DSRIP Frequently Asked Questions (FAQs)
A. Medicaid Redesign Team (MRT) Background
A1. Q: What is the MRT Waiver Amendment?
A: The MRT Waiver Amendment will allow the state over five years to reinvest $8 billion in federal savings generated by Medicaid Redesign Team (MRT) reforms to implement an action plan to save and transform the state´s health care system, bend the Medicaid cost curve, and assure access to quality care. The $8 billion reinvestment will be allocated in the following ways:
- $500 Million for the Interim Access Assurance Fund - temporary, time limited funding to ensure current trusted and viable Medicaid safety net providers can fully participate in the DSRIP transformation without unproductive disruption
- $6.42 Billion for Delivery System Reform Incentive Payments (DSRIP) - including DSRIP Planning Grants, DSRIP Provider Incentive Payments, and DSRIP Administrative costs
- $1.08 Billion for other Medicaid Redesign purposes - this funding will support Health Home Development through a State Plan Amendment, and investments in long term care workforce and enhanced behavioral health services through managed care contract payments
A2. Q: How does the Waiver Amendment relate to the Medicaid Redesign Team?
A: Established by Governor Cuomo in January 2011, the MRT brought together stakeholders and experts from throughout the state to work cooperatively to both reform New York State´s health care system and reduce costs. The MRT was charged with addressing underlying health care cost and quality issues in New York´s Medicaid program to create a first year Medicaid budget proposal, as well as develop a multiyear reform plan.
The MRT waiver amendment is an agreement that allows the state to reinvest over a five-year period $8 billion of the $17.1 billion in federal savings generated by MRT reforms. This reinvestment will lead to system transformation that will preserve essential safety net providers across the state and increase access for all New Yorkers to high-quality health care.
The MRT waiver amendment will enable New York to fully implement the groundbreaking MRT action plan to permanently restructure our health care system and continue to make New York a national model.
|back to table of contents||top of section| |top of page|
B. DSRIP Background
B1. Q: What is DSRIP?
A: The Delivery System Reform Incentive Payment (DSRIP) program is the main mechanism by which New York State will implement the Medicaid Redesign Team (MRT) Waiver Amendment.
DSRIP´s purpose is to fundamentally restructure the health care delivery system by reinvesting in the Medicaid program, with the primary goal of reducing avoidable hospital use by 25% over 5 years. Up to $6.42 billion from the MRT Waiver Amendment has been allocated to this program with payouts based upon achieving predefined results in system transformation, clinical management and population health.
B2. Q: What is considered avoidable hospital use?
A: Avoidable hospital use encompasses not only avoidable hospital readmissions, but also inpatient admissions that could have been avoided if the patient had received proper preventive care services. The following four measures will be used to evaluate DSRIP´s success in reducing avoidable hospital use:
- Potentially Preventable Emergency Room Visits (PPVs),
- Potentially Preventable Readmissions (PPRs),
- Prevention Quality Indicators- Adult (PQIs),
- Prevention Quality Indicators- Pediatric (PDIs).
B3. Q: How does the Statewide Health Innovation Plan (SHIP) relate to DSRIP?
A: SHIP and DSRIP can be considered synergistic. SHIP focuses on leveraging the work done with the state on the Patient Centered Medical Home (PCMH) by all payers, as well as the HIT connectivity being built through the Statewide Health Information Network of New York (SHIN-NY). In this context, SHIP will focus, in part, on building the Advanced Primary Care Model from the work done on the PCMH, building the All Payer Database to further build the analytics on health care in New York State, and enhancing the reach and utilization of the SHIN-NY to enhance the coordination and transparency of health care. With these three key pieces in place, quality of care can be monitored more efficiently and effectively, allowing payment reform to focus on payment for outcomes/payment for performance, one other key goal of SHIP.
Please review the SHIP documents on the NYS DOH website for additional details.
B4. Q: Where can I get information on DSRIP?
A: The state will provide information through three venues:
- The DSRIP website.
- The state utilizes a listserv to notify interested parties of updates including webinars.
- In addition, there is a dedicated DSRIP email to which questions can be submitted.
B5. Q: Is there a DSRIP program timeline available?
A: Yes, it is available on the DSRIP website.
B6. Q: How long does the DSRIP program last? What´s a DSRIP year?
A: The DSRIP program is a 5 year program; however, it included one year for planning. The years are structured as follows:
- DSRIP Year 0 (DY0): April 14, 2014 - March 31, 2015
- DSRIP Year 1 (DY1): April 1, 2015 - March 31, 2016
- DSRIP Year 2 (DY2): April 1, 2016 - March 31, 2017
- DSRIP Year 3 (DY3): April 1, 2017 - March 31, 2018
- DSRIP Year 4 (DY4): April 1, 2018 - March 31, 2019
- DSRIP Year 5 (DY5): April 1, 2019 - March 31, 2020
B7. Q. What was DSRIP Year 0? How does it differ from the other years?
A: DSRIP Year (DY) 0 was the year for planning, assessment and project development for Performing Provider Systems. The other years, DYs 1 through 5 are for project implementation, performance evaluations & measurement as well as metrics & milestones achievement.
B8.Q: What is the Project Approval and Oversight Panel (PAOP)? (New 7/1/2016)
(CMS), required the state and Independent Assessor (IA) to convene a panel to review DSRIP applications scored by an independent assessor and to advise the Commissioner of Health whether to accept, reject or modify those recommendations. The PAOP played an important role in approving DSRIP Project Plans from all areas of the state and will serve as advisors and reviewers of Performing Provider Systems status and project performance during the 5-year DSRIP duration. They will convene during DSRIP Year 2 to review the recommendations put forth by the IA for the Mid-Point Assessment and make recommendations on changes to PPS networks and DSRIP projects. In addition, the PAOP will meet with PPS Leads regionally on a bi-annual basis to receive updates on the status of projects and progress towards goals and objectives.
Information about the PAOP and previous PAOP meetings can be found on the DSRIP website.
B9. Q: What are the DSRIP Public Comment Days? (New 7/1/2016)
A: The 1115 Waiver and DSRIP Public Comment Days are provided as opportunities for the public to provide comments and feedback on all 1115 Waiver Programs. The DSRIP program is a significant waiver initiative, and members of the DSRIP Project Approval and Oversight Panel will join DOH staff in listening to the feedback provided by members of the public and stakeholders on these Public Comment Days. Feedback on all waiver programs is welcomed. Each Public Comment Day will be webcast live, and archived. These meetings are also open to the public, with no pre-registration required. All comments will be limited to five minutes per presenter, to ensure that all public comments may be heard.
These Public Comment Days are held regionally, with the downstate Public Comment Day on May 4th, 2016, in New York City and the upstate Public Comment Day on July 12th, 2016 in Albany.
More information on the Public Comment Days, and the link to the archived webcast can be found on the DSRIP website.
|back to table of contents||top of section| |top of page|
C. DSRIP Eligibility
C1. Q: What type of providers/care settings were able to submit an application to participate in DSRIP?
A: The DSRIP program was open to an array of providers across the state. However, different types of providers had to meet certain criteria to be deemed eligible as a DSRIP safety net provider. Being deemed a DSRIP safety net provider allows an organization to be an active participant who is eligible to not only to lead, but also share in the full amount of potential performance payments of a Performing Provider System (PPS) in the DSRIP program.
Eligibility Criteria for Hospitals - Hospitals could qualify as a DSRIP eligible provider by passing at least one of the three tests below.
Hospital Test #1:
- Must be either a public hospital, Critical Access Hospital or Sole Community Hospital.
Hospital Test #2: (Note that a hospital needs to meet both of these qualifications to pass this test)
- At least 35 percent of all patient volume in their outpatient lines of business must be associated with Medicaid, uninsured and Dual Eligible* individuals.
- At least 30 percent of inpatient treatment must be associated with Medicaid, uninsured and Dual Eligible* individuals; or
Hospital Test #3:
- Must serve at least 30 percent of all Medicaid, uninsured and Dual Eligible* members in the proposed county or multi-county community. (The state will use Medicaid claims and encounter data as well as other sources to verify this claim. The state reserves the right to increase this percentage on a case by case basis so as to ensure that the needs of each community´s Medicaid members are met.)
Eligibility Criteria for Non-hospital based providers - Those not participating as part of a state-designated health home, must have at least 35 percent of all patient volume in their primary lines of business associated with Medicaid, uninsured and Dual Eligible* individuals.
*Dual Eligible Individual: Refers to a Medicaid beneficiary who is also eligible to receive another type of health insurance, including commercial insurance or Medicare.
C2. Q: How do I find out if my organization meets the DSRIP safety net qualifications? (Revised 7/1/2016)
A: A list of DSRIP eligible safety net providers is available on the DSRIP website. The lists are divided by provider type into separate PDF documents. Each PDF document contains a complete list of entities within the state for that provider type, regardless whether or not the entity meets the DSRIP safety net provider definition. If a provider sees "True" listed in the "final results" column, then the provider has passed at least one of the eligibility tests and has qualified to be a DSRIP safety net provider. It should be noted that Safety Net determinations might be updated during the mid-point assessment.
C3. Q: Is there a way my organization can still participate in DSRIP even if it does not meet the eligibility requirements to be a safety net provider or qualify for a VAP Exception? (Revised 7/1/2016)
A: Yes. As stated in the STCs, non-safety net providers can participate in DSRIP. However, non-safety net providers are eligible to receive, in aggregate, DSRIP payments totaling no more than 5 percent of a project´s total valuation. Please contact your local PPS for possible participation. A list of PPS contact information can be found on the DSRIP website.
C4. Q: How is the 5% limit on non-safety net provider performance payments applied?
A: Each Performing Provider System´s DSRIP Project Plan received a maximum monetary valuation during the application process. All providers within a PPS that did not meet DSRIP-eligible safety net provider definition, in aggregate, are only able to receive up to 5% of the performance payments from a project´s total valuation. At least 95% of the performance payment must be made to the safety-net qualified PPS.
C5. Q: If private doctors are not considered qualifying safety net providers, would they be subject to the 5% cap?
A: If a private doctor does not meet the DSRIP safety net provider qualifications, they can still participate in a DSRIP PPS either as a non-qualifying provider (subject to the 5% earnings limit) or they could have applied to be part of the PPS through meeting the DSRIP Vital Access Provider (VAP) Exception criteria. (See Page 6, What was the DSRIP VAP Exception and how does it pertain to DSRIP safety-net eligibility?)
C6. Q: Since an Independent Practice Association (IPA) is not a Medicaid provider per se, can it be a PPS partner because its physician members are Medicaid providers or do the physicians need to participate in the PPS as individual practitioners?
A: The IPA would be a non-qualifying partner, and would be limited to 5% of total project valuation. However, the IPA can assist qualifying providers in their network. Examples include:
- Helping members qualify as safety net providers,
- Providing technical assistance on meeting DSRIP project goals, and
- Negotiating on their members´ behalf in establishing Performing Provider Systems.
|top of section| |top of page|
D. DSRIP Eligibility Appeals
D1. Q: Based on the safety net list on the DSRIP website, my organization was listed, but did not meet the qualifications to be a safety net provider in the DSRIP program. Can my organization appeal if we feel there was an error in the data used to determine eligibility?
Please review the DSRIP Safety Net Provider lists available on the DSRIP website.
The second and final DSRIP safety net appeal process is closed. Providers who were not included on the eligible provider lists above, and believed that they had met the safety net definition had the opportunity to appeal their safety net provider status. These appeals were due August 27, 2014. Late appeals were not accepted. Please note that the safety net appeals process was NOT for entities who were looking to pursue the DSRIP Vital Access Provider (VAP) Exception process, which closed October 24, 2014. A final posting of Safety Net lists and VAP Exceptions was finalized and posted on the DSRIP Safety Net Definition website.
D2. Q: What was the DSRIP VAP Exception and how does it pertain to DSRIP safety-net eligibility?
A: Under the DSRIP Vital Access Provider (VAP) Exception, the state considered exceptions (to the safety net definition) on a case-by-case basis if it was deemed in the best interest of Medicaid members and made clear that the provider system in question provides essential benefits within the larger system. The list of approved VAP Exceptions are on the DSRIP website. The application period for VAP Exception is closed and no new providers will be added to the list at this time. Those providers that received a DSRIP VAP Exception will be viewed as qualifying safety net providers in regards to the DSRIP program and will be eligible to share in safety net portion (≥95%) of performance payments allotted to a PPS.
There were three reasons under which DOH and CMS would grant a VAP Exception in the DSRIP program:
- A community would not be served without granting the exception because no other eligible provider is willing or capable of serving the community.
- Any hospital uniquely qualified to serve based on services provided, financial viability, relationships within the community, and/or clear track record of success in reducing avoidable hospital use.
- Any state-designated Health Home or group of Health Homes.*
*The Department submitted a draft list to CMS of those State Designated Health Homes and Network Care Management Agencies (CMAs) that had been previously approved as safety net providers, as well as those that were pending approval by CMS. The list of State Designated Health Homes and CMAs is posted to the Safety Net section of the DSRIP website. Initially, you did not need to submit a VAP Exception form if:
- Your Health Home appeared on the draft list as pending approval, as you would be granted a VAP Exception following CMS approval.
- The organization operating your Health Home/CMA already appeared on another safety net provider list.
If your Health Home organization did not appear on the draft Health Home list pending CMS approval, or on another approved safety net provider list, but your organization believed that it should qualify as a Health Home, you were asked to complete the VAP Exception form.
D3. Q: How do I apply for a Vital Access Provider Exception? (Revised 7/24/2016)
A: The Vital Access Provider Exception process is now closed. *The form to apply for a VAP Exception was posted on the DSRIP website in late September 2014. VAP Exception applications were due by October 24, 2014 and made public on the DSRIP website immediately for a 30-day comment period. CMS approval of exceptions were posted to the website in February 2015.
*During the DSRIP Demonstration Period, PPS Lead entities may have decided to pursue different corporate structures to facilitate DSRIP implementation. For this purpose, the NYS DOH will permit current PPS Lead entities ONLY to submit new corporation VAP exception applications for safety net designation.
|back to table of contents||top of section| |top of page|
E. Performing Provider Systems (PPS)
E1. Q: What is a Performing Provider System?
A: The entities that are responsible for creating and implementing a DSRIP project are called "Performing Provider Systems", abbreviated "PPS". Performing Provider Systems are providers that form partnerships and collaborate in a DSRIP Project Plan. PPS include both major public hospitals and safety net providers, with a designated lead provider for the group. Safety net partners can include an array of providers: hospitals, health homes, skilled nursing facilities, clinics & FQHCs, behavioral health providers, community based organizations and others. Performing Provider Systems must meet all requirements described in the Special Terms and Conditions (STCs), including the safety net definition described in STC VIII.2.
E2. Q: Can a provider still join a PPS at this point in time? If yes, can you still participate in the financial incentive payment? (Revised 8/31/2018)
A: At this time, the PPS provider networks are closed. However, annually until Measurement Year 5, PPS networks reopened for the addition of new partners for performance purposes only. We recommend reaching out to the PPS in your region regarding possible participation. A list of PPS contact information can be found on the DSRIP for Providers & Professionals website.
E3. Q: What is required of a DSRIP Performing Provider System?
A: It is important to understand that DSRIP payments are made based upon project performance. A PPS will be required to perform a community assessment of need, identify DSRIP strategies that are most consistent with addressing that need, develop a Project Plan incorporating those strategies, implement that Project Plan and monitor milestones and metrics to ensure the implementation is successful. There are certain strategies that will be required of all PPS. It is expected that at the end of the DSRIP program, the health care delivery system for Medicaid members and other New Yorkers will look fundamentally different, with greater focus on high quality ambulatory care and a de-emphasis on hospital inpatient and ED care, helping to meet the state goal of reducing avoidable hospital use, including emergency department and inpatient, by 25%.
E4. Q. If Medicaid makes up only a portion of a provider´s book of business, what are the impacts of the DSRIP program on the rest of a provider´s business?
A: The DSRIP program is an initiative specifically targeted to Medicaid and the uninsured population. However, as PPS entities work to transform their service delivery system and payment structure, the state expects that the DSRIP program will act as a catalyst for change to other parts of a provider´s book of business. In addition, pay for performance or value based purchasing by government and private insurers is becoming much more widespread, supporting the transformative changes from DSRIP.
E5. Q: Can a provider be a member of more than one PPS?
A: Yes. There is no requirement in the DSRIP program stating that a provider or organization can only join one PPS. Providers that serve large geographic areas which cross medical markets may join two (or more) PPS networks to best serve their patients.
However, providers who are considering joining multiple PPS should understand that there can be some drawbacks. Firstly, the attribution an organization brings to a PPS will diminish with each additional PPS the provider/organization joins. For example, if a clinic joins two PPS in the same county, the clinic´s attributed members will most likely be split between the two PPS networks it is partnered with. This could harm the clinic´s performance payment negotiations with each PPS, because the clinic will bring fewer lives to each PPS. Additionally, the clinic may see that there are greater administrative and reporting demands placed on the entity as it has to be responsive to two PPS.
For more information on attribution logic, see section titled "Attribution" or the presentation on Attribution and Valuation.
E6. Q: Are providers encouraged to work together? If so, what types of providers can collaborate as partners?
A: It is a requirement that eligible providers within a region/service area work together on a DSRIP project. Significant community collaboration by Medicaid and non-Medicaid providers is a key theme of DSRIP and is necessary in order to meet the performance aims of DSRIP.
Within a PPS there should be a wide variety of providers including hospitals, clinics, primary care physicians, specialists, home care, SNF, Health Homes, and behavioral health providers. Also, community based organizations such as housing providers should be key participants so that the PPS will have resources in the community and be able to address the social determinants of health.
E7. Q: Will there be collaboration between PPS?
A: Yes. Collaboration between PPS is critical to the overall success of DSRIP. Collaboration in general is seen as necessary for ensuring downstream providers are able to achieve clinical integration with PPS, particularly since many downstream providers may be engaged with multiple PPS. For this reason, the extent to which there is project overlap between regions with a similar patient base (based on a single community needs assessment as has been done in Westchester, Brooklyn and Long Island, for example), collaborative efforts between PPS will be a key lever to making sustainable change in a region.
Also, from DY1-DY5, PPS will be required to take part in DSRIP Learning Symposiums. These learning collaboratives will take place in person no less than once a year and will foster an environment of mutual assistance. PPS will be encouraged to share best practices and challenges, and receive assistance and guidance from other PPS counterparts on how to best implement and meet the objectives of their DSRIP Project Plans. This is particularly important as, in DY3, CMS began evaluating summative statewide performance on DSRIP benchmarks. There will be performance payment reductions across the board to all PPS if those statewide benchmarks are not met.
E8. Q: Are there any signed attestations required to confirm DSRIP Partnership?
A: Yes. Every PPS Lead partner is required to submit an attestation statement documenting that each partner included in its Network Tool partner list has formally consented to be part of the PPS. Attestation was required BOTH times the Network Tool was used - for initial and final attribution for valuation. PPS Lead partners are responsible for maintaining a file of signed partnership agreements from all partner organizations that can be made available to the state and/or CMS upon request.
If for any reason it is found that partner lists have been manipulated or inappropriately prepared, the Office of the NYS Medicaid Inspector General, as well as CMS, will be notified and appropriate action will be taken. If the PPS Lead partner does not have a signed partnership agreement with a provider, the lead entity should refrain from adding that provider to their partner list in the Network Tool.
E9. Q: What is the DSRIP Network Tool? (Revised 8/31/2018)
A: The DSRIP Network Tool is an electronic tool housed in New York´s Medicaid Analytics Performance Portal (MAPP), a web-based portal accessed through the Health Commerce System (HCS). The Network Tool is the means by which PPS entities updated/replaced their list of partner organizations during the DSRIP planning process. Providers were required to update their partner organization list, using this tool, by September 29, 2014, so that the state could begin the process of running initial attribution. PPS could continue to edit their partner organization lists via the Network Tool until December 1, 2014 when the tool was closed for the state to run attribution for valuation. The network for valuation is locked and closed for changes at this time. The network tool to add providers for performance, opened annually until the start of Measurement Year 5.
For more information on the DSRIP Network Tool, please visit the DSRIP Medicaid Analytics Performance Portal (MAPP) website.
E10. Q. Can you explain why there are some providers listed on the performance list that are not on the valuation list? (Revised 8/31/2018)
A: Each PPS has two partner network lists in the MAPP System: a valuation network and a performance network. Networks for valuation were closed December 1, 2014 and were used to attribute members for purposes of calculating valuation. Valuation networks were locked and will not be changed - it is basically a snapshot of the PPS on that date.
However, as the DSRIP program went forward, PPS needed to change their networks and add providers as they expanded services or needed a specific type of provider to meet their objectives. Hence, the performance network changed during the course of the DSRIP program. Providers could only be removed one time during the mid-point assessment, but were added annually when the DSRIP PPS network reopened. The performance network should be larger than the valuation network; this is why you will see some providers on the performance network, but not on the valuation network. The performance network is used to set baselines and then to measure performance on a quarterly basis.
E11. Q: How is a partner defined for the network list? (Revised 8/31/2018)
A: The DSRIP program was opened to an array of health providers and health-related and community service entities/providers across the state. These providers partnered with a PPS to develop and implement a DSRIP Project Plan. In the context of DSRIP, PPS partners are those providers that a PPS Lead submitted as part of its PPS in the DSRIP Network Tool. PPS partners included in the Network Tool are DSRIP safety-net qualified and non-safety net qualified entities, as well as providers who do not directly bill Medicaid.
What a PPS considered in making an entity a partner rather than an outside contractor was whether or not the partner was in a performance-based relationship with the PPS in implementing its DSRIP Project Plan. If the entity was held accountable for performance in helping the PPS reach its DSRIP objectives, it was important for the entity to be included as a partner to ensure alignment, and they signed a formal participation agreement with the PPS documenting this participation and alignment.
E12. Q: What is required for the network partnership agreements? (Revised 8/31/2018)
A: All PPS Leads were required to have signed partnership agreements from each partner in their files by the time they submitted their final partner list via the Network Tool. Partnership agreements related to the DSRIP program and connected the entities together for DSRIP attribution and program purposes. The state did not provide a standardized template, but issued the following guidance:
- PDF copies of the signed agreements are sufficient (meaning all these agreements can be kept electronically).
- These agreements do not have to be notarized.
- Each individual physician in a practice group does not have to submit their own letter; but, rather, a signed letter from the practice CEO stating that all the practitioners in a practice/organization are authorized to be added to a PPS´s list is sufficient.
For IPAs, if they had opt-out rules, then the PPS required one letter from the IPA CEO to add all providers to the PPS. If the IPA had opt-in rules, then the PPS needed to collect signatures from each member of the IPA that they wished to include in their network.
E13. Q: What happens if a partner drops out of the DSRIP process due to financial issues? (Revised 8/31/2018)
A: Financial sustainability is a key end point that the PPS will need to attain. It is expected that the transformation of the health care system will result in changes in provider mix, some increases and some decreases. These should be well understood based upon the comprehensive community needs assessment and considered in the developing of projects. A PPS should do its best to try to limit the risk of partners leaving the PPS due to financial issues by (1) allocating DSRIP performance funds within the PPS to aid partners in this situation, as well as (2) help those providers set up adequate restructuring plans to secure financial sustainability over the course of DSRIP and beyond.
Additionally, PPS governance plans addressed how the PPS proposed to manage lower performing / financially distressed members within the PPS network. This plan included progressive sanctions prior to any action to remove a member from the performing provider system. Unless the partner organization closes or there is some other extreme circumstance, PPS will not be able to alter their partner lists for valuation purposes. PPS were allowed to formally remove partners only at the Mid-Point Assessment period prior to the start of DY3 for various reasons. Only up to 10% of the PPS partner network could be removed. However, PPS were allowed to add partners annually when the network reopened. These new partners were added for performance only.
E14. Q: Can you remove partners after finalizing your partner list? (Revised 8/31/2018)
A: PPS networks were submitted via the DSRIP Network Tool for the purposes of calculating attribution for valuation and later, attribution for performance.
No more than once a year, Performing Provider Systems (PPS) were permitted to submit proposed modifications to an approved DSRIP Project Plan for state and CMS review. These modifications could not decrease the scope of the project unless they also proposed to decrease the project´s valuation.
Removal of any PPS member organization requires a proposed modification, and removal of any such lower performing member must follow the required governance procedures including progressive sanction requirements.
E15. Q: Can you add partners after finalizing your partner list? (Revised 8/31/2018)
A: Once a year, the state opened performance networks and PPS added partners. Please note, additional partners were for performance purposes only. Early Spring 2018 was the last network reopening and reflects Measurement Year 5.
E16. Q: What provider types qualify to be lead applicants in a DSRIP Performing Provider System?
A: Any qualifying DSRIP safety net provider could be a lead applicant, regardless of provider type. However, in the DSRIP Project Plan, the lead applicant was assessed on its ability to fulfill the role as the lead entity within the Performing Provider System. Qualifications that could have allowed an entity to fulfill the role as the lead applicant includes, but were not limited to:
- Previous collaborative experience,
- Unique leadership capabilities,
- Administrative capabilities,
- Financial stability.
It should be noted that while all PPS entities, as a whole, underwent a financial evaluation to ensure the entity´s ability to complete the program, lead organizations underwent a more intensive, individual financial assessment to ensure fiscal stability for the PPS through the DSRIP program. Furthermore, new governing structures ("NewCos"), rather than individual safety net providers, can serve as leads for Performing Provider Systems in the DSRIP program.
E17. Q: Within a PPS network, how much autonomy does a PPS have in distributing funds?
A: A PPS has the autonomy to allocate performance funds how it best sees fit, as long as at least 95% of performance payments go to safety net qualified partners and no more than 5% go to non-qualifying safety net partners. However, PPS funds allocation must be described in the DSRIP Budget & Flow of Funds section of the Project Plan Application and include a description of how DSRIP performance payments will be distributed amongst providers, and how the distribution of funds is consistent with the governance structure and DSRIP goals.
After DSRIP payments are received from the PPS Lead, partners are not restricted from making payments to other in-network or out-of-network providers (e.g., contracts for DSRIP-supportive services). Once a performance payment is properly received, the DSRIP program does not impose any additional restrictions on these funds.
The PPS Lead must have established a budget and funding distribution plan, (at the level of detail set forth in the DSRIP Project Plan Application and Award Letter and the DSRIP Implementation Plan) that specifies how DSRIP funds received are distributed among the participating providers in the PPS to incentivize providers to reach DSRIP performance goals. The PPS Lead in its budget plan needed to provide a distribution methodology taking into account five different categories:
- Project implementation costs
- Costs for delivery of services not reimbursed or under-reimbursed by Medicaid
- Provider performance payments
- Compensate revenue loss
- Other for administrative and other costs not included in previous categories
E18. Q: Will PPS networks be protected from laws on anti-competitive behavior?
A: Yes, in instances where a DSRIP PPS can show that a potential collaboration between providers will benefit the community, there will be an opportunity for the state to provide protections for a PPS. This protection will come in the form of a Certificate of Public Advantage (COPA), which will be granted if it appears that the benefits of a collaboration between PPS partners will outweigh any disadvantages attributable to their anticompetitive effects and will be subject to active state supervision. COPA regulations are explicated in Article 29-F of New York´s Public Health Law.
More information on COPA in relation to DSRIP is available at: http://www.health.ny.gov/health_care/medicaid/redesign/copa/index.htm
E19. Q: Will a data sharing agreement with the state be required? (Archived 7/24/2017)
A: Yes. The state will be delivering provider-specific Medicaid information through a DSRIP portal, Medicaid Analytics and Performance Portal (MAPP).
Minimally, a Data Exchange Application and Agreement (DEAA) will need to be executed with the state for data available in the portal and any data sharing outside of the portal. Additionally, PPS are required to have established Health Commerce System (HCS) accounts to access the DSRIP portal (MAPP).
Further information is available in the Data Sharing section of this FAQ, or in the DSRIP Data Sharing FAQ.
|back to table of contents||top of section| |top of page|
F. New Governing Structure ("NewCo")
F1. Q: Can a NewCo receive DSRIP award money directly from DOH?
A: Only PPS Lead entities will receive DSRIP award money directly from DOH.
For a NewCo to receive DSRIP award money directly from DOH, the NewCo would have to qualify as a PPS Lead entity, including being registered as a Medicaid provider, and either satisfying the requirements to be a Safety Net Provider or having been granted a Vital Access Provider (VAP) Exception.
Where there is a public hospital in a NewCo with multiple members, DSRIP payments will be made to the public hospital entity in order to enable Intergovernmental transfer (IGT) funding. The NewCo Lead will receive its DSRIP payments from the public hospital partner.
F2. Q: If a NewCo cannot receive DSRIP award money directly from DOH, can the NewCo function as the PPS Lead entity?
A: The NewCo has to be approved by DOH and CMS to be a PPS Lead entity per the requirements previously stated. If it is not approved, then it cannot serve as PPS Lead entity or receive funds directly.
F3. Q: Can a NewCo be used to create multiple Lead entities for a single PPS?
A: No. Only one legal entity can receive DSRIP award money, and that entity is the PPS Lead entity.
F4. Q: How can a PPS have a NewCo become the PPS Lead entity? (New 7/1/2016)
A: The PPS Lead that wishes their NewCo to become the PPS Lead entity should contact DOH to obtain a NewCo VAP Exception Form. This form must be completed and approved by CMS. Instructions can be found on the DSRIP website.
|back to table of contents||top of section| |top of page|
G. PPS Project Advisory Committee
G1. Q: What is the Project Advisory Committee?
A: Each emerging Performing Provider System (PPS) was required to form a Project Advisory Committee (PAC). The PAC advises the PPS on all elements of their DSRIP Project Plan. The PPS PAC should include representation from each of the PPS partners as well as workers and/or relevant unions. The PACs were a requirement for the DSRIP Design Grant application and are expected to be in place over the duration of the DSRIP program.
G2. Q: What is the scope of the Project Advisory Committee?
A: The PAC serves as an advisory entity within the PPS that offers recommendations and feedback on PPS initiatives. The PAC should be involved in the various facets of developing a PPS´s DSRIP Project Plan and then engaged in the implementation and oversight of the Project Plan.
PAC meetings/conference calls serve as forums to share and review proposals as well as discuss ideas that will affect the PPS and its workforce. PACs may choose to form sub-committees around various issues or projects, but sub-committees should attempt to maintain their representativeness of the PAC stakeholders. PACs should meet no less than once a month during the DSRIP planning phase and no less than once a quarter during the implementation and oversight phases.
|back to table of contents||top of section| |top of page|
H. Community Needs Assessment
H1. Q: Can you provide information about conducting and using a Community Needs Assessment?
A: Each project a Performing Provider System selected must be responsive to a thorough community needs assessment that ties to the DSRIP goals of system transformation and reducing avoidable hospital use, including emergency department and inpatient. More information and guidance on the requirements of the DSRIP Community Needs Assessment can be found in the Community Needs Assessment Guidance document. Additionally, two webinars explaining the Community Needs Assessment process were recorded and provided on the DSRIP site under Webinars and Presentations.
H2. Q: Does the currently required Hospital Needs Assessment suffice for the DSRIP Needs Assessment? (Archived 7/24/2017)
A: While the hospital needs assessment can be a good starting point for the community assessment, it will not likely be sufficient. DSRIP´s focus is health care for the population served by Medicaid. Their service needs may be different from that of the composite total population served by a hospital. For example, when performing zip code analysis of service utilization, there may be marked population differences. In addition, since DSRIP is about service delivery transformation, the community assessment must not be done as a hospital-centric assessment, but as a total community service provider assessment.
Additionally, two webinars explaining the Community Needs Assessment process were recorded and provided on the DSRIP site under Webinars and Presentations.
H3. Q. Will there be guidance with respect to continual updates to the community needs assessment conducted for the program?
A: The goal of DSRIP is continuous quality improvement with use of rapid cycle improvement methodology. The basis for the projects chosen for DSRIP were needs identified through the initial community needs assessment (CNA). As the CNA is intimately tied to the process of continuous quality improvement, the PPS should identify if those needs have been met/improved/not met through an updated community needs assessment.
|back to table of contents||top of section| |top of page|
I. Domains, Strategies & Projects
I1. Q: What are the DSRIP Project Plan, Domains, Projects and strategies?
A: A DSRIP Project Plan is the overall plan that a Performing Provider System submitted to the state. The Project Plan is composed of at least 5 projects, but no more than 11 projects, based upon projects chosen from a predetermined list. For the full list, see the DSRIP Project Toolkit..
There are four Domains in DSRIP that represent groupings of project milestones and associated metrics. The four Domains are:
- Domain 1 - Project progress milestones - measurement on completion of Project Plan
- Domain 2 - System transformation milestones - measurement of system transformation
- Domain 3 - Clinical improvement milestones - disease focused clinical improvements
- Domain 4 - Population-wide strategy implementation milestones - Prevention Agenda improvements
All DSRIP Project Plans have metrics attached to each Domain. Domain 1 metrics are measures of the completion of the DSRIP Project Plan. Domains 2, 3, and 4 have strategy sublists identifying specific strategies. For example, under Domain 2, there is a strategy sublist A called "Create Integrated Delivery Systems". Under each strategy sublist is a selection of projects that can be used to meet that goal of an integrated delivery system.
I2. Q: Are there minimum/maximum number of projects that are required? (Archived 7/24/2017)
A: Yes. DSRIP Project Plans include a minimum of 5 and no more than 10 projects for valuation purposes. However, if a PPS is eligible to pursue Project 2.d.i. the project plan may include 11 projects. At least two (and no more than four) Domain 2 system transformation projects (unless Project 2.d.i is included in which case up to five system transformation projects can be involved) at least two (and no more than four) in Domain 3 clinical improvement projects, and at least one (and no more than two) Domain 4 population-wide project(s) must be included in the PPS´s Project Plan.
One of the required Domain 2 projects must be chosen from strategy sublist A. The other required Domain 2 project can be selected from either strategy sublist B or C. One of the required Domain 3 projects must be chosen from the Behavioral Health strategy sublist.
As described further in the project valuation section of Attachment I, a maximum of 10 projects will be considered for project valuation scoring purposes, with the exception being those PPS pursuing Project 2.d.i ("the 11th Project"). Additional projects may be included in the application; however, a maximum of 10 projects will be used to assess application valuation.
Please refer to "Project 2.d.i." section for further regulations regarding the 11th Project.
I3. Q: For PPS picking 10 projects, is there any opportunity to pick more from Domains 2 and 3 instead of Domain 4? (Archived 7/24/2017)
A: No. Not including the 11th Project, a PPS can pick a maximum of four Domain 2 projects, four Domain 3 projects, and two Domain 4 projects.
I4. Q: If a PPS has multiple hubs (or sites), will it need to do all of the chosen projects in each?
A: No. A PPS will not need to do each project in each hub or each site. The community needs assessment identified the most significant health-related problems for a PPS and the sites where these problems are most significant. Targeted implementation of a project at such a site or sites would make the most impact. For example, the 11th Project must be implemented in a way that benefits all uninsured and low/non Medicaid utilizers in the geography served by the PPS. However, not every site will serve many people from this sub-population. Hence, as the project´s description suggests, a "hot spot" approach could make the most sense. However, the PPS should always keep in mind that while a "hot-spot" approach makes sense to efficiently allocate and manage resources to where they will be needed most, the project´s metrics will be measured based upon the entire PPS population attributed to that project.
I5. Q: Can a Performing Provider System´s DSRIP funds be used to supplant other, existing programs?
A: All projects undertaken by a Performing Provider System must be a new initiative for the entity and must be substantially different from other initiatives funded by CMS. If the Performing Provider System is building on a pre-existing, non-CMS funded initiative, the PPS must have demonstrated in their DSRIP Project Plan application how the coalition is significantly augmenting the initiative, allowing for substantial transformation over the status quo.
I6. Q: What types of primary care providers may be utilized to provide primary care in the Behavioral Health (BH) setting for 3.a.i.? NPs, PAs, tele-psychiatry, other?
A: The only types of "primary care providers" that may be utilized to provide primary care services within the BH site for 3.a.i are participating PCPs, NPs, and physician assistants working closely with a PCP. Tele-psychiatry by its nature is psychiatry and not primary care services. Tele-psychiatry could be utilized potentially in the third model, IMPACT, when there are insufficient psychiatrists to provide the onsite services.
I7. Q: Are pediatric members, who meet the definition of "actively engaged" for a project able to count towards committed numbers each year?
A: The basis for the actively engaged population is based on a subset of the total attributed population associated with the PPS, which includes all Medicaid beneficiaries (adults and children).
I8. Q: How will "actively engaged" patients be tracked? For example, for Project 3.f.i, how will the Scheduled Delivery Forms be submitted?
A: All guidance to date concerning Active Engagement is provided here.
For project 3.f.i, schedule delivery forms should be submitted for each case through the NYSDOH Health Commerce System. Additional details about project 3.f.i and the submission process may be found here.
I9. Q: For Project 3.c.i, the definition of "actively engaged" is "The number of participating patients with at least one hemoglobin A1c test within previous Demonstration Year". Since this actively engaged definition would include a Medicaid claim for the HgA1C, will the IA expect the PPS to show claims data for a patient to count as actively engaged? Or, given the lag in claims data, is the PPS´s own tracking system sufficient?
A: For the attributed members the PPS can run a report that demonstrates the number of members that have had an HgA1C in the last year. The Independent Assessor recognizes that data provided through Salient will only reflect paid claims. The PPS can demonstrate HgA1C services by producing reports from its own reporting tool.
I10. Q: For project 2.b.v, the "actively engaged" definition is "the number of participating members with a care transition plan developed prior to discharge". What are the criteria that define participating patients here, particularly those with cardiac, renal, diabetes, respiratory and/or behavioral health disorders?
A: The definition of "actively engaged" for project 2.b.v. includes Medicaid nursing home patients with recent hospital discharges who are at risk for re-hospitalization, with a care transition plan developed prior to discharge, and who are not readmitted within that 30-day period.
I11. Q: Are Article 28 clinics that offer primary care and are in DSRIP required to become Patient Centered Medical Homes?
A: Clinics that offer primary care and are involved in certain DSRIP projects must meet NCQA 2014 Level 3 PCMH accreditation and/or meet the state-determined criteria for Advanced Primary Care models by the end of DY3. Please refer to the DSRIP Project Toolkit for additional information.
I12. Q: How are Planned Parenthood Practices viewed as far as the requirement to become PCMH recognized in the PPSs? Generally, OBGYN clinicians are not viewed as a primary care specialty and are therefore not eligible for PCMH. However, some have parallel primary care clinicians in the same practice with panels of patients, but it is very limited. In this case, would the Planned Parenthood practice be eligible for PCMH? (New 7/1/2016)
A: Planned Parenthood practices with providers who are providing comprehensive primary care, and not just medical screening, MAY BE eligible to certify as a Patient Center Medical Home. Such practices are encouraged to contact NCQA and discuss their unique situation and its fit with the PCMH standards. Further information on PCMH can be found on the NCQA website.
I13. Q: How does the Patient Centered Medical Home (PCMH) fit in with DSRIP? (New 7/1/2016)
A: Project requirement language requiring practices to meet the 2014 NCQA Level 3 PCMH/NYS Advanced Primary Care Model recognition has been updated in the Independent Assessor´s Reporting and Validation Protocols to reflect that only eligible practices and providers are required to meet these requirements. For projects requiring recognition, the PPS will be required to submit documentation to support 100% of eligible PCPs obtaining appropriate recognition to demonstrate successful completion of the project milestone. For example, project requirement one of Project 2.a.ii: Increase Certification of Primary Care Practitioners with PCMH Certification and/or Advanced Primary Care Models (as developed under the New York State Health Innovation Plan (SHIP)), has been updated to the following:
Ensure that all eligible PCPs participating in the PPS achieve recognition for either NCQA 2014 Level 3 PCMH accreditation or for the NYS Advanced Primary Care Model meeting DSRIP standards by the end of DY3.
In order to substantiate completion of this milestone the PPS is accountable for ensuring that eligible PCPs obtain NCQA 2014 Level 3 PCMH/NYS Advanced Primary Care Model recognition and retains applicable supporting documentation for validation purposes.
|back to table of contents||top of section| |top of page|
J. Primary Care Plan
J1. Q: What is the PPS Primary Care Plan?
During the February 2015 DSRIP Project Approval and Oversight Panel (PAOP) meeting, the panel voted to require each PPS to submit a Primary Care Plan. The goal of the PPS Primary Care Plan is for PPS to address the question, "What is your over-arching DSRIP plan for Primary Care?" The purpose of the PPS Primary Care Plan is to:
- Assess current status of primary care in your network
- Detail plans for reaching primary care milestones
- Report on measures to assess progress towards achieving goals around access and capacity
J2. Q: What elements need to be included in a PPS´s Primary Care Plan?
A: All PPS Primary Care Plans should include the following six fundamentals:
- An assessment of current primary care capacity, performance and needs, and a plan for addressing those needs;
- How Primary Care expansion and practice and workforce transformation will be supported with training and technical assistance;
- How primary care will play a central role in an integrated delivery system;
- How the PPS will enable Primary Care to participate effectively in value-based payments;
- How PPS funds flow supports the PPS Primary Care strategies; and
- How the PPS is progressing toward integrating Primary Care and Behavioral Health
J3. Q: What is the difference between the New York State Health Improvement Plan (SHIP), State Innovation Model (SIM), and Advanced Primary Care plans? (New 7/1/2016)
A: SHIP is a broad plan versus SIM which is a grant application over several years and APC is only a component of that grant. The goal is multi-payer approach to align care AND payment reform focused on primary care that:
- Works to achieve triple aim goals
- Engages practices, patients, and payers
- Builds on evidence, experience, existing demonstrations, PCMH
- Is sustainable
- Not ´just´ a grant program
- Is supported by HIT/HIE, workforce, access Is statewide
|top of section| |top of page|
K. Project 2.d.i. ("Project 11" or "The 11th Project")
K1. Q: What is Project 2.d.i, or "the 11th project?"
A: This new Domain 2 project was created with the goal of incorporating uninsured (UI) members into DSRIP, and ensuring that the UI population, along with the non-utilizing (NU) and low-utilizing (LU) members, gain access to and utilize the benefits associated with a PPS´s DSRIP projects. This Project 2.d.i focuses on increasing patient and community activation related to health care, paired with increased resources that can help the UI, NU, and LU populations better access, particularly, primary care and preventive services.
K2. Q: Can any PPS select to pursue the 11th Project?
A: No. A PPS must have received state approval to pursue Project 2.d.i in a specified county. Major public hospitals had the right of first refusal in taking on the additional 11th Project. If the public PPS chose to pursue the 11th Project, no other PPS in that county could pursue it. If no public PPS exists in a county, or the public PPS chose not to pursue the 11th Project, then one or more non- public PPS serving that county may have been approved to pursue the project in that county. Approval to take on Project 2.d.i may have been granted if:
- The PPS elected to pursue a 10-project DSRIP application (not including Project 2.d.i.),
- The PPS demonstrated its network is capable of handling the 11th Project, and
- The PPS demonstrated how its network is suited to serve the UI, NU and LU populations in the counties in which it will be pursuing the 11th project.
K3. Q: How does the state define non-utilizing and low-utilizing Medicaid members?
A: Non-utilizing (NU) members are those who are enrolled in Medicaid yet do not use any services in a given year. Low-utilizing (LU) members are those who the state defined as utilizing three or fewer services per year and have little to no connectivity with their PCP or care manager.
|back to table of contents||top of section| |top of page|
L. Metrics & Milestones
L1. Q: What are the implications of changing target dates for project milestones?
A: The PPS has the option to change the target dates of a step/milestone only if that milestone is not attached to an achievement value. The steps/milestones for which the Independent Assessor set minimum target dates cannot be changed and cannot exceed what the Independent Assessor has put into the plan.
L2. Q: If all of a PPS´s projects are live by the end of year 2 and all providers have met all of the requirements, will the PPS no longer get the 7th achievement value (AV) for remaining years?
A: Correct. For the remaining years, the PPS no longer gets that 7th achievement value (i.e., they will be evaluated on 6 total AVs).
L3. Q. What constitutes a completed quarterly progress report for workforce process measures and milestones?
A: PPS will need to provide updates on milestone progress and workforce process measures for quarterly progress reports. Submission of both is what constitutes a completed quarterly progress report. However, it is the reporting and measuring of the workforce process measures that drive achievement values/payments, as opposed to the milestone updates.
L4. Q: When will the state be releasing the data to allow the PPS to see what performance targets are? (Revised 8/31/2018)
A: All statewide performance goals have been included in the DSRIP Measure Specification and Reporting Manual first published October 1, 2015. No changes have been made to statewide performance targets.
DOH is evaluating measures which are high-performance eligible and are currently defaulted to maximum values in the Measure Specification and Reporting Manual. The manual is updated annually in the spring and posted to the website in July/August for each Measurement Year 1, 2, 3, 4, and 5.
L5. Q: Some of the metrics are based on 3M proprietary software (PPV, PPR). Will the PPS have access to the proprietary software or data output that is used for some of the metrics?
A: The potentially preventable events (PPV and PPR) are calculated annually using the 3M proprietary logic. The latest annual results will be made available to the PPS with information about observed and expected events to provide PPS with information about improvement opportunities. Ongoing PPV and PPR results will not be available throughout the measurement year. Ongoing monitoring for readmissions and ED visits may be done using the events without the logic. Proxy PQI and PDI results for the PPS will be available with the other quality measures which will be made available to the PPS in MAPP, but will not be the same file that is used for calculation of PPS results for payment.
L6. Q: There are 4 metrics that indicate avoidable hospital use (PPV, PPR, PQI, and PDI). Is it expected that 25% reduction will be realized in each of the 4 metrics, and will these metrics be measured per project or by the PPS as a whole?
A: These four metrics are in Domain 2, System Transformation. As with other metrics, each PPS will be given a target gap to goal to close each year. The denominators will be based upon the entire eligible population from the PPS, which for these measures is the PPS´s full population. The 25% reduction is the total state goal.
L7. Q: There are multiple projects around redirecting patients from ED to more appropriate urgent care or BH services. How is the metric for 25% reduction in avoidable hospital use and PPV determined?
A: PPV is a measure of avoidable ED visits. Visits such as sore throat would be considered avoidable; trauma such as a fracture would not. The goals of these projects are to have patients become part of a primary care practice and learn how to use the health care system more effectively. Depending on the structure developed around these projects, the first ED visit, even though potentially requiring only a medical screening examination to identify if an emergency condition is present, may result in a low level medical claim that will be counted as an ED visit. If the condition meets the metrics for avoidable ED visit, it will count in that metric. It is anticipated that once the patient is engaged with a primary care physician, future ED visits for non-urgent conditions will be avoided.
L8. Q: The specific metrics for Domain 4 are divided into groups (a, b, c, d). As there are multiple projects in each group (b1, b2, etc.), do all the group b metrics count for any group b project?
A: Domain 4 is based upon the Prevention Agenda and includes a subset of projects listed in the Agenda and relevant metrics for the subset of projects. The metrics apply to all projects within the group. The PPS, however, is responsible for the full suite of metrics in Domain 4, i.e., those from all the groups. We recognize that there are many factors involved in moving this complete suite of metrics.
As noted, these are pay for reporting, but, in fact, the state is the one responsible for reporting. The state will continue to monitor the Prevention Agenda as it always has, and all metrics from Domain 4 will be reported by the state for the PPS. A PPS does not need to report metrics.
Also note, the Prevention Agenda includes all New York State residents and projects in this Domain should be inclusive of the total population. What the PPS will be monitored for in Domain 4 is how they meet the milestones for the implementation of their chosen project(s), including number of sites, impact on full population, etc.
|back to table of contents||top of section| |top of page|
M. Attribution
M1. Q: What is DSRIP Member Attribution?
A: Member attribution refers to how Medicaid beneficiaries are assigned to Performing Provider Systems. Members are assigned to a given PPS using geography, patient visit information, and health plan PCP assignment. Additionally, patient visit information is used to establish a "loyalty" pattern based on where most of the member´s services are rendered. This is discussed in Attachment I to the Special Terms and Conditions, and further updates provided in the Attribution and Valuation webinar on the DSRIP website.
M2. Q: Can a beneficiary be attributed to more than one PPS?
A: No. A beneficiary can only be attributed to one Performing Provider System at a time.
M3. Q: Are there any changes to attribution guidelines based on Project 2.d.i.?
A: No. Portions of the uninsured individuals in a given region may be attributed to a PPS based on their approval to undertake Project 2.d.i. Three PPS "types" will be referred to for attribution of uninsured individuals (UI), non-utilizing (NU) members, and low-utilizing (LU) members, which are as follows:
- Single PPS in a Region (Public Hospital Led/Involved or Non-Public)
- Multi PPS in a Region - Public Hospital Led/Involved
- Multi PPS in a Region - Non-Public Hospital Involved.
For further guidelines on attribution following Project 2.d.i., please refer to the above "Project 2.d.i." section.
M4. Q: How are members attributed when there is one PPS in a defined region?
A: Given the instance when a PPS is the sole one in a region, it would be attributed all Medicaid members (UM + NU + LU) for valuation purposes, regardless of whether the PPS pursues project 2.d.i or not. If the sole PPS pursues project 2.d.i, the sole PPS will be attributed 100% of the uninsured in the county as well.
M5. Q: If there is only one PPS in a region, does the geography trump the loyalty aspect of the attribution algorithm? In other words, even if patients in that geography are frequenting another PPS further away, will they still be attributed to the one PPS?
A: In sole PPS counties, for attribution for valuation purposes, the PPS would receive the attribution of all Medicaid members who receive most of their health care services in that county. "Most" is defined in relation to the Medicaid member and how many counties they receive Medicaid services in (serve as the denominator). Hence, if a Medicaid member has claims or encounters in two or three counties, if the member receives the highest percentage of claims in the sole PPS counties, relative to any other county they have received services in (regardless of the logic hierarchy), that member will be attributed to the sole PPS for valuation calculations.
M6. Q: How are members attributed when there is more than one PPS in a defined region?
A: When there is more than one PPS in a county, the attribution loyalty logic will be followed, which is illustrated in the Attribution and Valuation webinar, further explained in the section "Project 2.d.i" and shown below in the next question.
M7. Q: How are members matched to a PPS network through the loyalty logic?
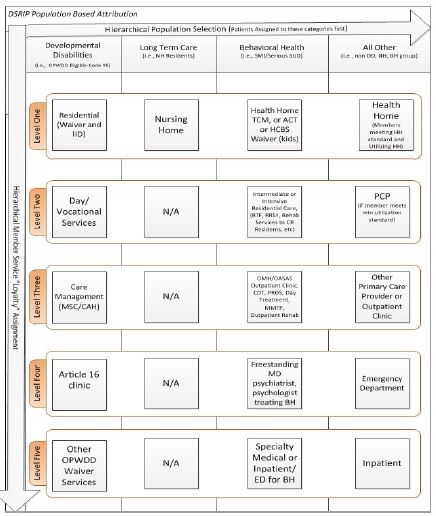
A: Recipient loyalty is assigned based on a patient´s claim and encounter data to a specific provider in a PPS network based on a hierarchy of the population categories and their specific attribution logic. A patient is attributed to a category (DD, LTC, BH, All Other) based upon the hierarchy of population categories. A patient is attributed to the first category they have a claim in based on the category hierarchy logic. Once attributed to a population category, the patient will then be assigned to a specific population subcategory. Patients are assigned to a specific subcategory based on a subcategory hierarchy logic (similar to the process that matched patients to a category). A patient is attributed to the first subcategory category they have a claim in (based on the subcategory hierarchy logic). The DSRIP loyalty logic hierarchy flow chart shown below. If the patient has claims in the same category bucket that is tied to a provider (or multiple providers) in two different PPS, the tie-break logic will be used to assign the patient.
M8. What happens when following the attribution loyalty logic produces a tie?
If more than one PPS has the highest number of visits based on the highest priority services, the methodology will be re-run to determine the following:
Tie-break level 1:
- If additional visits in other service types will cause one PPS to accumulate more visits.
Tie-break level 2:
- If a tie still results the recipient will be temporarily removed from the count and assigned at the end of the attribution process. Those recipients with no predominant provider utilization pattern will be assigned to the PPS in which most recipients in their zip code have already been assigned.
Please refer to the Attribution and Valuation webinar for further clarification.
M9. Q: Is there a minimum number of members required in a region to support a PPS? (Archived 7/24/2017)
A: Performing Provider Systems must have a minimum of 5,000 attributed Medicaid beneficiaries a year in outpatient settings per Attachment I. In order to ensure a meaningful presence in the county that the PPS hopes to serve, a PPS must have at least 1,000 attributed members in the county AND a PPS must serve at least 5% of the total attributed members for that county. If a PPS does not have a meaningful presence in a county, that PPS will have the county removed from its service area and hence, the PPS will not be eligible to receive attribution from that county. The exceptions to this threshold rule are for Lewis and Hamilton counties, which have no minimum attributed membership required. In addition, the state reserves the right to alter these thresholds based on attribution results.
M10. Q: What is the DSRIP measurement population?
A: The population of Medicaid recipients attributed to the PPS constitutes the measurement population. The attributed Medicaid population will be used to calculate the process and outcome population metrics as well as overall project values for DSRIP. The protocol for identifying this population will be found in Attachment I to the STCs. The state has been working on possible ways to include measurement for the uninsured population, but the lack of standardized data confounds this, so most measures will be related to impact on Medicaid recipients.
M11. Q: If attribution valuation is a part of the PPS application approval done in DSRIP Year 0, what happens if a PPS greatly expands during the DSRIP program? (Revised 7/24/2017)
A: Attribution related to project valuation occurred during the application process in DY0. This prospective attribution value will serve as the fixed valuation denominator for the whole DSRIP project.
M12. Q: What is the Comprehensive Provider Attribution (CPA) report and the Individual Provider Attribution Report?
The purpose of the Comprehensive Provider Attribution (CPA) report is to:
- Provide the PPS with the member level detail of their attributed cohort
- Catalog all Medicaid providers who provided a service to a PPS´ attributed member
- Display the number of visits by provider for each attributed PPS member
The CPA report includes only a PPS´ attributed members and does not include members attributed to another PPS. It also includes member interactions with all Medicaid providers, not just member interactions with the PPS´ in-network providers. More information can be found on the DSRIP webpage here.
The purpose of the Individual Provider Attribution (IPA) report is to show each PPS how many attributed member counts each their providers drove at the individual provider level and the results are de-duplicated. Both the CPA and the IPA reports were released in April 2016.
|back to table of contents||top of section| |top of page|
N. Integrated Services (New 7/1/2016)
N1. Q: Where can more detailed information about DSRIP and integrated services be found? (New 7/1/2016)
A: More information about integrated services and integrated care in DSRIP can be found under Integrated Services on the DSRIP Webinars and Presentations webpage in the Integrated Services section. This includes the Integration of Primary Care and Behavioral Health Services presentation, along with the recording of the webinar, the FAQ and the billing matrix.
|back to table of contents||top of section| |top of page|
O. Project Plan & Support Team
O1. Q: Did PPS need to submit a DSRIP Project Plan application? If so, when was it due?
A: Yes. Submission of a formal DSRIP Project Plan was the final step in the DSRIP application process. Performing Provider Systems needed to submit their Project Plans to the state by December 22, 2014. This application process is now closed. The Final DSRIP Project Plan Application was submitted electronically through the DSRIP/Health Home Portal.
O2. Q: What needed to be contained in the DSRIP Project Plan?
A. The DSRIP Project Plan provided rationale for project selection including target population, strategies, specific milestones, goals, how project will change the system, how stakeholders are engaged in the process; description of project activities including outcome metrics; and justification of the project funding, including a detailed project specific budget.
Finalized versions of the DSRIP Project Plan application and Review Tool were made available on November 14, 2014. These documents indicated precisely what needed to be included in the DSRIP Project Plan, as well as how the Project Plans would be evaluated and scored.
O3. Q: Was there help available to assist providers with completing the DSRIP Project Plan application?
A: New York hired a contractor, KPMG, to serve as the DSRIP Support Team (DST). The role of the DST was to help Performing Provider Systems with technical assistance in developing their DSRIP Project Plan. In addition, the state allocated a portion of the DSRIP funding to assist Performing Provider Systems with their DSRIP Project Plan development in the form of DSRIP Project Design Grants. Project Design Grant awards were made on August 6, 2014 to 42 of the Emerging PPS. Some PPS merged and there were ultimately 25 PPS that submitted Project Plan applications on December 22, 2014. More information on these awards can be found at the Performing Provider Systems (PPS) website.
Funding from these design grants was used to prepare the DSRIP Project Plan application for participation in DSRIP. Recipients of these awards were expected to submit a DSRIP Project Plan application.
O4. Q: Could a group of providers come together and submit a DSRIP Project Plan even if they did not apply for the Project Design Grant? (Revised 8/28/2015)
A: Yes. A PPS applicant could have submitted a DSRIP Project Plan without having submitted a DSRIP Project Design Grant application. However, the proposed PPS would not have had access to planning funds or access to the DSRIP Support Team to help them with their DSRIP Project Plan application or prepare for DSRIP implementation.
Additionally, a new PPS applicant would have had to submit a letter stating its intent to form a new PPS to the New York State Medicaid Director via the DSRIP e-mail account (dsrip@health.ny.gov) Additionally, a new PPS applicant would have had to submit a letter stating its intent to form a new PPS to the New York State Medicaid Director via the DSRIP e-mail account (dsrip@health.ny.gov) before October 1, 2014. The letter needed to include the PPS Name, Lead Entity Information, Primary and Secondary Contacts for the new emerging PPS, as well as proposed counties of service for the entity. The new PPS was also required to submit a list of network providers (with the state providing a template upon receipt of the official letter) and a signed attestation stating that the providers listed in the applicant´s proposed network list have agreed to partner with the PPS. New applicants were responsible for setting up the necessary Health Commerce System (HCS) accounts to gain access to the online network tool and Project Plan application. Every PPS had to have HCS access in order to submit their partner networks by the time the network tool closed (to perform attribution for valuation) on December 1, 2014.
Furthermore, if the emerging PPS was an entity that was turned down for a Project Design Grant, the entity would still have had to submit all of the materials stated above as well as provide an explicit explanation to the state responding how it remedied the issues the state brought forth when not approving the applicant for the DSRIP Project Design Grant. Specific guidance would have been given to these applicants on a case-by-case basis.
O5. Q: Were there any signed Attestations required for the DSRIP Project Plan?
A: Yes. Project Plan Application Attestation: The PPS Lead submitted an attestation statement documenting that the information provided in the Project Plan application was accurate at the time of submission and that the PPS, if accepted into the DSRIP program, would cooperate fully with the state in the implementation and monitoring of this project and participate in the required Learning Collaboratives related to this project. If the Performing Provider System is receiving funds from the public DSRIP pool, it also provided a description of the IGT source identified for the project and attested that this IGT derives from local, public funds.
O6. Q: What type of clinical information was required in the DSRIP Project Plan application, if any?
A: Since DSRIP is about system transformation, it was important for Performing Provider Systems to identify the most critical structural and clinical issues in their service area that affect their performance as a system. In essence, the Performing Provider System needed more information than just clinical information to develop a successful application.
Performing Provider Systems needed to complete a current community health assessment including population demographics, types and numbers of medical, behavioral health and community service providers and services, cost profile, designation as Health Professional Shortage Area, mortality and morbidity statistics, and health disparities. Refer to the Community Needs Assessment Guidance and associated webinars for additional specifics (link below). The state assisted Performing Provider Systems by providing a significant amount of this information through the DSRIP Performance Data site. The community needs assessments required for hospitals do not provide the breadth of information required in DSRIP.
From this information, PPS needed to choose critical issues causing poor performance, which they aligned with their chosen DSRIP projects. These critical issues needed to be supported/defended in the application by an assessment of patient co-morbidities, patient characteristics, social system support, system capacity for primary care and disease management, and institutional issues such as finances, confounders to health care system improvement including fragmentation of services, competition, and assessment of regional planning issues.
O7. Q: What is the relationship between DSRIP application budget and the capital budget for state allocation? (Revised 7/1/2016)
A: Under Sections 8, 8-a, 8-b, and 9 of the Health Article VII bill (S.6914/A.9205) in the Governor´s 2014-15 budget, the Department of Health was awarded $1.2 billion over a period of seven years to establish a Capital Restructuring Financing Program (CRFP) that will support capital projects in an effort to strengthen and promote access to essential health services. The majority of funding is aligned with DSRIP and support projects that will improve infrastructure and other capital investments aimed at promoting integrated health systems and developing additional primary care capacity. Further information regarding capital funds were provided via the listserv.
O8. Q: What qualifies as capital under the budget section of the DSRIP Project Plan application?
A: In relation to the budget section of the DSRIP Project Design Grant, capital refers specifically to funding for "bricks and mortar" infrastructure and the capital cost portion of IT investment needed to achieve DSRIP-principled goals.
|back to table of contents||top of section| |top of page|
P. Project Plan Assessment
P1. Q: What is the role of the Independent Assessor?
A: The DSRIP assessor´s tasks include, but are not limited to:
- Creating an application and application review tool;
- Creating a process for a transparent and impartial review of all proposed project plans;
- Reviewing all proposed Project Plans and making project approval recommendations to the state using CMS-approved criteria;
- Assembling a Project Plan application review panel based on standards set forth in the DSRIP STCs;
- Convening a series of DSRIP learning collaboratives to share best practices and receive assistance in implementing DSRIP projects;
- Conducting a transparent and impartial mid-point assessment of project performance during the second year to determine whether the DSRIP project plans merit continued funding or need plan alterations;
- Assisting with the ongoing monitoring of performance and reporting deliverables for the duration of the DSRIP program.
P2. Q: Who was selected as DSRIP´s Independent Assessor?
A: The state announced the award of DSRIP Independent Assessor procurement to Public Consulting Group (PCG) Inc.
P3. Q: How were the submitted DSRIP Project Plan applications reviewed and evaluated for selection?
A: The state developed a standardized application review tool that the DSRIP Independent Assessor used to review DSRIP Project Plans and to ensure compliance with all terms, conditions and protocols agreed to between CMS and the state. The application and review tool (which included a project scoring guide) were made available for public comment for a 30-day period on September 29, 2014; the application was revised based upon public comments received. The application and review tool was approved by CMS in November, 2014 and finalized versions were posted to the DSRIP site on December 3, 2014. The review tool defined the relevant factors, assigned weights to each factor, and included a scoring for each factor. Each factor addressed the anticipated impact of the project on the Medicaid and uninsured populations consistent with the overall purpose of the DSRIP program.
After DSRIP Project Plans were submitted by Performing Provider Systems on or before December 22, 2014, the Independent Assessor conducted an initial screen to ensure that they met the minimum submission requirements. The Independent Assessor notified the Performing Provider System in writing of any initial questions or concerns identified with the provider´s submitted DSRIP Project Plan and provided a 14-day period for Performing Provider Systems to address these concerns. All submitted DSRIP Project Plans were posted for a 30-day public comment period.
The Independent Assessor used the review tool to score all submitted DSRIP Project Plans. After scoring, the state convened a panel of non-conflicted relevant experts and public stakeholders with significant health care transformation experience. The panel held an open public meeting to review the assessor´s recommendations. The Independent Assessor presented each DSRIP Project Plan with its score and recommendation for approval or rejection to the panel. The panel had the opportunity to accept, reject, or modify the Independent Assessor´s recommendation.
The Independent Assessor then forwarded the panel´s recommendations to the New York State Commissioner of Health regarding approvals, denials, or recommended changes to Project Plans. The Commissioner then had the opportunity to accept or reject the panel´s recommendations. Any deviations from the Independent Assessor´s recommendations needed to be explained to, and approved by, CMS, which maintain its own monitoring process of these reviews.
P4. Q: Can a DSRIP Project Plan be modified or changed during the 5 year period after it is approved?
A: No more than once a year, Performing Provider Systems may submit proposed modifications to an approved DSRIP Project Plan for state and CMS review. These modifications may not decrease the scope of the project unless they also propose to decrease the project´s valuation. Removal of any PPS partner organization requires a proposed modification, and removal of any such lower performing member must follow the required governance procedures including progressive sanction requirements.
Also, if a DSRIP PPS has not successfully met its milestones, modifications may be allowed with the approval of the state and CMS. Based on the information contained in the Performing Provider System´s semiannual report or other monitoring and evaluation information collected, the state or CMS may identify particular projects as being "at risk" of not successfully completing its DSRIP project in a manner that will result in meaningful delivery system transformation.
|back to table of contents||top of section| |top of page|
Q. DSRIP Project Valuation
Q1. Q: What is DSRIP Project Valuation?
A: The DSRIP project valuation was calculated by the state with the assistance from the Independent Assessor according to the methodology described in Attachment I to the Special Terms and Conditions. The maximum valuation for a project was calculated based on the projects chosen, the external valuation benchmark, the application score and the number of Medicaid beneficiaries attributed to each project.
A maximum valuation for each DSRIP application was calculated based on a formula described in Attachment I. The maximum application value represents the highest possible financial allocation a Performing Provider System can receive for their plan over the duration of their participation in the DSRIP program. Performing Provider Systems may receive less than their maximum allocation if they do not meet metrics and/or if DSRIP funding is reduced because of the statewide penalty.
Q2. Q: What is a Project Index Score?
A: The value of a single project is expressed as an index score. Project index scores are based upon a grading rubric that evaluated the project´s ability to transform the health care system. The state assigned an index score to each project based on the grading rubric and the given project´s relative value to the other projects in the state´s menu. The final project index scores are presented in decimal form for valuation purposes and are available to providers in the DSRIP Project Toolkit. https://www.health.ny.gov/health_care/medicaid/redesign/docs/program_funding_and_mechanics.pdf
Q3. Q: Can the state provide a calculation example for a DSRIP Project Plan Valuation?
A: There is an example of a DSRIP Project Plan valuation available in Attachment I on the DSRIP website. Additionally, the DSRIP overview PowerPoint on the DSRIP website also offers a detailed walk-through of the valuation process using a specific example. Examples were provided subsequent to the creation of Project 2.d.i. in the attribution and valuation webinar. The three presentations are provided within the links. Also see proceeding Valuation example.
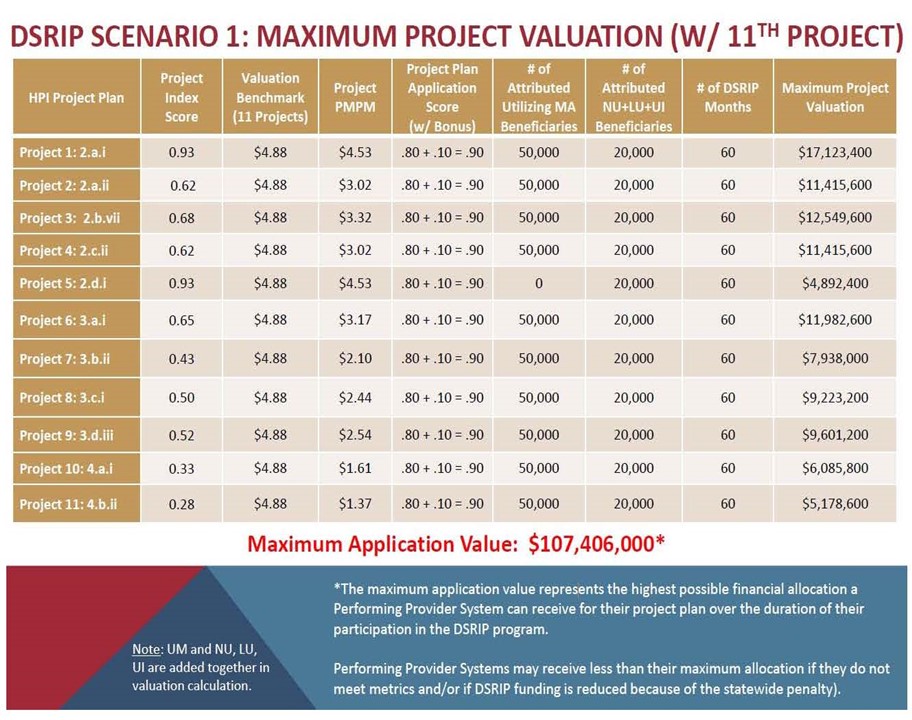
|top of section| |top of page|
R. DSRIP Reporting & Payments
R1. Q: How will PPS be assessed with regards to pay for reporting measures, and what are they required to report on?
A: In cases where the measure type is Pay for Reporting (P4R), Performing Provider Systems can earn incentive payment for successfully reporting the measures the PPS is responsible for reporting to NYS DOH within the timeframes for each Measurement Year (MY). Some of these measures are claims- based, while others will require medical records review and chart abstraction. Measures which are DOH responsibility for reporting will be credited to the PPS in P4R situations based upon Medicaid claims and other population health measures. All Domain 4 measures are P4R for the entire DSRIP Project period and it is expected that PPS will earn all AVs in Domain 4 due to limited PPS responsibility in measure reporting. Domain 2 and 3 measures that are P4R during the initial project years convert to P4P over the course of the DSRIP initiative. The details on the P4R measures can be found in the DSRIP Measurement and Reporting Manual, as well as in Attachment J in the official CMS waiver documents.
R2. Q: Can you please clarify how Domain 4 projects will be evaluated against their requirements? Do all requirements have to be met for all collaborators for Domain 4 projects? What are PPS reporting on in Domain 4?
A: Domain 4 is meant to enhance community collaboration regarding population health. DOH entities already have active initiatives aligned with Domain 4 projects, so PPS should look to join in these efforts. Domain 4 requirements are all self-reported per milestones communicated in the PPS application. Similar to the Domain 2 and 3 projects, PPS will be expected to update progress at a project-wide level via Quarterly Reports in MAPP.
The Domain 4 Reference Guide has been released to PPS. The "Reference Guide for DSRIP Domain 4 Projects Implementation Planning" was created by the NYS DOH Office of Public Health (OPH) and Office of Health Insurance Programs (OHIP). This document is part of the ongoing series of webinars and documents intended to help guide PPS through their project planning and implementation process. The purpose is to provide considerations on evidence-based project activities, milestones and metrics, and resources that PPS may choose to incorporate into their implementation planning efforts for DSRIP projects within Domain 4.
R3. Q: Can a PPS budget be modified in future reporting periods?
A: Budget projections for each DSRIP year need to be finalized within the DY1 Q1 Quarterly Report submission. Changes will only be allowed under extenuating circumstances; however, PPS will have the opportunity in the reporting structure to explain variations.
R4. Q What Domain 1 Achievement Values (AVs) is the PPS held accountable to in DY1? (Archived 7/24/2017)
A: DY1 Q2 is based on 6 AVs that come from the Governance, Workforce, Cultural Competency/Health Literacy, Financial Sustainability/Quarterly Progress Reports/Project Budget & Flow of Funds and Patient Engagement Speed measures. DY1 Q4 will include these same AVs. The AV for workforce prior to the updates will be based on organizational updates and work plan steps.
R5. Q: Will PPS be required to submit lists of participating providers for each project? (Archived 7/24/2017)
A: PPS will be required to identify the network providers that will be participating in each project as part of the October quarterly reporting process (due October 31, 2015). The number of total providers listed in each category must match the scale and speed table commitments from the PPS´s DSRIP application.
R6. Q: For tracking patient engagement, will the Independent Assessor (IA) audit the PPS or the specific provider?
A: PPS are required to submit supporting evidence that demonstrates active engagement based on application commitments. The IA reserves the right to audit any evidence of achievement towards active engagement commitments.
R7. Q: How will "actively engaged" be tracked and reported?
A: It is the PPS´s responsibility to track actively engaged patients. The Independent Assessor can audit actively engaged patients as part of program oversight.
R8. Q: How is the actively engaged commitment for a PPS influenced by other PPS operating in the same region and engaging the same patient population and how has the DOH mitigated this issue? (New 7/1/2016)
A: When PPS made their original "actively engaged" commitments, it was done without consideration of other PPS and now there is the potential for "double counting". The DOH has taken several steps to mitigate the issue:
- Two PPS working with the same provider on the same project can only count a given Medicaid member as "actively engaged" for one of the PPS (i.e., cannot double-count actively engaged members between PPS with the same provider for the same project). However, this does not apply when the same member is seen by different providers.
- For PPS in the same region that have overlapping providers and projects, the DOH calculated "actively engaged discounts" that will be applied to the commitments made by PPS. Where the "actively engaged discounts" are applied, PPS will have a lower target than their original commitment.
The IA will be cognizant of instances where two DSRIP partners/providers do not overlap, but between the partners a Medicaid member is reported twice for the same project across multiple PPS. In these cases, the member count would be included by both PPS. The IA will be in a stronger position to make this determination if PPS caveat actively engaged members with a unique provider identifier when submitting active engagement rosters. This will allow the IA to determine if the member has been activated by different providers along different portions of the continuum of care."
R9. Q: Will a PPS receive any extra financial benefit if they accelerate their timeline for Domain 1 AVs and achieve the AV sooner?
A: PPS were rewarded for aggressive commitments to project speed and scale in the scoring of the application and the valuation process. There is no additional financial performance award for Domain 1.
R10. Q: If project speed is met early, how is the AV determined and what is the impact on PPS payments?
A: The PPS becomes eligible for the high performance fund, and that AV becomes non-applicable for all periods after the measure was met.
R11. Q: How are PPS held accountable to the quarterly reports for those that do not drive payment, since the payoff is associated with every other report (at six month intervals)?
A: How the PPS fares on the reports that drive payment will be the determining numbers for payments. The quarterly reports that do not drive payments directly will be evaluated by the Independent Assessor for completeness. The Independent Assessor has indicated that unsatisfactory quarterly reports (also in non-payment times) may still have an effect on performance payments, depending on the severity of the assessed gaps.
R12. Q: In what quarter will PPS report on major system change requirements that are required to take no more than the first two years? (Archived 7/24/2017)
A: PPS will report on this for DY2 Q4, which is the quarter ending March 30th, 2017.
R13. Q: For the workforce milestone that requires documentation of a compensation and benefit analysis report, signed off by the PPS workforce governance body, subsequent quarterly reports will require an update on the implementation of your workforce transition roadmap, including updates on compensation and benefits. What is required in these updates, and will the PPS have to do this update every quarter or is it sufficient if, once the analysis is complete, they then they just report on progress?
A: The PPS needs to be sensitive to changes and able to accommodate for changes in their analysis when necessary. If none of the starting premises is altered, then it is unlikely that the analysis has to be updated, and an update on progress will likely suffice.
R14. Q: Will providers be required to submit data and/or progress reports? If so, how often and will it be required to be submitted in a secured manner?
A: Providers will be required to submit progress reports quarterly. The reports will be submitted using the standardized reporting form in MAPP approved by the state and CMS.
R15. Q: How will the state evaluate the providers´ DSRIP project data after it is collected and submitted?
A: Upon the approval of each DSRIP Project Plan, project specific metric baselines will be identified. In addition, the target high performance goal for each metric will be established. From those baselines, PPS will have to reach the pre-defined goal/benchmark targets in given metrics. Some metrics will be met based upon reporting specific data; some metrics will be met based upon actual progress to a predefined goal. This predefined goal will generally be closing the gap between current PPS performance and the statewide goal. More information on these targets and calculations can be found in the DSRIP Measure Specification and Reporting Manual, available on the DSRIP website.
R16. Q: Are DSRIP payments tied to the performance of the Performing Provider System?
A: Yes. DSRIP payments are tied to a PPS´s performance. DSRIP is specifically engineered to reward measurable outcomes. Each Performing Provider System will have process and outcome metric milestones that must be met in order to receive DSRIP payments. For some outcome metrics, success will be considered closing part of the gap of the provider compared to the goal.
R17. Q: What is the difference between a Process Milestone and an Outcome Milestone?
A: A process milestone is a milestone that denotes changes that are being made to the system such as training programs, realignment of clinics, adoption of appropriate EHRs, creating patient registries, etc. An outcome milestone is evidence of an actual change in the health care system such as improved control of diabetes or blood pressure or reduction in avoidable hospital use.
R18. Q: What are the criteria for achieving incentive payments?
A: At least two times per year, Performing Provider Systems seeking payment under the DSRIP program shall submit reports to the state demonstrating progress on each of their projects as measured by project- specific milestones and metrics achieved during the reporting period. The reports shall be submitted using the standardized reporting form in MAPP approved by the state and CMS. Based on the reports, the state will calculate the incentive payments for the progress achieved according to the approved DSRIP project plan. The Performing Provider System shall have available for review by the state or CMS, upon request, all supporting data and back-up documentation. These reports will serve as the basis for authorizing incentive payments to Performing Provider Systems for achievement of DSRIP milestones.
Incentive payments will be calculated based upon the progress of process milestones/metrics and outcome milestones/metrics. The value of each type of metric type is noted below. As the projects progress, less payment will be allocated to process milestones/metrics and more will be allocated to outcome milestones/metrics. Some payments will be based on submitting required reporting only (Pay for Reporting) and others will be based on attaining specific outcome targets (Pay for Performance). Please note that the DSRIP performance payment distribution (highlighted in the chart below) for the duration of the DSRIP program is based on the overall application value, not the valuation of individual projects.
| Metric/Milestone Domains |
Performance Payment* |
Year 1 (CY 15) |
Year 2 (CY 16) |
Year 3 (CY 17) |
Year 4 (CY 18) |
Year 5 (CY 19) |
|---|---|---|---|---|---|---|
| Project progress milestones (Domain 1) |
P4R/ P4P | 80% | 60% | 40% | 20% | 0% |
| System Transformation and Financial Stability Milestones (Domain 2) |
P4P | 0% | 0% | 50% | 72% | 93% |
| P4R | 20% | 40% | 10% | 8% | 7% |
* P4P is pay for performance; P4R is pay for reporting.
| Metric/Milestone Domains |
Performance Payment* |
Year 1 (CY 15) |
Year 2 (CY 16) |
Year 3 (CY 17) |
Year 4 (CY 18) |
Year 5 (CY 19) |
|---|---|---|---|---|---|---|
| Project progress milestones (Domain 1) |
P4R/ P4P | 80% | 60% | 40% | 20% | 0% |
| Clinical Improvement Milestones (Domain 3) |
P4P | 0% | 30% | 50% | 70% | 90% |
| P4R | 20% | 10% | 10% | 10% | 10% |
* P4P is pay for performance; P4R is pay for reporting.
| Metric/Milestone Domains 4 |
Performance Payment* |
Year 1 (CY 15) |
Year 2 (CY 16) |
Year 3 (CY 17) |
Year 4 (CY 18) |
Year 5 (CY 19) |
|---|---|---|---|---|---|---|
| Project progress milestones (Domain 1) |
P4R/ P4P | 80% | 60% | 40% | 20% | 0% |
| Population health Outcome Milestones (Domain 4) |
P4R | 20% | 40% | 60% | 80% | 100% |
* P4P is pay for performance; P4R is pay for reporting.
R19. Q: How does the state´s High-Performance Fund work?
A: A portion of DSRIP funds will be set aside to reward high performing systems. The high performance fund will be "seeded" with 3 percent of the available DSRIP performance funding and will also include "deposits" from performance payments surrendered by PPS´ that do not meet their performance targets. The total amount of funding paid out of the high performance fund shall be based on actual high performance goals met and will be distributed to qualifying providers based on meeting a specific set of Domain 2 and 3 metrics identified as a high performance metrics by the state, with input from the quality and measures committee.
Additional funds will be set aside within each fund for Performing Provider Systems reaching stretch/ bonus level targets for significant improvement in avoidable hospitalization reduction for their attributed behavioral health population.
For additional details on the DSRIP High Performance Fund, please refer to Attachment I
R20. Q: Will the state provide tools, baseline/benchmark data, and progress & feedback report educational materials to providers? (Revised 7/24/2017)
The state will support the projects in a number of ways:
- Dedicated KPMG/PCG Account Support team working 1:1 with PPS to discuss progress, challenges and strategies to achieve milestones and metrics as well as best processes to approach DOH with questions,
- Bureau Mail Log (BML) that encourages, accepts, tracks and answers any DSRIP related questions from PPS and stakeholders.
- Quarterly ALL PPS meetings to discuss and clarify currently relevant DSRIP program protocols and progress benchmarks
- Annual Learning Collaboratives as required by the STCs where PPS can showcase collaborative, transformational and innovative DSRIP activities.
- MAPP Dashboard updates that reflect adjudicated claims performance tracking, benchmark, gap to goal and High-Performance goals.
- MAPP Dashboard payment scorecard to track achieved payments to date as well remaining attributed payment value.
- PCG Independent Assessor is also responsible for reviewing the required and submitted PPS Quarterly reports throughout DY1-DY5 and issuing feedback on reported progress and performance related to claims based measures and non-claim based measures.
- Email communications to PPS on updated policies, protocols as well as links, supporting documents, resources and references available both on the DSRIP website and the PPS Digital Library
- NYS DOH DSRIP program also hosts and conducts webinars on policies, procedures, updates, educational and informational sessions on a breadth of DSRIP organizational, project and VBP related topics.
R21. Q: What are the intergovernmental transfer (IGT) risks for public providers?
A: Public providers do not have any risk associated with IGTs. If public providers achieve performance measures then they get their full award and make the full IGT required (which includes the safety net IGT). If public providers do not achieve performance measures then they are under no obligation to provide an IGT.
R22. Q: What is the role of the DSRIP Independent Evaluator?
A: The DSRIP Evaluator will conduct an interim and final summative statewide evaluation of the DSRIP program. The goals of the interim and summative statewide evaluations will be to examine the effect of DSRIP activities on achieving the state goals of (1) safety net system transformation at both the system and state level; (2) accountability for reducing avoidable hospital use and improvements in other health and public health measures at both the system and state level; and (3) efforts to ensure sustainability of delivery system transformation through leveraging managed care payment reform.
R23. Q: What is the role of Managed Care Organizations in DSRIP?
A: One of the goals of the DSRIP program is focused on ensuring sustainability of delivery system transformation through leveraging managed care payment reform. To do so, the state will reform managed care contracts to promote DSRIP objectives. The state will accomplish this by developing and executing payment arrangements and accountability mechanisms with its managed care contractors, ensuring that managed care payment systems recognize, encourage and reward positive system transformation. This includes, but is not limited to, promoting the establishment and continuation of integrated service delivery systems, procedures to reduce avoidable hospital use, as well as to ensure improvements in other health and public health measures.
In the broader context of Medicaid redesign, one of the core goals of MRT was to end Medicaid fee-for-service by moving all populations and services into managed care. Managed Care Organization (MCO) can help the state in achieving its DSRIP goals by aligning payments to PPS and by making sure that Medicaid beneficiaries have access to the full spectrum of health services that produce better health outcomes.
In the future state, meaning the NYS health system after the DSRIP program, managed care companies will pay PPS directly for a portion of the care on a PMPM basis for the people whose care the PPS is responsible for maintaining. This future state would be a true value and performance based health care system where silos across the health system have been broken down and where shared accountability exists at the provider level. The MCO payments to PPS would include not only traditional health care providers, but other non-traditional providers that impact health outcomes (like supportive housing providers).
The Department´s Value-based Payment roadmap was approved by CMS July 22, 2015 and is currently being revised.
|back to table of contents||top of section| |top of page|
S. IT Communications & Investments
S1. Q: Is the state working with and/or endorsing specific external IT vendors?
A: The state is not endorsing any particular external vendors at this time. There will be data feeds of member files and claims data initially. The PPS will need to take those files and feed them into their software and work with their own software vendor to meet their needs. In the latter part of the year, the same data will be available in MAPP and the PPS can work with their own IT vendor regarding how to pull the data to populate their own system for the PPS to use.
S2. Q: When did the Quarterly Reports go live in the MAPP tool?
A: MAPP Quarterly Reports were scheduled to go live on July 1, 2015; Q1 reports were initially due July 31, 2015, but was pushed back to August 7th to address technical issues with MAPP. For consistency, formatting has been kept as close as possible to the June Implementation Plan, and training documentation and webinars were made available to the public.
S3. Q: What are the state´s expectations around the implementation of EHR or other IT platforms being integrated into CBOs? Will interconnectivity and real time notification be expected at these locations?
A: Connectivity between providers is a key component to the DSRIP program, as it will better serve the population. It is expected that, where needed, the PPS will support CBOs to connect to the integrated network of care.
S4. Q: What sort of communication systems will be needed to make this program run effectively?
A: PPS Project Plans must include provisions for appropriate data sharing arrangements, including connections to RHIOs, that drive towards a high-performing PPS, while appropriately adhering to all federal and state privacy regulations. The PPS plan must include a process for rapid cycle evaluation (RCE) and indicate how it will tie into the state´s requirement to report to DOH and CMS on a rapid cycle basis.
S5. Q: Does the state offer support for IT investments that are needed to help achieve real-time secure data sharing and clinically integrated network formation?
A: The capital cost portion of IT investment needed to achieve DSRIP-principled goals is an eligible cost within the scope of a Capital Restructuring Financing Program project, which can also be used for bricks and mortar. The state expects PPS to use some portion of capital funds and performance payments to further develop HIT capabilities, especially in the early stages of implementation as networks develop interoperability amongst their partners.
|back to table of contents||top of section| |top of page|
T. Workforce Strategy
T1. Q: Is there a plan for care management agencies to grow to meet the demand for care management under DSRIP?
A: Yes. There is a plan for care management agencies to grow to meet demand under DSRIP program. The overarching DSRIP goal of a 25% reduction in avoidable hospital use (emergency department and admissions) will result in the transformation of the existing health care system - potentially impacting thousands of employees. This system transformation will create significant new and exciting employment opportunities for appropriately prepared workers. PPS Project Plans must identify all impacts on their workforce that are anticipated as a result of the implementation of their chosen projects, as well as a workforce plan for repurposing jobs that will free up as we lower avoidable hospitalization.
One clear area to repurpose those jobs will be to care management. Training and outreach for care management will be needed. The state is working with health homes to have them staff up for the demands of DSRIP, HARPs, and the community transition activities related to Olmstead.
|back to table of contents||top of section| |top of page|
U. Health Home Infrastructure
U1. Q: Previous communication from the state indicated that significant funding was planned to enhance the existing health home infrastructure. What is the current status and plans for infrastructure build out? (Revised 7/24/2017)
A: The Centers for Medicare and Medicaid Services (CMS) approved a State Plan Amendment (SPA) authorizing the State to distribute $190.6 million dollars of Health Home Development Funds (HHDF) authorized in the MRT 1115 Waiver Amendment. HHDF are to be utilized to fund health home infrastructure within four categories: Member Engagement and Health Home Promotion, Workforce Training and Retraining, Clinical Connectivity and Health Information Technology (HIT) Implementation, Joint Governance/Technical Assistance. Funds were distributed through a temporary rate add-on to per member per month (PMPM) Health Home claims and were paid to lead designated Health Homes in quarterly increments from March 2015 through December 2016.
|back to table of contents||top of section| |top of page|
V. Additional DSRIP Funds (New 8/28/2015)
V1. Q: Will performance standards be the same for the High Performance Fund and the Safety Net Equity Fund?
A: No. The High Performance fund is based on a percentage of exceeding project metrics and benchmarks. The Safety Net Equity fund is intended to address inequity for Non-Public, Safety Net PPS with lower performance PMPMs due to the attribution for valuation logic.
V2. Q: Will the Safety Net Guarantee payments be equally spread across the 5 years or be held to the same percentages as the project revenue spread over the 5 years?
A: The payments will be equally spread across the 5 years.
|back to table of contents||top of section| |top of page|
W. Data Sharing and Security (Revised 7/24/2017)
All information / questions about data sharing and data security have been updated in 2017. For updated information and policies, please contact the NYS DOH Division of Systems, Security and Privacy Bureau via email at DOH.SM.Medicaid.Data.Exchange@health.ny.gov
Other Topics (Archived 7/24/2017)
W1. Q: How do the definitions here apply to modern bulk or virtual storage pools such as NAS/SAN disk arrays? Is the use of commercial or certified secure deletion programs an allowable "Purge" option?
A: Should a NAS/SAN disk array be shared with other servers, the host server should implement an encrypting file system on its NAS/SAN volume, to protect the data at rest, wherever it may reside in the array. NYS standards at the following link address methods and tools to securely erase sensitive data, such as PHI.
Data Sharing for New Corporation (NewCo) (Revised 7/24/2017)
W2. Q: Is a NewCo required to store data at one of the co-lead locations, or can the NewCo set up a secure server to store data compliant with all policies and laws?
A: Any questions regarding data storage for a NewCo should be directed to the Division of Systems, Security and Privacy Bureau at doh.sm.Medicaid.Data.Exchange@health.ny.gov
W3. Q: Can the Department offer guidance to those NewCos that may consist of multiple partners, which are considered equally contributing to the composition of the NewCo. (Revised 7/24/2017)
A: Any questions regarding the NewCo composition and NewCo DEAA Amendment should be directed to the Division of Systems, Security and Privacy Bureau at doh.sm.Medicaid.Data.Exchange@health.ny.gov
W4. Q: Where can I find more detailed information about DSRIP Data Sharing and Security? (Archived 7/24/2017)
A: More information about DSRIP Data Security and Information Sharing may be found under Data Security on the DSRIP Webinars and Presentations webpage.
A more detailed DSRIP Data Sharing FAQ can be found here or contact the Division of Operations and Security at doh.sm.Medicaid.Data.Exchange@health.ny.gov
|back to table of contents||top of section| |top of page|
X. Opt-Out Process
X1. Q: What is the opt-out process?
A: The opt-out process refers to the DSRIP consent process where unless the Medicaid member formally opts-out of DSRIP data sharing, they are considered participating in data sharing. To "opt-out" means electing NOT to permit the sharing of PHI and other Medicaid data held by the Department to the PPS and its partners. DSRIP Performance measures will include opt-out members in the numerators and denominators, but drill-down information to these members will not be available. Members can opt-in or out of data sharing at any time.
X2. Q: What is the status of those Medicaid beneficiaries who do not respond to the opt-out? (Revised 8/31/2018)
A: Medicaid beneficiaries are considered opted-in to PPS data-sharing unless they call the Medicaid Call Center to opt-out or return the opt-out form. For mailers that come back as undeliverable, another attempt will be made if a better address is found; if not, the member will be placed in an unreachable state and their data will not be shared.
X3. Q: How will the PPS be notified of Medicaid members who do not want their data shared?
A: Those members who have selected to opt-out of DSRIP data sharing will not be refreshed in subsequent releases of the Member Roster files and will be identified to the PPS on a separate PHI Discontinued File.
X4. Q: Can the Department share the Opt-Out letter with the PPS to educate their beneficiaries? (Archived 7/24/2017)
A: Yes. The letter was shared with the PPS after it was finalized. It can be found on the DSRIP website
The Department is working towards finalizing the initial large-scale mailing of the Opt-Out letter by April 2016. Monthly mailings will continue thereafter to newly eligibility members.
X5. Q: Why does Medicaid want to share NYS Medicaid data with the Delivery System Reform Incentive Payment (DSRIP) program Performing Provider Systems (PPS)?
A: The PPS are responsible for working to improve health outcomes for their Medicaid patients, who are seeing the physicians and providers in the PPS. Data sharing is key for effective collaboration among the lead PPS and related network partners for providing and coordinating services to Medicaid members. Medicaid members´ information contained in the Medicaid Data Warehouse (MDW) will be shared with the PPS and its partners. By doing so, the PPS providers can do a better job coordinating care and services to those most in need and also transform how services are delivered for larger patient groups who might have the same needs (´Population management´).
X6. Q: What information will be shared under the DSRIP program?
A: The Department of Health will provide data sets containing member information via a Medicaid Member roster, a claims extract file, a comprehensive provider attribution report and a PHI Discontinued report to the PPS. Following completion of the initial Opt-Out phases, the Member roster will provide a list of Medicaid members (who have not opted out) that are attributed to the PPS. The claims extract file will provide a list of past claims and encounters for those members who have not opted out, with additional more-specific information (including providers and treatment codes). Information about a Medicaid member´s substance use diagnoses and treatment, however, is not included in this PPS claims information. By federal law, a person needs to give affirmative consent for this specific substance abuse diagnosis and treatment information to be released. The PHI discontinued roster will serve to formally notify PPS those members who have opted out and no longer want their PHI shared with the PPS or downstream partners, as the last point in time their member information (in the form of only a Medicaid Member Identification number) will be shared.
X7. Q: Where can more information regarding the opt-out process be found?
A: More information, including an Opt-Out FAQ can be found here.
Claims Data
X8. Q: If a PPS gets claims data for all attributed patients, does that mean the PPS Lead will know which patients are attributed to the PPS? How will new Medicaid members be reflected?
A: MAPP will provide both a Member Roster and a claims extract file to the PPS. The Member Roster will provide a list of members attributed to the PPS. Contact DOH for exact file contents and related information.
X9. Q: What patient information is included in the claims data?
A: MAPP will provide both a Member roster and a claims extract file to the PPS. The Member roster will provide a list of members attributed to the PPS and for each member include the member´s name, birthday, member´s county code, member address, member contact number, member´s Medicaid identification number and gender. The claims extract file will provide a list of claims for the attributed members and will include the following PHI info on the member: member´s name, birthday, member´s county code, member´s Medicaid identification number and gender.
X10. Q: How will these claims data affect the data in Salient? Will there be PHI in Salient data?
A: The Department intends to provide PHI through Salient Interactive Miner (SIM) and Salient Performance Dashboards for authorized users in the PPS. Salient is working with the Department to determine the requirements necessary for PHI views in SIM and to develop a timeline for access (access was granted on January 29, 2016). SIM and Performance Dashboards will not expose member level data for members who have opted-out. PPS users will still have the ability to view performance measures at the PPS (summary) level that include members who have opted out. No drill down to opted out members will occur.
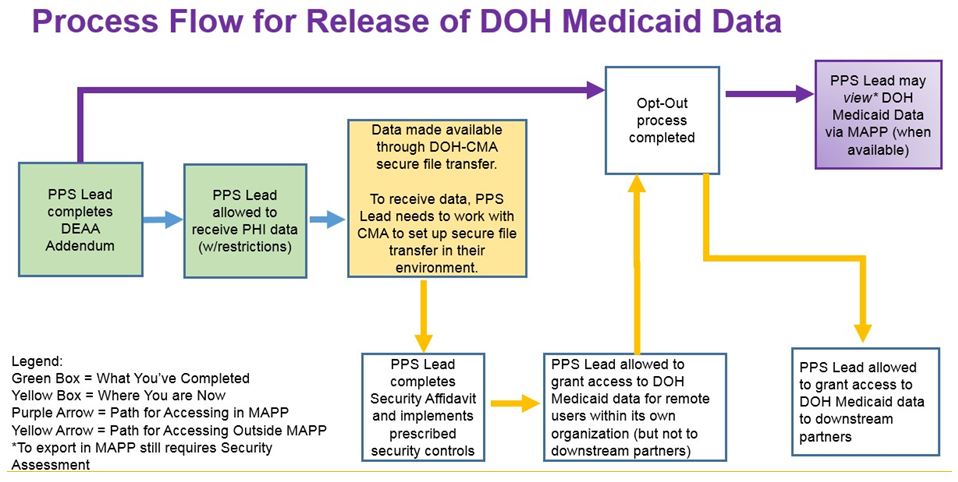
|top of section| |top of page|
Y. Medicaid Analytics Performance Portal (MAPP) & 2-Factor Authentication (2FA)
Y1. Are there any other IDs that will be accepted in lieu of a NYS DMV issued identification? (New 7/1/2016)
A: Yes, you can get MAPP access with an out-of-state license. In these instances, the MAPP user will work with their organization´s HCS Coordinator directly for authentication.
Y2. Q: Will the Department expand MAPP user slots per PPS?
A: Not at this time. The Department has expanded the MAPP user slots available to each PPS on multiple occasions since MAPP´s inception and continues to accept feedback from PPS regarding use based requests. If a PPS requires an update to understand their current MAPP users they may request this information via the DSRIP email address: dsrip@health.ny.gov
Y3. Q: Will MAPP permit exports of the list of patient data including PHI for leads and partners in the fall after 2FA is added?
A: Yes. MAPP will have the capability to allow exports of PHI data from MAPP for authorized users and also allow view only access to patient data based on our Performance Module dashboards. Any MAPP user who requests export ability of PHI in MAPP will be considered a point of access within your PPS requiring execution of the System Security Plan workbooks and Security Assessment Affidavit, and proceeds the opt-out process. PPS granting view-only access to patient data within MAPP will not be required to complete a Security Assessment for those MAPP users approved for this access by their Gatekeepers.
|back to table of contents||top of section| |top of page|
Z. Mid-Point Assessment
Z1. Q: What is the Mid-Point Assessment?
A: The Mid-Point Assessment is a required component of the New York Delivery System Reform Incentive Payment (DSRIP) Program as identified in Section VIII. 11.d. of the Special Terms and Conditions (STCs) of the 1115 Waiver that governs the DSRIP Program. The requirements of the Mid- Point Assessment are further detailed in Section VI.d. in Attachment I to the STCs.
Z2. Q: What are the requirements of the Mid-Point Assessment? (Revised 7/24/2017)
A: The Mid-Point Assessment requirements indicated that at a minimum, the following elements were to be assessed:
- Compliance with the approved DSRIP project plan, including the elements described in the project narrative;
- Compliance with the required core components for projects described in the DSRIP Strategies Menu and Metrics, including continuous quality improvement activities;
- Non-duplication of Federal funds;
- An analysis and summary of relevant data on performance on metrics and indicators to this point in time;
- The benefit of the project to the Medicaid and uninsured population and to the health outcomes of all patients served by the project (examples include number of readmissions, potentially preventable admissions, or adverse events that will be prevented by the project);
- An assessment of project governance including recommendations for how governance can be improved to ensure success. The composition of the performing provider system network from the start of the project until the midpoint will be reviewed. Adherence to required policies regarding management of lower performing providers in the network, as described in Section X of Attachment I, will be reviewed with a special focus on any action with regard to removing lower performing members prior to DYs 3, 4, and 5. (Note: Modifying PPS´ coalition members requires a plan modification);
- The opportunity to continue to improve the project by applying any lessons learned or best practices that can increase the likelihood of the project advancing the three-part aim; and
- Assessment of current financial viability of all lead providers participating on the DSRIP project.
Z3. Q: What is the process to review the implementation plans? (Revised 7/24/2017)
A: The Independent Assessor (IA) conducted the Mid-Point Assessment consistent with the requirements outlined in the STCs and Attachment I. The Mid-Point Assessment focused on the progress made by the PPS through the end of the first quarter of DSRIP Year 2 towards establishing the necessary organizational foundation and towards the implementation of the project requirements consistent with the approved DSRIP Project Plan (inclusive of DSRIP Application and DSRIP Implementation Plan). The IA used the following data sources to conduct the assessment: Approved DSRIP Project Plan Applications, PPS Quarterly Report Submissions - DY1, Q1 through DY2, Q1 and claims and non-claims data for P4R/P4P measures.
Z4. Q: What data sources will be used for the Mid-Point Assessment? (Revised 7/24/2017)
A: The Independent Assessor conducted the Mid-Point Assessment using data sources that were available at the time of the assessment and worked to minimize the amount of additional reporting required by the PPS. The primary data sources used in the Mid-Point Assessment were:
- Approved DSRIP Project Plan Applications
- PPS Quarterly Report Submissions - DY1, Q1 through DY2, Q1*
- Claims and non-claims data for P4R/P4P measures
The Independent Assessor used the available data to determine if the PPS were implementing the projects in accordance with their approved DSRIP Project Plans and assessed PPS progress towards meeting project implementation milestones.
*Please note that the Mid-Point Assessment was based on the PPS efforts through the DY2, Q1 PPS Quarterly Report to accommodate the timelines necessary to ensure the completion of all Mid-Point Assessment tasks prior to the start of DY3. While the Independent Assessor did not consider the PPS progress through DY2, Q2, PPS were able to use the progress that had been demonstrated through their DY2, Q2 PPS Quarterly Report to support their responses to the Independent Assessor recommendations or as the basis for the PPS recommendations submitted to the Independent Assessor.
Z5. Q: How will the Mid-Point Assessment be scored? (Revised 7/24/2017)
A: The Independent Assessor assigned a score to the overall DSRIP Project Plan for each PPS and to the individual projects in the PPS Project Plan. The scoring for the overall DSRIP Project Plan was evaluated for compliance with requirements set forth in the STCs and Attachment I as well as the plans defined by the PPS in the DSRIP Project Plan Application. Further details on mid-point assessment scoring and recommendations can be found on the DSRIP website here.
Z6. Q: What will be done with the Independent Assessor´s Mid-Point Assessment recommendations? (Revised 7/24/2017)
A: The Independent Assessor has completed its Mid-Point Assessment review and released its recommendations for public comment; the PPS had the opportunity to submit responses to the Independent Assessor´s recommendations. The Independent Assessor submitted a set of final recommendations to DOH based on the initial recommendations made by the Independent Assessor, the public comments received through the 30-day comment period, and the recommendations submitted by the PPS. DOH reviewed all recommendations submitted by the Independent Assessor and put forth a final set of recommendations for review by the Project Approval and Oversight Panel (Panel). The Panel convened to review the recommendations put for the by the Independent Assessor for the Mid-Point Assessment, focusing on a review of the recommendations to modify, consolidate, or discontinue DSRIP Project Plans. The Panel had the ability to Accept, Accept with Modifications, or Reject the recommendations made by the Independent Assessor. Following the conclusion of the Panel meetings to review the recommendations set forth through DOH, the final recommendations were compiled and presented to the Commissioner of Health. Consistent with the approach implemented for the DSRIP Project Plan Application scores, the final recommendations from the Commissioner of Health were submitted to CMS for final approval.
Further details can be found on the DSRIP website here.
Z7. Q: What is the timeline for implementing Mid-Point Assessment project plan modifications? (Revised 7/24/2017)
A: PPS had two months from the time the final recommendations were submitted by the Commissioner of Health to implement the recommended changes to the DSRIP Project Plans for the start of DY3. All recommended DSRIP Project Plan modifications were to be implemented for the start of DY3 to position the PPS for success as funding shifts from Domain 1 infrastructure and Domain 2 and 3 pay for reporting (P4R) to pay for performance (P4P).
The Independent Assessor monitored the PPS´ implementation efforts for the required modifications to the DSRIP Project Plans to ensure that they had the required modifications. In the event that the Independent Assessor determined that a PPS had not modified the project plan as required, the Independent Assessor submitted further recommendations to the Project Approval and Oversight Panel. These recommendations included:
- Suspension of the PPS project and associated funding; or
- Termination of the PPS project plan and funding
Z8. Q: Were PPS allowed to remove network partners at the time of the Mid-Point Assessment? (Revised 7/24/2017)
A: In addition to the recommendations submitted by the PPS for the DSRIP Project Plan, the PPS also included requests for modifications to their PPS network, including the removal of network partners. The modifications to the PPS network included both additions of partners to the network or the removal of network partners. For the addition of new partners to the PPS network, the PPS were required to follow a process similar to the process utilized for the networking reopening that occurred in November 2015. PPS received further guidance on the dates for the network reopening for the addition of new partners with the start of the Mid-Point Assessment.
A PPS wishing to remove network partners did so in accordance with Section X of Attachment I to the STCs. In support of the request to remove a network partner, the PPS demonstrated non-performance or failure of the network partner to meet DSRIP program requirements. Documentation would have included a description of the escalation process employed by the PPS for identifying and tracking non-performing network partners as well as the notifications to the under-performing network partners informing them of the performance concerns of the PPS. In requesting the removal of PPS network partners, the PPS were not able to remove more than 5% of their network partners.
Z9. Q: Was there be an opportunity to review the Safety Net status of PPS network partners at the time of the Mid-Point Assessment? (Revised 8/31/2018)
A: At the Mid-Point Assessment, PPS will have the ability to request a review of the Safety Net status of any network partners that are not currently designed at Safety Net providers. The review process will follow the process previously used during the Safety Net appeals at the outset of DSRIP. PPS will be responsible for submitting the applicable Safety Net Appeals Form for all providers that it wishes to have their Safety Net status reviewed.
Determinations on the Safety Net status of providers will be made consistent with the process utilized in the completion of initial Safety Net status determinations and in the initial round of Safety Net Appeals. The determinations will be based on the most recent data available and are subject to CMS approval, which were ultimately disapproved. As with the initial Safety Net determinations and the Safety Net Appeals, only Medicaid providers will be considered for Safety Net status.
|back to table of contents||top of section| |top of page|
AA. Equity Programs and VBP QIP
AA1. Q: What are the Equity Programs?
A: The Equity Programs consist of two programs, the Equity Infrastructure Program (EIP) and the Equity Performance Program (EPP). EIP payments will be paid to PPS for participating in select Delivery System Reform Incentive Payment (DSRIP) activities and implementing predetermined key DSRIP initiatives. EPP payments will be triggered by the PPS achieving a subset of DSRIP performance metrics.
AA2. Q: What determines eligibility for participation in the EIP, EPP, and AHPP?
A: Equity Programs participation was determined by DOH from the final DSRIP valuation calculation and is focused on mitigating an inequity between PPS. DOH noted an inequity with Safety Net PPS and public PPS in a sole PPS county in relation to project 2.d.i. Whereas, all PPS participating in DSRIP are eligible for Additional High-Performance Payment (AHPP).
VBP QIP
AA3. Q: What is the Value Based Payment Quality Improvement Program (VBP QIP)?
A: The program targets individual hospitals in severe financial distress, enabling them to maintain operations and vital services while they work towards long-term sustainability and improve quality, aligning closely with the NYS´ Value Based Payment (VBP) initiatives. Through this program, facilities will need to develop a transformation plan that will promote:
- Movement to VBP
- Improved Quality of Care
- Financial Stability
AA4. Q: Where can I find more information on the VBP QIP program?
A: More information can be found here.
|back to table of contents||top of section| |top of page|
Follow Us