Salient Performance Data
DOH and Salient Management Company have prepared a series of Data Workbooks as a resource to DSRIP applicants in preparing their grant applications. The source of this data is the Salient NYS Medicaid System used by DOH for Medicaid management. Workbooks can be used to assist potential DSRIP performing provider networks with better understanding of who the key Medicaid providers are in each region to assist with network formation and a rough proxy for Medicaid volume for DSRIP valuation purposes. More interactive data in dashboard format will be available in June.
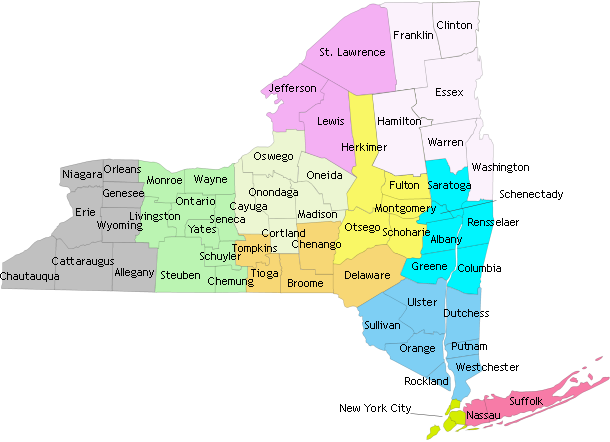
Color Legend
- Capital Region
- Central NY
- Finger Lakes
- Long Island
- Mid-Hudson
- Mohawk Valley
- North Country
- NYC
- Southern Tier
- Tug Hill Seaway
- Western NY
Part I: Salient Provider & Member Workbooks
Two workbooks are presented for each region to provide different vantage points on utilization:
1. Provider Service County: In these workbooks, county is defined as the service location of the provider. With the data in these workbooks, the user can identify the major providers who care for Medicaid members in that region – no matter which county in the region their patients come from.
- Service Regions Data:
- Region 1: Long Island Medicaid Service (XLS)
- Region 2: New York City Medicaid Service (XLS)
- Region 3: Northern Metro Medicaid Service (XLS)
- Region 4: Northeast Medicaid Service (XLS)
- Region 5: Utica/Watertown Medicaid Service (XLS)
- Region 6: Central Medicaid Service (XLS)
- Region 7: Rochester Medicaid Service (XLS)
- Region 8: Western Medicaid Service (XLS)
2. Member County: In these workbooks, the county is the Medicaid member's district of fiscal responsibility. In most cases, this is where the member lives, but may also include members who are the responsibility of one county, while living in a facility in another county or out of state. Use these workbooks to see the providers used by members living in the selected county or region.
- Members Regions Data:
- Region 1: Long Island Medicaid Members (XLS)
- Region 2: New York City Medicaid Members (XLS)
- Region 3: Northern Metro Medicaid Members (XLS)
- Region 4: Northeast Medicaid Members (XLS)
- Region 5: Utica/Watertown Medicaid Members (XLS)
- Region 6: Central Medicaid Members (XLS)
- Region 7: Rochester Medicaid Members (XLS)
- Region 8: Western Medicaid Members (XLS)
Part II: Salient Behavioral Health Workbooks
The behavioral health workbooks (below) are presented for each region to provide different vantage points on behavioral health utilization. Please note that the behavioral health workbooks are based off of PHIP regions, whereas the provider and member workbooks (above) are based of DOH regions. Please review the corresponding workbook series overview document to see which counties have been placed in each region.
- Region 1: Long Island Medicaid Behavioral Health (XLSX, 54KB)
- Region 2: New York City Medicaid Behavioral Health (XLSX, 92KB)
- Region 3: Mid-Hudson Medicaid Behavioral Health (XLSX, 83KB)
- Region 4: Capital Medicaid Behavioral Health (XLSX, 78KB)
- Region 5: Mohawk Medicaid Behavioral Health (XLSX, 65KB)
- Region 6: North Country Medicaid Behavioral Health (XLSX, 77KB)
- Region 7:Tug Hill Seaway Medicaid Behavioral Health (XLSX, 64KB)
- Region 8: Central Medicaid Behavioral Health (XLSX, 93KB)
- Region 9: Southern Tier Medicaid Behavioral Health (XLSX, 75KB)
- Region 10: Finger Lakes Medicaid Behavioral Health (XLSX, 88KB)
- Region 11: Western Medicaid Behavioral Health (XLSX, 93KB)
Part III: Long Term Care Workbooks
DOH and Salient Management Company have prepared a series of Data Workbooks as a resource to DSRIP applicants in preparing their grant applications. The source of this data is the Salient NYS Medicaid System used by DOH for Medicaid management. Workbooks can be used to assist potential DSRIP performing provider networks with better understanding of who the key Medicaid providers are in each region to assist with network formation and a rough proxy for Medicaid volume for DSRIP valuation purposes. More interactive data in dashboard format will be available soon. The first set of workbooks focused on all Inpatient, Clinic, Emergency Room and Practitioner services. The second set focused on Behavioral Health services. This third set focuses on Long Term Care services.
Overview:
Long Term Care Claims: Data is provided on Medicaid utilization of Long Term Care services by provider. Institutional and non-institutional long term care services are listed separately. Non-institutional services are further separated into Personal Care Services and Home Health and other home care services. Criteria for inclusion include categories of service and Medicaid Managed Care Operating Report Guidelines (MMCOR) for institutional long term care services, and DOH Division of Long Term Care approved rates and procedures for non-institutional long term care. Complete lists of codes are included on the criteria page of each workbook.
Time Frame: All data are for dates of service between July 1, 2012 and June 30, 2013. This year was chosen to ensure that the vast majority of services that were rendered during this time period have been paid for and are therefore reflected in the dataset.
Regional Workbooks: Data workbooks are organized by 11 Population Health Improvement Program (PHIP) regions. Regions are defined by DOH and include: Capital Region, Central NY, Finger Lakes, Long Island, Mid-Hudson, Mohawk Valley, NYC, North Country, Southern Tier, Tug Hill Seaway, and Western NY. Within each region are tabs for the provider service counties that make up the region (see map below). Provider Service County is the service location of the provider, as provided by the Medicaid Data Warehouse. In cases where there is no service location on the claim, the first service location listed on the provider's address file is used.
With the data in these workbooks, the user can identify the major providers who care for Medicaid members in that region – no matter which county in the region their patients come from. Please note, if a provider has lower claim or member counts than expected, they may be serving members from outside the region in view or have locations in multiple regions.
Top 50 Providers: Each of the regional workbooks is built up from a list of the top 50 providers in each county. When creating the regional summary view, any provider who made the top 50 ranking in any of the counties is included along with all of their activity in the region.
Measures: Each workbook includes two measures for all Long Term Care services:
- Claim counts – A count of the services (fee-for-service claims and managed care encounters) rendered during the measurement year. Claim counts may include a combination of claims that represent services, episodes, stays, days or multiple days, depending on the mix of services rendered by the provider.
- Unduplicated Member count – A count of the individual members who had one or more services from that provider during the year.
Format: All datasets are in Excel workbooks by Region. Each column includes drop-down filtering capability so you can view data by select values or ranges.
- Region 1: Long Island (XLSX)
- Region 2: New York City (XLSX)
- Region 3: Mid-Hudson (XLSX)
- Region 4: Capital Region (XLSX)
- Region 5: Mohawk Valley (XLSX)
- Region 6: North Country (XLSX)
- Region 7: Tug Hill Seaway (XLSX)
- Region 8: Central NY (XLSX)
- Region 9: Southern Tier (XLSX)
- Region 10: Finger Lakes (XLSX)
- Region 11: Western NY (XLSX)
Hospital Inpatient Prevention Quality Indicators
Access All Payer data on observed and expected rates for Hospital Inpatient Prevention Quality Indicators beginning in 2009 through 2012. One data set is organized by county and one data set is filterable by zip code.
- Hospital Inpatient Prevention Quality Indicators by Zip Code
- Hospital Inpatient Prevention Quality Indicators by County
- Medicaid Prevention Quality Indicators for Adult Hospital Discharges by Patient Zip Code: Beginning 2011
- Medicaid Inpatient Prevention Quality Indicators for Adult Discharges by Patient County: Beginning 2011
- Medicaid Beneficiaries, Inpatient Admissions, and Emergency Room Visits by Zip Code: Beginning 2012
- Medicaid Chronic Conditions, Inpatient Admissions and Emergency Room Visits by County: Beginning 2012
- Medicaid Chronic Conditions, Inpatient Admissions and Emergency Room Visits by Zip Code: Beginning 2012
- Medicaid Hospital Inpatient Potentially Preventable Readmission Rates by Hospital: Beginning 2011
- Medicaid Program Enrollment by Month: Beginning 2009
Medicaid Inpatient Admissions and Emergency Room Visits
This data set contains statewide Medicaid beneficiary counts by valid NYS five digit zip code. Also in this file are counts of beneficiaries who are dual eligible for Medicaid and Medicare, total inpatient admissions, total emergency room visits, and Prevention Quality Indicator-Adult (PQI) admissions.
This data set contains information on selected chronic health conditions in the Medicaid population at both the zip code and county level. The chronic health conditions were identified through 3M Clinical Risk Group software and Medicaid enrollment/eligibility, encounter, claim and pharmacy data over a 12 month period. The chronic health categories represented in the data file are: Diabetes Mellitus, Diseases and Disorders of the Cardiovascular System, Diseases and Disorders of the Respiratory System, HIV Infection, Mental Diseases and Disorders, Newborn and Neonates and Substance Abuse. All conditions that have 20 or less unique beneficiaries are suppressed from this data file.
This dataset contains information on selected chronic health conditions in the Medicaid population at the county level. The chronic health conditions were identified through 3M Clinical Risk Group software and Medicaid enrollment/eligibility, encounter, claim and pharmacy data over a 12 month period. The chronic health categories represented in the data file are: Diabetes Mellitus, Diseases and Disorders of the Cardiovascular System, Diseases and Disorders of the Respiratory System, HIV Infection, Mental Diseases and Disorders, Newborn and Neonates and Substance Abuse. All conditions that have 20 or less unique beneficiaries are suppressed from this data file.
This dataset contains Potentially Preventable Visit (PPV) observed, expected, and risk-adjusted rates for Medicaid beneficiaries by patient county and patient zip code beginning in 2011. The Potentially Preventable Visits (PPV), obtained from software created by 3M Health Information Systems, are emergency visits that may result from a lack of adequate access to care or ambulatory care coordination. These ambulatory sensitive conditions could be reduced or eliminated with adequate patient monitoring and follow up. The rates were calculated using Medicaid inpatient and outpatient data for the numerator and Medicaid enrollment in the county for the denominator. The observed, expected and risk adjusted rates for PPV are presented by resident county (including a statewide total).
This dataset contains Potentially Preventable Visit (PPV) observed, expected, and risk-adjusted rates for Medicaid beneficiaries by patient county and patient zip code beginning in 2011. The Potentially Preventable Visits (PPV), obtained from software created by 3M Health Information Systems, are emergency visits that may result from a lack of adequate access to care or ambulatory care coordination. These ambulatory sensitive conditions could be reduced or eliminated with adequate patient monitoring and follow up. The rates were calculated using Medicaid inpatient and outpatient data for the numerator and Medicaid enrollment in the zip code for the denominator. The observed, expected and risk adjusted rates for PPV are presented by resident zip code (including a statewide total).
The datasets contain number of Medicaid PDI hospitalizations (numerator), county Medicaid population (denominator), observed rate, expected number of hospitalizations and rate, and risk-adjusted rate for Agency for Healthcare Research and Quality Pediatric Quality Indicators – Pediatric (AHRQ PDI) for Medicaid enrollees beginning in 2011. The Agency for Healthcare Research and Quality (AHRQ) Pediatric Quality Indicators (PDIs) are a set of population based measures that can be used with hospital inpatient discharge data to identify ambulatory care sensitive conditions. These are conditions where 1) the need for hospitalization is potentially preventable with appropriate outpatient care, or 2) conditions that could be less severe if treated early and appropriately. Both the Urinary Tract Infection and Gastroenteritis PDIs include admissions for patients aged 3 months through 17 years. The asthma PDI includes admissions for patients aged 2 through 17 years. Eligible admissions for the Diabetes Short-term Complications PDI includes admissions for patients aged 6 through 17 years. The rates were calculated using Medicaid inpatient hospital data for the numerator and Medicaid enrollment in the county for the denominator. The observed counts and rates, expected counts and rates, risk-adjusted rates and the difference between the number of observed and expected PDI hospitalizations for each AHRQ PDI are presented by resident county (including a statewide total).
Follow Us