Value Based Payment Quality Improvement Program (VBP QIP)
Update Webinar
- Webinar also available in Portable Document Format (PDF)
November 2016
Today´s Agenda
- VBP QIP Updates
- Contracting for VBP
- VBP Contracting
- VBP Contract Terms
- VBP Contracting for Beginners
- Important Information
- Next Steps and Q&A
VBP QIP Timeline Update
Group 1 Key Upcoming Dates
| Milestone | Due Date |
|---|---|
| First steps towards VBP undertaken with PPS & MCO oversight in accordance with approved Facility Plan | Ongoing |
| Partners must reach Level 1 VBP contracting | March 31, 2017 |
Group 2 Key Upcoming Dates
| Milestone | Due Date |
|---|---|
| MCOs submit a revised VBP QIP Governance Document to DOH for review | December 9, 2016 |
| Final Facility Plans approved by MCO in collaboration with PPS (final copies should be sent to DOH) | December 9, 2016 |
| Partners must reach Level 1 VBP contracting | March 31, 2017 |
Note: Although deliverables can be completed before the red dates noted on the VBP QIP Timeline, DOH encourages participants to complete them as soon as possible, as the majority of VBP QIP in DY2 focuses on setting up VBP contracts, which must be in place between Facilities and MCOs by April 1st, 2017.
Acronyms:
MCO – Managed Care Organizations
PPS – Performing Provider Systems
DOH – Department of Health
DY – Demonstration Year
VBP QIP Governance Documents
- A blank Governance Document Scorecard can be found on the DOH VBP QIP website.
- The Scorecard outlines the areas DOH reviews, which MCOs can use to establish a solid approach for overseeing their program. This will reinforce the integrity of the program and will foster the parameters for MCOs to assist paired Facilities with achieving their VBP QIP objectives.
- Group 2 MCO Governance Documents are due on Friday, December 9th, 2016.
VBP QIP Facility Plans
- The Facility Plan Template provides guidance to participants on the information each party should consider when putting together their VBP facility plan.
- The Facility Plan Template can be found on the DOH VBP QIP website
- Group 1 Facility Plans were submitted to DOH on Friday, September 16th, 2016.
- Finalized Facility Plans should have been approved by partnered MCOs and PPS.
- DOH will schedule debrief calls with each of the Group 1 MCOs to discuss the VBP QIP Facility Plans and oversight responsibilities of the MCOs moving forward.
- Group 2 Facility Plans are due to DOH by Friday, December 9th, 2016.
VBP QIP Financing
- VBP QIP DY 2 Rates – April 2016 Rate Package
- DOH´s submission of the DY2 Rate Package to CMS & Division of Budget (DOB) was delayed
- DOH worked with DOB to gain approval for a state–funded advance for 3rd Quarter 2016 (October 2016 – December 2016) to get VBP QIP funds to the MCOs
- Advance until April 2016 rates are approved by CMS & DOB
- DOH anticipates the April 2016 rate package to be approved in late December 2016
- The State recouped advances made to MCOs for the 1st & 2nd Quarters of DY2 before the State had loaded the April 2016 (DY2) rate package
- DOH is currently working on resolving the issue and MCOs can expect to receive the funds within the coming days
- Please e–mail bmcr@health.ny.gov with any questions that you may have regarding this issue
Contracting for VBP
(Must be achieved by April 2017)
Contracting Entities / VBP Contractors
- Independent Practice Associations (IPA)
- Accountable Care Organizations (ACO)
- Individual Providers*
- Hospitals and/or Hospital Systems
- Federally Qualified Health Centers (FQHC) and large medical groups
- Smaller providers including community based organizations (CBOs)
*!
- Individual provider could either assume all responsibility and upside/downside risk or make arrangements with other providers; or
- MCOs may want to create a VBP arrangement through individual contracts with these providers
MCOs and Contractors Can Choose Different Levels of VBP
In addition to choosing which integrated services to focus on, the MCOs and contractors can choose different levels of VBP:
| Level 0 VBP | Level 1 VBP* | Level 2 VBP | Level 3 VBP (feasible after experience with Level 2; requires mature contractors) |
|---|---|---|---|
| FFS with bonus and/or withhold based on quality scores | FFS with upside-only shared savings available when outcome scores are sufficient (For PCMH/ APC, FFS may be complemented with PMPM subsidy) | FFS with risk sharing (upside available when outcome scores are sufficient) | Prospective capitation PMPM or Bundle (with outcome-based component) |
| FFS Payments | FFS Payments | FFS Payments | Prospective payments |
| No Risk Sharing | ↑ Upside Risk Only | ↑↓ Upside & Downside Risk | ↑↓ Upside & Downside Risk |
*As part of their participation in VBP QIP, Facilities must reach Level 1 VBP Contracting by April 1, 2017.
Acronyms:
FFS – Fee–for–Service
PCMH – Patient Centered Medical Home
PMPM – Per Member Per Month
APC – Advanced Primary Care

There are Numerous Options for VBP Contracting
- There is not a single path towards VBP. Rather, there are a variety of options that MCOs and providers can jointly choose from.
- Total Care for General Population (TCGP)
- Total Care for Special Needs Population (HIV/AIDS, HARP)
- Per integrated service for specific condition: Maternity Care bundle
- For Integrated Primary Care: includes Chronic Care bundle
- These VBP arrangements are limited to Medicaid–only members.
- Duals will be integrated in the VBP arrangements from 2017 on.
Different Types of VBP Arrangements
| Types | TCGP | IPC | Care Bundles | Special Need Populations |
|---|---|---|---|---|
| Definition | Party(ies) contracted with the MCO assumes responsibility for the total care of its attributed population | PCMH or APC includes:
|
Episodes in which all costs related to the episode across the care continuum are measured
|
Total Care for the Total Subpopulation
|
| Contracting Parties | IPA/ACO, Large Health Systems, FQHCs, and Physician Groups | IPA/ACO, Large Health Systems, FQHCs, and Physician Groups | IPA/ACO, FQHCs, Physician Groups and Hospitals | IPA/ACO, FQHCs and Physician Groups |
Note that the contracting parties in most of these VBP arrangements are not single entities; but rather, groups of providers working together to manage the care of a population. VBPQIP facilities, through improving quality (tied to their VBPQIP transformation plan measures) and through experience performing well in VBP Level 1 contract, will position themselves to be attractive partners in larger VBP contracting arrangements.
|top of page|Achieving Financial Benefits from VBP Contracting
For Hospitals, which don´t employ large numbers of community–based primary care providers, the financial benefits of participating in VBP contracting come from several different sources, driven by the VBP contract Level
Level 0: Participation in VBP QIP requires facilities to engage with a single MCO partner to earn payments based on improving quality. Qualification for payments is driven by "Pay for Performance" on achieving specific quality and process metrics outlined in the facility´s VBPQIP transformation plan.
Level 1: Level 1 contracts negotiated by the VBPQIP facility (before joining a larger VBP contracting entity) with all of its Medicaid MCO partners provide two additional opportunities for hospitals to financially benefit:
- Participating in a shared saving pool by delivering care at a cost below their negotiated target budget (based on a point below their "DRG rate")
- Gain experience in VBP contracting and VBP performance with downside risk and will allow for the development of a positive VBP track-record to make the facility a more attractive partner to larger VBP contracting entities (IPA/ACO)
Levels 2 and 3: Working with IPA, ACO or other partners, sharing in savings from various VBP arrangements (e.g., TCGP, IPC)
|top of page|Chronic Care Bundle
Facilities which demonstrate high quality and cost efficiency will be very attractive to provider partners contracting for VBP arrangements which include the costs related to the care and treatment of their attributed populations
Includes 14 chronic conditions:
- Asthma
- Bipolar
- Diabetes
- Depression and Anxiety
- Chronic Obstructive Pulmonary Disease (COPD)
- Congestive Heart Failure (CHF)
- Coronary Artery Disease (CAD)
- Arrhythmia
- Heart Block/Conduction Disorders
- Hypertension
- Substance Use Disorder
- Lower Back Pain
- Trauma and Stressors
- Osteoarthritis
- Gastro–Esophageal Reflux
Two criteria determined the current list of chronic conditions:
- Lead provider is, should and/or can be part of Integrated Primary Care (coordination with specialty care when needed is key)
- Highest volume and costs within Medicaid program
VBP Contracting for Beginners
Typical Provider Contract Terms*
- Parties and Definitions
- Scope of Services and Access to Services
- Payment Adjustments
- MCO Administrative Requirements (i.e. timely filing)
- Insurance
- Indemnification and Liability
- Compliance with all laws and Medicaid Model Contract
- Term and Termination
- Representations and Warranties
- Amendment
- Assignment
- Notices to MCO
- Dispute Resolution or Litigation
- Audits, Monitoring and Oversight
- Quality Metrics and Baseline Budget
* Details of the Provider Contract Terms can be found in Appendix A
|top of page|Contracting VBP: Top 4 Steps for Beginners
| 1 | Assess your readiness; address issues to be able to start at Level 1 |
| 2 | Understand what types of contracts you want to engage in based on the services you provide, the attributed population and outcome measures that impact savings, and the potential for realizing savings |
| 3 | Familiarize yourself with and utilize available resources (data from the State, technical assistance from potential partnering contractors, etc.) |
| 4 | Choose the partners that will help you succeed and that are adequate for the contracts you chose – build your partnerships |
Bolded print signifies priorities that facilities should be focusing on immediately
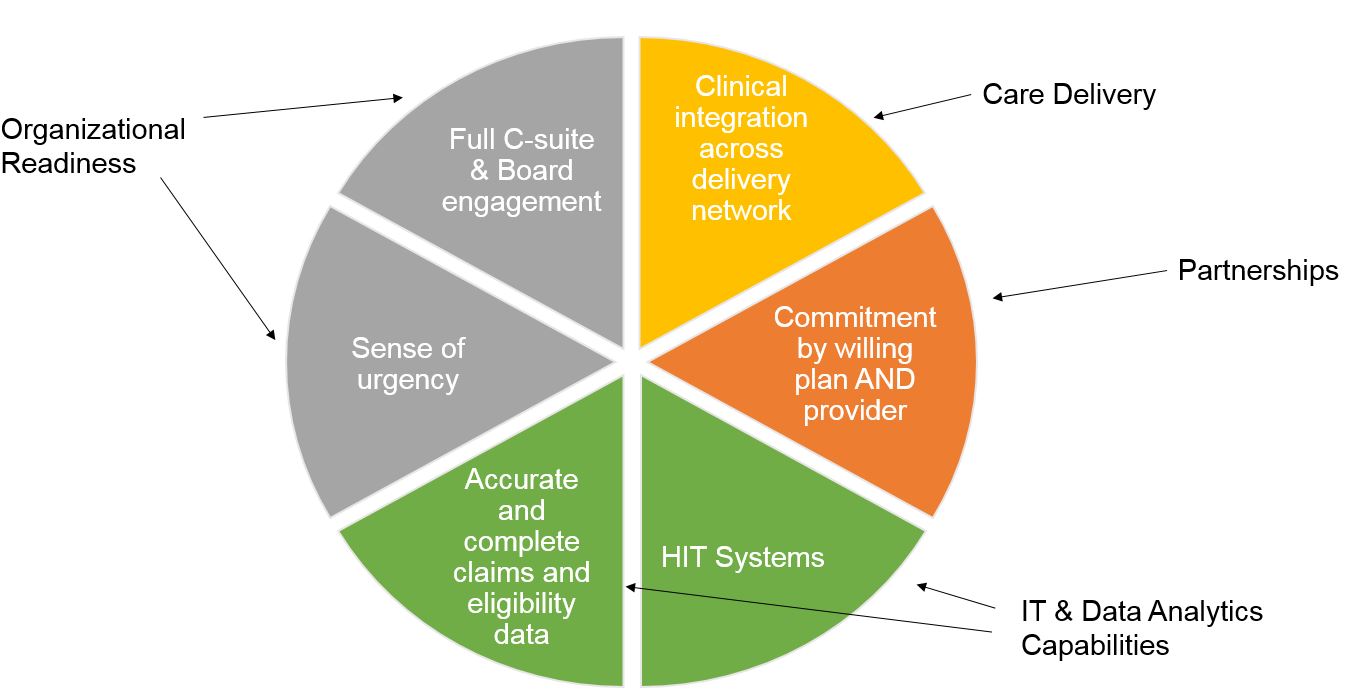
Keys to Achieving Level 1 by April 2017
Acronyms:
HIT – Health Information Technology
Clinical Advisory Groups (CAG) Objectives
CAG members convened to meet the following objectives:

CAG Reports, available on the DOH website, contain the recommendations provided by each CAG, specific to VBP arrangement definition and quality measures.
Facilities Responsibilities Leading into April 2017
- Leading into the contracting deadline of March 31st, 2017, VBPQIP facilities must:
- Review all current Medicaid MCO contracts
- Identify provisions which need modification to meet roadmap requirements for VBP contracts of Level 1 or above
- Negotiate with all current MCOs with which they contract/agree on which provisions need modifications
- Review/Develop baseline budgets
- Develop and execute contracts with each Medicaid Plan
- Facilities do not need to send their actual VBP contract(s) with other MCOs to their VBP QIP MCO partner
- To document that there is a VBP contract in place, facilities should provide an attestation to their VBPQIP MCO partner, signed by contracting VBP MCO stating that the MCO is in a Level 1 VBP contract with the facility
Final Thoughts
Important Information
VBP Support Materials
VBP Resource Library:
- Path: DSRIP Homepage → Value Based Payment Reform → VBP Resource Library
- Link: https://www.health.ny.gov/health_care/medicaid/redesign/dsrip/vbp_library
VBP Bootcamps Website:
- Path: DSRIP Homepage → Value Based Payment Reform → VBP Bootcamps
- Link: https://www.health.ny.gov/health_care/medicaid/redesign/dsrip/vbp_library
VBP Website:
- Path: DSRIP Homepage → Value Based Payment Reform
- Link: https://www.health.ny.gov/health_care/medicaid/redesign/dsrip/vbp_reform
Thank you for your continued support with VBP QIP!
- DOH will be reaching out to Group 1 MCOs to discuss the Facility Plans
- The next VBP QIP Update Webinar is scheduled for Wednesday, December 21st from 2:00 pm – 3:00 pm.
- Please let DOH of any topics that you would like discussed during next month´s webinar by submitting your requested topics to the VBP QIP inbox (vbp.qip@health.ny.gov).
- The remainder of this webinar is reserved for Q&A and an open forum session.
For any further questions, please contact the VBP QIP inbox: vbp.qip@health.ny.gov
|top of page|Appendix A
Provider Contract Key Terms
Out of the entire list of terms these are the most important:
1. Payment Adjustments
- Need to understand how these activities will be handled (for example, the timeframe and notice requirements and payment implications)
- Timely filing of claims
- Adjustments to payments
- Claim disputes and dispute resolution
- Retroactive enrollments
- Recoupments
2. Insurance
- MCOs will require providers to have malpractice insurance and general liability insurance
- Provider should understand its insurance limits and policy restrictions (Is contractual indemnification allowed?)
3. Indemnification and Liability
- Contractual indemnification – mutuality
- An MCO can´t transfer liability for its own acts onto a health care provider
- Joint and several liability
4. Term and Termination
- Automatic renewal or defined contract term
- "For cause" versus "without cause" termination
- Standard for material breach
- Length of notice for termination and non–renewal
- Due process rights
5. Representations and Warranties
- Valid corporation and properly licensed, certified or designated by DOH, OMH or OASAS (licensure obligations can also apply to employees of the provider)
- Legally binding and enforceable
- Neither provider nor employees have been suspended or terminated from a federal healthcare program or convicted of a criminal offense related to Medicaid or Medicare
6. Amendment
- Mutual agreement, automatic or upon 30 days´ notice without objection
- Changes due to regulatory requirements
7. Assignment
- On notice or with consent
- Change of control
8. Notice to MCO in the event the provider has:
- Any lapse, revocation, termination or suspension of license
- Any lapse, revocation or cancellation of insurance
- A disciplinary action initiated by a government agency
- Excluded, suspended, debarred or sanctioned from a federal program
- A grievance or legal action filed by an enrollee against the provider
- An investigation, conviction or plea for fraud, a felony, or a misdemeanor
9. Dispute Resolution / Litigation
- Claim disputes vs. other disputes
- Venue and choice of law
- Internal dispute resolution mechanism
- Timeframe for resolution
- Identify key management titles with the authority to resolve disputes
- Alternative dispute resolution or mediation
- Binding or non-binding
- American Arbitration Association, American Health Lawyers Association, etc.
10. MCO´s right to monitor and audit its participating provider
Below are some of the key provisions covered by Law. Providers should expect their MCO to include these in the VBP Contracts:
- Provisional credentialing
- Medical necessity appeals
- External appeals
- Limits on prior authorization
- Prudent layperson
- Prompt pay – timeframes and interest
- Overpayments
- Claim submission timeframes and exceptions
- No balance billing of consumers
- Continuity of Care
- Term and Termination
- Sharing of enrollee medical records and other personal health information, including HIV, substance abuse (SA), and mental health (MH) records
- Consent obtained on Medicaid enrollment application
Follow Us