Population Health Management Webinars
- Presentation is also available in Portable Document Format (PDF)
DST Webinar – Population Health Management
December, 2014
© 2014 KPMG LLP, a Delaware limited liability partnership and the U.S. member firm of the KPMG network of independent member firms affiliated with KPMG International Cooperative ("KPMG International"), a Swiss entity. All rights reserved. NDPPS 257815 The KPMG name, logo and "cutting through complexity" are registered trademarks or trademarks of KPMG International.
Contents
- Current Challenges for DSRIP
- DSRIP Vision
- Population Health – A Core Foundation for DSRIP
- Population Health Tools
- Criteria for Population Health Management
- Challenges in Implementing Population Health
- Population Health Management Vendors
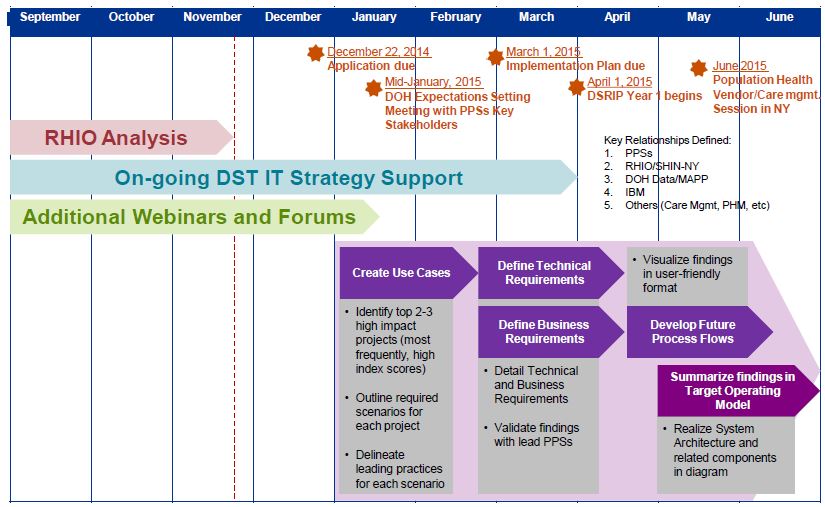
- Setting Expectations Session with PPSs – January 2015
- Summary
DSRIP and Population Health
The DSRIP Challenge – Transforming the Delivery System
DSRIP is a major effort to collectively and thoroughly transform the New York State (NYS) Medicaid Healthcare Delivery System. There is a focus on transitioning:
- From fragmented and overly focused on inpatient care → integrated and focused on outpatient care
- From a re–active and siloed system → pro–active, community and patient–focused system
Building upon the success of the Medicaid Redesign Team (MRT), the goal is to reduce avoidable admissions and collectively create a future–proof, high–quality and financially sustainable care delivery system.
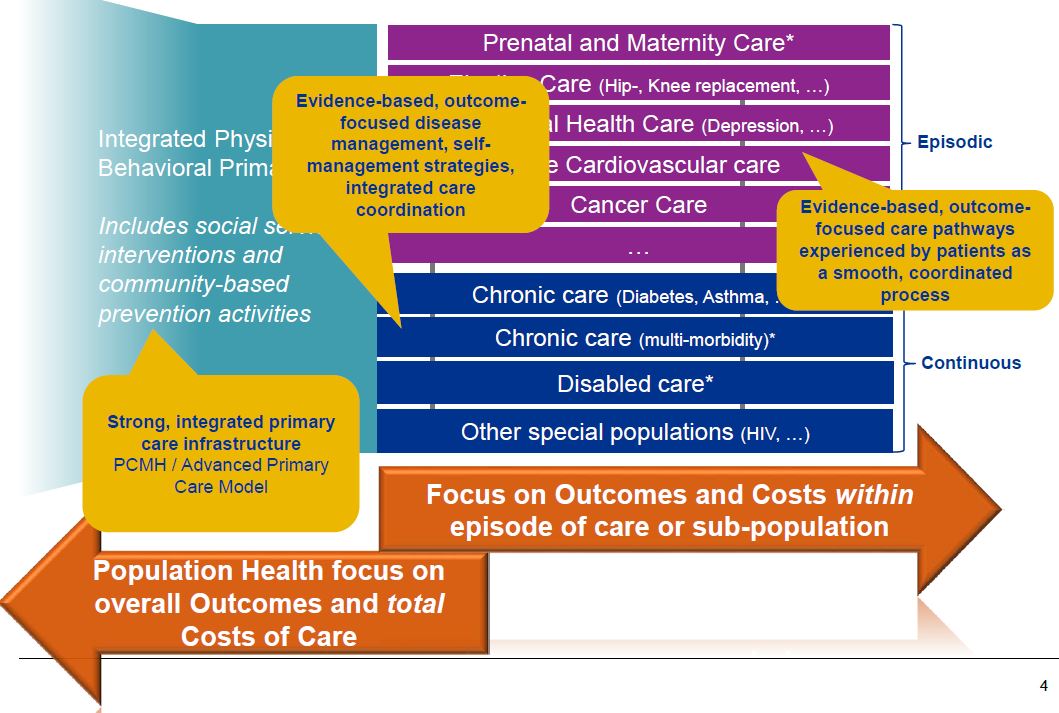
DSRIP Vision – How Should an Integrated Delivery System Function?
Core Foundation for Population Health – Having the Right Information
The DSRIP program and the metrics focus on improving population health
This requires complete, longitudinal information on what happens to patients over time and across organizational boundaries
Such information is rarely systematically available for any given provider
The State´s Medicaid Claims and Encounter data, completed with other data sources already available at State level form a strong basis to start with
- >90% of all DSRIP metrics are calculated by the State on the basis of these data
What information can PPSs expect to get from the State?
| Until Dec. 2014 |
|
| In DY 1 (gradual build–out) |
|
| In DY 2 (gradual build–out) |
|
Precise deadlines, scope and format of information may change
State Reports Will not Replace PPS Acquired Population Health Platform
DOH plans to provide claims–based reporting, but this may not be sufficient for real– time population health analytics and patient engagement needs for the PPSs due to the following constraints:
- Claims based reports have a lag of 6 month and don´t necessarily provide all clinical information like lab results
- Report will not be real–time but retrospective in nature
- Population management capabilities like Outreach to patients would not come from DOH reports
Legend:
★Primary target for PPS provided population health platform. These may not be provided by state in entirety
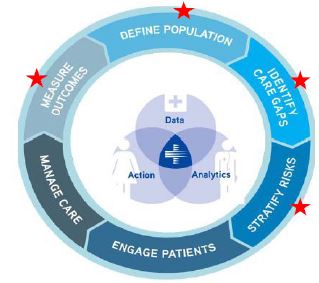
What you will receive from DOH will...
- Allow you to define and identify populations in your PPS to focus on
- Allow you to identify care gaps
- Allow you to stratify populations within your PPS based on clinical and financial risk
- Allow you to measure and monitor outcomes over time and attribute success/failure to partners within the PPS
- Allow you to benchmark your outcomes and trends with other PPSs in NYS and with national benchmarks
- Allow you to ‘pipe´ data streams into your own PPS specific PHM tools that can build upon this foundation
- Allow you to identify potential reductions in total cost of care per episode, subpopulation or at total Medicaid population level – crucial to start shared savings discussions with MCOs
Population Health Management Criteria
The following criteria are key to selecting a robust population health management platform:
- Patient Registries
Evidence–based definitions of patients to include in population health registries - Patient–Provider Assignment
Strategies and algorithms to assign patients to accountable physicians or clinicians - Precise Metrics in Registries
Discrete, evidence–based methods for flagging the patients in the registries that are difficult to manage or should be excluded - Clinical and Cost Metrics
Monitoring clinical effectiveness and cost of care to the system and patient - Basic Clinical Practice Guidelines
Evidence–based triage and clinical protocols for single disease states - Risk Management Outreach
Stratified work queues that feed care management teams and processes - Acquiring External Data
laboratory test results, and pharmacy data outside the core healthcare delivery organization - Communication with Patients
Engaging patients and establishing a communication system about their care - Educating and Engaging Patients
Patient education material and distribution system, tailored to the patient´s status and protocol - Complex Clinical Practice Guidelines
Evidence–based triage and clinical protocols for comorbid patients
Source: Health Catalyst
Challenges/ Issues Faced in Implementing Population Health Management
| 1 Complexity of data consolidation and normalization |
2 Access to real–time data for performance management |
3 Care intervention for a patient |
|---|---|---|
|
|
|
Population Health Management Vendor Current Landscape
The marketplace for Health Information Exchange (HIE) vendors includes Regional Health Information Organizations (RHIOs), NY State HIE vendors, as well as commercial HIE vendors. Current RHIOS are utilizing one of four NY State HIE vendors. Additional vendors in the marketplace may be able to provide population health functionality.
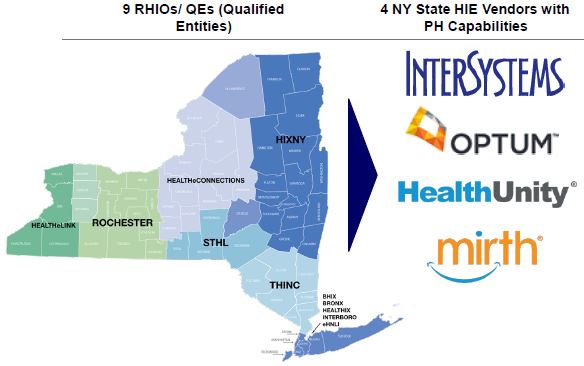
Vendors with PH Capabilities
- Covisint
- DBMotion
- eClinicalWorks
- Explorys
- GSI
- Kryptiq
- Lumeris
- McKesson
- Medecision
- The Advisory Board Company
- Wellcentive
- HIS Vendors
The DOH and PPS Support Activities: Proposed Support
Summary
Performing Provider Systems (PPSs) should take the necessary steps to ensure they have functional population health management tools in place help identify, monitor, and report on patient populations.
Population health management tools will help contribute to overall DSRIP goals of reducing avoidable hospital use and improving other health and public health measures, as well as by creating a cost–efficient Medicaid program with improved outcomes.
Disclaimers
This document was prepared by the Delivery System Redesign Incentive Payment (DSRIP) Support Team (DST). The advice, recommendations and information in the document included with this notice were prepared for the sole benefit of the New York State Department of Health, based on the specific facts and circumstances of the New York State Department of Health, and its use is limited to the scope of KPMG´s engagement as DST for the New York State Department of Health. It has been provided to you for informational purposes only and you are not authorized by KPMG to rely upon it and any such reliance by you or anyone else shall be at your or their own risk. You acknowledge and agree that KPMG accepts no responsibility or liability in respect of the advice, recommendations or other information in such document to any person or organization other than the New York State Department of Health. You shall have no right to disclose the advice, recommendations or other information in such document to anyone else without including a copy of this notice and, unless disclosure is required by law or to fulfill a professional obligation required under applicable professional standards, obtaining a signed acknowledgement of this notice from the party to whom disclosure is made and you provide a copy thereof to New York State Department of Health. You acknowledge and agree that you will be responsible for any damages suffered by KPMG as a result of your failure to comply with the terms of this notice.
Follow Us