Health Plans, Providers, and Professionals
- MLTC Policy 23.02 is also available in Portable Document Format
Office of Health Insurance Programs
Division of Health Plan Contracting and Oversight
Managed Long Term Care Policy 23.02: Coordination of Hospice Services
Date of Issuance: June 15, 2023
Effective Date: June 15, 2023
Includes: Attachment 1 - Hospice Care Recipient RR/E Code Update Form
The purpose of this policy is to provide Medicaid Managed Care Organizations (MMCO) guidance and instructions regarding coordination of hospice services. Adherence to this policy is necessary to identify a New York State (NYS) Medicaid recipient’s hospice participation to prevent duplication of services that are included in Medicare hospice and certain Managed Long Term Care (MLTC) products. As a reminder, certain hospice services are covered outside of the MLTC Partial and Medicaid Advantage Plus (MAP) benefit packages through fee-for-service.
Identifying Medicaid Recipients in Receipt of Hospice Care
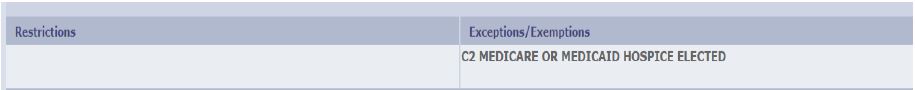
A new Recipient Restriction/Exception (RR/E) code, C2-HOSPICE-MM, has been established to identify Medicaid recipients who elect to receive hospice care. The C2 RR/E code is systematically added to a dual eligible Medicaid recipient’s record and returned on the ePACES eligibility response and also on the 834 file when a hospice election period is received on the Medicare Modernization Act (MMA) file.
The MMA file includes Medicare Parts A, B, C, and D eligibility and enrollment data including the hospice election date period. For non-dual Medicaid recipients, the C2 R/E code needs to be manually added to the recipient’s record.
If the MMCO becomes aware of a dual or non-dual Medicaid recipient receiving hospice care, the MMCO must verify that the recipient’s eMedNY file appropriately indicates that the recipient is in receipt of hospice care. If it does not, the MMCO is to request that DOH add the C2 R/E code. This is achieved by completing Attachment 1 and sending it to hospicebilling@health.ny.gov via a HIPAA compliant email with the subject: Hospice C2 R/E Code Needed MMCO.
If the MMCO becomes aware that a dual or non-dual Medicaid recipient has withdrawn their hospice election, the MMCO must verify that the C2 R/E code Thru Date in eMedNY coincides with the end date of their hospice election, i.e., it is not “12/31/9999” but is the actual date the hospice election ends. If it has not been end-dated, or the end date is “12/31’9999”, the MMCO must complete Attachment 1 and send it to hospicebilling@health.ny.gov via a HIPAA compliant email with the subject: Hospice End-Date Needed MMCO.
Medicaid fee-for-service recipients in receipt of hospice services are excluded from enrolling in Medicaid managed care including Mainstream, Health And Recovery Plans (HARP), HIV Special Needs Plan, MLTC Partial Capitation, Medicaid Advantage Plus (MAP), Programs for All-Inclusive Care for the Elderly (PACE), and Fully Integrated Duals Advantage for Individuals with Intellectual and Developmental Disabilities (FIDA-IDD).
Medicaid managed care enrollees, excluding PACE enrollees, who elect to receive hospice care may remain enrolled in the managed care plan of their choice for the duration of their hospice election.
Coordination of Hospice Services
When a Medicaid managed care recipient is in receipt of hospice services, the MMCO is responsible for coordinating services and financial obligations with the hospice provider, particularly for personal care/consumer directed personal assistance services (CDPAS) and Durable Medical Equipment and supplies. To assist in this coordination, DOH issued DHCBS 22-15 instructing hospice providers to complete form DOH-5778, Entity/Facility Notification of Hospice Non-Covered Items, Services, and Drugs, and to share it with other healthcare providers, Local Departments Social Services, and MMCOs, and those from whom the hospice recipient may seek items, services, or drugs.
MMCOs must:
- Ensure receipt of DOH-5778 from the hospice provider, documenting in their records when DOH-5778 was received.
- Incorporate the DOH-5778 into their records for appropriate care planning throughout the duration of treatment and be able to provide the form upon request of DOH and/or other entities (e.g., the Office of the Medicaid Inspector General, Centers for Medicare and Medicaid Services, etc.) for purposes of audit and/or surveillance to ensure there are no overlaps in services.
- Document in their progress/case notes the reason a service is provided outside of the hospice benefit (e.g., diagnoses, medical conditions) not related to the recipient's terminal illness.
Questions
Questions related to this guidance document may be sent to hospicebilling@health.ny.gov.
Follow Us