DRAFT
8/3/2015; Version 5
Value Based Payment Reform in New York State:
A Proposal to align Medicare´s and NYS Medicaid´s Reforms
- Proposal is also available in Portable Document Format (PDF)
July 2015
Draft for discussion in VBP Workgroup
"Let the care follow the patient, not the program" (Montefiore Health System)
Introduction
Both the Centers for Medicare & Medicaid Services (CMS) and New York State (NYS) have embarked on an ambitious journey to improve outcomes for patients and populations, reward the delivery of high value care by providers, and increase long–term financial sustainability. In this document, New York State presents an approach to maximally align CMS´ payment reform efforts for Medicare to the NYS´ Medicaid Payment Reform Roadmap which has recently been approved by CMS. NYS proposes to allow its providers and Managed Care Organizations to include Medicaid beneficiaries in CMS innovative payment models (ACOs, Integrated Primary Care models, Bundled Payments for Care Improvement (BPCI), Comprehensive Care for Joint Replacement Model (CCJR)). In parallel, NYS requests CMS to allow NYS providers to include Medicare FFS patients in the VBP Arrangements outlined in the NYS Payment Reform Roadmap. (Simultaneously, NYS will work with its Medicare Advantage plans to realize a complimentary alignment). Finally, NYS proposes to allow Montefiore Health System to be the first Accountable Care organization that assumes full financial risk and population health responsibility for its entire Medicaid and Medicare population.
Aligning these efforts across Medicaid and Medicare in NYS will have significant advantages for patients, providers, the State and CMS:
- Patients will no longer be confronted with barriers and discontinuities across systems (especially the almost 800,000 duals)
- Providers will be able to focus on a consistent set of Alternative Payment Models (APMs) for Medicaid and Medicare, allowing clinical and quality alignment across delivery system reform initiatives
- Providers´ incentives to transition to value based payment arrangements will be greatly increased with approx. 50% of total provider payments moving towards value based payments in unison
- Providers with experience in APMs in one program (Medicare) can seamlessly reuse their knowledge and VBP infrastructure in the other program (Medicaid), and vice versa
- Alignment between payment mechanisms (Medicaid and Medicare) greatly reduces administrative costs
- Financially weak safety–net providers in NYS will be greatly supported by the ability to be rewarded for delivering value consistently across Medicaid and Medicare
- Uniquely, NYS stakeholders (including providers and managed care organizations) have actively participated in the creation of the Roadmap and have committed themselves to the APMs described in the Roadmap (including ´off–menu´ APMs that will be equally value–oriented). These same stakeholders have pressed the State to request CMS to align its reforms with NYS (and vice versa). This offers a significant step for CMS to achieve its goal of realizing 50% of Medicare payments tied to quality or value through APMs by the end of 2018.
- Alignment across systems increases the numbers and diversity of beneficiaries that can be included in the APMs, enhancing the ability for providers to participate in these APMs as well as the ability for CMS to test these models more comprehensively.
- The NYS VBP Arrangements have been designed building upon the latest national and global insights and lessons learned, including those of CMS´ Innovation Center. Realizing and subsequently monitoring this alignment would be perfect input for the Health Care Payment Learning and Action Network.
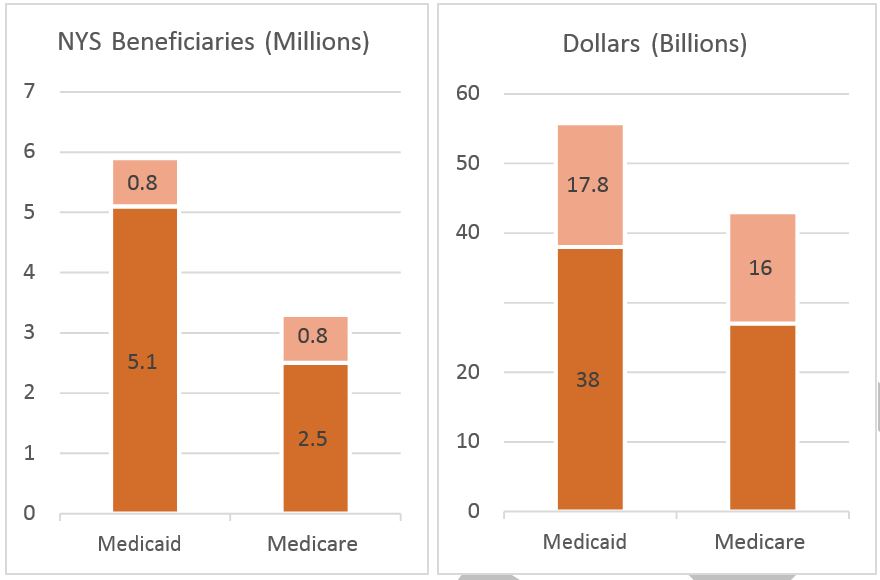
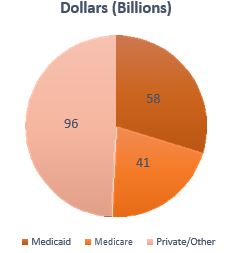
2014 data. The lighter colored bars indicate dual eligibles.
Sources: Kaiser Family Foundation (kff.org); Medicare–Medicaid Linked Enrollee Analytic Data Source (MMLEADS) Version 2.0 files (cms.gov);12–14 Medicare Enrollment File, https://www.cms.gov/Research–Statistics–Data–and–Systems/Statistics–Trends–and–Reports/MCRAdvPartDEnrolData/MA–State–County–Penetration–Items; DOH Oct 2014 data (5.6% underreporting) (Care Man Transition Chart (6/11/15 version). Medicare 2014 expenditures extrapolated from these datasets.
Background
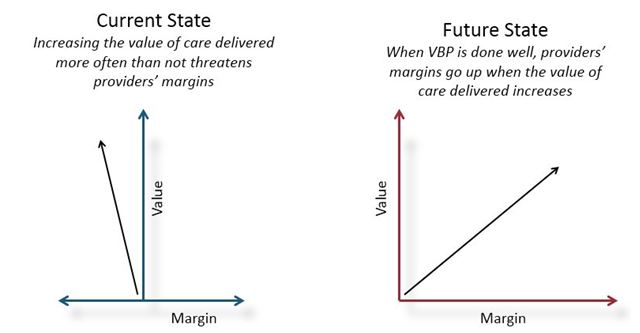
Value Based Payment (VBP) reform is a key component of the New York State (NYS) Delivery System Reform Incentive Payment (DSRIP) Program. The DSRIP program promotes community–level collaborations and aims to reduce avoidable hospital use by 25 percent over five years while financially stabilizing the State´s safety net. A total of 25 Performing Provider Systems (PPSs) have been established statewide to implement innovative projects focused on system transformation, clinical improvement and population health improvement. To ensure the long–term sustainability of the improvements made possible by the DSRIP investments, the State has worked closely with statewide stakeholders to create an ambitious, five–year Roadmap for comprehensive Medicaid Payment Reform, which has been approved by CMS July 22, 2015. Whereas currently, increasing the value of the care delivered (preventing avoidable admissions, reducing administrative waste) has a negative impact on the financial sustainability of providers, the NYS Roadmap aims to reward the delivery of high–value care with potentially higher margins, while remaining within the NYS Medicaid Global Spending Cap.
Parallels between Medicaid and Medicare Payment Reform Goals
The goals of New York´s State Medicaid Payment Reform Roadmap mirror the ambitions recently articulated for Medicare. Through regulatory and financial incentives, the Roadmap describes a path to a Medicaid payment model in which 80–90% of all Managed Care Organization (MCO) payments to providers will not only be value–based, but will leverage alternative payment models (APMs)1 by the end of 2019. These ambitious and comprehensive goals, and the approach to achieving them, have been wholeheartedly embraced by Secretary Burwell, who recently announced earlier this year to have 50% of all Medicare Fee–for–Service payments channeled through APMs by the end of 2018.
Comparing the NYS Medicaid and Medicare Payment Reforms
The NYS Medicaid Payment Reform Roadmap starts from a holistic and systematic perspective: 80–90% of the total of MCO to provider payments will have to leverage APMs. Building upon the latest research and (inter)national experience in payment reform, New York State recognizes that one size will not fit all: some types of patient care (such as maternity care) are optimally contracted and incentivized through bundled payments, for example, while integrated primary care may need its own specific sets of incentives. Likewise, the care for special needs subpopulations (such as the MLTC population) is more adequately contracted for through a total care for a specific subpopulation arrangement (a condition–specific or special–needs ACO). Similarly, some groups of providers may be better suited for a total care for a total population approach (moving towards an ACO with global capitation). On the other hand, others may prefer a more differentiated approach, competing with each other for some types of care (basic chronic care, elective care) while jointly contracting and being tightly integrated in their approach for the most vulnerable, co–morbid patients with significant behavioral health needs.
Fee–for–Service Medicare and Managed Care Medicaid
Over the next few years, NYS will complete its transition process from a largely FFS–based Medicaid program to a program that is almost entirely Managed Care–based. To impact provider payments, then, New York State´s payment reform focuses on how MCOs pay providers. In contrast, the starting point for Medicare´s Innovation Models is predominantly the Medicare FFS population (which in NYS is still 65% of the overall Medicare population). This has important practical consequences which are discussed later in the proposal.
The different APMs distinguished in the Roadmap can be mapped on those being tested by the Center for Medicare and Medicaid Innovation (CMMI):
| NYS Medicaid VBP Roadmap APMs (and unique feature(s) compared to Medicare APMs) | Comparable Medicare VBP APMs |
|---|---|
| All Care for Total Population | Medicare ACO |
| Integrated Primary Care With shared savings based on reduced downstream costs. |
Comprehensive Primary Care Initiative; Primary Care–led ACO; Cardiovascular Disease Risk Reduction Model |
| Bundles (acute and chronic) Bundles are based on national standard, are more narrowly defined and do not necessarily start with hospital admission. |
Bundled Payments for Care Improvement (BCPI) Oncology Care Model Comprehensive Care for Joint Replacement Payment Model |
| All Care for Subpopulation (MLTC, AIDS/HIV, individuals with co–occurrence of significant behavioral and physical health problems2 ) | Condition or disease–specific ACO |
In addition, the NYS Medicaid Payment Reform Roadmap distinguishes between four levels of VBP, moving from shared savings to assuming risk and finally to full, upfront capitation or bundled payments. These levels can be mapped on the CMS´s Payment Taxonomy Framework3 as follows:
| NYS Medicaid Level | Medicare Category |
|---|---|
| NA | Category 1 – Fee–for–Service with no link of payment to quality |
| Level 0 – Does not count towards the 80–90% goal | Category 2 – Fee–for–Service with a link of payment to quality |
| Level 1 – Upside only arrangements, built on FFS architecture (retrospective reconciliation) Level 2 – Up– and downside arrangement, built on FFS architecture (retrospective reconciliation) |
Category 3 – Alternative payment models built on Fee– for–Service (FFS) architecture |
| Level 3 – Per Member/Patient per Month payments (capitation/ prospective bundled payments) | Category 4 – Population–based payment |
As is the case in most Innovation models tested by the CMMI, the percentages of savings (or losses) to be shared with providers are not just dependent on the financial results, but also on the outcomes of care realized. (For more details, see the NYS Medicaid Payment Reform Roadmap).
The NYS Roadmap, then, in many ways builds upon the insights and lessons learned by CMS´ Innovative Center. It presents an overall vision of how the different APMs can be juxtaposed in varying ways to add up to a meaningful, mutually reinforcing whole, in which 80–90% of the total of provider payments will become value–based by 2019.
The NYS Dual Eligible Population and FIDA
The dual eligible population may seem relatively small (some 15% of Medicaid beneficiaries are also eligible for Medicare), but these 800,000 individuals comprise over 25% of total Medicaid spending, and over 33% of Medicare spending in NYS. Many of these individuals use long term care services (LTCS) as well as hospital and other services; the former costs are covered by Medicaid (often through a MLTC plan); the latter are generally covered by Medicare.
The potential quality and efficiency benefits of the ´pooling´ of Medicaid and Medicare dollars described in the text was the starting point of the joint CMS and NYS Department of Health Fully Integrated Duals Advantage (FIDA) program. This program is focused on those dually eligible beneficiaries with the largest health needs (and corresponding total costs). Creating one integrated MCO for the total Medicaid– Medicare costs for this population is a promising approach. The State´s suggestions in this proposal should be seen as complementary, increasing the opportunities to improve the quality and efficiency of the care for this most vulnerable group.
The Case for Further Medicaid/Medicare Payment Reform Alignment
For both NYS Medicaid and Medicare, the goal of payment reform is to create the proper incentives for providers to deliver high quality, integrated and patient centered care at a reasonable price. With this joint goal in mind, many of the stakeholders articulated a strong desire for alignment between the Medicaid and Medicare reforms in the State of New York during the process of creating the Medicaid Roadmap. Main arguments included the promise of reduced complexity and administrative burden for providers, the improved ability to strengthen financially weak Safety Net providers, and the opportunity to better address the significant quality and efficiency gaps impeding the care for the dually eligible population. In addition, further alignment in the third largest State in terms of Medicare spending offers the possibility for CMS to make a significant step towards its goal of 50% APM spending by 2018.
Improving the Quality of Care for Patients
The fragmentations in payment methodologies within and between Medicaid and Medicare are mirrored in the fragmented experiences of patients having to navigate care across these systems. Especially for the dually eligible individuals, this experience is matched by significant loss of quality (and cost).4 Many patients covered by NYS Medicaid´s Managed Long Term Care (MLTC) Plans regularly alternate between home care, nursing home care (Medicaid MLTC) and hospital care (mostly Medicare). Many MLTC providers recognize the substantial quality and efficiency gains that are achievable by e.g. reducing the number of people whose end–of–life care is characterized by repeated acute hospital admissions rather than by well–managed care in their home environment. Yet the financial incentives are simply too stacked up against them. A relatively small investment on the Medicaid side of the Medicaid–Medicare divide would save many Medicare dollars, but as long as (virtually) pooling the funds for these dual eligible patients remains impossible or prohibitively complicated, no progress will be made. Similarly, improvements to acute stroke care and other acute conditions affecting the elderly (mostly paid for by Medicare) have the opportunity to significantly reduce long term care dependencies which are often at the expense of the NYS Medicaid program. Again, more closely aligning the Medicare and Medicaid paths to payment reform will realize significant additional savings while increasing care outcomes for both the Medicaid and Medicare program.
These improvements are not limited to the Duals: because of the improved clinical and quality alignment across delivery system reform initiatives facilitated through the proposed alignment, Medicare– and Medicaid–only beneficiaries will equally benefit.
Increasing Impact by Reducing Complexity for Providers
Embracing APMs is a large step for providers, requiring nothing less than a business model change, in addition to significant investments in people and infrastructure. Although the impact of having one significant group of payers (NYS Medicaid MCOs) move towards APMs in a standardized way is substantial, the challenge remains that the next largest payer – Medicare – has its own payment mechanisms, with often contradictory incentives and administrative requirements. Having non–aligned, ambitious payment reform programs running in parallel is a grave risk to the success of both programs. When these programs move in unison, on the other hand, a strong incentive is created for providers to fully embrace the transformation from ´volume´ to ´value´, while significantly reducing the complexity of the required organizational change.
Improved Ability to Strengthen Financially Weak Essential Safety Net Providers
A core goal for DSRIP and its associated payment reform is to create a financially sustainable Safety Net for the State´s most vulnerable citizens. In many instances, this will require a substantial restructuring of these organizations, which is turn will only be viable when the underlying payment system starts to reward prevention over (re–)admissions, and care coordination over fragmentation. In New York State, many Safety Net providers (especially those Upstate) are heavily reliant on Medicare payments for their financial survival; Medicaid reform in and by itself will not suffice if Medicare incentives remain unchanged. Standardizing incentives across Medicaid and Medicare will make the transformation efforts of these financially fragile organizations both urgent enough and feasible.
Why Partner with New York?
As one of the largest States in the country, New York State ranks third or fourth in total number of Medicare beneficiaries (> 3 million), and total annual spend (> $34 billion).5 Aligning the NYS Medicaid reform with the proposed Medicare payment reform will be a significant step for CMS to achieve its goals of realizing 30% of Medicare payments tied to quality or value through alternative payment models by the end of 2016, and 50% of payments by the end of 2018. At this moment, providers see the CMMI Innovation Models as a broad array of individual options they can choose from if they want. The way the NYS payment reform model presents an integrated framework of APMs will help providers to see how the pieces of the puzzle (the individual APMs) can actually fit together in a meaningful, mutually reinforcing way.
In addition, the Roadmap has been created in a process with very active stakeholder participation. Currently, details of the VBP design are being fleshed out in 16 subcommittees, involving over 400 individuals representing all types of providers, managed care organizations, trade organizations, professionals, patient advocates, legal experts, population health & social determinants of health experts, and so forth. This unique amount of direct stakeholder involvement creates a strong commitment to the goals that the State has set. This is a strong foundation for CMS to help realize its goal of 50% of Medicare payments tied to quality or value through APMs by the end of 2018.
Suggested Approaches for Medicaid/Medicare Payment Reform Alignment in NYS
As mentioned in the introduction, the short version of NYS´ proposal is simple:
- NYS proposes to allow its providers and Managed Care Organizations to include Medicaid beneficiaries in CMS innovative payment models. These have already been included in the Roadmap as off–menu options that would be automatically accepted as valid Level 1 or higher VBP arrangements.
- In parallel, NYS requests CMS to allow NYS providers to include Medicare FFS beneficiaries in the VBP Arrangements outlined in the NYS Payment Reform Roadmap.
- Simultaneously, NYS will work with its Medicare Advantage plans to realize a complimentary alignment
- NYS proposes to allow Montefiore Health System to be the first Accountable Care Organization in the country that seamlessly encompasses both duals and Medicaid– and Medicare–only beneficiaries, managing population health and assuming financial risk across the entire spectrum.
Allowing NYS Providers to include Medicaid MCO beneficiaries in Medicare CMMI Innovation Models
NYS providers have been very active and successful participants in several Medicare CMMI Innovation Models (the ACO models, the BCPI program, Primary Care Initiatives, amongst others). NYS proposes to allow its providers and Managed Care Organizations to include Medicaid beneficiaries in CMS innovative payment models ((including the new Cardiovascular Risk Reduction Model). These CMMI models have already been included in the Roadmap as ´off–menu´ options that would be automatically accepted as valid Level 1 or higher VBP arrangements. This approach could be especially attractive for those providers already participating (or considering to participate) in one or more of these models. As these MCO Medicaid–only "off menu" options fall within the parameters of the 1115 waiver and do not affect any of the arrangements for Medicare FFS only or duals, they do not generate any specific requests of CMS.
Allowing NYS Providers to include Medicare FFS beneficiaries in the NYS VBP arrangements6
The large majority of the 3.3 million NYS Medicare beneficiaries is Medicare–only (2.5 million), and over 65% of Medicare beneficiaries are still enrolled in Medicare FFS.7 To significantly increase the numbers of Medicare FFS patients that are channeled through APMs, and thereby increase the overall positive impact of aligned payment reform incentives on the value delivered by the New York State provider community, the State requests that CMS allows providers to include Medicare FFS–only patients in the VBP payment models outlined by the NYS Medicaid Payment Reform Roadmap. This implies that providers could include Medicare patients in their bundled payment arrangements, advanced primary care arrangements, subpopulation arrangements (where applicable) and total population (ACO) arrangements, following the standard guidelines for baseline– and shared savings/losses calculations and outcome reporting as established in the Roadmap.8
In this approach, the Medicaid MCOs would not play a role in the administration of the VBP models to the Medicare FFS only population: providers would continue to receive Medicare reimbursement from CMS directly through the current payment systems. The State would assume the role of administrator for the Medicare FFS population: calculate and administer baseline data, shared savings, potential shared losses and (if required) adaptations to risk adjustment models for the Medicare FFS patients. Because the State is already set to fulfill these functions for the Medicaid MCO population, this additional task will require limited efforts (for the Medicaid MCO population, this is a ´shared service´ for both providers and MCOs). 9 NYS will report to CMS on a quarterly basis on enrollment, shared savings, quality outcomes, and other relevant trends.
Based on the State´s strong track record in bending the cost curve in Medicaid, a similar reduction in overall growth rate of Medicare costs for the included Medicare FFS beneficiaries is expected. In the initial two years, the State proposes to perform this administrative role at no cost to CMS: potential savings would be shared between providers and CMS. When, after two years, the Medicare cost growth rate has been reduced to a to–be–determined level, the State would request a limited portion of these savings for its administrative efforts.
| Inclusion of Medicare–only beneficiaries in NYS Medicaid VBP Models | |
|---|---|
| Benefit | – Allows providers opting for NYS Medicaid VBP models to include Medicare –only FFS beneficiaries into these models leveraging the same infrastructure and organizational change required for both populations – Increases volume of Medicare FFS population being served through APM models, thus directly driving towards CMS´ 2016 and 2018 APM goals. – Increases the momentum for providers to embrace Medicaid VBP models, thus helps to realize the State´s VBP goals |
| Role of MCO | The MCO would not be involved in either the management or the financial/administrative handling of the Medicare FFS beneficiaries. |
| Actions for State | The State would assume responsibility for the calculation and administration of baseline data, shared savings, potential shared losses, and adaptations to risk adjustment models for the Medicare FFS patients. NYS will inform report to CMS on a quarterly basis. |
| Request to CMS | The State requests that CMS allows providers to include Medicare FFS patients in the NYS Medicaid Reform payment models. Additional details (beneficiaries to be excluded; desired adaptations to risk–adjustment models and so forth) can be further discussed. |
In addition to the Medicare-only beneficiaries, there are approximately 800,000 dual eligibles in New York State. Although this is only approx. 25% of Medicare beneficiaries in NYS, they account for over 35% percent of Medicare spending (an estimated 16 billion dollars) and 33% percent of Medicaid spending, or about $17.8 billion a year. Including the Medicare FFS individuals amongst these would meaningfully increase the volume of Medicare payments channeled through APMs. Likewise, including these duals would strengthen NYS´ goals and further help the providers in realizing the common payment reform goals outlined above. Finally, improved care for these beneficiaries could reduce long term dependency on Long Term Care Services, thus enhancing quality of life and reducing the growth of the most expensive duals category.10 Therefore, the State requests that CMS also allows providers to include duals in the VBP payment models outlined by the NYS Medicaid Payment Reform Roadmap. As above, this implies that providers could include these duals in their bundled payment arrangements, advanced primary care arrangements, subpopulation arrangements (where applicable) and total population (ACO) arrangements, following the standard guidelines for baseline– and shared savings/losses calculations and outcome reporting as established in the Roadmap.11
NYS will maximally enroll these individuals in Managed Care plans (including Managed Long Term Care (MLTC) plans) for the Medicaid component of the expenditures. Unlike the existing FIDA program, MCOs would not play a role in the management or administration of the Medicare FFS component of the expenditures for these duals. In line with the philosophy of both the NYS and CMMI´s payment reforms, the providers would be primarily responsible for achieving total cost of care savings in their APMs for these patients. The State would facilitate the providers and MCOs by calculating and administering baseline data, shared savings, potential shared losses and (if required) adaptations to risk adjustment models for these patients, at the total cost of care per APM, including both Medicaid and Medicare components. The savings (and risk) not accruing to the providers would be divided equally among the MCOs and CMS (preferred model) or through another method of allocation (as e.g. the proportion of Medicaid vs Medicare funding within this dual population).
NYS will report to CMS on a quarterly basis on enrollment, shared savings, quality outcomes, and other relevant trends. The State will closely monitor (and report to CMS) the Medicaid – Medicare cost expenditures ratio and total trends for the duals to avoid potential cost–shifting.
As above, in the initial two years, the State proposes to perform this administrative role at no cost to CMS. When, after two years, the Medicare component cost growth rate in this population has been reduced to a to–be–determined level, the State would request a limited portion of these savings for its administrative efforts.
| Inclusion of dually eligible Medicare FFS beneficiaries in Medicaid VBP Models | |
|---|---|
| Benefit | – Allows providers opting for NYS Medicaid VBP models to include Medicare FFS duals into these models, thereby enabling them to leverage the same infrastructure and organizational arrangements for both Medicaid and this dual population. – Increases the volume of Medicare FFS population being served through APM models, directly serving CMS´ 2016 and 2018 APM goals. – Increases the volume of Medicaid beneficiaries being served through the New York State VBP models |
| Role of MCO | This population would be enrolled in Managed Care for the Medicaid component. The MCO would not be involved in either the management or the financial/administrative handling of the Medicare FFS component of this care. |
| Actions for State | Where that has not already happened, the State would enroll these beneficiaries in Managed Care for the Medicaid component. Subsequently, it would assume responsibility for the calculation and administration of baseline data, shared savings, potential shared losses, and (if required) adaptations to risk adjustment models for these duals, all at the total cost of care per APM (including Medicare and Medicaid). |
| Request to CMS | The State requests that CMS allows providers to include the Medicare component of Medicare FFS dual beneficiaries in the NYS Medicaid Reform payment models. Additional details (beneficiaries to be excluded; desired adaptations to risk-adjustment models and so forth) to be further discussed. The savings (and risk) not accruing to the providers would be divided equally among the MCOs and CMS (preferred model) or through another method of allocation (as e.g. the proportion of Medicaid vs Medicare funding within this dual population). |
Stimulate Medicare Advantage plans to align their payment methods with NYS Medicaid Roadmap and CMMI models
In NYS, 35% of Medicare beneficiaries are enrolled in Medicare Advantage plans. In some counties, such as Niagara and Eerie County, but also the Bronx, more than 50% of beneficiaries are enrolled in Medicare Advantage plans. In some cases, these plans are owned by insurers that also provide Managed Care Plans for Medicaid beneficiaries.
The State will work with these plans to request maximal alignment between the MCO and MA plans, so that providers are confronted with maximally similar VBP arrangements, rules and outcome measures. This increases the opportunity for both providers and Medicare Advantage plans to align contracts across payers, better integrate the delivery of care and create shared savings. This would not be an actual integration of these plans or of the risk pools; financially, the MCO and MA plans would be operated independently from each other as they are now. Shared savings/losses could either be compartmentalized per system (Medicaid/Medicare), or contractual arrangements could be created between the plans to allow for ´virtual´ pooling within the statutory limits in place for both types of plans.
| Working with Medicare Advantage Plans to align with Medicaid Payment Reforms and CMMI models | |
|---|---|
| Benefit | – Creates another option to integrate and better align Medicaid and Medicare spend through aiming at the MLTC duals within Medicare Advantage. – Furthers momentum for CMS´ ambitions for Medicare Payment Reform |
| Role of MCO | In this Approach, the Medicare Advantage Plans would obtain the opportunity to request a Medicaid ´wrap around´ which would allow them to manage the total Medicaid and Medicare expenditures for these patients. |
| Actions for State | Assess interest amongst MA plans and prepare ´wrap around´ functionality. This functionality would require contracting with ´special needs´ ACOs specifically focused on the MLTC duals subpopulation. |
| Request to CMS | [to be investigated whether permission from CMS is required here; this could fall entirely fall within the confines of the 1115 waiver and the regulatory framework for MA plans] |
Montefiore Health System as first mover towards truly integrated care: the Patient First demonstration
NYS is proud to be the home of the nation´s most successful Medicare Pioneer ACO, Montefiore Health System. To generate momentum towards the goals shared by both CMS and NYS, and to make visible what the benefits are of truly integrated care for patients, providers and (public) payers alike, NYS proposes to allow Montefiore Health System to be the first Accountable Care organization that assumes full financial risk and population health responsibility for its entire Medicaid and Medicare population. Montefiore´s proposal (see attached document) describes an approach firmly grounded in population– health, with the care following the needs of the patient rather than the system. This implies reducing administrative complexity so that more healthcare dollars can be directed toward patient care; replacing ´within–silo´ coordination with care management across the continuum of care regardless of origin of payment; and aligning care pathways, care improvement programs and quality targets across these same silo´s so as to create synergy and scale.
The demonstration serves as a template for arrangements between providers and payers entering into mature value–based payment arrangements in New York and a vision for the nation on how to incentivize providers and payers to manage patients holistically.
See the attached document for more details. [Document to be circulated separately]
________________________________
1. Currently, most value–based payments consist of pay for performance (P4P) models where a bonus or withhold is tied to the achievement of (mostly process–based) quality targets. In these models, the underlying Fee–for–Service (FFS) payment mechanism remains intact, and there is no incentive for providers to take overall outcomes or costs into account. In Alternative Payment Mechanism, the core drive is to move away from FFS towards e.g. ACOs or bundled payments, where providers will ultimately get paid for outcomes rather than inputs, and are rewarded for delivering high value care. APMs take a patient–centered perspective (the money follows the patient) rather than the traditional provider–centered FFS model, driving providers to cooperate and improve the contribution of their collective efforts on the overall outcomes and costs for the patient. 1
2. In NYS Medicaid, this population is called the HARP (Health and Recovery Plan) population. 2
3. Better Care. Smarter Spending. Healthier People: Paying Providers for Value, Not Volume. CMS Fact Sheet, 01–25– 2015. www.cms.gov/Newsroom/MediaReleaseDatabase/Fact–sheets/2015–Fact–sheets–items/2015––01–26–3.html. 3
4. Committee on Quality of Health Care in America. Crossing the quality chasm: a new health system for the 21st century. Washington, DC: National Academy Press; 2001; Chattopadhyay A, Bindman AB. Linking a comprehensive payment model to comprehensive care of frail elderly patients: a dual approach. JAMA. 2010;304:1948–9; Samis S, Detty A, Birnbaum M. Integrating and Improving Care for Dual Medicare–Medicaid Enrollees: New York´s Proposed Fully Integrated Duals Advantage (FIDA) Program. New York: United Hospital Fund, 2012. 4
5. 2012 resp. 2009 data, Kaiser Family Foundation data (http://kff.org/medicare/state–indicator/total–medicare–beneficiaries/). California and Florida are ranked first and second. Depending on the exact year and metric, NYS and Texas alternate 3rd and 4th position. 5
6. At this point, our proposal excludes the developmentally disabled dually eligible population, as this population is not yet transitioned to Medicaid Managed Care. 6
7. Medicare Enrollment 6–15 file, https://www.cms.gov/Research–Statistics–Data–and–Systems/Statistics–Trends–and–Reports/MCRAdvPartDEnrolData/MA–State–County–Penetration–Items 7
8. These guidelines are currently being further detailed by DOH based on recommendations from the VBP Work Group and its Subcommittees. 8
9. This arrangement assumes that at least initially, Level 3 arrangements (prospective payments) are out of scope. The State suggests to start discussing the appropriate approach for those providers aiming at a Level 3 VBP arrangements after one or two years of experience with the approach proposed here. 9
10. Al Dobson, ´Can Medicare Acute and Post–Acute Care Payment Bundles Improve Care for Dual Eligibles´?, National Dual Eligibles Summit 2012, http://www.ehcca.com/presentations/dualeligible1/3.5.pdf. 10
11. These guidelines will be further detailed in the forthcoming months. 11
Follow Us