Integrated Primary Care Value Based Payment Arrangement
Measurement Year 2018 Fact Sheet
- Fact Sheet also available in Portable Document Format (PDF)
February 2018 NYS Medicaid Value Based Payment
Integrated Primary Care Value Based Payment Arrangement
This fact sheet has been prepared to assist payers and providers to more thoroughly understand New York State´s Medicaid Integrated Primary Care (IPC) Value Based Payment (VBP) Arrangement. It provides an overview of the Arrangement including a summary of the components of care, the underlying episodes of care, and the categories of measures recommended for use in IPC Arrangements.
Introduction
The IPC VBP Arrangement is designed to incentivize primary care providers (PCPs) to collaborate with behavioral health and other specialty medical and community–based providers to improve the quality of preventive care, care for chronic conditions and sick care for New York State (NYS) Medicaid members. Although the services included in an IPC Arrangement constitute a significant portion of the total costs, the risk in this Arrangement is limited to the provision of services that most PCPs would consider to be within their control (i.e. preventive care, and costs associated with sick care and the most prevalent chronic conditions in the NYS Medicaid population).
The IPC Arrangement provides the impetus for significant investment in integrated primary care and facilitates the movement toward the provision of advanced primary care in NYS. Savings in an IPC contract are primarily based on reductions of downstream costs: expenditures for sick care and chronic care from hospital utilization that would be reduced when integrated primary care is functioning optimally.
This fact sheet provides an overview of New York State´s IPC VBP Arrangement and is organized into two sections and an appendix:
- Section 1: Describes the types of care included in the IPC Arrangement and the method used to construct the episodes of care;
- Section 2: Describes the quality measure selection process and the categories of measures recommended for use in IPC Arrangements; and,
- The appendix contains a glossary of terms used in this document.
Section 1: Defining the IPC Arrangement Episodes of Care
The IPC Arrangement: Three Distinct Components of Care
In the IPC Arrangement, the Medicaid Managed Care Organization (MCO) contracts with a provider organization, such as an Independent Practice Association (IPA), which may include Patient Centered Medical Homes (PCMH), Advanced Primary Care (APC) practices, or other PCPs, for integrated primary care services. The IPC Arrangement includes three distinct components of care. Each component of the Arrangement consists of episodes of care, or groups of clinically related services delivered by physicians, other licensed practitioners, and ancillary providers across settings of care during a pre–defined period.
As illustrated in Figure 1, the IPC Arrangement consists of the following three components and underlying episodes:
- The Preventive Care Component consists of a single episode (the Preventive Care episode);
- The Chronic Condition Component consists of 14 unique chronic condition episodes, and;
- The Sick Care Component includes three episodes: the Upper Respiratory Infection Episode, the Allergic Rhinitis/Chronic Sinusitis Episode, and the Routine Sick Care Episode.
Together, the three components of the IPC Arrangement include 18 unique, underlying episodes of care that reflect a focused subset of the integrated primary care services delivered to attributed members during the contract year. (See Figure 1)
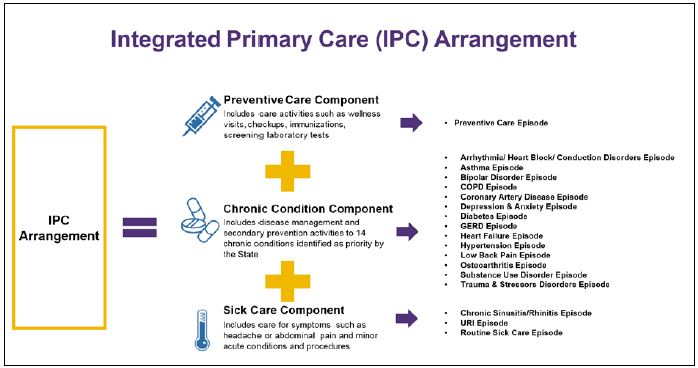
Figure 1: In the IPC model the Medicaid MCO contracts with a provider or group of providers for three components – Preventive Care, Care for priority Chronic Conditions, and Sick Care.
Constructing the IPC Arrangement Episodes of Care: Trigger Events, Time Windows, and Services
The episodes of care included in the IPC Arrangement are constructed using a set of rules, based on the PROMETHEUS Analytics system (the grouper). The grouper governs what "triggers" or signals the existence of an episode and includes the logic describing when the episode begins and ends (the time window), and the services to be included in the episode.
The first step to constructing the component episodes is to identify the potential trigger events that initiate the construction of the underlying episodes. The episodes within each component of the IPC Arrangement are uniquely defined with their own triggering criteria and time windows based on the nature of the episode (preventive care, chronic condition, acute medical care, procedure or surgical care, or inpatient and follow–up care for a condition caused by system related failures). System–related failures are those events that occur in the hospital that might have been prevented by better functioning systems, such as nosocomial infections or deep vein thromboses, for example.
The following section summarizes the criteria for the episodes of care within the 3 components of the IPC Arrangement, including the trigger events, time windows, and included service parameters for the episodes. A more detailed review of the episode construction rules, definitions, and trigger code sets is available on the PROMETHEUS Analytics website.1
The Underlying Episodes of the IPC Arrangement
Preventive Care Component
The Preventive Care Component of the IPC Arrangement consists of one episode, called the Preventive Care Episode, which specifically targets services oriented towards prevention.
Preventive Care Episode
- The Preventive Care Episode is initially triggered by a claim for an outpatient or professional office visit with a diagnosis code that is included in the Preventive Care Episode trigger code set.
- The Preventive Care Episode has a time window that is aligned with the contract year. Once triggered in the previous year, the Preventive Care Episode is designed to start at the beginning of the contract year (episode start), and includes all preventive care services delivered from the start of the contract year through the end of the contract year (episode end).
- All preventive care services delivered during the contract year are included in the episode, including well visits, age–appropriate physical exams, counseling, screenings, immunizations, and prevention–associated medications.
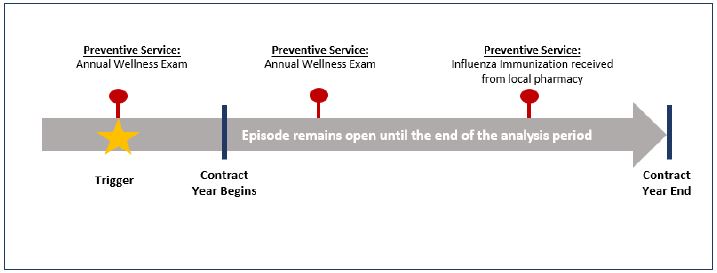
Figure 2: Preventive Care Episode example; The Preventive Care Episode is a single, unique episode spanning the course of the year and includes all preventive services delivered during that time. It is the only episode included in the Preventive Care component of the IPC Arrangement.
Chronic Condition Component
The Chronic Condition Component of the IPC Arrangement includes 14 unique episodes that focus on the care for chronic conditions identified by the State as priority chronic conditions with the highest prevalence and cost in the New York State Medicaid population. The 14 unique episodes are:
- Arrhythmia/ Heart Block/ Conduction Disorders Episode
- Asthma Episode
- Bipolar Disorder Episode
- Chronic Obstructive Pulmonary Disease Episode
- Coronary Artery Disease Episode
- Depression & Anxiety Episode
- Diabetes Episode
- Gastroesophageal Reflux Disease Episode
- Heart Failure Episode
- Hypertension Episode
- Low Back Pain Episode
- Osteoarthritis Episode
- Substance Use Disorder Episode
- Trauma & Stressors Disorder Episode
Each episode is defined based on the rules outlined below, along with the episode–specific code sets that can be found on the Altarum website.2 These 14 episodes are not mutually exclusive, and just as a member can have multiple co–morbidities, he/she can have multiple chronic condition episodes during the year.
Chronic Condition Episodes: 14 episodes based on the State–identified, priority, chronic conditions
- Chronic condition episodes included in the IPC Arrangement must meet the following requirements:
- The chronic condition episode has an initial triggering claim that occurs prior to the contract year, and, if required, a second confirming claim at least 30 days after the triggering claim. The confirmatory claim can occur at any time, including in the contract year. A diagnosis code for the condition must be included in each of the claims.
- The member receives services related to the chronic condition during the contract year as indicated through submission of at least one claim with a diagnosis for the chronic condition.
- Chronic condition episodes will include all services related to the chronic condition delivered during the contract year.
- Care specific to chronic conditions other than these 14 episodes, such as for Rheumatoid Arthritis, will not be included in this Chronic Condition Component. However, a member´s preventive care and sick care unrelated to Rheumatoid Arthritis will be included in the appropriate episode.
- Due to the requirement for an initial trigger occurring prior to the contract year, members newly diagnosed with one of the 14 chronic conditions will not have an episode during the year of the initial diagnosis for that condition.
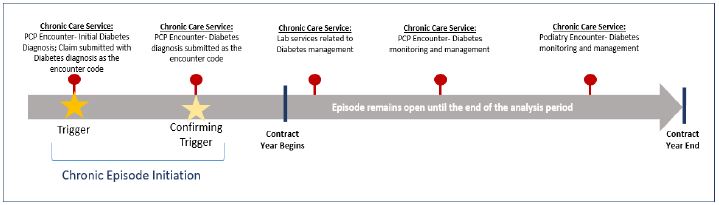
Figure 3: Chronic Care Episode example; Diabetes is one of the 14 priority chronic condition episodes in the Chronic Condition Component of the IPC Arrangement.
Sick Care3
The Sick Care Component of the IPC Arrangement includes the following three episodes:
- Allergic Rhinitis/Chronic Sinusitis Episode
- Upper Respiratory Infection Episode
- Routine Sick Care Episode
Allergic Rhinitis/Chronic Sinusitis Episode
- Consistent with the chronic condition episode logic previously described, the Allergic Rhinitis/Chronic Sinusitis Episode is triggered when both an initial triggering event occurs in a year prior to the contract year and the member receives care related to Allergic Rhinitis/Chronic Sinusitis during the contract year.
- The Episode includes all services delivered for the treatment of Allergic Rhinitis/Chronic Sinusitis during the contract year.
Upper Respiratory Infection Episode
- The Upper Respiratory Infection (URI) Episode is triggered by one or more claims that carry a relevant diagnosis code for acute Upper Respiratory Infection. Because URI is an acute medical episode, a trigger in the prior year is not required.
- The URI Episode is considered an acute medical episode with a time window limited to 21 days from the service date of the triggering claim. All services relating to treatment of the URI delivered during this 21–day period will be included in the episode.
- Note that a member can have multiple URI episodes during the contract year. After one URI episode time window ends, a new claim carrying the diagnosis codes for the acute diagnosis of URI will be considered a trigger event opening a second episode with a 21–day time window.
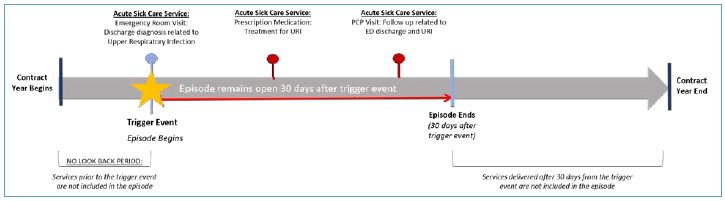
Figure 4: Upper Respiratory Infection Episode example; The Upper Respiratory Infection Episode is one of the episodes of care included in the Sick Care Component of the IPC Arrangement.
Routine Sick Care Episode
- The Routine Sick Care Episode is triggered by one of the following:
- An outpatient or professional office visit claim prior to the contract year with a diagnosis code included in the Routine Sick Care code set.4 Routine Sick Care trigger code examples include a: diagnosis related to pain, swelling, and/or redness of the eye and other eye inflammation diagnoses; nausea, vomiting, diarrhea, and abdominal pain or related diagnoses; joint pain, stiffness and swelling; and respiratory insufficiency, throat pain, or post–nasal drip.
- OR, a triggered URI or Allergic Rhinitis Episode prior to the contract year.
- The Routine Sick Care episode has a time window that is aligned with the contract year. Once triggered in the previous year, the routine sick care episode is designed to start at the beginning of the contract year (episode start), and includes all services delivered from the start of the contract year through the end of the contract year (episode end).
- The Routine Sick Care Episode will include all services directly related to a relevant diagnosis (inpatient, outpatient, ancillary, laboratory, radiology, pharmacy, and professional claims) delivered during the contract year.
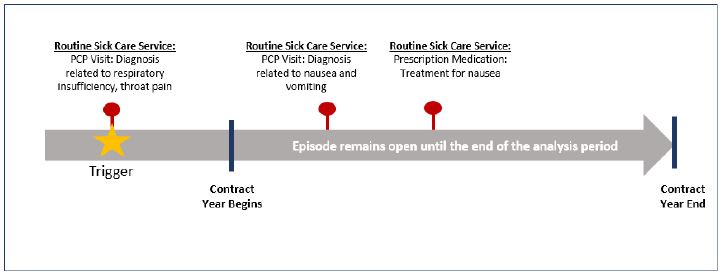
Figure 6: Routine Sick Care Episode example; The Routine Sick Care Episode is one of the episodes of care included in the Sick Care Component of the IPC Arrangement.
Member and Episode Eligibility
Medicaid MCO members are only included in the IPC Arrangement once they have triggered one of the episodes within the three components of care.
The IPC Arrangement only addresses a subset of services provided to members based on the services addressed through the three components of care. Accordingly, for each attributed member, only those services and associated costs captured by the episodes triggered will be included in the Arrangement. For example, a member who has an established diagnosis of Rheumatoid Arthritis (with no comorbid diagnoses identified) can be included in the Arrangement through the Preventive Care or Sick Care components of the Arrangement. In this example, only those services and costs associated with the Preventive Care and/or Sick Care component episodes triggered by the member will be included in the Arrangement. The services and associated costs provided to fully manage the member´s Rheumatoid Arthritis diagnosis will not be included in the Arrangement.
Additionally, episodes for members meeting the following criteria will be excluded:
- Medicaid members for whom Medicaid is not the sole payer: Medicaid members with contract year claims or encounters for which Medicaid is not the sole payer are excluded (e.g., dually eligible members and members with Medicaid as the payer of last resort on a commercial premium)
- Members eligible for inclusion under a VBP subpopulation arrangement: Members eligible for inclusion under the HIV/AIDS, Health and Recovery Plan (HARP), Managed Long Term Care (MLTC), or Intellectually/Developmentally Disabled (I/DD) VBP subpopulation arrangements are excluded.
The IPC Arrangement includes no additional requirements related to utilization of specific services or historical diagnostic information to be eligible for inclusion in the Arrangement. Members who are non–utilizers (those who do not seek services (including prescription drugs) during the year) are included in the eligible member population count and attributed to the primary care provider (PCP) as outlined below. These members will not contribute to the total cost calculation for the IPC Arrangement, but are included for tracking and quality purposes.
Member Attribution
The State guidance for attribution under the IPC Arrangement is based on member attribution to the Medicaid MCO–assigned PCP. VBP Contractors and the Medicaid MCOs can adopt alternative standards for attribution in their contracts from the guidance above, so long as the contract receives State approval for meeting VBP contracting requirements.
Calculation of Episode Costs
Once the episodes for the IPC Arrangement have been constructed for the attributed population, the costs within each of the underlying episodes (defined as the total amount paid by the Medicaid MCO for episode services) will be combined to produce a total cost of care for the Arrangement.
The aggregate costs can be further analyzed to identify and understand variation across the underlying episodes and by service type, leading to opportunities for improvement in quality of care and resource use.
Section 2: VBP Quality Measure Set for the IPC Arrangement
The 2018 TCGP/IPC Quality Measure Set5 was developed drawing on the work of a number of stakeholder groups convened by the Department of Health (DOH) to solicit input from expert clinicians around the state. The physical health measures were drawn from the measure sets developed by the Diabetes, Chronic Heart Disease, and Pulmonary Clinical Advisory Groups, or CAGs, and from the measures recommended for Advanced Primary Care (APC) by the Integrated Care Workgroup. Likewise, the behavioral health measures were drawn from the measure sets developed by the Behavioral Health CAG.
The State is recommending a full complement of physical and behavioral health measures to help ensure attributed members receive high quality physical, as well as behavioral, health care. Measures recommended by the CAGs were submitted to NYS DOH, the Office of Mental Health (OMH) and Office of Alcoholism and Substance Abuse Services (OASAS) for further feasibility review and, ultimately, to the VBP Workgroup, the group responsible for overall VBP design and final approval for NYS Medicaid. During the final review process, the IPC quality measure set was aligned with existing Delivery System Reform Incentive Payment (DSRIP) Program, Quality Assurance Reporting Requirements (QARR) measures, and measures utilized by Medicare and Commercial programs in NYS, where appropriate. The measures were further categorized as Category 1, 2, or 3 based on reliability, validity, and feasibility, and by suggested use as either Pay–for–Reporting (P4R) or Pay–for–Performance (P4P).
Measure Classification
In September and October of 2016, the CAGs published their initial recommendations to the State on quality measures support required for providers to be successful in improving the financial sustainability of New York State´s safety net. Additionally, the report addressed other implementation details related to a VBP IPC Arrangement. Upon receiving the CAG recommendations, the State conducted additional feasibility review and analysis to define a final list of measures for inclusion during the 2017 VBP Measurement Year (MY). Each measure was designated by the State as Category 1, 2, or 3, according to the following criteria:
- CATEGORY 1 – Approved quality measures that are felt to be both clinically relevant, reliable and valid, and feasible;
- CATEGORY 2 – Measures that are clinically relevant, valid, and probably reliable, but where the feasibility could be problematic. These measures will be further investigated during the VBP Pilot program; and,
- CATEGORY 3 – Measures that are insufficiently relevant, valid, reliable and/or feasible.
Note that measure classification is a State recommendation. Although Category 1 Measures are required to be reported, Medicaid MCOs and VBP Contractors can choose the measures they want to link to payment, and how they want to pay on them (P4P or P4R) in their specific contracts.
Category 1
Category 1 quality measures as identified by the CAGs and accepted by the State are to be reported by VBP Contractors. These measures are also intended to be used to determine the amount of shared savings for which VBP contractors would be eligible.6
The State classified each Category 1 measure as either P4P or P4R:
- P4P measures are intended to be used in the determination of shared savings amounts for which VBP Contractors are eligible.7 In other words, these are the measures on which payments in VBP contracts may be based. Measures can be included in both the determination of the target budget and in the calculation of shared savings for VBP Contractors; and,
- P4R measures are intended to be used by the Medicaid MCOs to incentivize VBP Contractors for reporting data to monitor quality of care delivered to members under the VBP contract. Incentives for reporting should be based on timeliness, accuracy, and completeness of data. Measures can be reclassified from P4R to P4P through annual CAG and State review or as determined by the Medicaid MCO and VBP Contractor.
Not all Category 1 measures will be reportable for Measurement Year 2018, as reporting on some of these measures will be phased in over the next 2 years. Please see the Value Based Payment Reporting Requirements Technical Specifications Manual8 for details as to which measures must be reported for the measurement year. This manual will be updated annually each fall, in line with the release of the final VBP measure set for the subsequent year.
Categories 2 and 3
Category 2 measures have been accepted by the State based on agreement of measure importance, validity, and reliability, but flagged as presenting concerns regarding implementation feasibility. These measures will be further investigated in the VBP pilots. The State requires that VBP Pilots select and report a minimum of one Category 2 measure per VBP arrangement for MY 2018 (or have a State and Plan approved alternative). VBP Pilot participants will be expected to share meaningful feedback on the feasibility of Category 2 measures when the CAGs reconvene during the Annual Measure Review.
Measures designated as Category 3 were identified as unfeasible at this time or as presenting additional concerns including accuracy or reliability when applied to the attributed member population for the IPC Arrangement. Several measures in the original CAG report were removed for small sample size at a VBP contractor level or already high performance at a statewide level, as examples, and therefore are no longer in the Category 1 or 2 measure list. These measures will not be tested in pilots or included in VBP arrangements in 2018.
Annual Measure Review
Measure sets and classifications are considered dynamic and will be reviewed annually. Updates will include additions, deletions, change in categorization, and reclassification from P4R to P4P or P4P to P4R based on experience with measure implementation in the prior year. During 2018, the CAGs and the VBP Workgroup will reevaluate measures and provide recommendations for MY 2019. A full list of the 2018 TCGP/IPC measures is located in the NYS VBP Resource Library on the DOH website.9
Appendix:
VBP Glossary
VBP Glossary
- Diagnosis codes: These are codes (as defined in the PROMETHEUS grouper) based on the International Classification of Diseases (ICD) that are used to group and categorize diseases, disorders, symptoms, etc. These codes help identify clinically related services to be included in the episode in conjunction with the relevant procedure codes. These codes may include trigger codes, signs and symptoms and other related conditions and are used to steer services into an open episode.
- Episode of Care: An Episode of Care includes groups of clinically related services (as defined in the PROMETHEUS Analytics grouper) delivered by physicians and ancillary providers across multiple settings of care during a defined period.
- Grouper: PROMETHEUS Analytics system. The rules for each episode are programmed into an analytic tool that runs on claims data in a systematic fashion. The analytic program – the grouper – governs what starts or "triggers" an episode, the length of time an episode will run, and the kinds of services that are grouped together to form the episode.
- Included Service: A service that is pulled into an episode by the PROMETHEUS Analytics system grouper is an included service.
- Initial and Confirming Triggers: An initial trigger initiates an episode based on diagnosis and/or procedure codes found on institutional or non–institutional claims data. For many episodes, a second trigger (the confirming trigger), is necessary to initiate the episode in the contract year. Sometimes an episode itself could serve as a trigger for another episode, e.g., the URI episode is a trigger for the Sick Care episode.
- Look Back & Look Forward: From the point in which an episode is triggered, episode costs and volume are evaluated within the associated time window for a predetermined number of days before and after the trigger date. Costs, volume, and other episode components that fall within this range are captured within the episode.
- Pharmacy codes: These are codes used to identify relevant pharmacy claims to be included in the episode. The PROMETHEUS Analytics system groups pharmacy National Drug Codes (NDC) into higher categories using the National Library of Medicine´s open–source RxNorm drug classification system.
- Procedure codes: These are codes used to identify clinically–related services to be included in the episode in conjunction with the typical diagnosis codes. Procedure codes include International Classification of Diseases (ICD) procedures, Healthcare Common Procedure Coding System (HCPCS), and Current Procedural Terminology (CPT) codes.
- Time–window: This is the time that an episode is open for analytic purposes. It may include the trigger event, a look–back period, and a look–forward period and could extend based on rules and criteria.
- Trigger code: A trigger code assigns a time window for the start and end dates of each episode (depending on the episode Type). Trigger codes can be ICD diagnosis or procedure codes, CPT codes, or HCPCS codes, and could be present on an inpatient facility claim, an outpatient facility claim, or a professional claim.
- VBP Contractor: An entity – either a provider or groups of providers – engaged with a Medicaid MCO in a VBP contract.
_____________________________________
1. Details on Episode of Care definitions and PROMETHEUS Analytics, including information on associated diagnostic and procedure codes, are available on the PROMETHEUS Analytics website (Link) 1
2. Ibid. 2
3. Beginning in Measurement Year 2018, the Tonsillectomy Episode will no longer be included in the grouping for the IPC Arrangement within the Sick Care Component, since tonsillectomy procedures are less directly impactable by PCPs. Therefore, providers contracting in an IPC Arrangement will not be held accountable for the episode costs associated with this procedure. (Link) 3
4. Ibid. 4
5. The IPC Arrangement measure set is the same set that will be used for the Total Care for the General Population (TCGP) Arrangement in MY 2018. Therefore, it is referred to as the TCGP/IPC quality measure set. 5
6. New York State Department of Health, Medicaid Redesign Team, A Path toward Value Based Payment: Annual Update, June 2016: Year 2, New York State Roadmap for Medicaid Payment Reform, June 2016, p. 34. (Link). 6
7. Ibid. 7
8. 2018 Value Based Payment Reporting Requirements; Technical Specifications Manual, Nov 2017, File is located in the Quality Measures tab of the VBP Resource Library (Link) 8
9. NYS Delivery System Reform Incentive Payment (DSRIP) - VBP Resource Library (Link) 9
Follow Us