NYS DOH | P4R |
| Age-adjusted percentage of adults with poor mental health for 14 or more days in the last month | eBRFSS | 4.a.i - 4.a.iii | Number of respondents age 18 or older who reported experiencing poor mental health for 14 or more days in the last month | Number of people age 18 or older | Pay for Reporting measure only | NYS DOH | P4R |
| Age-adjusted percentage of adult binge drinking during the past month | eBRFSS | 4.a.i - 4.a.iii | Number of respondents age 18 or older who reported binge drinking on one or more occasions in the past 30 days. Binge drinking is defined as men having 5 or more drinks or women having 4 or more drinks on one occasion. | Number of people age 18 or older | Pay for Reporting measure only | NYS DOH | P4R |
| Age-adjusted suicide death rate per 100,000 | NYS DOH Vital Statistics | 4.a.i - 4.a.iii | Number of deaths of people age 18 or older with an ICD-10 primary cause of death code: X60-X84 or Y87.0 | Number of people age 18 or older | Pay for Reporting measure only | NYS DOH | P4R |
| Percentage of adults who are obese | eBRFSS | 4.b.i - 4.b.ii | Number of respondents 18 or older who are obese. Obesity is defined as having a body mass index (BMI) of 30.0 or greater. | Number of people age 18 or older | Pay for Reporting measure only | NYS DOH | P4R |
| Percentage of children and adolescents who are obese | NYS excluding NYC: - Student Weight Status Category Reporting; NYC - Fitnessgram | 4.b.i - 4.b.ii | Number of public-school children who are obese. Obesity is defined as weight category greater than or equal to 95th percentile. Counties outside NYC: Grades K-12th; NYC counties: Grades K-8th. | Number of public-school children | Pay for Reporting measure only | NYS DOH | P4R |
| Percentage of cigarette smoking among adults | eBRFSS | 4.b.i - 4.b.ii | Number of people age 18 or older who report currently smoking cigarettes | Number of people age 18 or older | Pay for Reporting measure only | NYS DOH | P4R |
| Percentage of adults who receive a colorectal cancer screening based on the most recent guidelines - Aged 50-75 years | eBRFSS | 4.b.i - 4.b.ii | Number of respondents age 50-75 years who received a colorectal cancer screening exam (used a blood stool test at home in the past year; and/or, sigmoidoscopy in the past 5 years and blood stool test in the past 3 years; and/or, had a colonoscopy in the past 10 years) | Number of people age 50-75 | Pay for Reporting measure only | NYS DOH | P4R |
| Asthma emergency department visit rate per 10,000 | SPARCS | 4.b.i - 4.b.ii | Number of emergency department visits with primary diagnosis ICD-10-CM code J45 | Number of people | Pay for Reporting measure only | NYS DOH | P4R |
| Asthma emergency department visit rate per 10,000 - Aged 0-4 years | SPARCS | 4.b.i - 4.b.ii | Number of emergency department visits with primary diagnosis ICD-10-CM code J45 aged 0-4 years | Number of children aged 0-4 years | Pay for Reporting measure only | NYS DOH | P4R |
| Age-adjusted heart attack hospitalization rate per 10,000 | SPARCS | 4.b.i - 4.b.ii | Number of inpatient hospitalizations with a principal diagnosis ICD-10-CM code: I21, I22 | Number of people | Pay for Reporting measure only | NYS DOH | P4R |
| Rate of hospitalizations for short-term complications of diabetes per 10,000 - Aged 6-17 years | SPARCS | 4.b.i - 4.b.ii | Number of inpatient hospitalizations for children age 6-17 years with a principal diagnosis E1010, E1011, E10641, E1100, E1101, E11641 | Number of children age 6-17 years | Pay for Reporting measure only | NYS DOH | P4R |
| Rate of hospitalizations for short-term complications of diabetes per 10,000 - Aged 18+ years | SPARCS | 4.b.i - 4.b.ii | Number of inpatient hospitalizations for adults age 18 years or older with a principal diagnosis E1010, E1011, E10641, E1100, E1101, E11641 | Number of people age 18 or older | Pay for Reporting measure only | NYS DOH | P4R |
| Newly diagnosed HIV case rate per 100,000 | NYS HIV Surveillance System | 4.c.i - 4.c.ii | Number of people newly diagnosed with HIV, regardless of concurrent or subsequent AIDS diagnosis | Number of people | Pay for Reporting measure only | NYS DOH | P4R |
| Newly diagnosed HIV case rate per 100,000—Difference in rates (Black and White) of new HIV diagnoses | NYS HIV Surveillance System | 4.c.i - 4.c.ii | Rate of Black non-Hispanics newly diagnosed with HIV, regardless of concurrent or subsequent AIDS diagnosis | Rate of White non-Hispanics newly diagnosed with HIV, regardless of concurrent or subsequent AIDS diagnosis | Pay for Reporting measure only | NYS DOH | P4R |
| Newly diagnosed HIV case rate per 100,000—Difference in rates (Hispanic and White) of new HIV diagnoses | NYS HIV Surveillance System | 4.c.i - 4.c.ii | Rate of Hispanics newly diagnosed with HIV, regardless of concurrent or subsequent AIDS diagnosis | Rate of White non-Hispanics newly diagnosed with HIV, regardless of concurrent or subsequent AIDS diagnosis | Pay for Reporting measure only | NYS DOH | P4R |
| Gonorrhea case rate per 100,000 women - Aged 15-44 years | NYS STD Surveillance System | 4.c.iii - 4.c.iv | Number of women age 15-44 diagnosed with gonorrhea | Number of women age 15-44 | Pay for Reporting measure only | NYS DOH | P4R |
| Gonorrhea case rate per 100,000 men - Aged 15-44 years | NYS STD Surveillance System | 4.c.iii - 4.c.iv | Number of men age 15-44 diagnosed with gonorrhea | Number of men age 15-44 | Pay for Reporting measure only | NYS DOH | P4R |
| Chlamydia case rate per 100,000 women - Aged 15-44 years | NYS STD Surveillance System | 4.c.iii - 4.c.iv | Number of women age 15-44 diagnosed with Chlamydia | Number of women age 15-44 | Pay for Reporting measure only | NYS DOH | P4R |
| Primary and secondary syphilis case rate per 100,000 males | NYS STD Surveillance System | 4.c.iii - 4.c.iv | Number of men diagnosed with primary or secondary syphilis | Number of men | Pay for Reporting measure only | NYS DOH | P4R |
| Primary and secondary syphilis case rate per 100,000 females | NYS STD Surveillance System | 4.c.iii - 4.c.iv | Number of women diagnosed with primary or secondary syphilis | Number of women | Pay for Reporting measure only | NYS DOH | P4R |
| Percentage of preterm births | NYS DOH Vital Statistics | 4.d.i | Number of infants born at less than 37 weeks gestation among infants with known gestational age | Number of births within the measurement period | Pay for Reporting measure only | NYS DOH | P4R |
| Percentage of preterm births - Ratio of Black non-Hispanics to White non-Hispanics | NYS DOH Vital Statistics | 4.d.i | Percentage of preterm births for Black non-Hispanics | Percentage of preterm births for White non-Hispanics | Pay for Reporting measure only | NYS DOH | P4R |
| Percentage of preterm births - Ratio of Hispanics to White non- Hispanics | NYS DOH Vital Statistics | 4.d.i | Percentage of preterm births for Hispanics | Percentage of preterm births for White non-Hispanics | Pay for Reporting measure only | NYS DOH | P4R |
| Percentage of preterm births - Ratio of Medicaid births to non- Medicaid births | NYS DOH Vital Statistics | 4.d.i | Percentage of preterm births whose primary payer is Medicaid | Percentage of preterm births whose primary payer is non- Medicaid | Pay for Reporting measure only | NYS DOH | P4R |
| Percentage of infants exclusively breastfed in the hospital | NYS DOH Vital Statistics | 4.d.i | Number of infants exclusively fed breast milk in the hospital | Number of births within the measurement period | Pay for Reporting measure only | NYS DOH | P4R |
| Percentage of infants exclusively breastfed in the hospital - Ratio of Black non-Hispanics to White non-Hispanics | NYS DOH Vital Statistics | 4.d.i | Percentage of Black non-Hispanic infants exclusively fed breast milk in the hospital | Percentage of White non- Hispanic infants exclusively fed breast milk in the hospital | Pay for Reporting measure only | NYS DOH | P4R |
| Percentage of infants exclusively breastfed in the hospital - Ratio of Hispanics to White non-Hispanics | NYS DOH Vital Statistics | 4.d.i | Percentage of Hispanic infants exclusively fed breast milk in the hospital | Percentage of White non-Hispanic infants exclusively fed breast milk in the hospital | Pay for Reporting measure only | NYS DOH | P4R |
| Percentage of infants exclusively breastfed in the hospital - Ratio of Medicaid births to non- Medicaid births | NYS DOH Vital Statistics | 4.d.i | Percentage of infants exclusively fed breast milk in the hospital for births whose primary payer is Medicaid | Percentage of infants exclusively fed breast milk in the hospital for births whose primary payer is non- Medicaid | Pay for Reporting measure only | NYS DOH | P4R |
| Maternal mortality rate per 100,000 births | NYS DOH Vital Statistics | 4.d.i | Number of deaths to women from any causes related to or aggravated by pregnancy or its management that codes O00-95, O98-O99, and A34 (obstetrical tetanus)) | Number of births within the measurement period | Pay for Reporting measure only | NYS DOH | P4R |
| Percentage of children with any kind of health insurance - Aged under 19 years | US Census | 4.d.i | Number of children aged under 19 years with any kind of health insurance coverage in the past 12 months | Number of children aged under 19 years | Pay for Reporting measure only | NYS DOH | P4R |
| Adolescent pregnancy rate per 1,000 females - Aged 15-17 years | NYS DOH Vital Statistics | 4.d.i | Number of pregnancies (the sum of the number of live births, induced terminations of pregnancies, and all fetal deaths) in adolescent females aged 15-17 years | Number of females aged 15- 17 years | Pay for Reporting measure only | NYS DOH | P4R |
| Adolescent pregnancy rate per 1,000 females - Aged 15-17 years - Ratio of Black non- Hispanics to White non- Hispanics | NYS DOH Vital Statistics | 4.d.i | Rate of pregnancies in Black non-Hispanic adolescent females aged 15-17 years | Rate of pregnancies in White non-Hispanic adolescent females aged 15-17 years | Pay for Reporting measure only | NYS DOH | P4R |
| Adolescent pregnancy rate per 1,000 females - Aged 15-17 years—Ratio of Hispanics to White non-Hispanics | NYS DOH Vital Statistics | 4.d.i | Rate of pregnancies in Hispanic adolescent females aged 15-17 years | Rate of pregnancies in White non-Hispanic adolescent females aged 15-17 years | Pay for Reporting measure only | NYS DOH | P4R |
| Percentage of unintended pregnancy among live births | NYS DOH Vital Statistics | 4.d.i | Number of unintended pregnancies (current pregnancy indicated as ´Wanted Later´ or ´Wanted Never´) among live births | Number of live births | Pay for Reporting measure only | NYS DOH | P4R |
| Percentage of unintended pregnancy among live births - Ratio of Black non-Hispanics to White non-Hispanics | NYS DOH Vital Statistics | 4.d.i | Percentage of unintended pregnancies among Black non-Hispanic females | Percentage of unintended pregnancies among White non-Hispanic females | Pay for Reporting measure only | NYS DOH | P4R |
| Percentage of unintended pregnancy among live births— Ratio of Hispanics to White non- Hispanics | NYS DOH Vital Statistics | 4.d.i | Percentage of unintended pregnancies among Hispanic females | Percentage of unintended pregnancies among White non-Hispanic females | Pay for Reporting measure only | NYS DOH | P4R |
| Percentage of unintended pregnancy among live births— Ratio of Medicaid births to non- Medicaid births | NYS DOH Vital Statistics | 4.d.i | Percentage of unintended pregnancies for births whose primary payer is Medicaid | Percentage of unintended pregnancies for births whose primary payer is non- Medicaid | Pay for Reporting measure only | NYS DOH | P4R |
| Percentage of women with health coverage - Aged 18-64 years | US Census | 4.d.i | Number of female respondents aged 18- 64 who reported that they had health insurance coverage | Number of females aged 18- 64 | Pay for Reporting measure only | NYS DOH | P4R |
| Percentage of live births that occur within 24 months of a previous pregnancy | NYS DOH Vital Statistics | 4.d.i | Number of live births that occur within 24 months of a previous pregnancy | Number of live births | Pay for Reporting measure only | NYS DOH | P4R |
IX. Random Sample, Medical Record Review Guidelines,
and Early Elective Delivery Data Collection
Medical Record Chart/ Electronic Health Record Collection Steps
These guidelines apply to the following measures:
- Screening for Clinical Depression and Follow Up
- Controlling High Blood Pressure
- Comprehensive Diabetes Care
- Viral Load Suppression
- Prenatal/Postpartum care
- Childhood Immunization
- Lead Screening for Children (same sample as Childhood Immunization)
Step 1: NYS DOH will run the measure´s eligible population for the PPS´ attributed members. The measure´s eligible population is further defined by any measure-specific criteria based on the technical specifications for each measure (e.g. continuous enrollment, age or diagnosis).
Step 2: NYS DOH will draw a systematic random sample (n = 453) using a random index number after sorting the eligible population for each PPS. The random sample will include an oversample of 10% (453 + 46 = 499). Members will be identified as being included in the sample or being in the oversample. Members in the sample cannot be removed from the sample unless they meet an exclusion criterion for the measure. Members who are excluded from the measure, as defined by the specifications, will be excluded from the sample and the first member in the oversample will be brought into the sample, and so forth for each exclusion. Oversample members not included in the sample remain in the oversample. Every member in the sample and oversample will be accounted for in the member detail files returned to NYS DOH. (See Appendix B)
Step 3: The random sample, including the oversample, will be sent to the Medical record review (MRR) vendors using a secure file transfer mechanism. In addition to the sample, multiple files will be sent to the MRR vendor for each measure. These files contain member information such as Medicaid eligibility segments, PPS Identifier, Medicaid Client Identification Number, first and last name, and numerator information from administrative data. Additional files linking the member to services provided include information about the provider and visit/service information such as dates of visits/services, National Provider Identifier(s) (NPI) of the provider(s) associated with visits or services, and other measure specific requirements (i.e. HbA1C tests, or date of delivery).
Step 4: The MRR vendors will use abstraction tools and will develop training materials for review staff. The tool and materials must be approved by the licensed audit organization contracted by the Independent Assessor.
Step 5: Using the files as well as additional data sources, such as Qualified Entities (RHIOs) and health plans, the PPS and vendor will develop the record chases, using developed logic, to identify the practices and locations where records exist for the members that can be used in the medical record review.
Step 6: The PPS staff and MRR vendors are responsible for working with the providers to retrieve the required information from the medical records (paper or electronic). The PPS and vendors will coordinate the record retrieval and materials. Information is abstracted from records using trained medical record review staff. The abstracted information will be entered in the abstraction tool. If the medical record does not contain information for care provided in the measurement year, other medical records, if available, are pursued for review. Members cannot be excluded from the sample because no records are located. Each measure contains information about required and optional exclusions. Members meeting the measure criteria for exclusion can be removed from the sample and a member from the oversample will be moved into the sample. The PPS will receive additional administrative data from the State regarding claims or encounters for the measurement year that should be included in the chase logic for members who remain numerator non-compliant.
Step 7: In early December, the PPS and vendor will prepare a list of numerator compliant members for each measure by PPS. The licensed audit organization will determine a random sample and request a set of records from the PPS and vendor to use in validation. The licensed audit organization will conduct a medical record review validation for the sample of medical records (n = 30) per measure. If the validation process determines numerator-compliance findings to be invalid, the data will be invalidated and not incorporated into the PPS´s final result for that measure. Results from the licensed audit organization´s findings for each measure will be sent from the licensed audit organization to NYS DOH at the end of January.
Step 8: The PPS or MRR vendors will extract the abstracted data, determine numerator and denominator status for each member in the sample file and complete the member detail file.
Step 9: The PPS and MRR vendors will submit the completed member detail file to NYS DOH via a secure file transfer mechanism. Member attribution to the PPS will be reconciled. The information in the file, and the validation findings, will be incorporated with administrative data to calculate the PPS final result for the measure for the measurement year.
Measurement Year 5 MRR Timeline 2019-2020
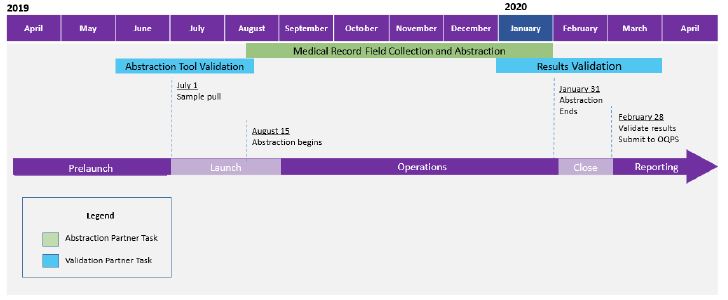
Reporting for Early Elective Delivery (Project 3.f.i)
Birthing hospitals associated with a PPS that has chosen project 3.f.i. will be required to review medical records for all inductions and cesarean sections that occur prior to onset of labor occurring at or after 36 0/7 weeks and before 38 6/7 weeks gestation during the time period of July 1 of the year prior through June 30 of the current year. Information collected for each qualifying delivery will be submitted to the NYS Perinatal Quality Collaborative by December 1 of the current year.
Step 1: The hospital will review all medical records for inductions and cesarean sections that occur prior to onset of labor occurring at or after 36 0/7 weeks and before 38 6/7 weeks gestation. Information about each qualifying delivery will be recorded on the appropriate form and submitted using the steps below.
Step 2: Trained medical record review staff should abstract information using the Scheduled Delivery Form for all scheduled deliveries with the relevant gestational age that occur within the measurement year (See Appendix C). If a hospital has zero inductions and cesarean sections that occur prior to onset of labor occurring at or after 36 0/7 weeks and before 38 6/7 weeks gestation, the hospital will be required to complete an aggregate data log indicating there were zero scheduled deliveries for that time period.
Step 3: The completed forms will be submitted through the NYS DOH Health Commerce System (HCS) using the application called the NYS Perinatal Quality Collaborative (NYSPQC) Scheduled Delivery Form System. Each hospital will need to have a designated person with an HCS account and proper roles assigned to access this secure system. For questions about getting an HCS account, or locating who in your organization may have an already existing account, please e-mail NYSPQC@health.state.ny.us.
Step 4: The information submitted will be used to calculate the PPS´s final result for the measure for the measurement year. For each PPS calculation, hospital-specific results will be aggregated and averaged across all birthing hospitals within each PPS network. If a hospital participates with more than one PPS, the hospital does not need to enter information more than once. The same hospital-specific data will be used for each PPS network in which the hospital participates.
X. Aggregate Data Reporting
Several measures will be reported by the PPS in aggregate, such as workforce milestones in Domain 1. The PPS will provide aggregated data to the Independent Assessor at the required intervals. Instructions about the file variables and mechanism for reporting data will be forthcoming from the Independent Assessor.
XI. Member Detail File Requirements and Layout
Each MRR vendor will submit the member detail file to NYS DOH via a secure file transfer by the February deadline for the measurement year. Information which contains invalid Client Identification Numbers or invalid values in the denominator or numerator fields will not be used. See Appendix B for the file layout and column value definitions.
XII. Final Result Calculation
For measures requiring medical record data, NYS DOH will incorporate information from the member detail file with the administrative data for the measurement year to calculate the PPS´ final results for the measurement year. Measures calculated by NYS DOH will be produced in February following the measurement year after the January refresh of the December encounter and claims data are loaded in the Medicaid data system. This allows a six-month run out of claims and encounters prior to calculating measure results.
XIII. Data to Performing Provider Systems and Independent Assessor
NYS DOH will aggregate all results and provide information to the Independent Assessor. The Independent Assessor will determine whether annual improvement targets and high-performance levels (where applicable) were attained. PPS will receive reports containing final measure results, achievement value attainment, and high-performance attainment for the completed measurement year, as well as annual improvement targets and high-performance levels for the next measurement year.
Appendix A - Domain 1 Project Milestones and Metrics
Domain 1 Project Milestones & Metrics are based largely on investments in training and recruiting personnel, identifying project leadership, and developing clinical protocols that will strengthen the PPS´ ability to successfully meet DSRIP project goals. Additionally, the project requirements include specific provider-level commitments to increase the availability of NCQA-certified PCPs, invest in HIT, and fully establish the project programs (medical villages, Ambulatory ICUS, etc.). Each requirement´s milestone and associated metrics are detailed. These requirements also comprise of the completion time period in addition to the unit level of reporting, both which are discussed in further detail below.
Completion of project requirements falls into three key timeframes:
- System Transformation Changes Due by Dy3
Based upon the work plan section in Attachment I (NY DSRIP Program Funding and Mechanics Protocol), no more than the first two years will be utilized to implement major system changes related to the project. For example, project requirements within this category include developing clinical protocols, training for care coordinators, identifying key project personnel, performing population health management activities, and using EHRs or other technical platforms to track actively engaged patients.- Requirements Requiring Completion by DY4
A number of project requirements detail prescribed end dates within their description. Two of these project requirements are safety net providers actively sharing medical records with RHIO/SHIN-NY by the end of DY3 and PCPs achieving NCQA 2014 Level 3 PCMH certification by the end of DY3.- Completion Adhering to Speed and Scale Commitments
The due dates for these project requirements are at the discretion of the PPS and should be consistent with commitments made in the speed and scale sections of the approved application. Example requirements include: implementing open access scheduling, deploying a provider notification/secure messaging system, and converting outdated or unneeded hospital capacity.Completion of project requirements is also delineated by the unit level of reporting:
- Project-Unit Level Reporting
These are Domain 1 requirements reported at the project-wide level and demonstrating the PPS´ overall project performance and success. Some of these requirements are performing population health management activities, developing a comprehensive care plan for each patient, establishing partnerships between primary care providers and participating Health Homes, and developing educational materials consistent with cultural and linguistic needs of the population.- Provider-Unit Level Reporting
These are Domain 1 requirements for which performance and success must be demonstrated and reported at the individual provider/practice site level. Note: Applicable provider types, by which reporting will be demarcated, refer to the classifications each PPS selected along with speed and scale submissions.Appendix B - Performing Provider System Member Detail File
The information from the medical record review will be used to determine denominator and numerator status for each member in the sample for the PPS. Members may be involved in more than one measure, and all of the measure information for that member will be in the single row. Files will be completed using the following file layout and formats in the table below. All rows will be the same length. Zero fill all columns that are not applicable to the member, such as measures not associated with the PPS´ projects.
Members identified as 1 through 453 in the sample file are considered to be the denominator for the measure and those identified from 454 through 499 are considered the oversample. For the member detail file, those who were in the denominator should be reflected with a value ‘1´. If a member meets exclusion criteria for the measure, the member´s denominator status will be ‘8´ indicating exclusion. The first member in the oversample will then be pulled into the denominator. All members from the oversample who are not included in the denominator will be indicated as ‘9´ in the denominator column. If the sample has less than 453 members and some are excluded, the final denominator will be less than 453. Most numerator status columns for the measure will also be indicated as ‘1´ if the member is numerator compliant for the measure or ‘0´ if numerator non-compliant. Two measures use a count of events in the numerator fields, so there may be more values than ‘1´ and ‘0´ in those columns.
Column Placement Name Direction Allowed Values Column 1-2 PPS ID Enter the PPS´ two-digit numeric PPS ID. ## Column 3-10 CIN A member´s client identification number. The field should be continuous without any spaces or hyphens. The field is alpha- numeric and should be treated as a text field. This field is mandatory - do not leave it blank!
- The CIN entered in this field should be for the CIN for the measurement year. For example, CINs for 2016 should be used.
- For Medicaid, use the 8-digit, alpha-numeric CIN.
AA#####A Column 11 Denominator for Screening for Clinical Depression and Follow Up Enter a ´1´ if this member is in the denominator of the Screening for Clinical Depression and Follow Up measure, ´0´ if the member is not in the denominator of this measure. If the member was excluded from the denominator, enter ´8´. If the member remained in the oversample and is not in the final denominator, enter ´9´. 1 = Yes
0 = No
8 = Exclusion
9 = OversampleColumn 12 Numerator component 1 for Screening for Clinical Depression and Negative Result Enter a ´1´ if this member is in the numerator component 1 of the Screening for Clinical Depression and Follow Up measure, ´0´ if the member is not in the numerator component 1 or the information is missing. 1 = Yes
0 = NoColumn 13 Numerator component 2 for Screening for Clinical Depression and Follow Up Enter a ´1´ if this member is in the numerator component 2 of the Screening for Clinical Depression and Follow Up measure, ´0´ if the member is not in the numerator component 2 or the information is missing. 1 = Yes
0 = NoColumn 14 Numerator component 3 for Screening for Clinical Depression and Follow Up Enter a ´1´ if this member is in the numerator component 3 of the Screening for Clinical Depression and Follow Up measure, ´0´ if the member is not in the numerator component 3 or the information is missing. 1 = Yes
0 = NoColumn 15 Numerator component 4 for Screening for Clinical Depression and Follow Up Enter a ´1´ if this member is in the numerator component 4 of the Screening for Clinical Depression and Follow Up measure, ´0´ if the member is not in the numerator component 4 or the information is missing. 1 = Yes
0 = NoColumn 16 Denominator for Controlling High Blood Pressure (CBP) Enter a ´1´ if this member is in the denominator of the CBP measure, ´0´ if the member is not in the denominator of this measure. If the member was excluded from the denominator, enter ´8´. If the member remained in the oversample and is not in the final denominator, enter ´9´. 1 = Yes
0 = No
8 = Exclusion
9 = OversampleColumn 17 Numerator for Controlling High Blood Pressure (CBP) Enter a ´1´ if this member is in the numerator of the CBP measure, ´0´ if the member is not in the numerator or the information is missing. 1 = Yes
0 = NoColumn 18 Denominator for Comprehensive Diabetes Care (CDC) Enter a ´1´ if this member is in the denominator of the CDC measures, ´0´ if the member is not in the denominator of this measure. If the member was excluded from the denominator, enter ´8´. If the member remained in the oversample and is not in the final denominator, enter ´9´. 1 = Yes
0 = No 8 = Exclusion 9 = OversampleColumn 19 Numerator 1 for CDC - HbA1c Test Enter a ´1´ if this member is in the numerator of the CDC HbA1c Test measure, ´0´ if the member is not in the numerator or the information is missing. 1 = Yes
0 = NoColumn 20 Numerator 2 for CDC - HbA1c Poor Control (>9%) Enter a ´1´ if this member is in the numerator of the CDC HbA1c Poor Control measure (which includes no test performed and test result missing from the record as well as HbA1c ≥ 9.0%), ´0´ if the member is not in the numerator or if the member´s HbA1c ≤ 9.0%. 1 = Yes
0 = NoColumn 21 Numerator 3 for CDC - Eye Exam Enter a ´1´ if this member is in the numerator of the CDC Eye Exam measure, ´0´ if the member is not in the numerator or the information is missing. 1 = Yes
0 = NoColumn 22 Numerator 4 for CDC - Medical Attention for Nephropathy Enter a ´1´ if this member is in the numerator of the CDC Medical Attention for Nephropathy measure, ´0´ if the member is not in the numerator or the information is missing. 1 = Yes
0 = NoColumn 23 Denominator for Viral Load Suppression Enter a ´1´ if this member is in the denominator of the Viral Load Suppression measure, ´0´ if the member is not in the denominator of this measure. If the member was excluded from the denominator, enter ´8´. If the member remained in the oversample and is not in the final denominator, enter ´9´. 1 = Yes
0 = No
8 = Exclusion
9 = OversampleColumn 24 Numerator for Viral Load Suppression Enter a ´1´ if this member is in the numerator of the Viral Load Suppression measure, ´0´ if the member is not in the numerator or the information is missing. 1 = Yes
0 = NoColumn 25 Denominator for Prenatal and Postpartum Care (PPC) Enter the number of times this member is in the denominator of the Prenatal and Postpartum Care measures, ´0´ if the member is not in the denominator of this measure. If the member was excluded from the denominator, enter ´8´. If the member remained in the oversample and is not in the final denominator, enter ´9´. 0 - 2 8 = Exclusion 9 = Oversample Column 26 Numerator 1 for PPC - Timeliness of Prenatal Care Enter the number of times this member is in numerator of PPC - Timeliness of Prenatal Care measure, ´0´ if the member is not in the numerator or the information is missing. 0 - 2 Column 27 Numerator 2 for PPC - Postpartum Care Enter the number of times this member is in the numerator of PPC - Postpartum Care measure, ´0´ if the member is not in the numerator or the information is missing. 0 - 2 Column 28 Denominator for Childhood Immunization (CIS) Enter a ´1´ if this member is in the denominator of the CIS measure, ´0´ if the member is not in the denominator of this measure. If the member was excluded from the denominator, enter ´8´. If the member remained in the oversample and is not in the final denominator, enter ´9´. 1 = Yes
0 = No
8 = Exclusion
9 = OversampleColumn 29 Numerator 1 for CIS - Four DTaP Enter the number of times this member has a vaccination meeting HEDIS® specifications for DTaP in numerator of the CIS- Four DTaP measure. Enter ´0´ if this member did not receive any DTaP vaccinations meeting HEDIS® specifications. 0-9 Column 30 Numerator 2 for CIS - Three IPV Enter the number of times this member has a vaccination meeting HEDIS® specifications for IPV in numerator of the CIS - Three IPV measure. Enter ´0´ if this member did not receive any IPV vaccinations meeting HEDIS® specifications. 0-9 Column 31 Numerator 3 for CIS - One MMR Enter the number of times this member has a vaccination meeting HEDIS® specifications for MMR in numerator of the CIS - One MMR measure. Enter ´0´ if this member did not receive any MMR vaccinations meeting HEDIS® specifications. Enter ´1´ if the member has a history of illness or seropositive result. 0-9 Column 32 Numerator 4 for CIS - Three HiB Enter the number of times this member has a vaccination meeting HEDIS® specifications for HiB in numerator of the CIS - Three HiB measure. Enter ´0´ if this member did not receive any HiB vaccinations meeting HEDIS® specifications. 0-9 Column 33 Numerator 5 for CIS - Three Hepatitis B Enter the number of times this member has a vaccination meeting HEDIS® specifications for Hepatitis B in numerator of the CIS - Three Hepatitis B measure. Enter ´0´ if this member did not receive any Hepatitis B vaccinations meeting HEDIS® specifications. Enter ´3´ if the member has a history of illness or seropositive result. 0-9 Column 34 Numerator 6 for CIS - One VZV Enter the number of times this member has a vaccination meeting HEDIS® specifications for VZV in numerator of the CIS - One VZV measure. Enter ´0´ if this member did not receive any VZV vaccinations meeting HEDIS® specifications. Enter ´1´ if the member has a history of illness or seropositive result. 0-9 Column 35 Numerator 7 for CIS - Four Pneumococcal Conjugate Enter the number of times this member has a vaccination meeting HEDIS® specifications for Pneumococcal Conjugate in numerator of the CIS - Four Pneumococcal Conjugate measure. Enter ´0´ if this member did not receive any Pneumococcal Conjugate vaccinations meeting HEDIS® specifications. 0-9 Column 36 Denominator for Lead Screening for Children Enter a ´1´ if this member is in the denominator of the Lead Screening for Children measure, ´0´ if the member is not in the denominator of this measure. If the member was excluded from the denominator, enter ´8´. If the member remained in the oversample and is not in the final denominator, enter ´9´. 1 = Yes
0 = No
8 = Exclusion
9 = OversampleColumn 37 Numerator for Lead Screening for Children Enter a ´1´ if this member is in the numerator of the Lead Screening for Children measure, ´0´ if the member is not in the numerator or the information is missing. 1 = Yes
0 = NoAppendix C - New York State Perinatal Quality Collaborative
Scheduled Delivery Form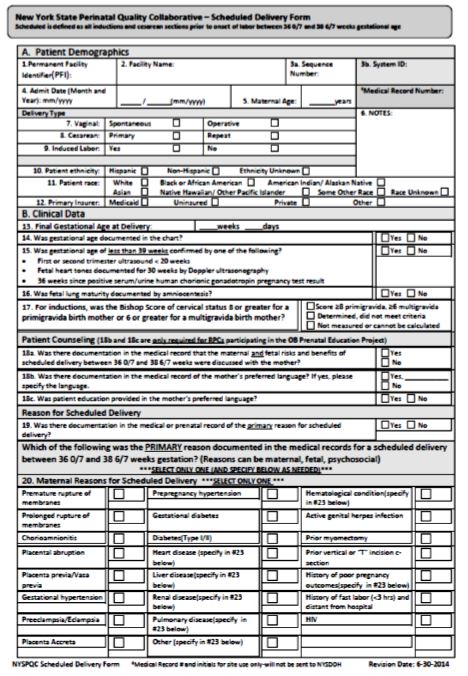
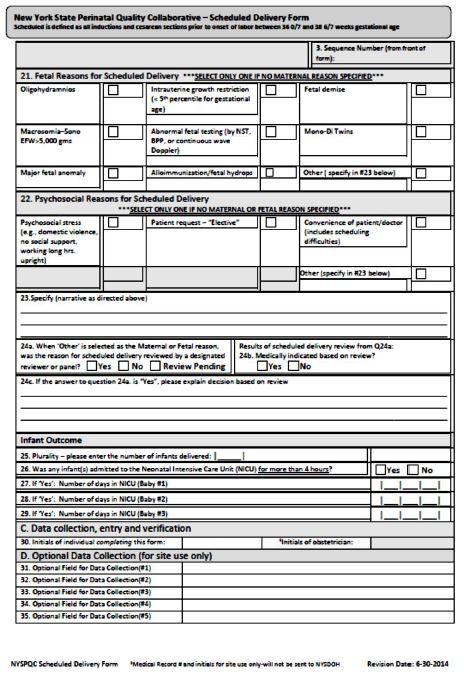
Appendix D - Example of PAM Data File
All PPS should submit the following data file as an attachment to the 2.d.i. module in regular quarterly reports. Data files must be in .csv format. Fields should be left justified and blank filled for the column width. All fields are required.
Data submission requirements:
- All data must be submitted for performance-eligible individuals only (those having received at least two PAMs over the course of DSRIP)
- All data must apply only to the last survey administered in each applicable Measurement Year; do not submit multiple scores for the same individual
- Any individuals who were ineligible at baseline (e.g. were enrolled in a Health Home at time of first PAM or insured commercially) should be removed from results (current years and previous years)
- No survey results that have been indicated as "outliers" in Flourish should be included.
Column Placement Variable Description Value Labels Details/Comments 1-2 PPS ID 2 Characters 3-17 User Identifier 15 Characters 18-32 Insignia ID 15 Characters 33-46 Survey Type 14 Characters Ex: PAM10, ParentPAM10, CaregiverPAM10 47-54 Survey Date Completed mmddyyyy 99999999 = Missing 8-digit date field (do not include dashes or slashes) 55 Measurement Year (MY) 1 Character Numerical digit 1-5 56 Cohort 1 Character Cohort A = Individuals receiving first PAM assessment during MY 1
Cohort B = Individuals receiving first PAM assessment during MY 2
Cohort C = Individuals receiving first PAM assessment during MY 3
Cohort D = Individuals receiving first PAM assessment during MY 4
Cohort E = Individuals receiving first PAM assessment during MY 557-60 PAM Score 3 Characters If the PAM score is one or two digits, enter with preceding zeros (ex: 001) Decimals may be included when necessary (ex: 45.5) 61 PAM Level 1 Character Appendix E - NYSDOH C&G CAHPS Survey of the Uninsured File Layout
- Data file must be in text file format.
- All fields are required.
Column Placement Variable Description Value Labels Details/Comments 1-10 Unique Record ID 10 Characters 10-digit, numeric field 11-47 PPS Name 30 Characters PPS name consistent with MAPP reporting tool. 48-49 PPS ID 2 Characters 2-digit, numeric field
Adirondack Health Institute = 23
Better Health for Northeast NY = 01
Central New York Care Collaborative = 08
Alliance for Better Health = 03
Finger Lakes PPS = 09
Millennium Collaborative Care = 48
Leatherstocking Collaborative Health Partners = 22
Nassau Queens PPS = 14
One City Health = 52
Staten Island PPS = 43
North Country Initiative = 45
Suffolk Care Collaborative = 16
Care Compass Network = 44
WMCHealth = 2150-69 Practice Site Name 20 Characters 70-79 Provider NPI or ID 10 Characters National Provider Identifier or a Unique ID for each provider. Resident doctors can be submitted using ´res´ in the Provider ID followed by 7 alphanumeric characters (i.e. res9A64944). 80 Survey Disposition Code 1 = Mail
2 = On Site at Provider Office
3 = Phone or Other
9 = Missing81 Survey Complete Flag 0= Complete
1 = IncompleteA survey is complete if respondents did not say ´No´ to Question 1 ("Our records show that you got care from the provider named below in the last 6 months. [PROVIDER NAME]. Is that right?" and they did not answer ´none´ to Question 4 ("In the last 6 months, how many times did you visit this provider to get care for yourself?") and if they provided a response to at least one question. 82-83 Survey Received Date - month mm 99 = Missing 2-digit date field (do not include dashes or slashes) 84-85 Survey Received Date - day dd 99 = Missing 2-digit date field (do not include dashes or slashes) 86-89 Survey Received Date - year yyyy 99 = Missing 4-digit date field (do not include dashes or slashes) 90 Q1. Our records show that you got care from the provider named below in the last 6 months. Is that right? 1 = Yes
2 = No
8 = Multiple mark
9 = Missing91 Q2. Is this the provider you usually see if you need a check-up, want advice about a health problem, or get sick or hurt? 1 = Yes
2 = No
8 = Multiple mark
9 = Missing92 Q3. How long have you been going to this provider? 1 = Less than 6 months
2 = At least 6 months but less than 1 year
3 = At least 1 year but less than 3 years
4 = At least 3 years but less than 5 years
5 = 5 years or more
8 = Multiple mark
9 = Missing93 Q4. In the last 6 months, how many times did you visit this provider to get care for yourself? 1 = None
2 = 1 time
3 = 2
4 = 3
5 = 4
6 = 5 to 9
7 = 10 or more times
8 = Multiple mark
9 = Missing94 Q5. In the last 6 months, did you contact this provider´s office to get an appointment for an illness, injury, or condition that needed care right away? 1 = Yes
2 = No
8 = Multiple mark
9 = Missing95 Q6. In the last 6 months, when you contacted this provider´s office to get an appointment for care you needed right away, how often did you get an appointment as soon as you needed? 1 = Never
2 = Sometimes
3 = Usually
4 = Always
8 = Multiple mark
9 = Missing96 Q7. In the last 6 months, did you make any appointments for a check-up or routine care with this provider? 1 = Yes
2 = No
8 = Multiple mark
9 = Missing97 Q8. In the last 6 months, when you made an appointment for a check-up or routine care with this provider, how often did you get an appointment as soon as you needed? 1 = Never
2 = Sometimes
3 = Usually
4 = Always
8 = Multiple mark
9 = Missing98 Q9. In the last 6 months, did you contact this provider´s office with a medical question during regular office hours? 1 = Yes
2 = No
8 = Multiple Mark
9 = Missing99 Q10. In the last 6 months, when you contacted this provider´s office during regular office hours, how often did you get an answer to your medical question that same day? 1 = Never
2 = Sometimes
3 = Usually
4 = Always
8 = Multiple mark
9 = Missing100 Q11. In the last 6 months, how often did this provider explain things in a way that was easy to understand? 1 = Never
2 = Sometimes
3 = Usually
4 = Always
8 = Multiple mark
9 = Missing101 Q12. In the last 6 months, how often did this provider listen carefully to you? 1 = Never
2 = Sometimes
3 = Usually
4 = Always
8 = Multiple mark
9 = Missing102 Q13. In the last 6 months, how often did this provider seem to know the important information about your medical history? 1 = Never
2 = Sometimes
3 = Usually
4 = Always
8 = Multiple mark
9 = Missing103 Q14. In the last 6 months, how often did this provider show respect for what you had to say? 1 = Never
2 = Sometimes
3 = Usually
4 = Always
8 = Multiple mark
9 = Missing104 Q15. In the last 6 months, how often did this provider spend enough time with you? 1 = Never
2 = Sometimes
3 = Usually
4 = Always
8 = Multiple mark
9 = Missing105 Q16. In the last 6 months, did this provider order a blood test, x-ray, or other test for you? 1 = Yes
2 = No
8 = Multiple Mark
9 = Missing106 Q17. In the last 6 months, when this provider ordered a blood test, x-ray, or other test for you, how often did someone from this provider´s office follow-up to give you those results? 1 = Never
2 = Sometimes
3 = Usually
4 = Always
8 = Multiple mark
9 = Missing107-108 Q18. Using any number from 0 to 10, where 0 is the worst provider possible and 10 is the best provider possible, what number would you use to rate this provider? 00 = 0 Worst provider possible
01 = 1
02 = 2
03 = 3
04 = 4
05 = 5
06 = 6
07 = 7
08 = 8
09 = 9
10 = 10 Best provider possible
88 = Multiple Mark
99 = Missing109 Q19. In the last 6 months, did you take any prescription medicine? 1 = Yes
2 = No
8 = Multiple Mark
9 = Missing110 Q20. In the last 6 months, how often did you and someone from this provider´s office talk about all the prescription medicines you were taking? 1 = Never
2 = Sometimes
3 = Usually
4 = Always
8 = Multiple mark
9 = Missing111 Q21. In the last 6 months, how often were clerks and receptionists at this provider´s office as helpful as you thought they should be? 1 = Never
2 = Sometimes
3 = Usually
4 = Always
8 = Multiple mark
9 = Missing112 Q22. In the last 6 months, how often did clerks and receptionists at this provider´s office treat you with courtesy and respect? 1 = Never
2 = Sometimes
3 = Usually
4 = Always
8 = Multiple mark
9 = Missing113 Q23. In general, how would you rate your overall health? 1 = Excellent
2 = Very good
3 = Good
4 = Fair
5 = Poor
8 = Multiple Mark
9 = Missing114 Q24. In general, how would you rate your overall mental or emotional health? 1 = Excellent
2 = Very good
3 = Good
4 = Fair
5 = Poor
8 = Multiple Mark
9 = Missing115 Q25. What is your age? 1 = 18 to 24
2 = 25 to 34
3 = 35 to 44
4 = 45 to 54
5 = 55 to 64
6 = 65 to 74
7 = 75 or older
8 = Multiple Mark
9 = Missing116 Q26. Are you male or female? 1 = Male
2 = Female
8 = Multiple mark
9 = Missing117 Q27. What is the highest grade or level of school that you have completed? 1 = 8 th grade or less
2 = Some high school, but did not graduate
3 = High school graduate or GED
4 = Some college or 2-year degree
5 = 4-year college graduate
6 = More than 4-year college degree
8 = Multiple Mark
9 = Missing118 Q28. Are you of Hispanic or Latino origin or decent? 1 = Yes, Hispanic or Latino
2 = No, not Hispanic or Latino
8 = Multiple Mark
9 = Missing119 Q29a. What is your race? Mark one or more. White 0 = Not Selected
1 = Selected120 Q29b. What is your race? Mark one or more. Black or African American 0 = Not Selected
1 = Selected121 Q29c. What is your race? Mark one or more. Asian 0 = Not Selected
1 = Selected122 Q29d. What is your race? Mark one or more. Native Hawaiian or Other Pacific Islander 0 = Not Selected
1 = Selected123 Q29e. What is your race? Mark one or more. American Indian or Alaska Native 0 = Not Selected
1 = Selected124 Q29f. What is your race? Mark one or more. Other 0 = Not Selected
1 = Selected125 Q30. Did someone help you complete this survey? 1 = Yes
2 = No
8 = Multiple mark
9 = Missing126 Q31a. How did that person help you? Mark one or more. Read the questions to me 0 = Not Selected
1 = Selected127 Q31b. How did that person help you? Mark one or more. Wrote down the answers I gave 0 = Not Selected
1 = Selected128 Q31c. How did that person help you? Mark one or more. Answered the questions for me 0 = Not Selected 1 = Selected 129 Q31d. How did that person help you? Mark one or more. Translated the questions into my language 0 = Not Selected
1 = Selected130 Q31e. How did that person help you? Mark one or more. Helped in some other way 0 = Not Selected
1 = SelectedAppendix F - IPOS Assessment File Layout (Palliative Care)
- Data file must be in text file format. Fields should be left justified and blank filled for the column width. Each row should be 82 columns in length.
- All fields are required. For item 10, if there is more than one selection, use the additional fields to record all responses. If there is only one response, additional fields should be left blank.
- Each assessment should be a unique row in the file.
Column Placement Variable Description Value Labels Details/Comments 1-2 PPS ID 2 Characters Adirondack Health Institute = 23
Community Partners of Western New York = 46
Central New York Care Collaborative = 08
Alliance for Better Health = 03
Community Care of Brooklyn = 33
Leatherstocking Collaborative Health Partners = 22
One City Health = 52
Staten Island PPS = 43
New York Presbyterian Hospital PPS = 39
New York-Presbyterian Queens PPS = 40
Care Compass Network = 443-32 Practice Site or Facility Name 30 Characters 33-42 Unique Patient Identification # 10 Characters Unique patient identification indicator (such as medical record number) 43-50 Assessment Date 8 Characters mmddyyyy (do not include dashes or slashes), 99999999 if missing 51 Setting 1 Character Office = 1, Nursing home = 2 52 Assessment Type 1 Character Initial = 1
Change = 2
Routine = 353 Insurance Type 1 Character Commercial only = 1
Medicaid only = 2
Medicare only = 3
Uninsured = 4
Medicaid and Medicare = 5
Medicaid and Commercial = 6
Medicaid, Medicare and Commercial = 754 Survey Version 1 Character Patient = 1
Staff = 2
Other = 3 (for use in IPOS-Dem version)55 Question 2 (pain) Score 1 Character Score 0-4 56 Question 2 (pain) Intervention Indicator 1 Character Yes = 1,
No = 057-58 Question 2 (symptoms) Count 2 Characters SUM OF all symptom related questions* (excluding pain symptom question) that have a score of 2, 3, or 4
Must report using leading zero for values less than ten
*IPOS Staff Survey includes symptom questions related to: shortness of breath, weakness or lack of energy, nausea, vomiting, poor appetite, constipation, sore or dry mouth, drowsiness, poor mobility.
IPOS Patient Survey includes symptom questions related to: shortness of breath, weakness or lack of energy, nausea, vomiting, poor appetite, constipation, sore or dry mouth, drowsiness, poor mobility.
IPOS Dem Survey (Non-Responsive Patients) includes symptom questions related to: shortness of breath, weakness or lack of energy, nausea, vomiting, poor appetite, constipation, dental problems, sore or dry mouth, drowsiness, poor mobility, swallowing problems, skin breakdown, difficulty communicating, sleeping problems, diarrhea, hallucinations, agitation, wandering.59-60 Question 2 (symptoms) Intervention Count 2 Characters SUM OF all symptom related questions* (excluding pain symptom question) that have a score of 2, 3, or 4
AND indicate "yes" for intervention offered/provided by staff Must report using leading zero for values less than ten
*IPOS Staff Survey includes symptom questions related to: shortness of breath, weakness or lack of energy, nausea, vomiting, poor appetite, constipation, sore or dry mouth, drowsiness, poor mobility.
IPOS Patient Survey includes symptom questions related to: shortness of breath, weakness or lack of energy, nausea, vomiting, poor appetite, constipation, sore or dry mouth, drowsiness, poor mobility.
IPOS Dem Survey (Non-Responsive Patients) includes symptom questions related to: shortness of breath, weakness or lack of energy, nausea, vomiting, poor appetite, constipation, dental problems, sore or dry mouth, drowsiness, poor mobility, swallowing problems, skin breakdown, difficulty communicating, sleeping problems, diarrhea, hallucinations, agitation, wandering.61 Question 3 (worried) Score 1 Character Score 0-4 62 Question 3 (worried) Intervention Indicator 1 Character Yes = 1, No = 0 63 Question 4 (anxious) Score 1 Character Score 0-4 64 Question 4 (anxious) Intervention Indicator 1 Character Yes = 1, No = 0 65 Question 5 (depressed) Score 1 Character Score 0-4 66 Question 5 (depressed) Intervention Indicator 1 Character Yes = 1, No = 0 67 Question 6 Score (at peace) 1 Character Score 0-4 68 Question 6 (at peace) Intervention Indicator 1 Character Yes = 1, No = 0 69 Question 7 (share feelings) Score 1 Character Score 0-4 70 Question 7 (share feelings) Intervention Indicator 1 Character Yes = 1, No = 0 71 Question 8 (information)Score 1 Character Score 0-4 72 Question 8 (information) Intervention Indicator 1 Character Yes = 1, No = 0 73 Question 9 (practical problems) Score 1 Character Score 0-4 74 Question 9 (practical problems) Intervention Indicator 1 Character Yes = 1, No = 0 75 Question 10 (advance directives) Health Care Proxy 1 Character Yes = 1, No = 0 76 Question 10 (advance directives) Living Will 1 Character Yes = 1, No = 0 77 Question 10 (advance directives) Organ Donation 1 Character Yes = 1, No = 0 78 Question 10 (advance directives) Documentation of Oral Advance Directive 1 Character Yes = 1, No = 0 79 Question 10 (advance directives) None 1 Character Yes = 1, No = 0 80 Question 10 (advance directives) Cannot assess 1 Character Yes = 1, No = 0 81 Question 10 (advance directives) Intervention Indicator 1 Character Yes = 1, No = 0 82 Question 11 (how questionnaire was completed) On my own 1 Character Yes = 1, No = 0 83 Question 11 (how questionnaire was completed) With help from a friend or relative 1 Character Yes = 1, No = 0 84 Question 11 (how questionnaire was completed) With help from a member of staff 1 Character Yes = 1, No = 0 Appendix G - New York-Specific Measures
Screening for Clinical Depression and Follow Up Plan
Screening for Clinical Depression and Follow Up Plan
Description:
Percentage of Medicaid enrollees age 18 and older who were screened for clinical depression using a standardized depression screening tool, and if a positive screen, received appropriate follow-up care. The intention of the measure is to capture early identification and intervention for persons with positive scores on screening tools within the context of routine preventive care visits.
Definitions:
Screening
Completion of a standardized, validated clinical or diagnostic tool used to identify people at risk of developing or having a certain disease or condition. This measure looks for screening with a standardized tool being conducted in the practitioner´s office during preventive care or evaluation and management visits.Adult Standardized Screening tool (Ages 18 and older)
An assessment tool that has been normalized and validated for the adult population (e.g. Patient Health Questionnaire [PHQ-9], Beck Depression inventory [BDI or BDI-II], Mood Feeling Questionnaire [MFQ], Center for Epidemiologic Studies Depression Scale [CES-D], Depression Scale [DEPS], Duke Anxiety-Depression Scale [DADS], Geriatric Depression Scale [GDS], Hopkins Symptom Checklist [HSCL], Zung Self-Rating Depression Scale [SDS], Cornell Scale Screening, PRIME MD-PHQ-2, and Edinburgh Postnatal Depression Scale [EPDS]). Assessment tools may be named, or a complete tool may be embedded in the medical record and not named.Depression screen scoring
Standardized depression screening tools do not diagnose depression, but rather indicate whether or not there is a need for more detailed follow-up by a clinician. Standardized depression screening tools are typically scored, and the scoring includes established cut points for depression based on established sensitivity, specificity and positive and negative predictive values of the scores for detecting depression. Established scoring cut points for the most commonly used screens in primary care (PHQ) are detailed in Medical Record Specifications below.Follow Up Plan
Documentation of follow-up must include one or more of the following:
- Recommendation or prescription for an antidepressant medication in the 30-day period following the initial positive screen (inclusive of the screening visit date);
- Recommendation or referral for a follow-up visit with behavioral health provider in the 30-day period following the initial positive screen (inclusive of the screening visit date) or evidence of a follow-up visit with a behavioral health provider occurring in the 30-day period following the initial positive screen (inclusive of the screening visit date);
- Recommendation for or scheduling of a follow-up outpatient visit with any provider, including the PCP or other provider administering the original screen, for further assessment within 30 days of the positive screen (inclusive of the screening visit date);
- Further assessment on the same day of the positive screen which includes documentation of additional depression assessment indicating no depression (such as positive score from PHQ-2 with a negative PHQ- 9 or documented negative findings after further evaluation);
- Referral to emergency department for crisis services on the same day of the positive screen; or
- Arrangement for inpatient admission for mental health diagnosis on the same day as the positive screen.
Intake Period
July 1 of the prior year through June 1 of the measurement year.DSRIP Measurement Year July 1 of the prior year through June 30 of the current year. For example, measurement year 3 is July 1, 2016 to June 30, 2017.
Eligible Population
Product Line: Medicaid
Ages: 18 years or older as of July 1, the first day of the intake period. Report two age stratifications and a total result.
- 18 - 64 years
- 65 years and older
- Total
Continuous Enrollment: Continuous enrollment in Medicaid for the measurement year. The allowable gap is no more than one month during the measurement year.
Anchor Date: June 30 of the measurement year.
Event diagnosis: Members who had a qualifying outpatient visit during the intake period (listed in table CDF- A)
CDF-A: Qualifying outpatient visits
Coding System Qualifying Codes CPT 96150, 96151, 99201, 99202, 99203, 99204, 99205, 99212, 99213, 99214, 99215 HCPCS G0402, G0438, G0439, G0444
Denominator
A systematic sample drawn from the eligible population.
Required (listed in table CDF-B)
- Remove members with: A diagnosis of a depressive disorder in the year prior to the measurement year or an active diagnosis of depression during the measurement year but prior to the date of the first standardized screen in the measurement year. If there is no standardized screen in the measurement year, remove any member with an active diagnosis of depression at any time in the measurement year as confirmed by the medical record denominator exclusions.
- A diagnosis of Bipolar disorder in the year prior to the measurement year or prior to the date of the first standardized screen in the measurement year. If there is no standardized screen in the measurement year, remove any member with a diagnosis at any time in the measurement year as confirmed by the medical record denominator exclusions.
- A diagnosis of severe intellectual disability or dementia in the year prior or during the measurement year.
NOTE: Medical record confirmation of the diagnosis is not required in the measurement year or year prior.CDF-B: Diagnoses codes for exclusions
Diagnosis ICD-9-CM Codes ICD-10-CM Codes Depressive disorders 296.20-296.25,
296.30-296.35,
298.0, 300.4, 311F32.0-F32.4, F32.9, F33.1-F33.41, F33.9, F34.0-F34.1, F34.8-F34.9 Bipolar disorder I or II 296.00-296.05,
296.10-296.15,
296.40-296.45,
296.50-296.55,
296.60-296.65,
296.7F30.10-F30.13, F30.2, F30.3, F30.8, F30.9, F31.10-F31.13, F31.2, F31.30-F31.32, F31.4, F31.5, F31.60-F31.64, F31.70-F31.77, F31.81, F31.89, F31.9 Severe/profound intellectual disability 318.1-318.2 F72-F73 Vascular dementia with behavioral problems 290.40 F01.51 Dementia in other diseases classified elsewhere with behavioral disturbance 294.11 F02.81
Numerator
Members who were screened for clinical depression with a standardized tool in the measurement year and if positive, had appropriate follow-up care within 30 days (inclusive) of the positive result.
Administrative Specifications
Administrative Denominator Exclusions (Prior MY only):
If the member has a diagnosis of depressive disorder, bi-polar, or severe physical/intellectual incapacity by diagnostic claim code (table CDF-B) in the year prior to the measurement year, the member can be excluded, and the claim does not need to be validated by medical record review.
Administrative Compliance (During the MY only):
HCPCS Code Description G8431 Screening for clinical depression is documented as positive and follow-up plan is documented G8510 Screening for clinical depression is documented as negative; a follow-up plan is not required NOTE: Although medical record documentation need not be reviewed if administrative specification criteria are met for numerator compliance, the PPS should ensure appropriate use of the HCPCS G8431 and G8510 codes by their providers. As providers are encouraged to use the HCPCS codes to allow monitoring of improvement in administrative data, the PPS needs to ensure that the coding is associated with the standardized depression tools, scoring and follow-up documentation as defined and specified in this measure.
Medical Record Specifications
Medical Record Denominator Exclusions (During the MY only):
If there is no exclusion diagnosis (i.e., depressive disorder, bi-polar, or severe intellectual/physical incapacity) by diagnostic claim code (table CDF-B) in the year prior to the measurement year, the medical record for all qualifying visits for the measurement year must be reviewed.
- If there is an exclusion diagnosis by diagnostic claim code in the measurement year, the medical record must be reviewed to validate the documentation of the diagnosis in the medical record. The member is excluded if:
- the date of the diagnosis documented in the medical record precedes the date of the first documented standardized screen in the measurement OR
- there is no documented screening in the medical record and the diagnosis is documented at any time in the measurement year.
- If the first screening documented in the medical record in the measurement year precedes the documented diagnosis (or is for the same date as the diagnostic claim), the screening documentation must be reviewed for numerator compliance, rather than exclusion.
- If there is no documented diagnosis and no documented standardized screening in the medical record during the measurement year, i.e., the diagnostic claim cannot be validated, the record is non- compliant rather than excluded.
Required Denominator Exclusions
Remove members with medical record documentation of:
- Any history of bipolar disorder or diagnosis of an active depressive disorder during the measurement year but prior to the date of the first standardized screen in the measurement year. Active diagnosis is defined as a diagnosis that is documented on the patient´s problem list, a relevant diagnosis code is listed on the encounter, or the diagnosis is documented in a progress note indicating that the patient is being treated or managed for the depression. Evidence of management does not require medication management but may include it. If there is no standardized screen in the measurement year, remove any member with a diagnosis of bipolar disorder or depressive disorder at any time in the measurement year. Diagnoses of depressive disorders include major depressive disorder (MDD), persistent depressive disorder (dysthymia), or unspecified depressive disorder.
- Severe mental and/or physical incapacity where the person is unable to express himself/herself in a manner understood by others. Examples include members with delirium or severe cognitive impairment.
Numerator
The following steps are used to determine numerator component compliance and will be used in the calculation of numerator events:Step 1
Review all qualifying visits within the intake period to determine if a standardized depression screen was conducted. If the member has qualifying visits with more than one provider, records from each of the applicable providers can be used in the review. Primary care provider records should be prioritized in chase logic. Additionally, information from all visits with the providers associated with at least one qualifying visit can be included in the review. For example, if the member had three visits with a provider in the intake period and two of the three are not a qualifying visit, information from the two non-qualifying visits can be included in the review for standardized screening. Visits with providers that are not associated with at least one qualifying visit cannot be included in the review.Step 2
Identify all of the members with a standardized screening tool documented during the intake period. If a member has more than one visit with a standardized screen during the intake period, use the result from the first date. Members with one or more completed standardized screening tools are compliant for numerator component 1.Step 3
For all the members with a documented screening, determine the result of the screening. Identify members whose result is negative by: 1) Clinician documentation that screening results are negative, or, if there is no clinician documentation of screening results; 2) Negative screening score using the cut point criteria specified for the tool. Members who screen negative are compliant for numerator component 2.Negative screens for PHQ tools:
- PHQ-9: A member with a PHQ-9 score < 5 is considered to have screened negative for depression.
- PHQ-2 with numeric scale: A member with a PHQ-2 score < 3 when a scored PHQ-2 instrument is used is considered to have screened negative for depression.
- PHQ-2 without a numeric scale: A member who answers "no" to both of the two questions is considered to have screened negative for depression.
Step 4
For all the members with a documented screening, determine the result of the screening. Identify members whose result is positive by: 1) Clinician documentation that screening results are positive, or, if there is no clinician documentation of screening results; 2) Positive screening score using the cut point criteria specified for the tool. Members who screen positive are compliant for numerator component 3.Positive screens for PHQ tools:
- PHQ-9: A member with a PHQ-9 score ≥ 5 is considered to have screened positive for depression.
- PHQ-2 with numerical scale: A member with a PHQ-2 Score ≥ 3 when a scored PHQ-2 instrument is used is considered to have screened positive for depression.
- PHQ-2 without numerical scale: A member who answers "yes" to either of the two questions is considered to have screened positive for depression.
Step 5
For all of the members from Step 4, count members for whom follow-up care was provided within 30 days (inclusive) of the date of the positive screen. Members who have documented follow-up plans are compliant for numerator component 4.Follow up documentation must include one or more of the following:
- Recommendation or prescription for an antidepressant medication in the 30-day period following the initial positive screen (inclusive of the screening visit date);
- Recommendation or referral for a follow-up visit with behavioral health provider in the 30-day period following the initial positive screen (inclusive of the screening visit date) or evidence of a follow-up visit with a behavioral health provider occurring in the 30-day period following the initial positive screen (inclusive of the screening visit date);
- Recommendation for or scheduling of a follow-up outpatient visit with any provider, including the PCP or other provider administering the original screen, for further assessment within 30 days of the positive screen (inclusive of the screening visit date);
- Further assessment on the same day of the positive screen which includes documentation of additional depression assessment indicating no depression (such as positive score from PHQ-2 with a negative PHQ-9 or documented negative findings after further evaluation);
- Referral to emergency department for crisis services on the same day of the positive screen; or
- Arrangement for inpatient admission for mental health diagnosis on the same day as the positive screen.
Step 6
Sum the total of the members compliant with numerator component 1 AND 2 (screened negative) and with numerator component 1 AND 3 AND 4 (screened positive with documented follow-up plan) for the total numerator events.Numerator Events = Screened negative (members compliant with both Numerator components 1 and 2) + Screened positive with documented follow-up plan (members compliant with Numerator components 1, 3 and 4)
References
American Psychiatric Association. DSM V Implementation and Support. Available here. Accessed May 9, 2016
Centers for Medicare and Medicaid Services (CMS). Decision Memo for Screening for Depression in Adults (CAG-00425N). October 14, 2011. Retrieved here.
Institute for Clinical Systems Improvement. Depression, Adult in Primary Care. Guideline Summary March 2016. Retrieved here.
Instruction Manual. Instructions for Patient Health Questionnaire (PHQ and GAD-7 Measures. (n.d.) Retrieved here.
Maurer DM. Screening for Depression, 2012. Retrieved from American Family Physician website, American Academy of Family Physicians at www.aafp.org/afp.
National Quality Forum. #0418 Preventive Care and Screening: Screening for Clinical Depression and Follow-Up Plan. Retrieved here.
O´Connor E, Rossom RC, Henninger M, Groom HC, Burda BU, Henderson JT, Bigler KD, Whitlock EP. Screening for Depression in Adults: An Updated Systematic Evidence Review for the U.S. Preventive Services Task Force. Evidence Synthesis No. 128. AHRQ Publication No. 14-05208-EF-1. Rockville, MD: Agency for Healthcare Research and Quality; 2016.
Pignone MP, Gaynes BN, Rushton JL, et al. Screening for depression in adults: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med 2002 May 21; 136(10):765-76. PMID: 12020146.
Siu AL and the U.S. Preventive Services Task Force (USPSTF). Screening for Depression in Adults: US Preventive Services Task Force Recommendation Statement. JAMA 2016; 315(4):380-387. Retrieved here.
U.S. Preventive Services Task Force (USPSTF). Clinical Summary: Depression in Adults: Screening. October 2014. Retrieved here.
Screening for Clinical Depression and Follow Up flow chart
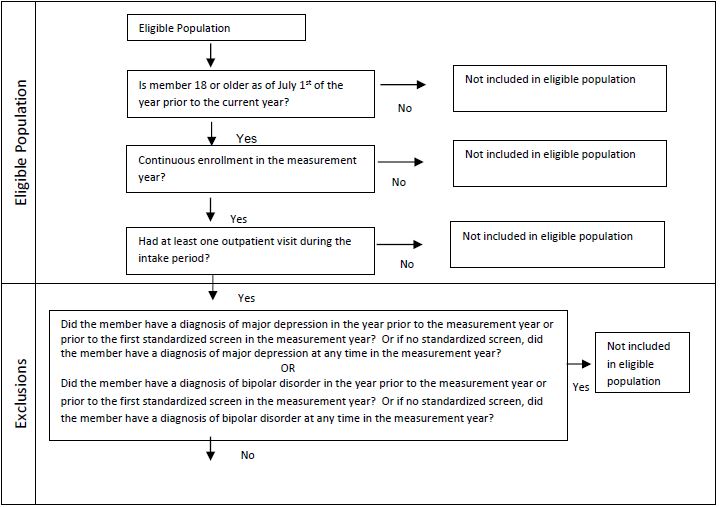
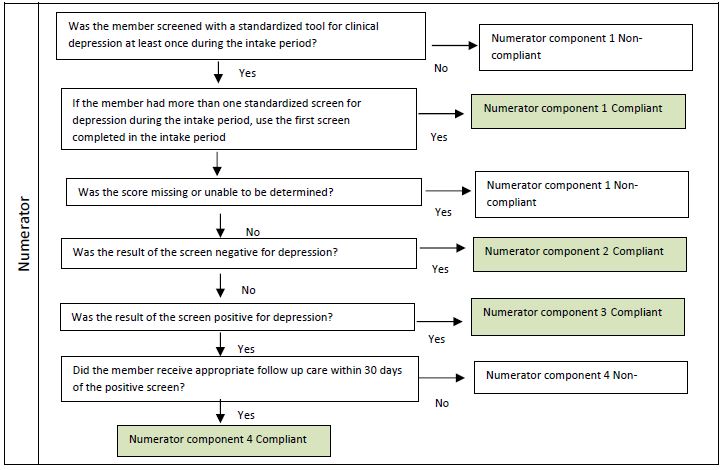
Additional Notes on documentation of screening and results:
Use of standardized tools embedded in forms or electronic medical records -
If all of the questions and response categories from a standardized screening tool are used within medical records that allow the same consistency of creating a score for determining positive and negative results, the information would be acceptable evidence of numerator compliance whether the name of the tool is present or not. The key requirements for numerator compliance are:
- All questions from a standardized tool are included
- Same standardized tool response options are available
- Documented score or finding of negative or positive screen
- Follow up plan documented if positive
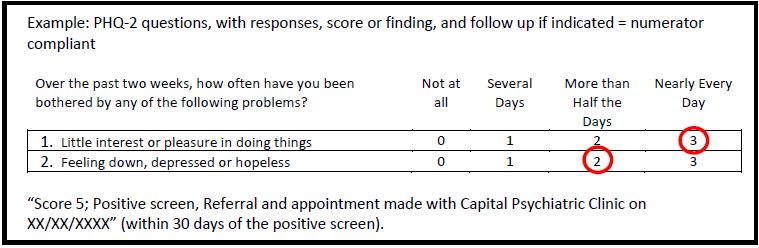
Use of Summary of Findings from Standardized tools -
Documentation that indicates a standardized tool was used for screening for clinical depression with a score, and if the score indicates a positive screen, the follow-up plan is documented.Example: Standardized tool completed, with score or finding and follow-up if indicated = numerator compliant
"PHQ-2 assessment completed, negative screen. No follow-up indicated"Use of Summary of Findings from Symptom Queries -
Documentation about findings from queries or discussion without specific questions from a standardized tool or score is NOT numerator compliant.Example: No indication of tool, or finding, or general query statements = numerator non-compliant
"depression screening negative" or "depression screen done" or "denies depression"Viral Load Suppression
Viral Load Suppression
Description:
The percentage of Medicaid enrollees who qualified through at least one method as living with HIV/AIDS during the year prior to the measurement year who had an HIV viral load less than 200 copies/mL at the last HIV viral load test during the measurement year.
Definitions:
HIV Viral Load: The HIV viral load is the number of copies of the human immunodeficiency virus (HIV) in the blood or bodily fluid.
HIV Viral Load Test: The HIV viral load test measures the number of HIV copies in a milliliter of blood.
DSRIP Measurement Year: July 1 of the prior year through June 30 of the current year. For example, measurement year 1 is July 1, 2014 to June 30, 2015.
Eligible Population:
Product Line: Medicaid
Ages: All members of the eligible population ages 2 and older as of June 30 of the measurement year.
Continuous Enrollment: 12 months of continuous enrollment for the measurement year. The allowable gap is no more than one month during the measurement year.
Anchor Date: June 30 of the measurement year.
Index Episode Event: Identify members as having HIV or AIDS who met at least one of the following criteria during the year prior to the measurement year with at least one of the 4 methods listed below:
Method 1: At least one acute inpatient encounter (Acute Inpatient Value Set) with a diagnosis of HIV (HIV Value Set) or an inpatient DRG for HIV during the year prior to the measurement year (Table HIV-A)
Table HIV-A: Inpatient DRG and Diagnosis Codes for HIV and AIDS
Description NYS APRDRG Codes MS DRG Codes Inpatient DRG 890, 892, 893, 894 (all severity levels included) 969-970, 974-977
Description ICD 9 CM ICD 10 CM Codes Diagnosis Codes with CPT 042, V08 B20, Z21 WITH 99221-99223, 99231-99233, 99238, 99239, 99251-99255, 99291 Diagnosis Codes with Revenue 042, V08 B20, Z21 WITH 010x, 0110-0114, 0119, 0120-0124, 0129, 0130-0134, 0139, 0140-0144, 0149, 0150- 0154, 0159, 016x, 020x, 021x, 072x, 080x, 0987 Method 2 At least one outpatient visit (Ambulatory Visits Value Set/ Table HIV-C), with a primary or secondary diagnosis indicating HIV/AIDS (HIV Value Set/ Table HIV-B).
Table HIV-B: Diagnosis Codes for HIV and AIDS
Description ICD 9 CM Diagnosis ICD 10 CM Diagnosis HIV/AIDS 042, V08 B20, Z21 Table HIV-C: Codes to Identify Outpatient and ED Visits
Description CPT HCPCS UB Revenue ICD 9 CM Diagnosis ICD 10 CM Diagnosis Outpatient Visit 99201-99205,
99211-99215,
99241-99245,
99341-99345,
99347-99350,
99381-99387,
99391-99397,
99401-99404,
99411, 99412,
99429G0402,
G0438,
G0439,
G0463051x, 0520-
0523, 0526-
0529, 0982,
0983V20.2, V70.0,
V70.3, V70.5,
V70.6, V70.8,
V70.9Z00.00, Z00.01,
Z00.121, Z00.129,
Z00.5, Z00.8,
Z02.0-Z02.6,
Z02.71, Z02.79,
Z02.81-Z02.83,
Z02.89, Z02.9ED Visit 99281, 99282, 99283, 99284, 99285 450, 451, 452 Method 3 At least one ED Visit (ED Value Set/ Table HIV-C), with a primary or secondary diagnosis indicating HIV/AIDS (HIV Value Set/ Table HIV-B).
Method 4 At least one dispensing event for ARV medications (Table HIV-D) during the year prior to the measurement year AND without a primary or secondary diagnosis of Hepatitis B or HTLV-1 (Table HIV-F) in any setting (Acute Inpatient Value Set, Ambulatory Visits Value Set, Table HIV-A, and Table HIV-C). Members identified as having HIV/AIDS because of at least one dispensing event, where Truvada (Tenofovir disoproxil fumarate + emtricitabine or TDF/FTC), Viread, Vemlidy, Emtriva, Descovy, Retrovir, Epivir, or Combivir was dispensed or Isentress or Tivicay when used with one or more of the above, must also have at least one diagnosis of HIV/AIDS (HIV Value Set / Table HIV-B) during the year prior to the measurement year. A dispensing event is one prescription of an amount lasting 30 days or less. To convert dispensing events for prescriptions longer than 30 days, divide the days´ supply by 30 and round down.
Table HIV-D: An excel file with NDC Codes to Identify Antiretroviral Medications is available here.
Table HIV-E: An excel file with NDC Codes to Identify HIV Antiretroviral Diagnosis is available at: here.
Table HIV-F: Diagnosis Codes for Hepatitis B or HTLV 1
Description ICD 9 CM Diagnosis ICD 10 CM Diagnosis Hepatitis B 070.20, 070.21, 070.22, 070.23, 070.30, 070.31, 070.32, 070.33, V02.61 B16.0., B16.1, B16.2, B16.9, B17.0, B18.0, B18.1, B19.10, B19.11, Z22.51 HTLV 1 079.51 B97.33 Denominator
A systematic sample drawn from the eligible population.
Denominator Required Exclusions
Medical record
Any member found to be HIV negative during the measurement year or the year prior.
- Evidence for determining HIV negative status include: negative diagnostic test results such as HIV Antibody test results or HIV rapid test results, documentation in the medical record of HIV negative status, or provider attestation of HIV negative status for the member. Statements such as "rule out HIV," "possible HIV", "questionable HIV" are not sufficient to confirm the diagnosis if such statements are the only notations of HIV in the medical record.
- Evidence must be dated for the measurement year or year prior. If the documentation is for the year prior, there must not be any further documentation of HIV positive status after the negative notation. For example, a member with a negative HIV test in the year prior must have the documentation for the measurement year reviewed for indication of no more recent HIV test or status. Documentation of the negative HIV status must be before June 30 of the measurement year.
- Attestations may be obtained from providers after the measurement year, as long as the document specifies the member´s HIV negative status for the measurement year or the year prior. Attestations from providers must be from the providers associated with the member´s health care. Obtaining attestations from all involved providers is necessary to ensure that the appropriate providers associated with the diagnosis are the ones attesting to the HIV negative status.
- Exclude from the eligible population all members who had a nonacute inpatient admission during the measurement year.
Numerator
The number of Medicaid enrollees in the denominator with a HIV viral load less than 200 copies/mL for the most recent HIV viral load test during the measurement year.
Medical Record Specifications
Numerator: The following steps are used to determine numerator compliance:
Step 1:
Review all medical record documentation for visits during the measurement year to determine dates of viral load testing.Step 2:
If there is more than one viral load test during the measurement year, determine the most recent viral load test in the measurement year.Step 3:
Determine the viral load level from the most recent viral load test during the measurement year. Results for particular assays may need to be converted to determine if the result equates to below 200 copies/mL (such as log-10 results).
- Test results indicating viral load levels of less than 200 copies/mL; or
- Documentation of levels less than 200 copies/mL with the test date.
Step 4: Sum the total of members identified in Step 3 for the total numerator events.
NOTE: Members without a viral load test during the measurement year or missing the result for the most recent test in the measurement year are numerator non-compliant.
Viral Load Suppression flow chart
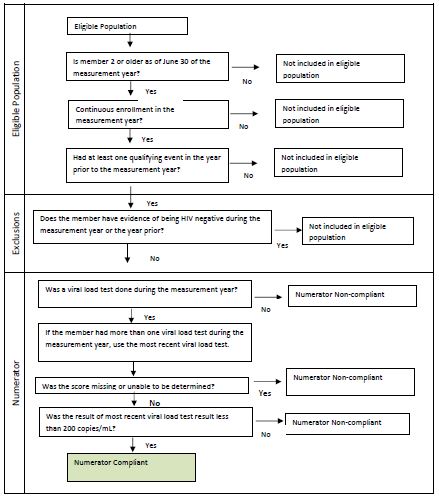
Emergency Department Use by the Uninsured
Emergency Department Use by the Uninsured ±
Description:
The percentage of emergency department visits during the measurement year for individuals who are uninsured at the time of the visits.
Purpose: Increasing health insurance coverage among those who are uninsured can increase access to medical care, improve one´s health status, and reduce the burden of medical costs on the patient. 1
Data Source: New York State SPARCS Outpatient file
Eligible Population: Patients with emergency department visits at hospitals (Article 28) participating in a Performing Provider System (PPS) network
Denominator Description: Emergency department visits that do not result in an inpatient admission
Denominator Exclusions: Emergency department visits for out of state residents are excluded
Numerator Description: The emergency department visits among individuals with self-pay payer typology (i.e., first digit=´8´; excluding ‘822´, ‘823´, and ‘85´) in any of the all payer typology fields
Numerator Exclusions: not applicable
Ratio: The ratio is calculated by dividing the current year measure result by the baseline measure result on an annual basis
± A lower rate is desirable.
Meaningful Use Certified Providers
Meaningful Use Certified Providers who have a Participating Agreement; and Meaningful Use Certified Providers Who Conduct Bidirectional Exchange (two measures)
Description:
The percentage of Meaningful Use certified providers who are identified in the measurement year data file as having:
Participating Agreement - a participating agreement with at least one Qualified Entity (RHIO)
Bidirectional Exchange - evidence they conduct bidirectional exchange using the Statewide Health Information Network for New York (SHIN-NY)* with at least one Qualified Entity (or RHIO).
Purpose:
Increasing the number of eligible providers who participate with Qualified Entities and adopt, implement, upgrade, or demonstrate meaningful use of certified electronic health record (EHR) technology improves the quality, safety, and efficiency of care while reducing disparities; promotes public and population health; improves care coordination; and promotes the privacy and security of patient information.
Data Source: Data files submitted by the Qualified Entities in New York State
Eligible Population: Providers who are participating in a Performing Provider System (PPS) who are Meaningful Use certified (able to use electronic health record technology)
Participating Agreement
Denominator Description: Number of providers who are Meaningful Use certified who are participating in a PPS
Denominator Exclusions: Providers who are not Meaningful Use certified
Numerator Description: Number of providers who have signed a participation agreement with at least one Qualified Entity
Numerator Exclusions: not applicable
Bidirectional Exchange
Denominator Description: Number of providers who are Meaningful Use certified who are participating in a PPS
Denominator Exclusions: Providers who are not Meaningful Use certified
Numerator Description: Number of providers who conduct bidirectional exchange by meeting both criteria: 1) make data available and 2) access data using the Statewide Health Information Network for New York (SHIN-NY) with at least one Qualified Entity
Numerator Exclusions: not applicable
* The SHIN-NY is a "network of networks" that links New York´s eight regional Qualified Entities (QEs) throughout the state. Each Qualified Entity (or RHIO - Regional Health Information Organization) operates its own network that collects electronic health records from participating providers.
Primary Care Providers meeting PCMH or APC Standards
Primary Care Providers Meeting Patient Centered Medical Home or Advanced Primary Care Standards
Description:
The percentage of primary care providers meeting Patient Centered Medical Home (PCMH) (NCQA) or Advanced Primary Care Standards (as developed under the NYS Health Innovation Plan (SHIP)) during the measurement year.
Purpose:
Patient centered medical home and advanced primary care are promising models for transforming the organization and delivery of high-quality primary care for all Medicaid members. Increasing the implementation of PCMH and advanced primary care has many benefits including, but not limited to, better coordinated and personalized care, improved access to medical care, improved health outcomes, especially for patients who have chronic conditions, increased provider satisfaction and efficient, cost-effective care.
Data Source: Provider Network Data System (PNDS), NCQA PCMH Certification File, and APC status file (as developed under SHIP)
Eligible Population: Primary care providers participating in a PPS network
Denominator Description: The number of primary care providers in the PPS network
Denominator Exclusions: Large medical groups or clinics that are categorized by an organizational National Provider Identifier (NPI)
Numerator Description: The number of primary care providers meeting patient centered medical home or advanced primary care standards using any level and any standard year
Numerator Exclusions: not applicable
Non-Use of Primary and Preventive Care
Non-use of Primary and Preventive Care ±
Description:
The percentage of attributed members with no evidence of primary care or preventive care services in the measurement year.
Purpose:
Improving health care services depends in part on ensuring that people have a usual and ongoing source of care. People with a usual source of care have better health outcomes and fewer disparities and costs.1
Data Source: Medicaid Data Warehouse (MDW)
Eligible Population: The attributed population in the measurement year
Denominator Description: All PPS attributed members as of June 30th of the measurement year, who meet continuous enrollment and age criteria for the Adult Access to Preventive or Ambulatory care and Children´s Access to Primary Care measure specifications
Denominator Exclusions: Members eligible for Medicaid and Medicare (dual) at any time in the measurement year
Numerator Description: The percentage of attributed members who do not have at least one service with a preventive services CPT or equivalent code in the measurement year. The preventive services CPT or equivalent codes included in this measure are available in the HEDIS 2019 Technical Specifications Manual. This measure references the same code sets called out in the HEDIS value sets for "Adult Access to Ambulatory Care (AAP)" and "Children´s Access to Primary Care (CAP)".
Numerator Exclusions: not applicable
Ratio: The ratio is calculated by dividing the current year measure result by the baseline measure on an annual basis.
± A lower rate is desirable.
Medicaid ER and Inpatient Spending
Medicaid Spending on Emergency Room and Inpatient Services ±
Description:
Total Medicaid spending on emergency room (ER) and inpatient (IP) services during the measurement year per PPS attributed member per month.
Purpose:
The Affordable Care Act2 is working to improve quality and lower health care costs. The sources of inefficiency that are leading to increasing health care costs include payment for emergency room and inpatient care, and a lack of focus on disease prevention and engaging patients in primary care.Data Source: Medicaid Data Warehouse
Eligible Population: All attributed members in the measurement year
Denominator Description: Total months enrolled in Medicaid (Member Months) for members attributed to the PPS as of June 30th of the measurement year
Denominator Exclusions: Members eligible for Medicaid and Medicare (dual) at any time in the measurement year.
Numerator Description: Total Medicaid amount paid for ER and IP services in the measurement year for the PPS attributed members
Numerator Exclusions: not applicable
± A lower rate is desirable.
Medicaid Primary Care and Community Based Behavioral Healthcare
Medicaid Spending on Primary Care and Community Based Behavioral Health Care
Description:
Total spending on primary care (PC) and community behavioral health care (CBHC) during the measurement year per PPS attributed member per month.
Purpose:
The Affordable Care Act2 is working to improve quality and lower health care costs. Important to this effort are primary care providers and the integration of physical health and behavioral health services.
Data Source: Medicaid Data Warehouse
Eligible Population: All attributed members in the measurement year
Denominator Description: Total time enrolled in Medicaid (Member Months) for members attributed to the PPS as of June 30th of the measurement year
Denominator Exclusions: Members eligible for Medicaid and Medicare (dual) at any time in the measurement year
Numerator Description: Total paid amount for PC and CBHC services in the measurement year for the PPS attributed members
Numerator Exclusions: not applicable
Care Transition-Hospital Consumer Assessment of Healthcare Providers and Systems Survey
Care Transition - Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) Survey
Description: HCAHPS is a national, standardized survey of hospital patients about their experiences during a recent inpatient hospital stay.
The HCAHPS Care Transition composite is identified by H_COMP_7 and is reported as the sum of the "top-box" and "middle-box" responses. The "top-box" scores, represented by the variable H_COMP_7_SA, consist of the most positive responses to the Care Transition Survey Questions, in this case the most positive response would be "Strongly Agree". The "middle-box" scores, H_COMP_7_A, contain the intermediate responses or "Agree" to the question. More information about HCAHPS "Boxes" can be found under the Summary Analyses section of the HCAHPS Web site at www.hcahpsonline.org.
The Care Transition composite (H-COMP_7) includes the following HCAHPS survey questions, but the result that is available is a percentage of positive (both Strongly Agree and Agree) responses:
- During this hospital stay, staff took my preferences and those of my family or caregiver into account in deciding what my health care needs would be when I left.
- When I left the hospital, I had a good understanding of the things I was responsible for in managing my health.
- When I left the hospital, I clearly understood the purpose for taking each of my medications.
Purpose: Improved patient satisfaction leads to an enhanced patient experience and is associated with improved treatment outcomes.3 Measuring patients´ perceptions of their hospital experience provides useful information for identifying gaps and developing effective action plans for quality improvement in healthcare organizations.
Data Source: Centers for Medicaid and Medicare (CMS) website.
- Select the Hospital file
- Filter by state (NY) and HCAHPS Measure ID (H_COMP_7_A and H_COMP_7_SA)
- HCAHPS scores are based on four consecutive quarters of patient surveys, which are publicly reported on the website four times each year, with the oldest quarter of surveys rolling off as the newest quarter rolls on.
- Use the previous rolling year time period for each measurement year (i.e., MY2 uses 4/1/2015- 3/31/2016; MY3 uses 4/1/2016-3/31/2017; MY4 uses 4/1/2017-3/31/2018; MY5 uses 4/1/2018- 3/31/2019).
Eligible Population: Hospitals participating in a PPS network
Measure Result Description: Mean of all the hospital percentages by PPS.
Exclusions: Hospitals that did not have a completed survey for the reporting period. Hospitals that had too few cases/patients to report for Care Transition questions 23, 24 or 25.
Other NYS Specific Measures
Other NYS Specific Measures
- Medicaid Provider Reimbursement with Methods other than Fee-for-Service (FFS): This non-FFS measure, "Percent of total Medicaid provider reimbursement received through sub-capitation or other forms of Non-FFS reimbursement" is in development in alignment with Value-Based Purchasing (VBP) and financial sustainability elements in the DSRIP program and in coordination with the VBP workgroup and VBP Roadmap. It is expected the Non-FFS measure baseline data collection will begin following CMS approval of the VBP Roadmap. NY DSRIP VBP resources are available here.
- HIV/AIDS Comprehensive Care: Engaged in Care, Viral Load Monitoring and Syphilis Screening - See 2019 QARR Technical Specifications Manual
- Palliative Care measure specifications were approved by the Centers for Medicare and Medicaid Services (CMS) in August 2016. Palliative care measures were implemented in MY3 as of January 2017.
- Patient Activation Measure (PAM) metrics were officially approved following CMS´ acceptance of the program´s amended Attachment I on January 19, 2016.
_________________________________
1. Healthy People.gov (see Access to Health Services) 1
2. Key Features of the Affordable Care Act 2
3. Patients´ Perception of Hospital Care in the United States 3
Follow Us