VBP QIP Demonstration Year 4 Guidance Document
- Guidance is also available in Portable Document Format (PDF)
Updated as of 5/10/18
Table of Contents
P4R Penalties and Measure Credits
VBP QIP Facility Plan Schedule & Key DY3 Goals
Appendix A: Deliverable Submission Table
Purpose of this Document
The purpose of this document is to provide Value Based Payment Quality Improvement Program (VBP QIP) participants information to progress into the fourth demonstration year (DY4) of the program. This document is designed to be useful to both Group 1 and Group 2 participants. This document should be considered as a supplement to other programmatic documents released by DOH, including guidance documents, frequently asked questions, presentations, etc.
|top of section| |top of page|VBP QIP Payments
VBP QIP is designed to provide distressed facilities the opportunity to earn program payments through both Pay for Performance (P4P) and Pay for Reporting (P4R) activities. With performance measures and VBP contracting milestones established in the Facility Plan, VBP QIP funds have begun flowing to facilities based on achievement of those established measures and milestones in DY3.
In DY4, P4R and P4P will occur simultaneously. P4R funds represent 20% of DY4 total funds, and these dollars will be earned if the facility is able to achieve 80% of their Medicaid Managed Care revenue in VBP arrangements by June 29, 2018. This date has been revised from the original P4R deadline of April 1, 2018. P4P funds account for 80% of DY4 total funds and they are earned by facilities demonstrating improvement on the measures selected in the Facility Plans. In DY5, all programmatic funds flow through achievement of performance metrics. [See Figure 1a & 1b below for details].
Figure 1a: DY3–DY5 Annual Payment Distribution
| DY3 | DY4 | DY5 | |
|---|---|---|---|
| VBP Contracting Progress (P4R) % |
50% (Paid in Q1 & Q2) |
20% | 0% |
| Performance Improvement (P4P) % |
50% (Paid in Q3 & Q4) |
80% | 100% |
Figure 1b: DY3–DY5 Quarterly Payment Distribution
| DY3 | DY4 | DY5 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | Q1 | Q2 | Q3 | Q4 | Q1 | Q2 | Q3 | Q4 | |
| VBP Contracting Progress (P4R) % |
25% | 25% | 5% | 5% | 5% | 5% | 0% | |||||
| Performance Improvement (P4P) % |
25% 1 | 25% | 20% | 20% | 20% | 20% | 25% | 25% | 25% | 25% | ||
*All percentages are a proportion of annual payments
P4R activities are designed to assess progress made towards VBP contracting arrangements.
P4P activities are designed to capture improvements in quality through measurement of performance outlined in the Facility Plan.
|top of section| |top of page|P4P Measure Selection
As part of the submission of the VBP QIP Facility Plan, each facility was instructed to select six (6) All–Payer2 quality measures for pay for performance (P4P) evaluation. the facility will be assessed on its performance on these quality measures for the remainder of VBP QIP, barring corporate restructuring/reorganization.
Retired Measure Substitution
In the event that a facility has selected a measure that has been identified to be retired, the facility must select a substitute measure from the same measure focus area/domain (i.e., timely and effective care).
Figure 2 provides the menu of All–Payer quality developed by the Office of Quality and Patient Safety (OQPS) for the purpose of VBP QIP:
- Nationally recognized measures (e.g. NQF, NCQA, AHRQ, CMS, CDC)3
- Avoidable hospital use measures
- Measures tracking Hospital Acquired Infections.
Figure 2: VBP QIP Recommended P4P Measure Menu
| # | Measure Name | Data Steward | Focus Area/Domain |
|---|---|---|---|
| 1 | Acute MI Mortality (IQI #15) | AHRQ | Mortality |
| 2 | Stroke Mortality (IQI #17) | AHRQ | Mortality |
| 3 | Pneumonia Mortality (IQI #20) | AHRQ | Mortality |
| 4 | CAUTI Rate per 10,000 Patient Days (Population Rate) or CAUTI Rate per Device Days | NHSN | Hospital Acquired Conditions |
| 5 | CLABSI per 10,000 Patient Days (Population Rate) or CLASBI per Device Days | NHSN | Hospital Acquired Conditions |
| 6 | CDI Healthcare Facility – Onset Incidence Rate per 10,000 Patient Days | NHSN | Hospital Acquired Conditions |
| 7 | Falls with Injury | NDNQI | Hospital Acquired Conditions |
| 8 | 3–Hour Sepsis Bundle | NYSDOH | Hospital Acquired Conditions |
| 9 | Pressure Ulcer Rate, Stage III or IV | NDNQI | Hospital Acquired Conditions |
| 10 | Episiotomy Rate | Pediatric Measure Center of Excellence | Maternity |
| 11 | Primary C–Section (IQI #33) | AHRQ | Maternity |
| 12 | Avoidable ED Use | 3M 4 | Utilization |
| 13 | Avoidable Admissions | 3M 4 | Utilization |
| 14 | Fibrinolytic Therapy Received with 30 minutes of ED Arrival (OP–2) | CMS | Timely and Effective Care |
| 15 | Median Time to Transfer to Another Facility for Acute Coronary Intervention (OP–3) | CMS | Timely and Effective Care |
| 16 | Median Time to ECG (OP–5) | CMS | Timely and Effective Care |
| 17 | EDTC Emergency Department Transfer Communication (All or None) | NQF/ Stratis Health | Transitions of Care |
The highlighted measures are available for selection for only Rural and Critical Access hospitals. For the purposes of VBP QIP, a hospital is classified as rural if it has fewer than 100 licensed medical/surgical beds.
Once the facility has selected a substitute measure, the facility must submit a Retired Measure Substitution Form prior to the expiration of the retiring measure. Once DOH has approved the measure, the facility must notify their paired MCO of the newly selected measure. Facilities will be required to submit the baseline and quarterly performance retroactive to June 2017.5
As an alternative, facilities were permitted to choose quality measures not included in Figure 2 as long as the measures selected follow criteria similar to the OQPS measure selection logic listed on the previous page. If alternate measures were chosen, the facility is required to not only document the reasons for using alternatives measures, but also state how data will be collected and reported to its paired MCO. If the facility had not previously selected two (2) alternative measures, the facility may select one as a replacement for a retiring measure if the measure falls within a similar domain/focus area. As with all measures in the Facility Plan, the facility´s paired–MCO has to review and accept an approach using alternate measures. Recommended criteria for alternate measure selection include:
- Other nationally recognized measures not included in Figure 2.
- Measures similar to nationally recognized measures that are currently in use at the facility as part of existing quality improvement efforts. Some examples fitting this description may include measures with facility–defined specifications related to:
- Length of stay
- Hospital acquired infections
The facility should select alternate measures where it has the ability to show improvement. Some examples of alternate measures could include:
- Sepsis Mortality
- Care Transition Measure (HCAHPS – CTM–3)
- ED–1 Median time for ED arrival to ED departure for admitted ED patients
- ED–2 Admit Decision Time to ED Departure Time for Admitted Patients
- SSI
- 6–hour Sepsis Bundle
- MRSA Infection Rate
- AMI–08a Primary PCI Received Within 90 Minutes of Hospital Arrival
- VTE–6 Incidence of potentially preventable VTE
PPS/Facility Partnership in Measure Selection
VBP QIP facilities and their paired PPS are expected to collaboratively select the six P4P quality measures. A facility´s selected measures should align with the PPS´ DSRIP goals and the paired PPS should also provide support (non–financial) and guidance to the participating facility. By the facility and PPS aligning measures, the PPS can help the facility identify areas of improvement that will not only help the facility meet its VBP QIP metrics, but also help the PPS meet its DSRIP metrics. The facility will not only benefit by focusing on a specific set of actions to perform well in both the VBP QIP and DSRIP program, but the facility will also benefit from guidance and help the PPS can share in aligned areas.
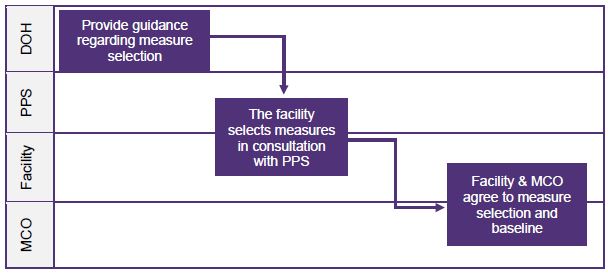
For reference, Figure 3a (below), provides a visual on the measure selection process that should be undertaken in developing a VBP QIP Facility Plan.
Figure 3a: Measure Selection Process
P4P Measures with Low Denominators
- If a facility selects a measure where the denominator is under 30 events for a given reporting period, that measure´s performance cannot count as achieved for the reporting period. Hence, the facility´s P4P performance for the period would then be based on the 5 other valid measures with the facility needing to achieve four (4) out of five (5) remaining valid measures to ensure it earns the full allowable payment for that period.
- If multiple denominators are invalid during the same reporting period, more valid measures will need to be achieved for a facility to earn full payment for the period. Performance for at least 4 measures will need to be achieved in a reporting period for the facility to earn full payment for that period.
- If 3 or more measures have invalid denominators during a reporting period, the facility will earn up to the amount of achieved valid measures. Since less than 4 valid measures can be achieved, unearned P4P dollars will be available through the AIT.
- The facility could also not earn performance for a measure where the rolling annual denominator was less than 30 in the following/next quarter, because there would not be a most recent valid rolling annual quarter with which to measure success. Therefore, the measure would be reported to the MCO and recorded so that the valid quarterly measurement could be used as a baseline to assess the performance on the measure in the following quarter. Hence, for a reporting period following a period where a facility was not able to report valid performance, the facility´s P4P performance for the period would then be based on the other measures with valid denominators with the facility needing to achieve 4 of the remaining measures with valid denominators to ensure it earns the full allowable payment for that period.
- If a facility´s measure denominator is invalid for two or more periods during a baseline measurement or performance measurement period, the measure will be deemed invalid and will not be considered for AIT, meaning that the facility will need to achieve other measures with valid AIT baselines and performance measurements to receive AIT awards.
Figure 3b (below) illustrates a scenario where multiple measures´ denominators fall below the allowable threshold throughout a demonstration year.
In DY4 Q1, this non-rural facility has three (3) measures where denominators were less than 30. Since the facility is required to achieve four (4) out of six (6) measures to receive 100% of the quarterly award amount, the facility could only receive a maximum of 75% of the quarterly award amount in DY4 Q1 if it achieves three (3) out of the three (3) remaining measures.
Although the six (6) measures have denominators of at least 30 in DY4 Q2, the three (3) measures that were invalid in the prior quarter are still invalid because there is no baseline from the prior quarter to compare the current quarter against. Since the facility is required to achieve four (4) out of six (6) measures to receive 100% of the quarterly award amount, the facility could only receive a maximum of 75% of the quarterly award amount in DY4 Q1 if it achieves three (3) out of the three (3) remaining measures.
All six (6) measures have valid denominators in DY4 Q3. The three (3) measures that were originally invalid in DY4 Q1 had denominators are now valid in DY4 Q3 because they have denominators above 30 and a baseline from the previous quarter. The facility needs to achieve at least four (4) out of six (6) measures to receive 100% of the DY4 Q3 award amount.
In DY4 Q4, the denominator for Measure 6 falls below 30 again. Therefore, the denominator is deemed invalid for DY4 Q4 and the facility is required to achieve four (4) out of five (5) valid measures to receive 100% of the DY4 Q4 award amount.
Figure 3a: Example of P4P Measures with Low Denominators
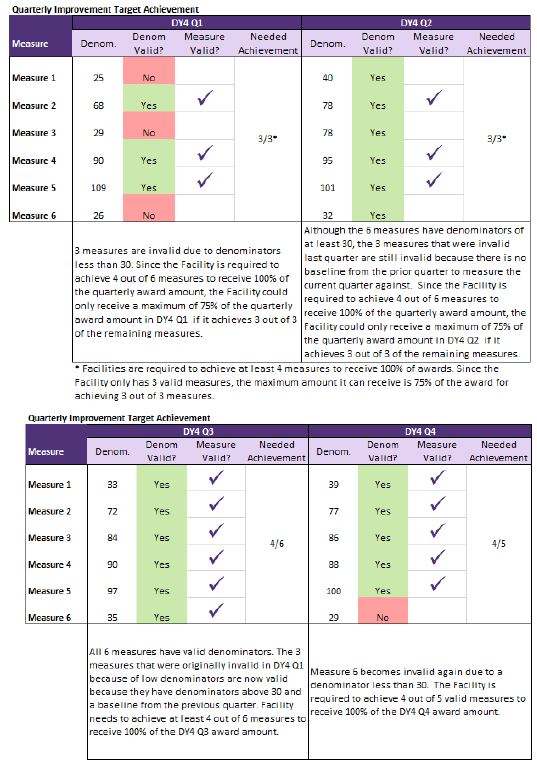
The facility has the opportunity to earn the previously unearned P4P funds that it missed in DY4 Q1 and DY4 Q2 if it meets its AIT. Since the denominators for Measures 1 and 3 only fell below 30 for one (1) quarter, they are still valid to evaluate for performance for AIT. Conversely, since the denominator for Measure 6 fell below 30 for more than one (1) quarter in DY4, this measure is deemed invalid when evaluating AIT. Therefore, the facility would need to achieve performance in four (4) of the five (5) remaining measures to meet its AIT.
Annual Improvement Target Achievement
| Measure | Valid for DY4 AIT | Measure Valid? | Needed Achievement/ Valid Measures |
|---|---|---|---|
| Measure 1 | Yes | ✓ | Facility has the opportunity to earn back unearned funds from DY4 Q1 and Q2. Since Measure 6 had two or more instances of denominators under 30 during the year, the measure is invalid for AIT. Therefore, the facility needs to achieve at least 4 out of the 5 remaining measures to receive 100% of the remaining funds. |
| Measure 2 | Yes | ✓ | |
| Measure 3 | Yes | ✓ | |
| Measure 4 | Yes | ✓ | |
| Measure 5 | Yes | ✓ | |
| Measure 6 | No |
P4P Measure Reporting
P4P measure results will be provided quarterly using a "rolling annual" calculation. A "rolling annual measurement" process is being utilized to not only minimize the impact of any unusual variations in any given DY quarter´s results, but to also minimize issues pertaining to low denominators.
Facilities, through a report on measure performance accompanied by an attestation signed by a senior leader within the facility6, will submit their P4P measure results to their VBP QIP paired MCO four times a year following the completion of each DY quarter. DOH recommends a 180–day timeline from the quarterly measurement period end for MCOs to notify facilities of their decision on the report and prepare payment.
While the terms are to be agreed upon between the paired MCO and facility, DOH proposes that facilities submit quarterly reports to the MCO no later than one hundred and twenty (120) days following the close of each DY quarter. In reporting quarterly to the MCOs on their results, the facilities will compare the most recently completed DY quarter´s rolling annual results with the immediately preceding DY quarter´s rolling annual results.
In addition, as part of the Facility Plan development process, it is recommended that for each measure facilities also include measure collection and reporting specifications. This will not only ensure consistency of self–reported data, but also serve as a reference should any governing body, choose to review measure performance. These measure collection specifications should include, at minimum, numerator and denominator information for each quality measure, but also details as to how the facility pulls, aggregates and reports measurement information. PPS and MCOs should be engaged in this process.
Furthermore, due to the possibility that there may be only small differences in performance between reporting periods, partners should also consider agreeing to the number of places after the decimal point used in calculating and reporting on performance. These mutual decisions should be stated in the measure specifications that the facility provides to the MCO. For partner´s information, NYSDOH usually uses four places after the decimal (ten– thousandths) when calculating and reporting on performance measures.
Finally, DOH proposes that MCOs have a 60–day period to review reports, notify the facility of their decision, and prepare payment. Specifically, DOH recommends MCOs complete their review and approval of VBP QIP related reports no later than 45 days after the initial submission of materials from the facility. This will allow the remaining 15 days within the 180– day reporting and review cycle for the MCO to notify facility and PPS partners of their decision and to finalize payment procedures, so that the MCO can execute payment (as long as the MCO has received payment from DOH for that payment cycle).
|top of section| |top of page|P4P Measure Evaluation
The section below describes the recommended mechanism MCOs and facilities could use in order to define quality improvement for the purposes of the P4P incentives in VBP QIP. Facilities and paired MCOs are required to:
- Agree to the methodology for reporting Quarterly Improvement Targets (QITs) and Annual Improvement Targets (AITs);
- Agree to the methodology for calculating, reviewing and approving the results for each measure in each reporting period (MCO is the final authority as to whether or not a measure has been met).
Calculating Quarterly Improvement
Improvement for each P4P quality measure will be assessed every DY quarter starting in DY3 Q4. The most recently completed DY quarter´s rolling annual results will be compared with the immediately preceding7 DY quarter´s rolling annual results for each quality measure. Quarterly Improvement will be considered achieved for a given P4P quality measure if the most recently completed quarter´s annual rolling results indicate maintaining or improving the level of quality over the preceding quarter´s annual rolling results regardless of the magnitude of improvement.
For example, if the DY3 Q4 result for a quality measure remained constant over the baseline established in DY3 Q3, Quarterly Improvement is considered achieved. Similarly, if DY4 Q1 results are improved over DY3 Q4, Quarterly Improvement is also considered achieved for DY4 Q1. Figure 4 (below) is a chart that highlights the P4P payment period and its corresponding performance/measurement period.
Figure 4: Measurement Period gets Paid Out in Corresponding Performance Period
| P4P Payment Date | P4P Measurement Period | Rolling Annual Performance Measurement Timeframe | Rolling Annual Baseline Timeframe |
|---|---|---|---|
| DY3 Q3 | DY2 Q4* | April 2016 – March 2017 | *N/A – payment is tied to reporting baseline for DY3 Q1. |
| DY3 Q4 | DY3 Q1 | July 2016 – June 2017 | April 2016 – March 2017 |
| DY4 Q1 | DY3 Q2 | October 2016 – September 2017 | July 2016 – June 2017 |
| DY4 Q2 | DY3 Q3 | January 2017 – December 2017 | October 2016 – September 2017 |
| DY4 Q3 | DY3 Q4 | April 2017 – March 2018 | January 2017 – December 2017 |
| DY4 Q4 | DY4 Q1 | July 2017 – June 2018 | April 2017 – March 2018 |
| DY5 Q1 | DY4 Q2 | October 2017 – September 2018 | July 2017 – June 2018 |
| DY5 Q2 | DY4 Q3 | January 2018 – December 2018 | October 2017 – September 2018 |
| DY5 Q3 | DY4 Q4 | April 2018 – March 2019 | January 2018 – December 2018 |
| DY5 Q4 | DY5 Q1 | July 2018 – June 2019 | April 2018 – March 2019 |
Quarterly P4P Payments (Starting DY3 Q3 – DY5 Q4)
Reporting on performance of P4P quality measures is a critical part of VBP QIP starting in DY3. Quarterly award dollars based on performance of quality measures will start flowing P4P in DY3 Q3
VBP QIP partners should keep in mind that although performance is measured on a quarterly basis, VBP QIP payments are still expected to be paid out on a monthly basis. See Figure 5a below for a visual representation of the VBP QIP P4P performance, reporting and payment timeline.
Figure 5a: P4P – QIT Timeline
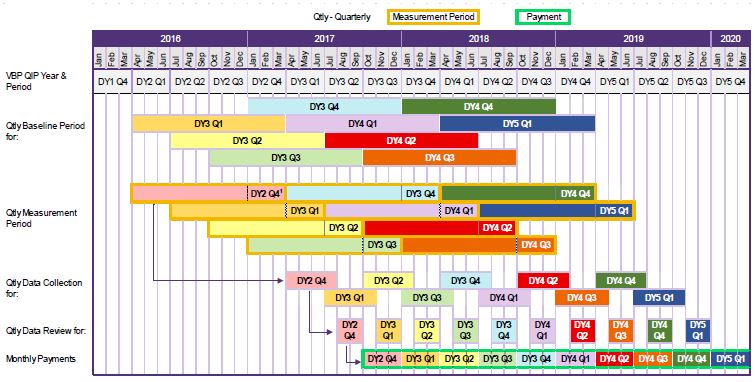
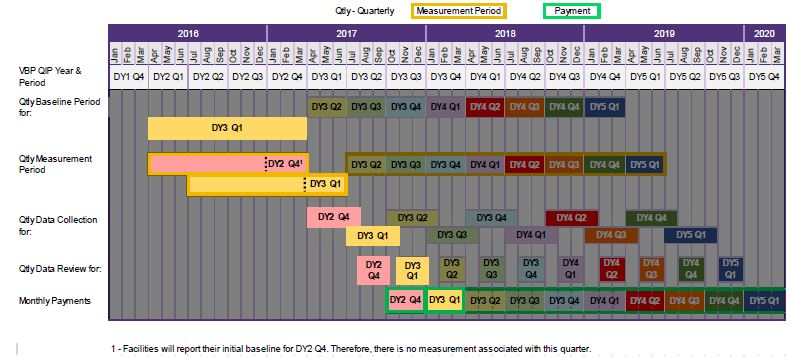
Figure 5b below illustrates an example of the QIT timeline.
- VBP QIP Year and Period – illustrates the period in the program and shows when the actual performance achieved will be paid out. For example, performance achieved in DY3 Q3 will be paid out monthly in DY4 Q2.
- Qtly Baseline Period – displays the baseline period as the prior quarter’s rolling annual calculation. The rolling annual in DY3 Q3 will be measured against its baseline, the rolling annual calculation in DY3 Q2, including the three months of DY3 Q2 + the nine preceding months (April 2016 – March 2017).
- Qtly Measurement Period – shows the measurement period included in the quarter’s rolling annual calculation. In this example, the rolling annual for DY3 Q1 includes the three months of DY3 Q1 + the nine preceding months (October 2016 – September 2017).
- Qtly Data Collection – demonstrates the 120–day window the facility has to collect and report P4P measure data to their paired MCO.
- Qtly Data Review – includes the 60 days MCOs have to review the facility submitted reports and prepare payments.
- Monthly Payments – shows when payments for P4P performance achieved in that quarter should get distributed.
Figure 5b: P4P – QIT Quarterly Example
Quarterly Percentage of P4P Payment by Number of Measures Achieving Maintenance or Improvement
Quarterly P4P payments to facilities will be based on the number of P4P quality measures the facility either maintained or improved on compared to the preceding quarter´s annual rolling results. A facility will receive 100% of its quarterly P4P award if at least four of its six P4P quality measures have either maintained or improvement over the rolling annual results from the preceding quarter. The P4P award amounts for a quarter will be reduced by 25% for each P4P quality measure that did not maintain or improvement over the rolling annual results from preceding quarter below 4 measures, as shown in Figure 6 below.
Figure 6: Quarterly Percentage of P4P Payment by Number of Measures Achieving Improvement
| Measures Achieved | 4+ | 3 | 2 | 1 | 0 |
|---|---|---|---|---|---|
| Percentage of Quarterly P4P Awarded Earned | 100% | 75% | 50% | 25% | 0% |
Annual Improvement Target (AIT) [DY 4 & DY5 Only]
A facility meeting its AIT at the end of DY4 and DY5, will be provided the opportunity earn any remaining quarterly P4P award dollars the facility did not already earn for achieving quarterly improvement during the DY. Through achievement of the AIT, a facility can earn up to the full amount of VBP QIP P4P DY allocation that the State designated for the facility. Unearned P4R funds cannot be earned back through achieving AITs.5
For DY4 & DY58, an AIT will be calculated by the facility and reviewed by its paired MCO to confirm improvement over the course of a four–quarter "measurement period" compared to a "baseline period." DOH recognizes that due to updating process flows to achieve better performance, facilities may see temporary declines in performance metrics, potentially leading to missed quarterly achievement on a P4P quality measure. Facilities will have an opportunity to earn P4P dollars in DY4 and DY5 that may have been missed in quarterly performance periods due to these short–term variations in performance by calculating an AIT and reviewing its paired MCO to confirm improvement over the course of a four–quarter measurement period.
For alternate measures, the facility is responsible for the calculation. The facility must use NYS data for comparison in the second requirement of each DY. If this data is not available, the facility can use a national average for the measure. The facility must use the most recent published reports at May 1, 2017 for DY4 and May 1, 2018 for DY5. The MCO is responsible for confirming the sources for alternate measures.
If a facility meets four (4) of their six (6) measures for the AIT, the facility is entitled to the full potential annual P4P award at the end of the DY. (Any payments previously withheld by not achieving QIT will be awarded to the facility). If a facility fails to meet four (4) of their six (6) measure for AIT, the potential annual P4P award will be reduced by 25% for each measure missed below four (4) measures. Figure 8b below, shows the percentage of potential annual P4P award earned based on the number of AIT achieved.
An AIT will be considered achieved for a specific measure as follows:
For Payment in DY4:
- If the DY4 Annual Measurement Period result is better than the DY4 Annual Baseline Period result (performance improves over the baseline); AND
- If the facility achieves results for the DY4 Annual Measurement Period that are better than the mean NYS results for the specific measure as per the most recently published report by the designated data source (NYSDOH, CMS, AHRQ, NHSN, NQF, etc.).
For Payment in DY5:
- If the DY5 Annual Measurement Period result is better than the DY5 Annual Baseline Period result (performance improves over the baseline); AND
- If a facility achieves a result for the DY5 Annual Measurement Period that is better than the mean NYS results for the specific measure as per the most recently published report by the designated data source (NYSDOH, CMS, AHRQ, NHSN, NQF, etc.).
For the second requirement for AIT payment in each DY, the facility is required to compare its results to the mean of the NYS results for the specific measure. Figure 7 below outlines the 13 P4P measures and includes the units and data source of the NYS results. OQPS and GNYHA will provide the data for comparison for the measures below. The mean included in the table below is the most recent published data for the measures for illustrative purposes only. OQPS will release the NYS mean results for DY4 in June 2017. Mean data will be pulled based on the most recent data available as of May 1, 2017.
Figure 7: P4P Measure Data Source and Units for AIT
| # | Measure Name | Data Steward | Focus Area/Domain | Measure Definitions | Units | Data Source | Period | Rate, Mean (30+ or more Disch) for Illustration Only* |
|---|---|---|---|---|---|---|---|---|
| 1 | Acute MI Mortality (IQI #15) | AHRQ | Mortality | In–hospital deaths per 1,000 hospital discharges with acute myocardial infarction (AMI) as a principal diagnosis for patients ages 18 years and older. Excludes obstetric discharges and transfers to another hospital. | Rate per 1000 Discharges | NYSDOH (SPARCS) | 2014 | 84.26 |
| 2 | Stroke Mortality (IQI #17) | AHRQ | Mortality | In–hospital deaths per 1,000 hospital discharges with acute stroke as a principal diagnosis for patients ages 18 years and older. Includes metrics for discharges grouped by type of stroke. Excludes obstetric discharges and transfers to another hospital. | Rate per 1000 Discharges | NYSDOH (SPARCS) | 2014 | 90.3 |
| 3 | Pneumonia Mortality (IQI #20) | AHRQ | Mortality | In–hospital deaths per 1,000 hospital discharges with pneumonia as a principal diagnosis for patients 18 years and older. | Rate per 1000 Discharges | NYSDOH (SPARCS) | 2014 | 40.19 |
| 4 | CAUTI Rate per 10,000 Patient Days (Population Rate) or 1,000 Device Days | NHSN | Hospital Acquired Conditions | Catheter–associated urinary tract infections (CAUTI) | CAUTI Rate per 10,000 Patient Days or 1,000 Device Days | GNYHA / CMS | 2015 | 12.77 |
| 5 | CLABSI per 10,000 Patient Days (Population Rate) | NHSN | Hospital Acquired Conditions | Central line–associated bloodstream infections (CLABSI) | CLABSI Rate per 10,000 Patient Days or 1,000 Device Days | GNYHA / CMS | 2015 | 9.93 |
| 6 | CDI Healthcare Facility – Onset Incidence Rate per 10,000 Patient Days | NHSN | Hospital Acquired Conditions | Clostridium difficile (C diff) Laboratory–identified Events | CDI Rate per 10,000 Patient Days | CMS | 2015 | 5.99 |
| 7 | Falls with Injury | NDNQI | Hospital Acquired Conditions | Acute Patient Fall Rate | Falls per 1,000 Patient Days | GNYHA / CMS | 2013 | 0.52 |
| 8 | 3–Hour Sepsis Bundle | NYSDOH | Hospital Acquired Conditions | The percentage of adult patients with sepsis treated in the emergency room with the hospital´s sepsis protocol who received all the recommended early treatments in the 3–hour early management bundle within three (3) hours of their arrival | Percent Compliance | NYSDOH | TBD** | |
| 9 | Pressure Ulcer Rate, Stage 2 or higher | NQF | Hospital Acquired Conditions | Stage III or IV pressure ulcers or unstageable (secondary diagnosis) per 1,000 discharges among surgical or medical patients ages 18 years and older | Rate per 1,000 discharges among surgical or medical patients ages 18 years and older | GNYHA / NYSDOH (SPARCS), PSI #03 | 2014 | 0.73 |
| 10 | Episiotomy Rate | Pediatric Measurement Center of Excellence | Maternity | Patients who underwent an episiotomy | Per 100 Vaginal Deliveries | NYSDOH | 2014 | 15.87 |
| 11 | Primary C– Section (IQI #33) | AHRQ | Maternity | First–time Cesarean deliveries without a hysterotomy procedure per 1,000 deliveries. Excludes deliveries with complications (abnormal presentation, preterm delivery, fetal death, multiple gestation diagnoses, or breech procedure). | Rate per 1000 Deliveries | NYSDOH (SPARCS) | 2014 | 189.1 |
| 12 | Avoidable ED Use | 3M | Utilization | Potentially Avoidable ED Use | Rate per 100 Discharges | NYSDOH (SPARCS) | 2014 | 72.23 |
| 13 | Avoidable Admissions | 3M | Utilization | Potentially Avoidable Admissions | Rate per 100 Admissions | NYSDOH (SPARCS) | 2014 | 23.97 |
| 13 | Fibrinolytic Therapy Received with 30 minutes of ED Arrival (OP–2) | CMS | Timely and Effective Care | Outpatients with Chest Pain or Possible Heart Attack Who Got Drugs to Break Up Blood Clots Within 30 Minutes of Arrival (OP–2) | Percent Compliance | CMS | 2016 | 78 |
| 14 | Median Time to Transfer to Another Facility for Acute Coronary Intervention (OP–3) | CMS | Timely and Effective Care | Average (median) number of minutes before outpatients with chest pain or possible heart attack who needed specialized care were transferred to another hospital | Minutes | CMS | 2016 | 71.88 |
| 15 | Median Time to ECG (OP–5) | CMS | Timely and Effective Care | Average (median) number of minutes before outpatients with chest pain or possible heart attack got an ECG | Minutes | CMS | 2016 | 10.2 |
| 17 | EDTC Emergency Department Transfer Communication (All or None) | NQF/ Stratis Health | Transitions of Care | Patients who are transferred from an ED to another healthcare facility have all necessary communication with the receiving facility within 60 minutes of discharge | Rate per 100 transfers | Stroudwater | .78 |
*This column´s data is for illustration purposes only. Updated SPARCS and CMS data will be available and used to establish the mean NYS result (applicable to the DY4 AIT payment) by June 30, 2017 – before the start of the DY4 Measurement Period.
**This benchmark is currently unavailable and data will be released in the near future.
Facilities that elected to use means provided by GNYHA must commit to using the specific measure definition for the duration of the program.
As seen in Figure 8a below, facilities will work with their paired-MCO to establish AIT baselines before the start of the AIT performance period, so the facility can be aware of how their performance compares to the statewide mean.
Figure 8a: AIT Timeline
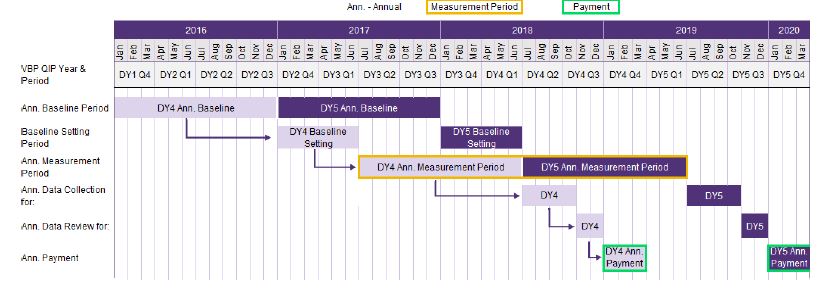
Figure 8b: Annual Award Dollar Percentage by P4P Quality Measures Achievement
| Measures Achieved | 4+ | 3 | 2 | 1 | 0 |
|---|---|---|---|---|---|
| Percentage of Potential Annual P4P Award Earned | 100% | 75% | 50% | 25% | 0% |
As show in in the calculation below, the payout for the annual award will be equal to the potential Annual P4P Award less the total dollars earned through quarterly payments throughout the DY.13
Annual Award Payout Calculation:
Annual P4P Award Payout = Potential Annual P4P Award – Total DY Quality Achievement Payments
|top of section| |top of page|P4R Requirements
Starting in DY3, the P4R requirements for VBP QIP will shift to promote a focus on VBP Contracting. Since the adoption of VBP is an essential component of VBP QIP, the P4R portion of VBP QIP funds for DY3 through DY5 will be earned through facilities reporting to their VBP QIP paired MCO on their achievement of VBP contracting milestones14. In DY4, VBP QIP facilities are expected to update current or have entered into new Medicaid MCO contracts where at least 80% of total Medicaid MCO contracted payments15 to the facility are tied to at least Level 1 value-based purchasing components by June 29, 2018. P4R dollars account for 20% of the DY4 funds a facility can potentially earn and these dollars are tied to the completion of this VBP Contracting milestone.
In order to enter into a qualified VBP contract, a VBP QIP facility may decide to enter into a VBP contract on its own or create or join qualified VBP contracting entities. While the roadmap provides guidelines for attribution used on PCP connections for a consortium of providers coming together, entities are able to work with their MCO VBP contracting partner to create attribution models that will work for individual providers (like hospitals).
The facility will be required to maintain at least 80% of total Medicaid MCO contracted payments in at least a Level 1 VBP contract In DY5. See Figure 9 (below) for a summary of P4R requirements.
Figure 9: P4R Payment Requirements
| DY | P4R Deliverables |
|---|---|
| 3 9 | DY3 Q1 Payment: By April 1, 2017, a VBP QIP facility must provide the following:
|
DY3 Q2 Payment: By July 1, 2017, a VBP QIP facility must provide the following:
|
|
| 4 |
|
| 5 | Facility must comply with DY4 P4R requirement and maintain 80% MMC dollars in VBP arrangements through DY5. |
Inability to meet these deadlines or on the contrary, exceeding them, may result in either incurring financial penalties or achieving measure credits, all described in the section below.
|top of section| |top of page|P4R Service Exclusion Waiver
DOH understands that facilities may not be able to reach the DY4 P4R milestone for reasons that are outside of their ability to control. As a result, DOH created an alternative VBP P4R calculation which will determine a facility’s progress towards the 80# threshold for only Inpatient and Emergency Department Medicaid Managed Care dollars.
In order to qualify for this alternative calculation, facilities will need to complete an application for this Service Exclusion Waiver. The application is available here as well as on the VBP QIP website. Facilities that choose to apply for the Service Exclusion Waiver will need to:
- Identify and explain the reason for requesting the waiver;
- Identify all facilities or organizations with whom they have attempted to partner or will attempt to partner; and
- Detail the value of all existing Medicaid Managed Care contracts as well as the value of all Inpatient and Emergency Department services.
Applications are to be sent to the VBP QIP inbox at vbp_qip@health.ny.gov and will be accepted through June 27, 2018. If a facility is approved, it is possible that DOH may require additional reporting by the facility in order to monitor progress towards VBP, ensure sufficient dollars are captured in these VBP arrangements, or determine the level of effort the facility has taken to partner with other local healthcare providers.
|top of section| |top of page|P4R Roles
PPS Roles in VBP Contracting
While PPS themselves are not qualified VBP contractors, these entities can be a valuable resource to VBP QIP facilities in their VBP contracting efforts. There are many PPS entities that are working to become qualified VBP contractors by forming state recognized contracting entities like Accountable Care Organizations (ACOs) or Independent Practice Associations (IPAs). VBP QIP facilities can join these IPAs or ACOs to meet the facility´s VBP QIP P4R contracting milestones. These entities will need hospitals in their networks and VBP QIP facilities, through their work on quality measures, can be attractive partners as they can help the entity yield significant performance gains. Additionally, many PPS have resources knowledgeable about contracts, measures and partnerships who can assist facility leadership serving as a "match maker" and "dating tutor" to facilities looking for partners.
MCOs Roles in VBP Contracting
The State has incentivized MCOs to come to the table and work on VBP contracts with providers throughout the state. Beginning in State Fiscal Year (SFY) 2017 (April 1, 2016 – March 31, 2017), the State allocated $85 million in stimulus funding as a down payment for MCOs to enter into VBP contracts (at any level). MCOs may use these dollars to further incentivize providers to move into VBP contracts. This "guaranteed" stimulus funding will only be available for SFYs 2017 and 2018 and beginning [SFY19 (April 1, 2018–March 31, 2019)] the "guaranteed" stimulus dollars will be used to fund MCO premium stimulus adjustments directly tied to MCO level of VBP contracting.
Furthermore, not only are there opportunities for MCOs to earn stimulus funds, but starting in April 2018, MCOs will also face penalties for failing to meet certain dollar thresholds of total MCO expenditures in Level 1 VBP contracts. Hence, 2017 is an ideal time for VBP QIP facilities to work with MCOs to enter into VBP arrangements.
Note that although PPS and MCOs play an important role in VBP contracting for VBP QIP, it is ultimately the facility´s responsibility to enter into Level 1 VBP contracts per program requirements.
|top of section| |top of page|P4R Penalties and Measure Credits
Penalties
For Facilities that do not meet the specified VBP contracting expectations, DOH advises that VBP QIP pairings abide by the following penalties shown in Figure 10 & Figure 11:
Figure 10: P4R Payment Requirements with Potential Penalties
Each deliverable listed in each time period should be evaluated separately on a pass/fail basis. Hence, there is no partial credit for individual deliverables. For example, if a facility only provides a few of the remaining LOIs for the July 1, 2017 requirement, partial credit tied to that individual deliverable should not be awarded.
| DY | P4R Deliverables | % of Total P4R Payment in DY |
|---|---|---|
| 3 10 | DY3 Q1 Payment: By April 1, 2017, a VBP QIP facility must provide the following:
|
Penalty if Not Met: (Up to 50% of P4R Funds in DY3) (50%–100% DY3 Q1 Payment) DOH recommends that each deliverable is weighted equally (50%) for the DY3 Q1 payment. |
DY3 Q2 Payment: By July 1, 2017, a VBP QIP facility must provide the following:
|
Penalty if Not Met: (Up to 50% of P4R Funds in DY3) 33%–100% of DY3 Q2 Payment DOH recommends that each deliverable is weighted equally (33.34%) for the DY3 Q2 payment. *Note: MCO Contract List will not be accepted in this quarter without a signed attestation. |
|
| 4 | DY4 Payments: By July 1, 2018, a VBP QIP facility must provide the following:
|
Value Lost if Not Met: 100% of P4R Funds in DY4 |
| 5 | Facilities must comply with DY4 P4R requirement and maintain 80% Medicaid Managed Care dollars in VBP arrangements through DY5. | Penalty: 50% of P4P Funds in DY5 11 |
Figure 11: Penalties tied to missing P4R Deliverables
| VBP Contract | By Dy3 (April 1) |
By DY3 (July 1) |
By DY4 (April 1) |
By DY5 (April 1) |
|---|---|---|---|---|
| No LOI with at least 1 MCO | Penalty | – | – | – |
| No MCO Contract List (with signed attestation in July 2017) | Penalty | Penalty | – | – |
| No Level 1 VBP Contract with at least 1 MCO | – | Penalty | – | – |
| No LOIs with Remaining VBP Contracting MCOs | – | Penalty | – | – |
| VBP arrangements are not present in components that drive at least 80% of dollars for the facility´s Medicaid MCO contracts | – | – | Penalty | Penalty |
| VBP arrangements are not present in components that drive at least 80% of dollars for the facility´s Medicaid MCO contracts through Dy5 | – | – | – | Penalty |
Moreover, please remember that unearned P4R funds due to penalties for not meeting VBP contracting deliverables cannot be made–up through performance on the facility´s AIT. AIT awards only apply to unearned P4P funds.
Finally, VBP QIP facilities should thoroughly document their efforts to enter into VBP contracts. While there are incentives to bring VBP partners to the table, the facility´s VBP QIP paired–MCO and the State understand that there may be situations where, even with significant effort, a facility may not be able to get a partner to contract in a timely fashion. In such a special case, the VBP QIP paired MCO may choose to award a percentage of the P4R dollars for that period based on effort. Again, the burden is on facilities to document its efforts, including notifying their paired MCO and the state of contracting difficulties with sufficient time in advance of a reporting deadline. MCOs have the final authority to make determinations but can seek guidance from the state should such situations like the one described above arise.
Additionally, the paired MCO may distribute funds to the facility for P4R deliverables upon the submission. However, DOH reserves the right to validate the LOIs, MCO listings, and VBP contracts and may recoup P4R funds if the submissions do not align with program requirements.
Measure credits
Starting in DY3, facilities that complete certain VBP contracting milestones earlier than expected will be granted measure credits for their efforts. Measure credits can be used by a facility to meet performance targets for VBP QIP P4P quality measures. If a facility earns a measure credit, the credit will be applied to both the calculation of VBP QIP quarterly and annual12 measure achievement by adding an additional achieved measure to the numerator of each calculation, while keeping the denominator constant.
All credits start in the quarter the qualification is met and measure credits can only be applied to calculations in the year earned and cannot be carried over into future demonstration years. As the administrator of the program, it will be the responsibility of the MCO to keep track of a facility´s measure credit eligibility, but facilities should include measure credit eligibility in their calculation of QIT and AIT through reports submitted to MCOs. A facility cannot earn more than one (1) measure credit in a given reporting period.
The facility earns a quarterly measure credit in the current quarter the requirement is met and the three subsequent quarters. In the example below in Figure 12a, the facility executed a Level 2 VBP contract on August 15, 2017. Therefore, it would receive a measure credit in the current quarter, DY3 Q2, and the three subsequent quarters, DY3 Q3 to DY4 Q1. If the Level 2 VBP contract extends through later years, the Facility is required to re–certify that a contract is in place to earn a measure credit the next year.
Figure 12a: Measure Credits for QITs Example
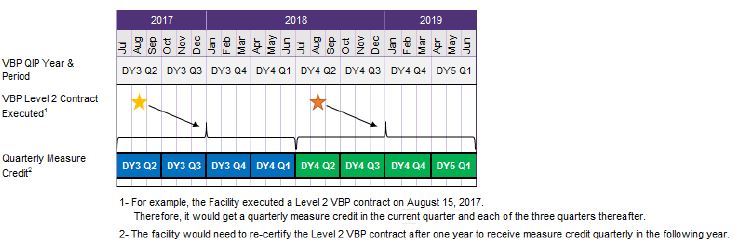
If during the first quarter, the facility initially achieved performance on four out of the six measures, the measure credit would be added as one more achieved measure to the final calculation making the total measure achievement for that quarterly reporting period: five out of six measures achieved (100% of quarterly performance funds earned). While in this first quarter, the measure credit did not have an impact, it is possible that a facility improves its quality, it may become increasingly difficult for the facility to maintain or increase performance on these measures on a quarterly basis. If by the fourth quarter of that year the facility only initially achieves performance on three out of six measures, when applying the measure credit in the calculation, the PPS will then meet its quarterly performance target and earn the full performance award for that quarter.
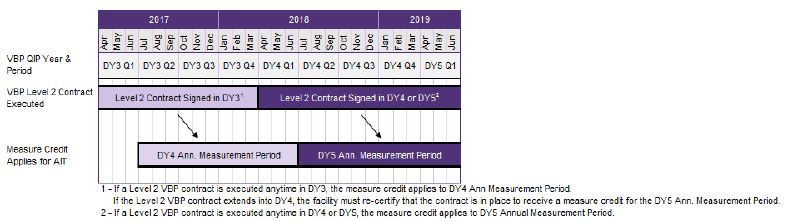
If a facility has unawarded P4P funds during the DY for not meeting its full QITs, it has the opportunity to earn these funds by meeting its AIT. As illustrated below in Figure 12b, if a facility has an executed Level 2 VBP contract during DY3, it can earn an additional measure credit applied to the DY4 AIT measures. If the facility has an executed Level 2 VBP contract in DY4 or DY5, it can earn an additional measure credit applied to the DY5 AIT measures. If the Level 2 VBP contract is executed in DY3 and extends through later years, the Facility is required to re–certify that a contract is in place to earn a measure credit for its DY5 AIT.
Figure 12b: Measure Credits for AITs
The State advises that VBP QIP pairings abide by the following measure credits qualifications in situations where facilities exceed specified VBP contracting expectations:For DY3, DY4 & DY5:
- Facilities that are part of at least one Level 2 or higher qualified VBP contract
Figure 12c: Measure Credits
| VBP Contract | By DY3 | By DY4 | By DY5 |
|---|---|---|---|
| Level 2 or Higher qualified VBP Contract | Measure Credit | Measure Credit | Measure Credit |
VBP QIP Facility Plan Schedule & Key DY3 Goals
Figure 13: Updated Program Schedule
| Date | Milestone* |
|---|---|
| March 31, 2017 | Updated Facility Transformation Plans are due for both Group 1 and 2. |
| April 1, 2017 | Letters of Intent (LOI) and MCO Contract List |
| July 1, 2017 | At least 1 Contract Attestation of a Level 1 VBP contract, outstanding LOIs for Medicaid MCOs to contract by April 1, 2018, and updated MCO Contract List with signed attestation. |
| June 1, 2018 | VBP QIP Facility must have Medicaid MCO contracts where at least 80% of total Medicaid MCO contracted payments (based on CY2016 data) to the facility are tied to Level 1 value–based purchasing components. |
* Please note: inability to achieve the milestones will result in penalties to the facility.
|top of section| |top of page|Appendix A: Deliverable Submission Table
| Report | Submitted by | Submitted to | Frequency | Location |
|---|---|---|---|---|
| VBP QIP Contracts | MCOs | DOH | As updated | vbp_qip@health.ny.gov |
| Approved Facility Plans | MCOs | DOH | March 31, 2017 | vbp_qip@health.ny.gov |
| 1 LOI or Contract Attestation | Facilities | MCOs & DOH | April 1, 2017 | vbp_qip@health.ny.gov |
| MCO Contract List with 2015 data | Facilities | DOH | April 1, 2017 | vbp_qip@health.ny.gov |
| 1 Contract Attestation for Level 1 VBP | Facilities | MCOs | July 1, 2017 | |
| Remaining LOIs (or Contract Attestations) | Facilities | MCOs & DOH | July 1, 2017 | vbp_qip@health.ny.gov |
| MCO Contract List with 2016 data and Facility Attestation | Facilities | DOH | July 1, 2017 | vbp_qip@health.ny.gov |
| Remaining Contract Attestations | Facilities | MCOs & DOH | April 1, 2018 | vbp_qip@health.ny.gov |
| Documentation of achievement of P4P metrics | Facilities | MCOs | Quarterly | |
| Documentation of approval of P4P deliverables and supporting documentation | MCOs | DOH | Quarterly | vbp_qip@health.ny.gov |
___________________________________________
1. To be clear, the P4P payment in DY3 Q3 is made for a facility reporting baselines on all six VBP QIP quality measures the facility has chosen. DY3 Q4 is the first quarter where payment is driven by the facility´s ability to maintain or improve performance on the quality measures. 1
2. All–Payer measures are recommended over Hospital/MCO specific measures or Medicaid only populations because there would be the possibility of running into "small cell size/denominator" issues. 2
3. Spelling of abbreviations: NQF: National Quality Forum; NCQA: National Committee for Quality Assurance; AHRQ: Agency for Healthcare Research and Quality; CMS: Centers for Medicare & Medicaid Services; CDC: Centers for Disease Control and Prevention. 3
4. 3M (SPARCS) Measures: Facilities looking to select measure #12 or #13 should confirm that they have the mechanisms/partnerships in place to report out on this data to MCOs within 120 days following the end of the performance period. Facilities may face challenges reporting out on SPARCS data in a timely fashion, because either the facility will need to have a 3M software license and knowledge on how to appropriately use the software or have an outside organization do the performance calculations and report back on performance to the facility before the quarterly report is due to the facility's VBP QIP paired MCO. 4
5. To be clear, the AIT only applies to unearned P4P funds and does not apply to unearned P4R funds due to penalties for not meeting VBP contracting deliverables. 5
6. A facility´s VBP QIP paired MCO as well as any other governing authority has the right to seek additional information to validate results submitted by the facility. If there is a situation where proprietary information to the facility is in question, the facility´s VBP QIP paired MCO may bring those concerns to the State for further review. 6
7. Baseline metrics reflect a facility´s actual experience for that measure in the previous quarter (using a rolling annual) or previous year (in the case of AIT). Baselines will be reported by the facility, not the State or Independent Assessor. 7
8. An AIT will not be paid in DY3 because there is only one quarter where payment is based on actual performance (DY3 Q4). Payment in DY3 Q3 is based on reporting on quality measures that will be used as a baseline. 8
9. See the P4R Penalties and Measure Credits for information on deliverable weightings 9
10. In DY3 Q1 the P4R deliverables have two components and each component is worth 50% of the payment for that quarter. In DY3 Q2 the P4R deliverables have three components and each component is worth approximately 33.33%. 10
11. Funds forfeited by VBP QIP facility due to the DY5 penalty for not having VBP Contracts in place by April 1, 2019 cannot be earned back through meeting AITs. 11
12. Measure credit for AITs are only applicable in DY4 & DY5. 12
13. If the total DY Quarterly Achievement Payments equal the Potential Annual P4P Award in a given DY, the AIT Award payout at the end of the DY will be zero. A facility cannot earn more than its expect VBP QIP annual award valuation that is tied to P4P. 13
14. Please note that in the VBP arrangements, the facilities´ performance will also be evaluated based on the VBP arrangement quality measures developed by the Clinical Advisory Groups and reviewed and approved by the DOH. 14
15. Due to the nature of services offered by VBP QIP facilities (hospitals), we are expecting most of these contracts to be mainstream (including HARPs) contracts. However, the type of MCO contract is not as important as the total amount of dollars, in aggregate, the facility has tied to VBP arrangements with its Medicaid MCOs. 15
Follow Us