Better Health for Northeast New York
BHNNY Cares
- BHNNY Cares is also available in Portable Document Format (PDF)
Kallanna Manjunath, MD, FAAP, CPE
Charlene Schlude, BSN, MPA, CCM
BHNNY Cares
- Program overview
- Components of BHNNY Cares Program
- Why partner with a MCO?
- Additional partner engagement
- Critical success factors
BHNNY Cares
A care management program sponsored by
Better Health
for Northeast New York
BHNNY Cares – Objectives
- Identify, engage, address identified needs
- Clinical, medication adherence, self–management support
- Facilitate access
- Primary care, BH services, Health Homes,
- Enhance communication and data sharing
- Care plans, access to Hixny (RHIO)
- Collaborate to address relevant Social Determinants of Health (SDH)
- Housing, Transportation, Health Literacy/Health Coaching
- Community–based support for members with Asthma & Hypertension
BHNNY Cares – Component of a developing IDS
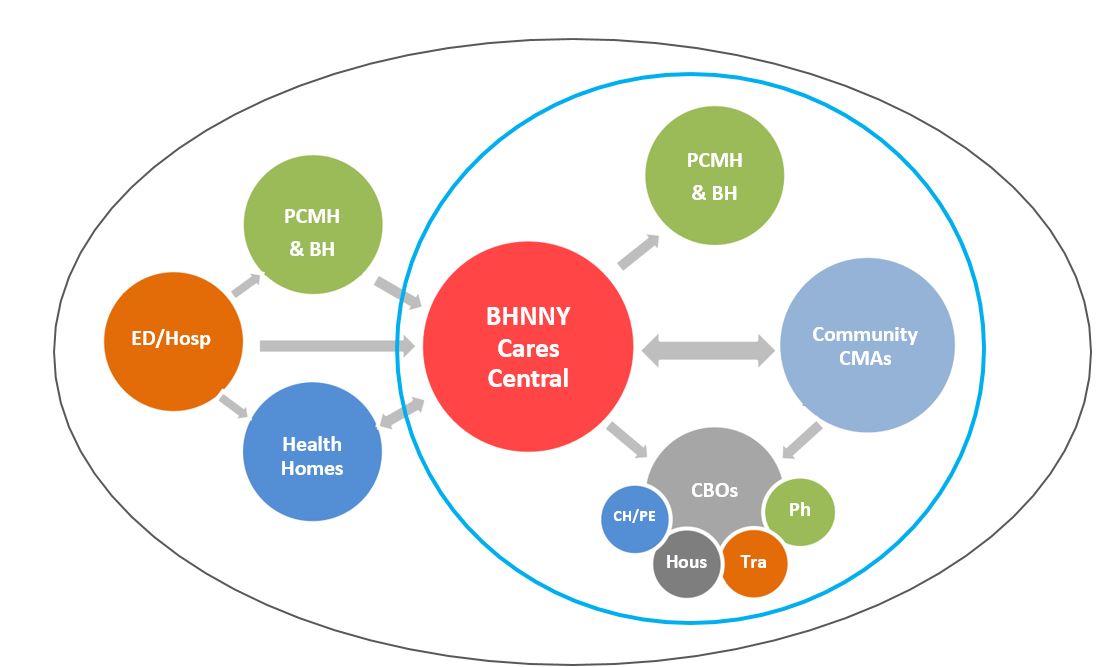
Keys:
PCMH – Patient Centered Medical Homes
BH – Behavioral Health Providers
CMAs – Care Management Agencies
ED/Hosp – Emergency Departments/Hospitals
CBOs – Community–Based Organizations
(Pharmacy, Transportation, Housing, CHW/Peer Coaching)
BHNNY Cares Central – Why Partner with a MCO?
- CDPHP – Prominent physician–led regional MCO with an effective community–based care management program
- BHNNY´s need to align with HHARI project objectives & meet milestone timelines
- BHNNY´s desire to develop a potentially sustainable program to minimize negative impact on patients and providers
- CDPHP´s extensive primary care and behavioral health provider networks
BHNNY Cares – Additional Partner Engagement
- Community Care Management Agencies
- Alliance for Positive Health
- Catholic Charities Care Coordination Program
- Mental Health Association of Columbia and Greene
- Rehabilitation Support Services
- Non–clinical care coordination needs
- Linkages to community–based providers to address
BHNNY Cares – Additional CBO Engagement
- Working on establishing agreements with CBOs to address SDH
- Transportation – Circulation Platform – Collaboration with other PPSs
- Housing – Collaboration with Alliance for Better Health & AHI PPS
- Health literacy & Health coaching – Collaboration with ABH PPS & AHI PPS
- CVD self–management support –Albany County DOH CHW program
BHNNY Cares – Target Population
- Priority Groups for Initial CM Interventions
- Patients identified by partnering providers
- Patients with frequent ED visits/Hospitalizations
- Patients identified by data analytics – patients without PCP assignment, high risk, high users, P4P gap list, etc.
- Additional groups – Hospital CM feedback
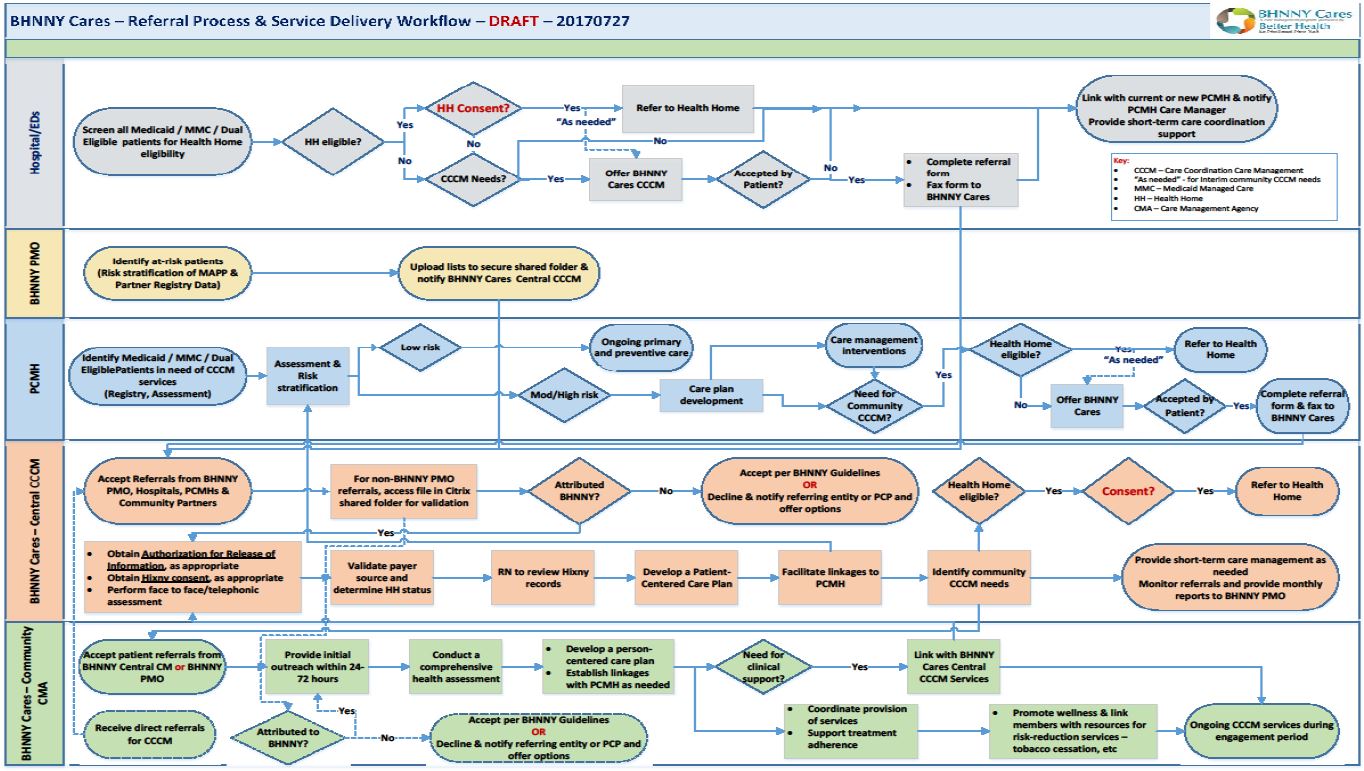
BHNNY Cares – Referrals are easy!
- Identified patients can be referred with a simple fax or a call
- Fax (518) 810–0021
or - Call (518) 810–0002
BHNNY Cares – Critical Success Factors
- Shared vision
- Active leadership support
- Active practitioner / organizational participation
- Effective member / consumer engagement
- Availability and utilization of health information systems – risk stratification, real–time exchange of care plans, data analytics
- Ability to demonstrate value – reduce cost and improve care
Centralized Care Management in Partnership with CDPHP
Charlene Schlude BSN, MPA, CCM
Director Centralized Care Management
Innovative Partnership: MCO and PPS collaborate on a unique centralized care management model
How did we come together?
- Strong hospital partnership between CDPHP and PPS affiliated hospitals
- CDPHP´s mission aligns well with BHNNY Cares population health strategy
- Solid relationships with community partners
- Alignment in our roles for supporting primary care practices
- Demonstrated success of CDPHP´s Medicaid case management program
Centralized Care Management Model
- Dedicated Multidisciplinary Care Team
- ✓ Care Coordinators
- ✓ RN Case Manager
- ✓ SW case managers (behavioral health background)
- ✓ Pharmacist
- Comprehensive Assessment
- Patient Activation Measure (PAM)
- Person Centered Care Plan
- A hybrid model : triage and refer /triage and management for defined subsets of the population
- Monthly reporting in support of DSRIP requirements
Key Program Deliverables
- Perform care transitions after an ER encounter
- Address all social determinants of health
- Facilitate engagement with NCQA Level 3 PCMH practices
- Maintain relationships with community–based resources and refer as appropriate
- Maintain relationships with payers and evaluate benefits and services offered
- Use health information technology to link services
- Maintain accurate data and provide timely, meaningful data to PPS
- Perform regular monitoring of all referrals to assess for care plan modifications
- Facilitate health home referrals as appropriate
Challenges along the way...
- Limited options for case management system on go live date
- Restricted access to alternate PPS data
- Difficulty identifying health home eligibility
Expected Outcomes...
- Strong focus on DSRIP milestones
- Follow guiding principles of the Triple Aim
- ✓ Reduce avoidable IP/ ER admissions
- ✓ Demonstrate improved access to Level 3 PCMH practices
- ✓ Engage with rising risk populations that are not health home eligible
Program status...
7/14/17 through 8/30/2017
- 25 enrolled
- 95% engagement rate
- Referral source : primary care practices
Follow Us