MLTC VBP Financing Webinar
- Webinar is also available in Portable Document Format (PDF)
December 15, 2017
Agenda Items
- MLTC VBP Overview
- MLTC Stimulus and Penalty Incentive
- MLTC VBP Quality Payments
- MLTC VBP Timeline
- FAQ
MLTC VBP Overview
MLTC Partial Cap Plans and VBP
| Level 1 VBP: An MLTC Level 1 VBP Arrangement is a performance bonus agreement between an MLTC plan and a provider that is based on meeting performance targets for a set of specific quality measures agreed to in a VBP contract between an MLTC Plan and a provider or group of providers (the "VBP Contractor"). Such agreement must include the Potentially Avoidable Hospitalization (PAH) measure as required by the VBP Roadmap. |
| Level 2 VBP: MLTC VBP Level 2 is still being defined in the CAGs but will likely include components of pulling in Medicare data and incorporate "upside bonuses" and "downside penalties". |
Summary of VBP Additions
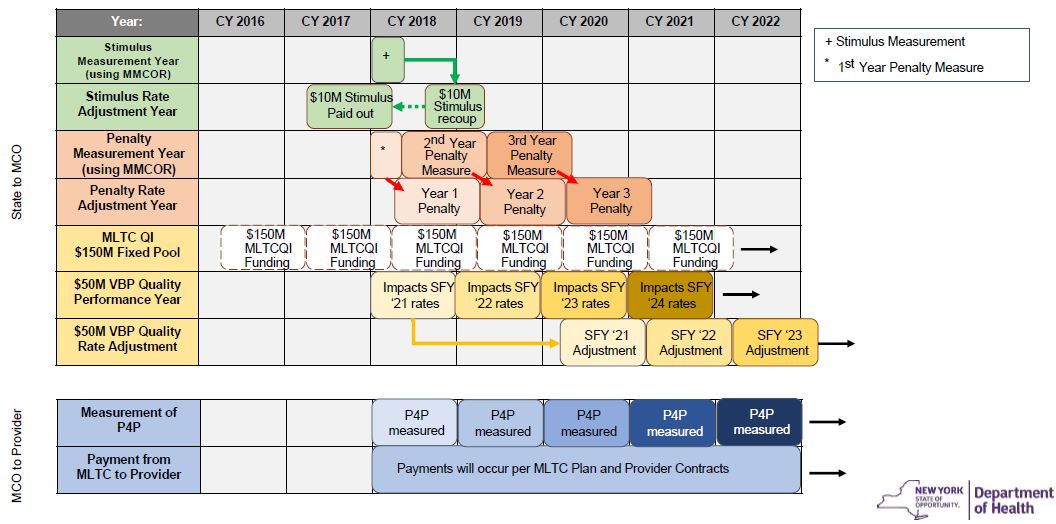
- MLTC Stimulus Incentive: (SFY2017–18) To incentivize and to assist the transition into VBP, MLTC plans and providers will receive a portion of the $10M stimulus adjustment conditional on contracting VBP level 1.
- MLTC Penalty Incentive: (SFY2018–19) To incentivize MLTC plans and providers into contracting VBP level 1.
- MLTC VBP Quality Payments: (SFY2020–21) $50M will be made available for plans to earn for MLTC VBP Quality. The primary measures will be Quality and Efficiency from the MLTCQI.
MLTC Stimulus and Penalty Incentive
MLTC Stimulus and Penalty Funding
- The State is aiming to move all MLTC contracts to a minimum of VBP Level 1.
- This will require plans to contract with providers using a pay for performance model using PAH.
- It is currently mandated that MLTC plans move all LHCSA, CHHA and SNF contracts to MLTC Level 1 VBP arrangements.
- As a part of the transition to VBP:
- The State is committing $10M to help MLTC partial caps plans and providers comply with new contracting requirements and investments in alignment into VBP.
- The stimulus will require 100% VBP contracting to earn the full stimulus.
- The State will implement the MLTC contracting penalties similar to mainstream to help incentivize plans and providers into VBP Level 1.
- The penalty will require different percentages of VBP contracting to avoid the penalty. The requirements range from 10% in Level 1 in year 1 to 80% in Level 1 and 15% in Level 2 in year 3.
- The State is committing $10M to help MLTC partial caps plans and providers comply with new contracting requirements and investments in alignment into VBP.
VBP MLTC Contracting Stimulus Funding
- $10 Million of new stimulus funding to incentivize and support MLTC plans and providers into VBP contracts. Funding will be paid in the April 2017 rates.
- The stimulus adjustment available for MLTC plans including Partial Caps is &38211; LHCSA, CHHA, and SNF.
- The percentage of dollars not in VBP would have that portion of the stimulus funding recouped. The recoupment is based on VBP Survey
VBP MLTC Contracting Penalty
- MCO is measured based on expenditure per VBP level compared to the total expenditure by an MCO.
- Penalties are levied on the difference between the required threshold an MCO must reach and the MCO´s contracted amount.
- For Level 1, MLTC plans will only be measured on contracting with LCHSA, CHHA, and SNF.

Penalty Adjustment: Example
- If in SFY ´19–20, an MCO has 45% in Level 1 or higher and 1% in Level 2 or higher, what percentage penalty will they pay?
Level 1 (50%) Level 2 (5%) MCO A 45% 1% - If in SFY ´19–20, an MCO has 45% in Level 1 or higher and 1% in Level 2 or higher, what percentage penalty will they pay?
Level 1 (50%) Level 2 (5%) MCO A 45% 1% Shortfall 5% 4% - The MCO will only pay the larger of the two penalties. Therefore, they will be penalized based upon the 5% shortfall from their Level 1 spending.
MLTC VBP Quality Payments
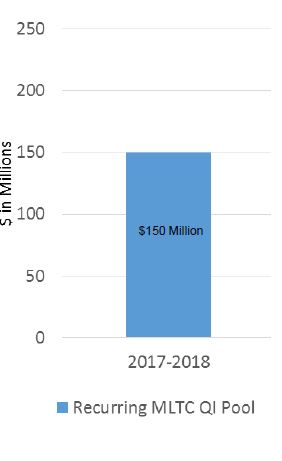
Current MLTC Quality Incentive Pool
- The MLTC QI Pool is a fixed pool of $150M. This portion of the pool will remain unchanged.
| Quality Measures (50 Points) | The allotted 50 points for quality are distributed evenly for all quality measures. The 2017 MLTC Quality Incentive includes 10 quality measures with each measure being worth a maximum of 5 points. |
| Satisfaction Measures (30 Points) | The 2017 MLTC Quality Incentive includes 6 satisfaction measures with each measure being worth a maximum of 5.0 points. |
| Compliance Measures (10 Points) | Compliance measures are based on the timely submission of required reports or assessment information. The compliance component consists of one measure from each of the following five areas: Medicaid Encounter Data System (MEDS), Medicaid Managed Care Operating Report (MMCOR), Ratio, Provider Network, and Community Health Assessments (CHA). Each measure is worth a maximum of 2 points. |
| Efficiency Measures (10 Points) | Potentially Avoidable Hospitalization (PAH) is a measure of efficiency. A PAH is an inpatient hospitalization that might have been avoided if proper outpatient care was received in a timely fashion. The hospitalization is identified as potentially avoidable if the primary diagnosis is any one of the following conditions: heart failure, respiratory infection, electrolyte imbalance, sepsis, anemia, or urinary tract infection. |
MLTC VBP Quality Funding
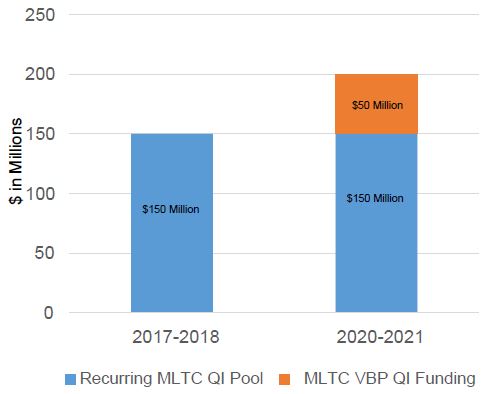
- The funding available for MLTC partial cap plans and providers is a fixed pool
- In the first year, the new $50M will be based on potentially avoidable hospitalizations (PAH).
Proposed $50M MLTC VBP Quality Weighting Efficiency Measures (100 Points) Quality Measures (0 Points) - The VBP quality funding ($50M) is intended to fund the CY2019 MLTC VBP pay–for–performance and accordingly should be primarily passed on to the providers.
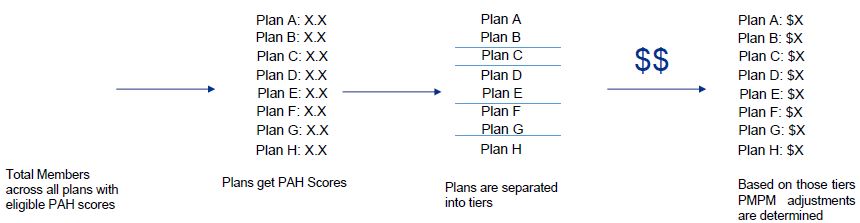
MLTC VBP Quality Funding Measurement
- All plans with eligible members (PAH scores available) are included in the measurement.
- Plans will be placed into tiers based on their PAH scores.
- The tiers will determine the PMPM adjustment a plan is to receive.
- The total pool of dollars will be $50M.
MLTC VBP Quality Funding
Maintenance of Existing Programmatic Requirements
- DOH will require that plans continue scoring in the current programmatic measures for the$150M MLTC QI.
Prospective VBP Quality Payments
- The new $50M fixed pool is moving to a prospective rate setting mechanism. This means that the adjustments will be built into the premium rather than a single lump sum payment at the end of the performance period.
Greater Weighting of VBP Measures
- In the first year, the $50M VBP funding will be based on potentially avoidable hospitalizations (PAH).
- Measures recommended by the MLTC Clinical Advisory Group (CAG) will receive greater weighting in future years.
MLTC VBP Timeline
MLTC VBP Timeline
MLTC VBP FAQs
Frequently Asked Questions
- What will be the start date of the MLTC VBP Quality Adjustments?
- The first MLTC VBP Quality Adjustment will be based on a base year of 2016, measurement year 2018, and payment year 2020–2021.
- How will the recoupment for the $10M MLTC stimulus be implemented?
- Each plan´s percentage of dollars not in VBP will be tracked via the VBP Survey, and that portion of a specific plans stimulus funding will be recouped. The recoupment is based on VBP Survey results that will be collected after the respective contracting deadline for each plan type.
- Are there additional provider types, other than SNFs, LHCSAs and CHHAs, that the 100% VBP Level 1 Contracting requirement applies to?
- The 100% VBP Level 1 contracting requirement only apples to these provider types. As plans progress into higher levels of VBP or generate more robust level 1 arrangements, other provider types may be included within arrangements to encourage greater care coordination.
- Will the state provide risk adjusted quality data to the plans in order for them to draw comparisons between providers in their networks?
- No, the State will not be able to provide risk adjusted quality data due the multitude of permutations of PAH.
- Are plans required to submit VBP contract amendments to DOH for review?
- Yes, plans will be required to submit VBP Contract amendments to DOH in accordance with the Provider Contracting Guidelines.
- Will DOH continue to provide PAH data on a provider-level basis?
- Yes, the State will continue to provide PAH data on a provider-level basis as it is currently done.
- What are the performance expectations for PAH from plan to downstream providers?
- It will be left to the contract negotiations of the plans and providers to determine the performance expectations and level of funding to be passed down.
- In order to meet the goal of 100% of VBP arrangements with these providers, can we contract directly with providers with a small population base if they do not enter into arrangements with larger providers?
- Small providers (with populations less than 30 members) can partner with one or multiple other small providers within a network.
- For example, a small LHCSA could partner with a group of other small LHCSAs in the same provider network. Within that network, one LHCSA (possibly the LHCSA with the largest membership) would need to be identified as the lead VBP contractor. DOH can calculate the aggregated PAH rate if a plan specifies which providers are included in the arrangement. This is particularly useful for lead agencies with fewer than 30 attributed members.
- On an ad hoc basis, the Department of Health can calculate PAH rates for plans that identify small sample size providers for aggregation.
- For example, if a plan has several nursing home facilities or LHCSA providers that fail to meet the sample size threshold, the plan can ask the DOH to aggregate the selected facilities. The DOH will provide an aggregate PAH rate for those small sample size facilities.
|top of section|
|top of page|
- Small providers (with populations less than 30 members) can partner with one or multiple other small providers within a network.
Follow Us