2019 Value Based Payment Reporting Requirements
Technical Specifications Manual
- Manual is also available in Portable Document Format (PDF)
_______________________________________________________________________
New York State Department of Health
Email Address: nysqarr@health.ny.gov
__________________________________________________
HEDIS® is a registered trademark of the National Committee for Quality Assurance (NCQA).
__________________________________________________
Last revised December 14, 2018
2019 Value Based Payment Technical Specifications Manual
Table of Contents
- Introduction
- Categorization of Quality Measures
- Classification of Quality Measures
- Organizations Required to Report
- Reporting Requirement Guidelines
- Specific Instructions per contracted VBP arrangement:
- New Measures
- Where to Submit VBP Reporting Data
- What to Send for VBP Reporting
- Questions Concerning 2018 VBP Reporting
- The NYS PCMH Patient–Level Detail File
- Patient Attribution File
- Attribution Methodology:
- File Format:
- File Submission:
- Attribution Methodology:
- File Format:
- Field Definitions:
- File Submission:
I. SUBMISSION REQUIREMENTS
Introduction
The purpose of this document is to make stakeholders aware of the quality measure reporting requirements for Medicaid Managed Care Organizations (MCOs) participating in the New York State Medicaid (NYS) VBP program. The 2019 Value Based Payment Reporting Requirements refer to 2018 Measurement Year (MY) data, except for Managed Long-Term Care plans, for which the reporting requirements refer to 2019 MY data. Section II of the document includes guidance on the organizations responsible for reporting, the subset of measures for which reporting will be required by VBP Arrangement, and the changes to the reportable set of MY 2018 Quality Measure Sets (see the VBP Quality Measure tab).
The New York State Department of Health (NYS DOH) is mid-way through the first phase of a health transformation effort, known as the State Innovation Model (SIM) award, which focuses on transformation of primary care delivery and payment models statewide. The New York State Patient Centered Medical Home (NYS PCMH) model as part of the SIM initiative is intended to integrate a service delivery and reimbursement model to improve health quality outcomes that are financially sustainable. To reduce the burden on MCOs participating in both the NYS PCMH model and Medicaid VBP, we are aligning the reporting for both programs and utilizing the NYS PCMH Scorecard data request to fulfill reporting requirements for both programs. Section III describes File Specifications required for reporting. More information on the State Health Innovation Plan can be found here.
VBP Arrangements and Associated Quality Measures
The VBP Roadmap outlines five types of VBP arrangements to be included for MY 2018:
- Total Care for the General Population (TCGP) Arrangement: Includes all costs and outcomes for care, excluding certain subpopulations (specified below).
- Total Care for Special Needs Subpopulation Arrangements: Includes costs and outcomes of total care for all members within a subpopulation exclusive of TCGP.
- Health and Recovery Plans (HARP): For those with Serious Mental Illness or Substance Use Disorders
- HIV/AIDS
- Managed Long Term Care (MLTC)
- Episodic Care Arrangements:
- Integrated Primary Care (IPC): Includes all costs and outcomes associated with primary care, sick care, and a set of chronic conditions selected due to high volume and/or costs.
- Maternity Care: Includes episodes associated with a pregnancy, including prenatal care, delivery and postpartum care through 60 days post–discharge for the mother, and care provided to the newborn from birth through the first month post–discharge.
Categorization of Quality Measures
Through a multi–group stakeholder engagement process, a set of quality measures was defined for each arrangement. Based on an analysis of clinical relevance, reliability, validity, and feasibility, each measure was placed into one of three categories:
- Category 1: Selected as clinically relevant, reliable, valid, and feasible. These measures are outlined in Table 1 below.
- REQUIREMENT: Only the Category 1 measures that are indicated in this document as "Required to Report" are to be reported by the MCO to the State.
- Category 2: Seen as clinically relevant, valid, and reliable, but where the feasibility could be problematic. Category 2 measures are listed in the appendix of this guide.
- Category 3: Rejected based on a lack of relevance, reliability, validity, and/or feasibility. These measures are not included in this manual.
Classification of Quality Measures
Each Category 1 measure is classified as either Pay–for–Performance (P4P) or Pay–for–Reporting (P4R). Pay–for– Performance measures are intended to be used in the determination of shared savings amounts for which VBP Contractors are eligible. P4R measures are intended to be used by the MCOs to incentivize the VBP Contractors for reporting data to monitor quality of care delivered to members in a VBP contract. At least one Category 1 P4P measure must be included in a VBP contract.
|table of contents|Organizations Required to Report
Medicaid Managed Care Organizations with Level 1 or higher value–based contracting arrangements or MCOs with a VBP Pilot contract are required to report.
|table of contents|Reporting Requirement Guidelines
- Table 1 lists, by arrangement, the 2018 VBP Category 1 Measure sets and indicates the 2018 measures the State is requiring for reporting.
- Table 2 lists, by arrangement, the 2019 MLTC VBP Category 1 Measure set and indicates the 2019 measures required for reporting.
- Section III describes File Specifications required for reporting.
- This manual describes reporting requirements only. For VBP contracting questions, please contact nysqarr@health.ny.gov
- Organizations must purchase the HEDIS® 2019 Technical Specifications for descriptions of the required HEDIS® measures. For specifications for other non–HEDIS measures, please contact the measure steward for the correct version of the specification.
Specific Instructions per contracted VBP arrangement:
TCGP/IPC: The State is requesting that Medicaid Managed Care (MMC) plans submit data files that leverage their 2019 QARR (HEDIS) submission which will be used to create aggregated quality results by VBP Contractor. Specifically, the State is asking insurers to provide a modified version of NYS Patient–Level Detail (PLD) file, along with provider and practice information. Submission of the Advanced Primary Care (APC) Scorecard file will fulfill this reporting requirement. The NYS PCMH Patient–Level Detail File layout is included in Section III. A separate Patient Attribution file is not required for this arrangement. Patient attribution is included in the NYS PCMH Patient–Level Detail File.
Maternity: The State is requesting that MMC plans submit data files that leverage their 2019 QARR Live Birth Files. Include the provider/practice that was attributed to the member using your own plan’s attribution methodology for all members included in the 2019 QARR Live Birth File. Several fields regarding the provider and practice site of the service have been added to the layout request for this purpose. The Patient Attribution file layout is included in Section III.
HARP: HARP arrangements are required to report relevant TCGP/IPC measures and HARP–specific measures. The State is requesting that MMC plans submit data files that leverage their 2019 QARR (HEDIS) submission which will be used to create aggregated quality results by VBP Contractor. The State is asking plans to provide a modified version of NCQA’s Patient–Level Detail (PLD) file, along with provider and practice information. Submission of the NYS PCMH Scorecard file will fulfill the IPC reporting requirement. Additionally, the State is asking insurers to provide an attribution file for all members enrolled in your HARP arrangement. The attribution file will be used to link to the 2019
QARR Patient–Level Detail (PLD) file and NYS calculated measure results to create aggregate quality results for HARP–specific measures by VBP Contractor. The Patient Attribution file layout is included in Section III.
HIV/AIDS: HIV/AIDS arrangements are required to report relevant TCGP/IPC measures and HIV–specific measures. The State is requesting that MMC plans submit data files that leverage their 2019 QARR (HEDIS) submission which will be used to create aggregated quality results by VBP Contractor. The State is asking plans to provide a modified version of NCQA’s Patient–Level Detail (PLD) file, along with provider and practice information for all lines of business operating in New York. Submission of the NYS PCMH Scorecard file will fulfill the IPC reporting requirement. Additionally, the State is asking insurers to provide an attribution file for all members enrolled in your HIV/AIDS arrangement. The attribution file will be used to link to the 2019 NYS calculated measure results to create aggregate quality results for HIV–specific measures by VBP Contractor. The Patient Attribution file layout is included in Section III.
MLTC: The State is requesting insurers to submit a Patient Attribution file, which will be used to create aggregated quality results by Provider or VBP Contractor. DOH will calculate all reportable Category 1 quality measure results for the arrangements. The attribution methodology and Patient Attribution file layout is included in Section III.
|table of contents|Measure Changes
Changes to the Reporting Requirements for 2018 Measure Set were made based on the feedback received by the DOH from the Clinical Advisory Groups, Measure Support Task Force and Sub–teams, and from other stakeholder groups. Those changes are indicated below. In instances where a measure was moved from Category 1 in MY 2018 to Category 2 in MY 2019 or removed entirely, the State will not require reporting of the data related to those measures.
TCGP/IPC:
Category 1: Changes
- Comprehensive Diabetes Care: Foot Exam; removed as a Category 1 Measure.
- Comprehensive Diabetes Care: Hemoglobin A1c (HbA1c) Control (<8.0%); removed as a Category 1 Measure.
- Comprehensive Diabetes Care: Hemoglobin A1c (HbA1c) testing [performed]; removed as a Category 1 Measure.
- Comprehensive Diabetes Screening: All Three Tests (HbA1c, dilated eye exam, and medical attention for nephropathy); removed as a Category 1 Measure.
- Statin Therapy for Patients with Diabetes; removed as a Category 1 Measure.
HARP:
Category 1: Changes
- Comprehensive Diabetes Care: Foot Exam; removed as Category 1 Measure Set.
- Comprehensive Diabetes Care: Hemoglobin A1c (HbA1c) Control (<8.0%); removed as Category 1 Measure Set.
- Comprehensive Diabetes Care: Hemoglobin A1c (HbA1c) testing [performed]; removed as Category 1 Measure Set.
- Comprehensive Diabetes Screening: All Three Tests (HbA1c, dilated eye exam, and medical attention for nephropathy); removed as Category 1 Measure Set.
- Statin Therapy for Patients with Diabetes; removed as Category 1 Measure.
HIV/AIDS:
Category 1: Changes
- Comprehensive Diabetes Care: Foot Exam; removed as Category 1 Measure.
- Comprehensive Diabetes Care: Hemoglobin A1c (HbA1c) Control (<8.0%); removed as Category 1 Measure.
- Comprehensive Diabetes Care: Hemoglobin A1c (HbA1c) testing [performed]; removed as Category 1 Measure.
- Comprehensive Diabetes Screening: All Three Tests (HbA1c, dilated eye exam, and medical attention for nephropathy); removed as Category 1 Measure.
- Statin Therapy for Patients with Diabetes; removed as Category 1 Measure.
- Substance Abuse Screening; moved from Category 1 to Category 2
Maternity:
Category 2: Changes
- Monitoring and Reporting of NICU Referral Rates; removed as Category 2 Measure.
MLTC:
Category 1: Changes
- Percentage of members who did not have falls resulting in medical intervention in the last 90 days; removed as a Measure.
- Percentage of members who did not have an emergency room visit in the last 90 days; removed as a Measure.
New Measures
TCGP/IPC:
Category 1: Changes
- Adolescent Preventive Care Measures; added as a Category 1 Measure.
- Adolescent Well–Care Visits; added as a Category 1 Measure.
- Annual Dental Visit; added as a Category 1 Measure.
- PDI #14 Asthma Admission Rate; added as a Category 1 Measure.
- Follow–Up Care for Children Prescribed ADHD Medication; added as a Category 1 Measure.
- Immunizations for Adolescents; added as a Category 1 Measure.
- Well–Child Visits in the First 15 Months of Life; added as a Category 1 Measure.
- Well–Child Visits in the Third, Fourth, Fifth, and Sixth Year of Life; added as a Category 1 Measure.
Category 2: Changes
- Developmental Screening Using Standardized Tool, First Three Years of Life; added as a Category 2 Measure.
- Follow–Up After Emergency Department Visit for Alcohol and Other Drug Dependence; added as a Category 2 Measure.
- Follow–Up After Emergency Department Visit for Mental Illness; added as a Category 2 Measure.
- Maternal Depression Screening; added as a Category 2 Measure.
- Screening for Reduced Visual Acuity and Referral in Children; added as a Category 2 Measure.
- Use of First–Line Psychosocial Care for Children and Adolescents on Antipsychotics; added as a Category 2 Measure.
MLTC:
Category 1: Changes
- Percentage of members who did not experience falls that resulted in major or minor injury in the last 90 days; added as a new measure.
Where to Submit VBP Reporting Data
- Electronically submit all files (no later than 11:59 p.m. ET on August 1, 2019) via a secure file transfer facility. Do not mail materials.
- Specific delivery instructions are given for each file.
What to Send for VBP Reporting
All submissions must be received electronically by 11:59 p.m. ET on August 1, 2019.
☐ Patient–Level Detail file: IPC, TCGP, HARP, HIV/AIDS
☐ Patient Attribution File: Maternity, HARP, HIV/AIDS, MLTC
|table of contents|Questions Concerning 2018 VBP Reporting
Please submit all questions to nysqarr@health.ny.gov
|top of section| |table of contents|II. REPORTING REQUIREMENTS
Table 1: 2018 VBP List of Required Measures
| Measures | Notes | Arrangement Type | NQF ID | Specifications | Class | ||||
|---|---|---|---|---|---|---|---|---|---|
| TCGP | IPC | Maternity | HARP | HIV/AIDS | |||||
| Total Care for the General Population (TCGP)/ Integrated Primary Care (IPC) | |||||||||
| Adherence to Mood Stabilizers for Individuals with Bipolar I Disorder | NR | NR | NA | NA | NR | 1880 | HEDIS 2019 | P4P | |
| Adolescent Preventive Care Measures | 2 | NR | NR | NA | NA | NA | NYS 2019 | P4R | |
| Adolescent Well–Care Visits | ✓ | ✓ | NA | NA | NA | HEDIS 2019 | P4R | ||
| Annual Dental Visit | ✓ | ✓ | NA | NA | NA | 1388 | HEDIS 2019 | P4R | |
| Antidepressant Medication Management | ✓ | ✓ | NA | NA | ✓ | 0105 | HEDIS 2019 | P4P | |
| PDI #14 Asthma Admission Rate | NR | NR | NA | NA | NA | 0728 | AHRQ | P4P | |
| Breast Cancer Screening | ✓ | ✓ | NA | ✓ | ✓ | 2372 | HEDIS 2019 | P4P | |
| Cervical Cancer Screening | 2 | ✓ | ✓ | NA | ✓ | ✓ | 0032 | HEDIS 2019 | P4P |
| Childhood Immunization Status – combination 3 | 2 | ✓ | ✓ | NA | NA | NA | 0038 | HEDIS 2019 | P4P |
| Chlamydia Screening in Women | ✓ | ✓ | NA | ✓ | NA | 0033 | HEDIS 2019 | P4P | |
| Colorectal Cancer Screening | 2 | ✓ | ✓ | NA | ✓ | ✓ | 0034 | HEDIS 2019 | P4P |
| Comprehensive Diabetes Care: Eye Exams | 2 | ✓ | ✓ | NA | ✓ | ✓ | 0055 | HEDIS 2019 | P4P |
| Comprehensive Diabetes Care: Hemoglobin A1c (HbA1c) Poor Control (>9.0%) | 2 | ✓ | ✓ | NA | ✓ | ✓ | 0059 | HEDIS 2019 | P4P |
| Comprehensive Diabetes Care: Medical Attention for Nephropathy | 2 | ✓ | ✓ | NA | ✓ | ✓ | 0062 | HEDIS 2019 | P4P |
| Controlling High Blood Pressure | 2 | ✓ | ✓ | NA | ✓ | ✓ | 0018 | HEDIS 2019 | P4P |
| Diabetes Screening for People with Schizophrenia or Bipolar Disorder Using Antipsychotic Medications | ✓ | ✓ | NA | ✓ | ✓ | 1932 | HEDIS 2019 | P4P | |
| Follow–Up Care for Children Prescribed ADHD Medication | ✓ | ✓ | NA | NA | NA | 0108 | HEDIS 2019 | P4R | |
| Immunizations for Adolescents – Combination 2 | ✓ | ✓ | NA | NA | NA | 1407 | HEDIS 2019 | P4P | |
| Initiation and Engagement of Alcohol & Other Drug Abuse or Dependence Treatment | ✓ | ✓ | NA | ✓ | ✓ | 0004 | HEDIS 2019 | P4P | |
| Initiation of Pharmacotherapy upon New Episode of Opioid Dependence | ✓ | ✓ | NA | ✓ | ✓ | NYS 2019 | P4P | ||
| Medication Management for People with Asthma | ✓ | ✓ | NA | ✓ | ✓ | 1799 | HEDIS 2019 | P4P | |
| Potentially Avoidable Complications (PAC) in Routine Sick Care or Chronic Care | NR | NR | NA | NA | NA | Altarum | P4R | ||
| Preventive Care and Screening: Body Mass Index (BMI) Screening and Follow–Up Plan | NR | NR | NA | NR | NR | 0421 | CMS 2018 | P4R | |
| Preventive Care and Screening: Influenza Immunization | NR | NR | NA | NR | NR | 0041 | AMA v1.0 | P4R | |
| Preventive Care and Screening: Screening for Clinical Depression and Follow–Up Plan | NR | NR | NR | NR | NR | 0418 | CMS 2018 | P4R | |
| Preventive Care and Screening: Tobacco Use: Screening and Cessation Intervention | NR | NR | NA | NR | NR | 0028 | AMA v1.0 | P4R | |
| Statin Therapy for Patients with Cardiovascular Disease | ✓ | ✓ | NA | ✓ | ✓ | HEDIS 2019 | P4R | ||
| Use of Pharmacotherapy for Alcohol Abuse or Dependence | ✓ | ✓ | NA | ✓ | ✓ | NYS 2019 | |||
| Use of Spirometry Testing in the Assessment and Diagnosis of COPD | ✓ | ✓ | NA | ✓ | ✓ | 0577 | HEDIS 2019 | P4R | |
| Weight Assessment and Counseling for Nutrition and Physical Activity for Children/Adolescents | 2 | ✓ | ✓ | NA | ✓ | ✓ | 0024 | HEDIS 2019 | P4P |
| Well–Child Visits in the First 15 Months of Life | ✓ | ✓ | NA | NA | NA | 1392 | HEDIS 2019 | P4P | |
| Well–Child Visits in the Third, Fourth, Fifth, and Sixth Year of Life | ✓ | ✓ | NA | NA | NA | 1516 | HEDIS 2019 | P4P | |
| Maternity | |||||||||
| Contraceptive Care – Postpartum | NA | NA | NR | NA | NA | 2902 | US Office of Population Affairs | P4R | |
| C–Section for Nulliparous Singleton Term Vertex (NSTV) | NA | NA | NR | NA | NA | 0471 | TJC 2017 | P4R | |
| Exclusively Breast Milk Feeding | NA | NA | NR | NA | NA | 0408 | TJC 2017 | P4R | |
| Incidence of Episiotomy | NA | NA | NR | NA | NA | 0470 | Christiana Care Health | P4R | |
| Low Birth Weight [Live births weighing less than 2,500 grams (preterm v. full term)] | 1 | NA | NA | ✓ | NA | NA | 0278 | AHRQ v7.0 | P4R |
| Percentage of Preterm Births | NA | NA | NR | NA | NA | NYS 2019 | P4R | ||
| Prenatal and Postpartum Care | 2 | NA | NA | ✓ | NA | NA | 1517 | HEDIS 2019 | P4P |
| Health and Recovery Program (HARP) | |||||||||
| Continuity of Care from Inpatient Detox to Lower Level of Care | NA | NA | NA | ✓ | NA | NYS 2019 | P4P | ||
| Continuity of Care from Inpatient Rehabilitation for Alcohol and Other Drug Abuse or Dependence Treatment to Lower Level of Care | NA | NA | NA | ✓ | NA | NYS 2019 | P4P | ||
| Follow–Up After Emergency Department Visit for Mental Illness | NA | NA | NA | ✓ | NA | 2605 | HEDIS 2019 | P4P | |
| Follow–Up After Emergency Department Visit for Alcohol and Other Drug Dependence | NA | NA | NA | ✓ | NA | 2605 | HEDIS 2019 | P4P | |
| Follow–Up After Hospitalization for Mental Illness | NA | NA | NA | ✓ | NA | 0576 | HEDIS 2019 | P4P | |
| Maintaining/Improving Employment or Higher Education Status | 1 | NA | NA | NA | ✓ | NA | NYS 2019 | P4R | |
| Maintenance of Stable or Improved Housing Status | 1 | NA | NA | NA | ✓ | NA | NYS 2019 | P4R | |
| No or Reduced Criminal Justice Involvement | 1 | NA | NA | NA | ✓ | NA | NYS 2019 | P4R | |
| Percentage of Members Enrolled in a Health Home | 1 | NA | NA | NA | NR | NA | NYS 2019 | P4R | |
| Potentially Preventable Mental Health Related Readmission Rate 30 Days | 1 | NA | NA | NA | ✓ | NA | NYS 2019 | P4P | |
| HIV/AIDS | |||||||||
| HIV Viral Load Suppression | 1 | NA | NA | NA | NA | ✓ | HRSA | P4P | |
| Potentially Avoidable Complication (PAC) in Patients with HIV/AIDS | 1 | NA | NA | NA | NA | NR | Altarum | P4R | |
✓ – Required to Report NA – Not Applicable to the Arrangement Shading (NR) – Purple– Not required to be reported
1 – There are no reporting requirements for this measure. NYS will calculate the measure result for MY 2017
2 – For measures that you may have reported using the hybrid sample in the PLD for QARR, we request that you
report the administrative denominator and numerator for VBP.
Table 2: 2019 MLTC VBP List of Required Measures
| Measures | Notes | Arrangement Type | NQF ID | Specifications | Class | ||||
|---|---|---|---|---|---|---|---|---|---|
| MLTC | |||||||||
| Managed Long Term Care (MLTC) | |||||||||
| Percentage of members who did not have an emergency room visit in the last 90 days | 1 | ✓ | NYS 2019 | P4P | |||||
| Percentage of members who did not have falls resulting in medical intervention in the last 90 days | 1 | ✓ | NYS 2019 | P4P | |||||
| Percentage of members who received an influenza vaccination in the last year | 1 | ✓ | NYS 2019 | P4P | |||||
| Potentially Avoidable Hospitalizations (PAH) for a primary diagnosis of heart failure, respiratory infection, electrolyte imbalance, sepsis, anemia, or urinary tract infection | 1, 2 | ✓ | NYS 2019 | P4P | |||||
| Percentage of members who remained stable or demonstrated improvement in pain intensity | 1 | ✓ | NYS 2019 | P4P | |||||
| Percentage of members who remained stable or demonstrated improvement in Nursing Facility Level of Care (NFLOC) score | 1 | ✓ | NYS 2019 | P4P | |||||
| Percentage of members who remained stable or demonstrated improvement in urinary continence | 1 | ✓ | NYS 2019 | P4P | |||||
| Percentage of members who remained stable or demonstrated improvement in shortness of breath | 1 | ✓ | NYS 2019 | P4P | |||||
| Percentage of members who did not experience uncontrolled pain | 1 | ✓ | NYS 2019 | P4P | |||||
| Percentage of members who were not lonely and not distressed | 1 | ✓ | NYS 2019 | P4P | |||||
✓ – Required to Report NA – Not Applicable to the Arrangement Shading (NR) – Purple– Not required to be reported
1 – There are no reporting requirements for this measure. NYS will calculate the measure result for MY 2017
2 – NYS will calculate this measure for the community-based providers and the Nursing Homes separately.
III. FILE SPECIFICATIONS
NYS PCMH Scorecard Patient–Level Detail File
Please use your 2019 QARR/HEDIS data warehouse as the source for this information. Do not recalculate or update measure results. However, in addition to the measure elements that you reported for QARR/HEDIS in 2019 we are requesting that you include the provider/practice that was attributed to the member using your own plan’s attribution methodology for the IPC or TCGP arrangement. Several fields regarding the provider and practice site of the service have been added to the layout request for this purpose (Fields #6–20, #103), specifically two separate fields for TIN: practice TIN and contractor TIN. In addition to contractor TIN as health plans contract with different types of entities, such as providers, hospital systems, Independent Practice Associations (IPAs), and Accountable Care Organizations (ACOs) we have added a Contractor Type field. This information has been added to allow us to aggregate the results by VBP Contractor across all New York State MCOs.
The NYS PCMH data file is modeled after the HEDIS 2019 Patient–Level Detail file (PLD) that you prepared as part of your HEDIS submission, and many of the data elements in the NYS PCMH file follow the same definitions and format as used to define the data elements in the HEDIS PLD. You may find it helpful to use the PLD as a resource or starting point in completing the NYS PCMH file. We ask that you populate the PLD with all Lines of Business that you serve, e.g., Medicaid. Once completed, please upload the file to IPRO’s ftp site. A subfolder in the "QARR 2019" folder where you will upload your 2019 QARR files entitled "NYS PCMH 2019" will be created for your submission. If someone other than your QARR liaison will be responsible for NYS PCMH reporting, please contact Paul Henfield at the email address below for access to the FTP site. Please note that the deadline for submission is Thursday, August 1, 2019.
Exceptions to the PLD file are noted below:
- The NYS PCMH file requests Medicare HEDIS data, which is not required for QARR reporting.
- The Plan ID is not your plan’s QARR ID. The Plan ID field should be populated with the Organization ID that you used to submit the IDSS to NCQA. Note that the Organization ID is different from the Submission ID, which is specific to a particular Line of Business. The Organization ID provides for six digits. If your plan’s ID is smaller, please right justify.
- The Childhood Immunization measure requires only a 0 or 1 for the numerator value while QARR requests the actual number of antigens provided. Also, we request that you provide the results for Combo 3 and not by antigen.
- For Medicaid, we ask that you populate the member’s CIN in the ID field; for other products, please use an internally–defined ID number.
- Provider/Practice attribution information is required for NYS PCMH. Such information is not required for QARR.
Specific Instructions:
- Please be aware that although the member ID for all products except Medicaid is an internal number assigned by your plan, you will need to link the member to the provider of service. You should use a naming convention that will facilitate this process.
- If a member is reported for a specific measure in more than one product line (e.g., duals), please report them for only one product, using the following priority: Commercial, then Medicare, then Medicaid. This instruction affects only members who may be reported twice for the same service.
- A Unique Member ID (Field #3), may be included on the file more than once if the member is in more than one product line during the reporting period.
- For measures that you may have reported using the hybrid sample in the PLD, we request that you report the administrative denominator and numerator from the IDSS for NYS PCMH.
- Members in the file must be in at least one measure.
- Measures that are not applicable to the member should be zero–filled.
- Practice Name must be populated in the Practice Name (Field #9) only.
- Practice Address Line 1 (Field #10) must contain the street address of the Practice, not the Practice Name.
- For Fields #6–20, leave these fields blank if the member cannot be attributed to any provider and you are not able to identify the provider.
- The IET Engagement numerator (Field #77 and 80) value must be less than or equal to the Initiation numerator (Field #76 and 79) value.
- For the AAB (Field #72) and LBP (Field #74) measures, provide the actual numerator (non–inverted), e.g., for AAB, the numerator would be members receiving the antibiotic.
For questions regarding this request, please contact Paul Henfield of IPRO at phenfield@ipro.org or 516–209–5670.
The NYS PCMH Patient–Level Detail File Layout will be released in mid–December.
|table of contents|Patient Attribution File
The State is asking insurers to provide an attribution file for all members enrolled in each arrangement per the methodology specified in your state–approved contract. The attribution file will be used in combination with other quality measure sources (e.g. 2019 NYS Patient–Level Detail File) to aggregate quality results for the 2019 Category 1 population–specific measures by VBP Contractor.
NOTE: MLTC attribution instructions are different than for other populations. Follow the specified attribution methodology and file layout for each arrangement.
|table of contents|Attribution Methodology:
Maternity: Include the provider/practice TIN and contractor TIN that was attributed to the member using your own plan’s attribution methodology for all members included in the 2019 QARR Live Birth File in any VBP Level 1 or higher arrangement.
HARP: Include the provider/practice TIN and contractor TIN that was attributed to the member using your own plan’s attribution methodology for all members included in any VBP Level 1 or higher arrangement.
HIV/AIDS: Include the provider/practice TIN and contractor TIN that was attributed to the member using your own plan’s attribution methodology for all members included in any VBP Level 1 or higher arrangement.
|table of contents|File Format:
| Element # | Name | Direction | Allowed Values | Required/Optional | Length | Start | End |
|---|---|---|---|---|---|---|---|
| 1 | Plan ID# | Organization ID used to submit the IDSS to NCQA. | ###### = IDSS Organization ID | R | 6 | 1 | 6 |
| 2 | Product Line | A member´s product line at the end of the measurement period. | 1 = MA 2 = SNP 3 = Medicare 4 = CPPO 5 = CHMO 6 = QHMO 7 = QPOS 8 = QPPO 9 = QEPO 10 = CEPO 11 = HARP | R | 2 | 7 | 8 |
| 3 | Unique Member ID# | Medicaid Client ID Number (CIN) The field is alphanumeric and should be treated as a text field. This field is mandatory – do not leave it blank! | R | 15 | 9 | 23 | |
| 4 | County of Residence | Enter the 3-digit county FIPS code for each member´s residence of county. See the attachment for codes and values to enter here. | ### = FIPS Code 000 = Outside of NYS | R | 3 | 24 | 26 |
| 5 | Zip Code of Residence | R | 5 | 27 | 31 | ||
| 6 | Practice Tax ID# | R | 9 | 32 | 40 | ||
| 7 | PCMH Site ID# | If available plan must include a PCMH Site ID# or an Internal plan practice site ID# (see element #8) | O | 10 | 41 | 50 | |
| 8 | Practice Site ID# | Internal plan practice site ID# | O | 10 | 51 | 60 | |
| 9 | Practice Name | R | 50 | 61 | 110 | ||
| 10 | Practice Address Line 1 | R | 35 | 111 | 145 | ||
| 11 | Practice Address Line 2 | O | 35 | 146 | 180 | ||
| 12 | Practice Address Line 3 | O | 35 | 181 | 215 | ||
| 13 | Practice Address City | R | 25 | 216 | 240 | ||
| 14 | Practice Address State | R | 2 | 241 | 242 | ||
| 15 | Practice Address Zip Code | ##### | R | 5 | 243 | 247 | |
| 16 | Practice Telephone Number | ########## | O | 10 | 248 | 257 | |
| 17 | Physician NPI | R | 10 | 258 | 267 | ||
| 18 | Physician First Name | R | 15 | 268 | 282 | ||
| 19 | Physician Middle Name | O | 1 | 283 | 283 | ||
| 20 | Physician Last Name | R | 35 | 284 | 318 | ||
| 21 | Contractor Tax ID# | Populate with valid TINs only. If member is NOT in a VBP level 1 or higher arrangement set to | ######### | R | 9 | 319 | 327 |
| 22 | Contractor ´DBA´ Name | R | 50 | 328 | 377 | ||
| 23 | Contractor Type | Enter ´1´ If the contractor is a provider (provider includes hospitals), ´2´ if the contractor is an IPA, ´3´ if the contractor is an ACO, ´9´ if Unknown | R | 1 | 378 | 379 |
File Submission:
Files for the Maternity, HARP, HIV/AIDS arrangements are to be submitted to the New York State Department of Health via the Secure File Transfer 2.0 of the Health Commerce System. Files should be submitted to Lindsay Cogan (ljw02). Files are to be submitted by close of business on August 1, 2019.
|table of contents|MLTC Attribution File
For 2019, all P4P Category 1 measures for the MLTC arrangement will be computed by DOH to reduce the burden on the MTLC plans.
|table of contents|Attribution Methodology:
Partial/MAP/PACE/FIDA: Plan enrollees who have four or more months of continuous enrollment from April 2018 through June 2019 should be submitted in this attribution file. This attribution should be to provider organizations of CHHA, LHCSA, and SNF, which had the most frequent contact with the member and, therefore, could potentially affect the need for hospitalization or not. Services being received by the member through Consumer Directed Personal Assistance (CDPAS) should not be include in this attribution file.
|table of contents|File format:
- Include only members who had 4 months or more continuous enrollment in an MLTC plan from April 2018 through June 2019.
- For those meeting the criteria in step 1, provide at least one row for every member who was enrolled in the MLTC plan during the reporting period
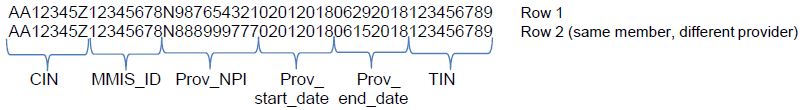
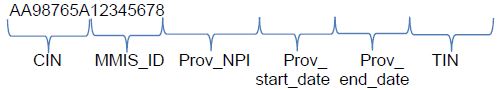
- For each member from step 2, list all provider organization(s) that provided at least one service per month, for 4 or more continuous months from April 2018 through June 2019. The data should be formatted in a long form containing one row of data for each member/provider combination. Please provide one row of data for every provider a member was serviced by (see Example 1 below). If a member does not have any providers from which they received 4 or more continuous months of care, THE MEMBER SHOULD STILL BE LISTED (see example 2 below).
- The text file must be either: 1) fixed–width and named PROVIDERS_MLTC.TXT, or 2) comma separated values (CSV) and named PROVIDERS_MLTC.CSV.
- Fixed–width files
- Must have column start/end locations as documented in the following table.
- Data must not include column names. The first row in the file must be data.
- CSV files
- Must not have additional columns beyond those shown in the following table.
- Data must include column names. The first row in the file must be the column names as documented in the following table.
- Fixed–width files
- The following table provides instructions on the submission of member–level data.
| # | Field Name | Data Type | Start Column Placement |
End Column Placement |
Details/Comments |
|---|---|---|---|---|---|
| 1 | CIN | Varchar | 1 | 8 | A Participant´s Medicaid client identification number. The field should be continuous without any spaces or hyphens. The field is alpha– numeric and should be treated as a text field. This field may not be NULL. |
| 2 | MMIS_ID | Varchar | 9 | 16 | The MLTC Plan´s numeric eight–digit ID. This field may not be NULL. |
| 3 | Prov_NPI | Varchar | 17 | 26 | The unique 10–digit National Provider Identifier (NPI) for provider 1, by which the member was serviced by during the reporting period. |
| 4 | Prov_start_date | Date | 27 | 34 | MMDDYYYY – Must be between April 2018 – June 2019 |
| 5 | Prov_end_date | Date | 35 | 42 | MMDDYYYY – Must be between April 2018 – June 2019 |
| 6 | Contractor TIN | Varchar | 43 | 51 | The unique 9–digit tax identification number of the VBP Contractor. Only submit the TIN, if this member is included in a Level 2 arrangement with a VBP Contractor. If not applicable, fill with 99999999. |
Field Definitions:
Prov_NPI: This is the unique 10–digit National Provider Identifier (NPI) of the provider the member was serviced by during the reporting period. This should be a provider organization which had frequent contact with the member and, therefore, could potentially affect the need for hospitalization or not. A member may be serviced by multiple providers during the same time period (provide one row of data for every provider a member was serviced by).
Prov_start_date: This is the service start date with the provider. This date must be during the reporting period. It should be in the format of MMDDYYYY with no intervening "–" or "/". The format is the same if data is submitted via a fixed–width file or CSV.
Prov_end_date: This is the service end date with the provider. This date must be during the reporting period. It should be in the format of MMDDYYYY with no intervening "–" or "/". The format is the same if data is submitted via a fixed–width file or CSV.
Contractor TIN: This is the unique 9–digit tax identification number of the VBP Contractor (not the provider) that the member is assigned to for a Level 2 arrangement during the reporting period. A member can only be assigned to one VBP contactor at a time. If not applicable, fill with 999999999.
VBP Contractor: The VBP Contractor may be an ACO, IPA or large LHCSA/CHHA that is coordinating services for many LHCSAs or CHHAs.
|table of contents|File Submission:
Files are to be submitted to the New York State Department of Health via the Secure File Transfer 2.0 of the Health Commerce System. Files should be submitted to OQPS MLTC Evaluation mailbox. Files are to be submitted by close of business on August 1, 2019.
NOTE: When an NPI has overlapping service dates for a member, the service dates should be collapsed into one record with the earliest start date and furthest end date.
|table of contents|Submission Examples:
Example 1:
The example below illustrates two different providers, with overlapping services dates, aiding a single member from February through June 2018.
Example 2:
The example below illustrates a member who was continuously enrolled for 4 or more months in the health plan, but did not receive at least one service per month from a provider organization, for 4 or more continuous months from April 2018 through June 2019.
Fully Capitated Plans: Because the HEDIS and CMS based P4R category 1 measures cannot be calculated by the State, plans must calculate and report Plan/Provider– VBP Contractor performance to the State by June 17, 2019. Files are to be submitted to the New York State Department of Health via the Secure File Transfer 2.0 of the Health Commerce System. Files should be submitted to OQPS MLTC Evaluation mailbox. Plans should submit an Excel file with the following format. Submit a row for each measure being reported. Plans are required to report on all measures for each plan–provider ("VBP Contractor") combinations
| # | Field Name | Data Type | Excel Column Placement | Details/Comments |
|---|---|---|---|---|
| 1 | MMIS_ID | Varchar | Column A | The MLTC Plan´s numeric eight–digit ID. This field may not be NULL. |
| 2 | Prov_NPI | Varchar | Column B | The unique 10–digit National Provider Identifier (NPI) for the provider by which the member was serviced by during the reporting period. This field may not be NULL. For PACE plans reporting on their own performance, use the MMIS_ID in this field. |
| 3 | TIN | Varchar | Column C | The unique 9–digit tax identification number of the VBP contractor, if applicable. If not applicable, fill with 99999999. |
| 4 | Measure | Varchar | Column D | The name of the P4R measure. |
| 5 | Measure ID | Varchar | Column E | Use the NQF measure ID for the HEDIS measures, for the CMS measures assign 1=advance directive, 2=Not in Nursing home, 3= ED use. |
| 6 | Denominator for Measure | Varchar | Column F | Report the total number of members included in the denominator for the given measure |
| 7 | Numerator for Measure | Varchar | Column G | Report the total number of members that were included in the numerator for the given measure |
| 8 | Exclusions for Measure | Varchar | Column H | Report the number of members excluded from the given measure |
| 9 | Rate for Measure | Varchar | Column I | Report the rate to the hundredth decimal place |
IV. APPENDIX
Table 3: 2018 VBP List of Category 2 Measures
| Measures | Notes | Arrangement Type | NQF ID | Measure Steward | ||||
|---|---|---|---|---|---|---|---|---|
| IPC | TCGP | Maternity | HARP | HIV/AIDS | ||||
| Integrated Primary Care (IPC)/ Total Care for the General Population (TCGP) | ||||||||
| Asthma: Assessment of Asthma Control – Ambulatory Care Setting* | Cat 2 | Cat 2 | NA | Cat 2 | Cat 2 | The American Academy of Allergy, Asthma & Immunology (AAAAI) | ||
| Continuing Engagement in Treatment (CET) Alcohol and Other Drug Dependence | Cat 2 | Cat 2 | NA | Cat 2 | Cat 2 | NYS TBD | ||
| Continuity of Care from Inpatient Detox to Lower Level of Care | Cat 2 | Cat 2 | NA | Cat 2 | Cat 2 | NYS 2019 | ||
| Continuity of Care from Inpatient Rehabilitation for Alcohol and Other Drug Abuse or Dependence Treatment to Lower Level of Care | Cat 2 | Cat 2 | NA | Cat 2 | Cat 2 | NYS 2019 | ||
| Developmental Screening Using Standardized Tool, First Three Years of Life | Cat 2 | Cat 2 | NA | NA | NA | 1488 | Oregon Health and Science University | |
| Follow–up after Emergency Department Visit For Alcohol and Other Drug Dependence | Cat 2 | Cat 2 | NA | NA | NA | |||
| Follow–up after Emergency Department Visit For Mental Illness | Cat 2 | Cat 2 | NA | NA | NA | |||
| Home Management Plan of Care (HMPC) Document Given to Patient/Caregiver (asthma) | Cat 2 | Cat 2 | NA | Cat 2 | Cat 2 | 0338 | The Joint Commission | |
| Initiation of Pharmacotherapy upon New Episode of Alcohol Abuse or Dependence | Cat 2 | Cat 2 | NA | Cat 2 | Cat 2 | NYS 2019 | ||
| Lung Function/Spirometry Evaluation (asthma) | Cat 2 | Cat 2 | NA | Cat 2 | Cat 2 | AAAAI | ||
| Asthma Action Plan | Cat 2 | Cat 2 | NA | Cat 2 | Cat 2 | AAAAI | ||
| Topical Fluoride for Children at Elevated Caries Risk, Dental Services | Cat 2 | Cat 2 | NA | Cat 2 | Cat 2 | 2528 | American Dental Association | |
| Use of Pharmacotherapy for Alcohol Use Disorder | Cat 2 | Cat 2 | NA | Cat 2 | Cat 2 | 0034 | NYS 2019 | |
| Use of Pharmacotherapy for Opioid Dependence | Cat 2 | Cat 2 | NA | Cat 2 | Cat 2 | 0055 | NYS 2019 | |
| Maternity | ||||||||
| Antenatal Hydroxyprogesterone | NA | NA | Cat 2 | NA | NA | TBD | ||
| Antenatal Steroids | NA | NA | Cat 2 | NA | NA | 0476 | TJC | |
| Appropriate DVT Prophylaxis in Women Undergoing Cesarean Delivery | NA | NA | Cat 2 | NA | NA | 0473 | Hospital Corporation of America | |
| Experience of Mother with Pregnancy Care | NA | NA | Cat 2 | NA | NA | TBD | ||
| Hepatitis B Vaccine Coverage Among All Live Newborn Infants Prior to Hospital or Birthing Facility | NA | NA | Cat 2 | NA | NA | 0475 | Centers for Disease Control and Prevention | |
| Intrapartum Antibiotic Prophylaxis for Group B Streptococcus (GBS) | NA | NA | Cat 2 | NA | NA | 1746 | Massachusetts General Hospital | |
| Monitoring and Reporting of NICU Admission Rates | NA | NA | Cat 2 | NA | NA | TBD | ||
| Postpartum Blood Pressure Monitoring | Cat 2 | TBD | ||||||
| Vaginal Birth After Cesarean (VBAC) Delivery Rate, Uncomplicated | Cat 2 | AHRQ | ||||||
| Health and Recovery Program (HARP) | ||||||||
| Health and Recovery Program (HARP) | ||||||||
| Adherence to Mood Stabilizers for Individuals with Bipolar I Disorder | NA | NA | NA | Cat 2 | NA | 1880 | CMS | |
| Mental Health Engagement in Care – 30 Days | NA | NA | NA | Cat 2 | NA | |||
| Percentage of HARP Enrolled Members Who Received Personalized Recovery Oriented Services (PROS) or Home and Community Based Services (HCBS) | NA | NA | NA | Cat 2 | NA | NYS 2019 | ||
| HIV/AIDS | ||||||||
| Diabetes Screening | NA | NA | NA | NA | Cat 2 | NYS DOH AIDS Institute | ||
| Hepatitis C Screening | NA | NA | NA | NA | Cat 2 | HRSA | ||
| Housing Status | NA | NA | NA | NA | Cat 2 | HRSA | ||
| Linkage to HIV Medical Care | NA | NA | NA | NA | Cat 2 | NYS 2019 | ||
| Prescription of HIV Antiretroviral Therapy | NA | NA | NA | NA | Cat 2 | HRSA | ||
| Sexual History Taking: Anal, Oral, and Genital | NA | NA | NA | NA | Cat 2 | NYS DOH AIDS Institute | ||
| Substance Abuse Screening | NA | NA | NA | NA | Cat 2 | HRSA | ||
Table 4. 2019 VBP MLTC Category 2 Measures
| Measures | Notes | Arrangement Type | Measure source/Steward |
|---|---|---|---|
| MLTC | |||
| Percentage of long stay high risk residents with pressure ulcers | 1, 2 | Cat 2 | MDS 3.0 + /CMS |
| Percentage of long stay residents who received the pneumococcal vaccine | 1, 2 | Cat 2 | MDS 3.0/CMS |
| Percentage of long stay residents who received the seasonal influenza vaccine | 1, 2 | Cat 2 | MDS 3.0/CMS |
| Percentage of long stay residents experiencing one or more falls with major injury | 1, 2 | Cat 2 | MDS 3.0/CMS |
| Percentage of long stay residents who lose too much weight | 1, 2 | Cat 2 | MDS 3.0/CMS |
| Percentage of long stay residents with a urinary tract infection | 1, 2 | Cat 2 | MDS 3.0/CMS |
| Care for Older Adults – Medication Review | Cat 2 | NCQA | |
| Use of High–Risk Medications in the Elderly | Cat 2 | NCQA | |
| Percentage of long stay low risk residents who lose control of their bowel or bladder | 1, 2 | Cat 2 | MDS 3.0/CMS |
| Percentage of long stay residents whose need for help with daily activities has increased | 1, 2 | Cat 2 | MDS 3.0/CMS |
| Percentage of members who rated the quality of home health aide or personal care aide services within the last 6 months as good or excellent | 3 | Cat 2 | MLTC Survey/New York State |
| Percentage of members who responded that they were usually or always involved in making decisions about their plan of care | 3 | Cat 2 | MLTC Survey/New York State |
| Percentage of members who reported that within the last 6 months the home health aide or personal care aide services were always or usually on time | 3 | Cat 2 | MLTC Survey/New York State |
| Percentage of long stay residents who have depressive symptoms | 1, 2 | Cat 2 | MDS 3.0/CMS |
| Percentage of long stay residents with dementia who received an antipsychotic medication | 1, 2 | Cat 2 | MDS 3.0/Pharmacy Quality Alliance |
| Percentage of long stay residents who self–report moderate to severe pain | 1, 2 | Cat 2 | MDS 3.0 + /CMS |
1 – Included in the NYS DOH Nursing Home Quality Initiative measure set
2 – MDS 3.0 denotes the Centers for Medicare and Medicaid Services Minimum Data Set for nursing home members
3 – Included in the NYS DOH MLTC Quality Incentive measure set
Follow Us