MLTC Policy 24.02: Updated Resumption of MLTC Involuntary Disenrollment Guidance
- MLTC Policy 24.02 is also available in Portable Document Format
Office of Health Insurance Programs
Division of Health Plan Contracting and Oversight
Managed Long Term Care (MLTC) Policy 24.02: Updated Resumption of MLTC Involuntary Disenrollment Guidance
Date of Issuance and Revision: September 3, 2024
Effective Date: November 1, 2024
NOTE: This MLTC Policy 24.02 updates and replaces MLTC Policy 23.03 - Resumption of MLTC Involuntary Disenrollment Guidance, by adding within Section B. Mandatory Involuntary Disenrollment Reasons, the new reason: xi. Enrollee refused to cooperate or was unable to be reached to complete the required assessment. Completed evidence packets may be submitted to NYMC for this new reason, the earliest, beginning October 3, 2024, for November 1, 2024 effective dates, and thereafter.
Purpose: The purpose of this policy is to provide guidance and instructions on the Managed Long Term Care (MLTC) Involuntary Disenrollment process. Effective November 1, 2023, MLTC plans, including Partial Capitation (MLTCP), Programs of All-Inclusive Care for the Elderly (PACE), and Medicaid Advantage Plus (MAP) plans must follow the below guidance for the acceptable and resumed involuntary disenrollment reasons. Section B, new reason xi, is effective November 1, 2024.
Introduction: In March 2020, the Families First Coronavirus Response Act instituted flexibilities to suspend some Medicaid disenrollment reasons for Medicaid managed care enrollees during the Public Health Emergency (PHE). In November 2020, the Centers for Medicare and Medicaid Services (CMS) rulemaking allowed states to resume some involuntary disenrollments as long as comparable coverage was maintained. On October 1, 2021, January 1, 2022, and July 1, 2022, the New York State Department of Health (the Department) resumed select involuntary disenrollment reasons in the MLTC program. With the end of the Continuous Enrollment Condition authorized by the Families First Coronavirus Response Act, effective March 2023, the Department is beginning the PHE unwind process including the resumption of the involuntary disenrollment of MLTC enrollees per the MLTC model contract requirements. Any previous involuntary disenrollment guidance is superseded by this MLTC Policy 24.02 document.
The policy does not include the involuntary disenrollments that result from a Medicaid discontinuance. Local Department of Social Services (HRA/LDSS) initiated disenrollment reasons include instances where the Enrollee is no longer eligible for Medicaid, the Enrollee is deceased, the Enrollee is incarcerated, etc.
Note: The Involuntary Disenrollment Reason Table (Appendix 3) summarizes the involuntary disenrollment reasons, required supporting documentation, and disenrollment outcomes specified in Section B and Section C of this Policy.
A. Mandatory vs. Optional Involuntary Disenrollment
A plan initiated MLTC involuntary disenrollment is a disenrollment initiated by the MLTC plan without agreement from the Enrollee when that Enrollee no longer meets the conditions for enrollment. The plan-initiated involuntary disenrollment requests must be submitted to New York Medicaid Choice (NYMC), the Department's managed care enrollment broker. The involuntary disenrollment process is initiated when the plan sends the Enrollee the Intent to Disenroll letter (Appendix 1) as the first step and then the plan submits a completed Managed Long Term Care Involuntary Disenrollment Request Form (Appendix 2) to NYMC.
There are two types of involuntary disenrollments, mandatory or optional:
- A mandatory involuntary disenrollment is a required action that the plan MUST take following a specific triggering event. Based on the circumstances of the triggering event, if an Enrollee does not request or agree to disenroll from the plan, the plan MUST initiate an involuntary disenrollment within five (5) business days of the date the plan is notified of the triggering event.
- An optional involuntary disenrollment is an action where under limited circumstances the plan MAY initiate an involuntary disenrollment.1
B. Mandatory Involuntary Disenrollment Reasons:
- Enrollee no longer resides in the Plan's service area.
- This reason is applicable to all MLTC plan types. The plan is required to initiate the involuntary disenrollment process within five (5) business days of notification that the Enrollee no longer resides in the plan's service area. The plan must submit the Managed Long Term Care Involuntary Disenrollment Request Form to NYMC with the new address and include dates of when HRA/LDSS was notified of the new address.
- Also, the plan must immediately notify the HRA/LDSS of the new residential address when the plan has verified that an Enrollee has moved out the plan's service area.
- Note: The enrollee's residential address must be updated by the HRA/LDSS in order for the disenrollment/transfer to be processed by NYMC. If the involuntary disenrollment is disregarded by NYMC (as listed on the NYMC D File) because the address has not been updated, the plan must resubmit the involuntary disenrollment after the address is updated.
- For approved involuntary disenrollment requests for this reason, mandatory enrollees will be notified by NYMC that they may transfer to another MLTC plan in the county where they now reside. Eligible enrollees who do not choose a plan will be auto assigned to a new MLTCP in the new service area. Those enrollees who are not eligible for MLTC, will be disenrolled to Medicaid fee-for-service (FFS).
- >Enrollee has been absent from the Plan's service area for more than 30 consecutive days.
- This reason is applicable to all MLTC plan types. The plan is required to initiate the involuntary disenrollment process with NYMC within five (5) business days of notification that the Enrollee has been absent from the plan's service area (i.e., visiting family in another state) for more than thirty (30) consecutive days.
- Before initiating the involuntary disenrollment process, the plan is required to make five (5) reasonable attempts (as described below) to contact the Enrollee and document the status in the monthly Care Management record. The record should reflect any services received during this period. Upon a successful contact with the Enrollee and/or their designee, the plan must inform the Enrollee of the disenrollment potential. The plan must advise the Enrollee and/or their designee of the requirement to be in the service area to maintain their membership with the plan. If at any time, the Enrollee self discloses that they will be out of the service area for more than thirty (30) consecutive days, the plan should discuss with the Enrollee, the option of a voluntary disenrollment or a voluntary transfer to another plan. If the plan is unable to contact the Enrollee or if the Enrollee does not request to voluntarily disenroll, the plan is required to proceed with the involuntary disenrollment process.
- Reasonable Attempts to Contact the Enrollee would include:
- Outreach to the Medicaid authorized representative on file
- Visits to the Enrollee's residence of record
- Conducting target outreach to the Enrollee throughout the month
- If no contact was made with Enrollee and/or with their Medicaid authorized representative, the plan must document at least five (5) attempts using at various methods to contact the Enrollee prior to submitting a completed involuntary disenrollment request to NYMC.
- The plan is required to submit a written statement from the Enrollee's Home Care Agency, or other pertinent evidence, that an effort was made to contact the Enrollee including the date of the last contact with the Enrollee. The plan must submit supporting documentation along with the Managed Long Term Care Involuntary Disenrollment Request Form to NYMC.
- For approved involuntary disenrollment requests for this reason, Enrollee will be disenrolled to FFS. The disenrollment confirmation notice will indicate that the Enrollee should contact NYMC to discuss enrollment options that may be available to them.
- Enrollee enters an OMH, OPWDD, OASAS residential program or OMH state operated psychiatric center that is not a MLTC Plan covered benefit for 45 consecutive days or longer.
- This reason is applicable to all MLTC plan types. The plan is required to initiate the involuntary disenrollment with NYMC within five (5) business days from the date the plan knows the Enrollee enters a residential program with the Office of Mental Health (OMH), Office for People with Developmental Disabilities (OPWDD), Office of Addiction Services and Supports (OASAS) or an OMH state operated psychiatric center that is not a MLTC plan covered benefit for forty-five (45) consecutive days or longer. Plans must submit the Managed Long Term Care Involuntary Disenrollment Request Form to NYMC and include the following information:
- Type of Program (OMH, OPWDD, OASAS or OMH state operated psychiatric center)
- Name of Program
- Date of admission
- For approved involuntary disenrollment requests for this reason, the Enrollee will be disenrolled. The disenrollment confirmation notice will indicate that the Enrollee should contact NYMC to discuss enrollment options that may be available to them upon discharge from the residential program. More information on the OMH state operated psychiatric centers are available with Office of Mental Health (OMH) and details on the OMH/OASAS residential program are provided in the New York State MAP Plans Behavioral Health Billing and Coding Manual. Details on the OPWDD residential program can be found here.
- This reason is applicable to all MLTC plan types. The plan is required to initiate the involuntary disenrollment with NYMC within five (5) business days from the date the plan knows the Enrollee enters a residential program with the Office of Mental Health (OMH), Office for People with Developmental Disabilities (OPWDD), Office of Addiction Services and Supports (OASAS) or an OMH state operated psychiatric center that is not a MLTC plan covered benefit for forty-five (45) consecutive days or longer. Plans must submit the Managed Long Term Care Involuntary Disenrollment Request Form to NYMC and include the following information:
- For Partial Capitation plan only, Enrollee is hospitalized for 45 days or longer.
- This reason is applicable to MLTCP plans only. The plan is required to initiate the involuntary disenrollment with NYMC within five (5) business days from the date the plan knows the Enrollee has been hospitalized for forty-five consecutive (45) days or longer and does not have an active discharge plan. MLTC plans must have up-to-date case management notes while the Enrollee is hospitalized and ongoing status of the Enrollee during the hospitalization.
- The plan must submit documentation that includes the name of the hospital and the date of hospital admission. MLTCP plans must submit the Managed Long Term Care Involuntary Disenrollment Request Form to NYMC and include the following information:
- Name of Hospital
- Date of admission
- Enrollee does not have a discharge plan
- For approved involuntary disenrollment requests for this reason, the Enrollee will be disenrolled. The disenrollment confirmation notice will indicate that the Enrollee should contact NYMC to discuss enrollment options that may be available to them upon discharge from the hospital.
- For MAP only, Enrollee is not enrolled in the aligned Medicare Advantage Dual Eligible Special Needs Plan.
- This reason is applicable to MAP plans only. The plan is required to make three (3) reasonable attempts (as described in Section B. Reason ii.) over five (5) business days to contact the Enrollee to inform them that the plan received notification that the Enrollee was no longer enrolled in the aligned Medicare Advantage Dual Eligible Special Needs Plan. Upon a successful contact with the Enrollee and/or their designee, the plan must inform the Enrollee of their disenrollment from the aligned Medicare Advantage Dual Eligible Special Needs Plan. If the Enrollee would like to remain enrolled in the MAP plan, the plan would assist the Enrollee in reinstating the enrollment in the aligned Medicare Advantage Dual Eligible Special Needs Plan to remain aligned in a single Medicare and MAP plan. The MAP plan would not submit an involuntary disenrollment to NYMC in this instance.
- If the Enrollee acknowledges that the Medicare and Medicaid enrollment is not aligned and the Enrollee requests to voluntary disenroll from the MAP plan, the plan is required to initiate the voluntary disenrollment process by submitting a completed voluntary disenrollment form to NYMC. This situation would not be considered an involuntary disenrollment reason.
- If the plan is unable to contact the Enrollee or if the Enrollee does not want to reinstate their Medicare enrollment in the aligned Medicare Advantage Dual Eligible Special Needs Plan, the plan is required to initiate the involuntary disenrollment with NYMC. The involuntary disenrollment package, as defined in Section F, must be submitted within five (5) business days from the date the plan receives notification that the Enrollee was no longer enrolled in the aligned Medicare Advantage Dual Eligible Special Needs Plan. The plan must submit the Managed Long Term Care Involuntary Disenrollment Request Form to NYMC and include the Medicare Disenrollment Date.
- For approved involuntary disenrollment requests for this reason, mandatory enrollees will be notified by NYMC that they may transfer to another MLTC plan. Eligible enrollees who do not choose a plan will be auto assigned to a MLTCP in their service area. Voluntary or exempt enrollees who do not select a new plan, will be disenrolled. The disenrollment confirmation notice will indicate that the Enrollee should contact NYMC to discuss enrollment options that may be available to them.
- For PACE only, Enrollee is not enrolled in the aligned PACE Medicare Health Plan, if applicable.
- This reason is applicable to PACE plans only. The plan is required to make three (3) reasonable attempts (as described in Section A. Reason ii.) over five (5) business days to contact the Enrollee to inform them that the plan received notification that the Enrollee was no longer enrolled in the aligned PACE Medicare Health Plan. Upon a successful contact with the Enrollee and/or their designee, the plan must inform the Enrollee of their disenrollment from the aligned PACE Medicare Health Plan. If the Enrollee would like to remain enrolled in the PACE plan, the plan would assist the Enrollee in reinstating the enrollment in the aligned PACE Medicare Health Plan. The PACE plan would not submit an involuntary disenrollment to NYMC in this instance.
- If the Enrollee acknowledges that the Medicare and Medicaid enrollment is not aligned, and wishes to voluntary disenroll from the PACE plan, the plan is required to submit the Enrollee's voluntary disenrollment request.
- If the plan is unable to contact the Enrollee or if the Enrollee does not want to reinstate the enrollment in the aligned PACE Medicare Health Plan, the plan is required to initiate the involuntary disenrollment with NYMC. The involuntary disenrollment package must be submitted within five (5) business days from the date the plan receives notification that the Enrollee was no longer enrolled in the aligned PACE Medicare Health Plan. The plan must submit the Managed Long Term Care Involuntary Disenrollment Request Form to NYMC and include the Medicare Disenrollment Date.
- For approved involuntary disenrollment requests for this reason, mandatory enrollees will be notified by NYMC that they may transfer to another MLTC plan. Eligible enrollees who do not choose a plan will be auto assigned to a MLTCP in their service area. Voluntary or exempt enrollees who do not select a new plan, will be disenrolled to FFS. The disenrollment confirmation notice will indicate that the Enrollee should contact NYMC to discuss enrollment options that may be available to them.
- For PACE or MAP, an Enrollee is no longer eligible for enrollment because they no longer meet the nursing home level of care based on the assessment tool prescribed by the Department and cannot be deemed eligible.
- This reason is applicable to PACE and MAP plan types. The plan is required to initiate the involuntary disenrollment with NYMC within five (5) business days of a Community Health Assessment (CHA) where the Enrollee was assessed as no longer meeting nursing home level of care.
- Prior to initiating the involuntary disenrollment request, should the plan believe that the absence of continued coverage under the plan would negatively impact the Enrollee's condition and the Enrollee would be reasonably expected to meet the nursing home level of care requirement within the next six months, the plan must submit a deemed eligibility review request to the Department.
- The plan must submit supporting documentation within five (5) business days of the CHA determination. This information should be submitted to the Department at MLTCMDReview@health.ny.gov.
- The supporting documentation must include the CHA and a statement from the plan's Medical Director or clinical staff clearly stating the rationale for deemed eligibility based on the member's chronic condition. Supporting documentation may include but is not limited to medical records, relevant tests, an assessment by specialists, formal and informal supports that may impact the stability of the member's condition in the next six months. The Department reserves the right to request additional supporting documentation including an attestation from the Enrollee's primary care provider. If the deemed eligibility review is approved, the Enrollee's enrollment would continue uninterrupted.
- However, if the deemed eligibility review request is not approved by the Department, the plan is required to initiate the involuntary disenrollment with NYMC within five (5) business days of the deemed eligibility review determination.
- The plan must submit the deemed eligibility review outcome with the Managed Long Term Care Involuntary Disenrollment Request Form to NYMC. The plan must indicate on the form that the Enrollee is not be deemed eligible.
- For approved involuntary disenrollment requests for this reason, mandatory enrollees in the PACE or MAP plans will be notified by NYMC that they may transfer to a MLTCP plan. Eligible enrollees who do not choose a plan will be auto assigned to a MLTCP in their service area. Voluntary or exempt enrollees, who do not select a new plan, will be disenrolled to FFS. The disenrollment confirmation notice will indicate that the Enrollee should contact NYMC to discuss enrollment options that may be available to them.
- Note: Nursing home level of care may be identified at any reassessment.
- For Partial Capitation plan only, a non-dual eligible Enrollee or a dual eligible Enrollee aged 18 to 20 who is no longer eligible for enrollment because the Enrollee no longer meets the nursing home level of care based on the assessment tool prescribed by the Department.
- This reason is applicable to MLTCP plans only and applies to individuals under twenty-one (21).
- The plan is required to initiate the involuntary disenrollment with NYMC within five (5) business days of the comprehensive reassessment.
- Note: Nursing home level of care may be identified at any reassessment.
- The plan must submit the CHA with the Managed Long Term Care Involuntary Disenrollment Request Form to NYMC.
- For approved involuntary disenrollment requests for this reason, the Enrollee will be disenrolled to FFS. The disenrollment confirmation notice will indicate that the Enrollee should contact NYMC to discuss enrollment options that may be available to them.
- Enrollee is no longer eligible for enrollment because the enrollee was assessed as no longer in need of a Community Based Long Term Services and Supports (CBLTSS) for more than 120 days.
- This reason is applicable to all MLTC plan types. The plan is required to initiate the involuntary disenrollment with NYMC within five (5) business days of the comprehensive reassessment.
- The plan must submit the CHA with the Managed Long Term Care Involuntary Disenrollment Request Form to NYMC.
- For approved involuntary disenrollment requests for this reason, the Enrollee will be disenrolled to FFS. The disenrollment confirmation notice will indicate that the Enrollee should contact NYMC to discuss enrollment options that may be available to them.
- Note: New York Independent Assessor Program (NYIAP) CHA Determinations
- Once the reassessments are transferred to NYIAP, there may be circumstances where a plan disagrees with the clinical determination impacting the Enrollee's CBLTSS eligibility. Should the plan disagree with the CBLTSS determination, the plan must initiate the CHA Variance request process by completing the NYIAP CHA Variance Form with supporting documentation as described in MLTC Policy 22.01.
- Enrollee does not receive at least one of the following Community Based Long Term Services and Supports (CBLTSS) within previous month:
- Nursing services in the home
- Therapies in the home
- Home health aide services
- Personal care services in the home (Level 2)
- Adult day health care
- Private duty nursing
- Consumer Directed Personal Assistance Services
- This reason is applicable to all MLTC plan types. The plan is required to initiate the involuntary disenrollment with NYMC within five (5) business days of confirming that the Enrollee has not received CBLTSS within the previous calendar month. The plan must submit all of following documents with the Managed Long Term Care Involuntary Disenrollment Request Form:
- The Intent to Disenroll letter,
- A statement indicating that the Enrollee that has not received at least one of the CBLTSS identified in the Person-Centered Service Plan (PCSP),
- A statement specifying the authorized schedule of services for the Enrollee and the name of the authorized provider of the services, if available; and
- Include in the statement the calendar month in which the Enrollee did not receive CBLTSS following the authorization date.
- If no contact was made with the Enrollee or their authorized representative, the statement must include the reason the Enrollee has not received the services, the specific dates, time, and type of contact attempts made by the plan. The three (3) outreach attempts should be conducted on different days of the week and different times of day.
- The statement must include the safe discharge plan which includes information about any referrals to other providers of applicable services or supports made on behalf of the Enrollee and the status of such referral(s).
- For approved involuntary disenrollment requests for this reason, the Enrollee will be disenrolled to FFS. The disenrollment confirmation notice will indicate that the Enrollee should contact NYMC to discuss enrollment options that may be available to them.
- Examples: When to and When Not to Initiate Involuntary Disenrollment when the Enrollee Does Not Receive CBLTSS
- The following are examples of instances in which a plan must initiate involuntary disenrollment due to lack of Enrollee receiving CBLTSS within previous calendar month:
- An Enrollee chooses not to receive plan services because family or other natural supports are providing the needed assistance, and the Enrollee does not agree to voluntarily disenroll.
- The plan identifies that the Enrollee is not receiving services, and the plan has been unable to communicate with the Enrollee despite three (3) reasonable attempts (as described in Section B. Reason ii.) over five (5) business days.
- Per MLTC Policy No. 13.03, 13.05, and 13.11, the Enrollee has been identified as only receiving Social Adult Daycare (SADC) services. Note: The need for SADC services alone does not meet the eligibility criteria to remained enrolled in a MLTC plan. Enrollees must need a CBLTSS in addition to SADC to remain enrolled in a MLTC plan. MLTC enrollees who are disenrolled to FFS will not be able to access the SADC service.
- Per MLTC Policy No. 13.15, the Enrollee has been assessed as needing only discreet level 1 housekeeping services.
- The following are examples of instances in which a plan would not initiate involuntary disenrollment due to the Enrollee not receiving CBLTSS within previous calendar month:
- Nursing services in the home is the only service in the Enrollee's plan of care, and the scheduled frequency results in no scheduled nursing service within previous calendar month.
- An Enrollee has been assessed to need personal care or personal assistance, but the plan is unable to locate an in-network provider to furnish the service and is working to find an out-of-network provider to furnish services.
- Enrollee is hospitalized during the calendar month that the Enrollee was identified as not receiving CBLTSS.
- The following are examples of instances in which a plan must initiate involuntary disenrollment due to lack of Enrollee receiving CBLTSS within previous calendar month:
- Enrollee refused to cooperate or was unable to be reached to complete the required assessment.
- This reason is applicable to all MLTC plan types. The plan is required to initiate the involuntary disenrollment with NYMC within five (5) business days of exhausting all efforts to gain the Enrollee's cooperation with completing the required assessment (the mandatory annual assessment or significant change in condition assessment, if needed). Enrollees, whether auto-assigned, passively, or voluntarily enrolled, are subject to be involuntarily disenrolled if the Enrollee refuses an assessment after any applicable continuity of care period.
- The plan must submit the following required documentation:
- A statement detailing all efforts used to gain the Enrollee's cooperation with scheduling and completing the required assessment.
- A statement detailing at least ten (10) outreach attempts over the course of thirty (30) calendar days to schedule and complete the required assessment. The outreach attempts must be conducted on different days of the week and different times of day. There must be at least two (2) visits to the Enrollee's home which may include the utilization of existing providers as outlined below.
- A statement demonstrating how the plan worked with the Enrollee's existing providers to educate the Enrollee and gain cooperation to schedule and complete the required assessment. Plans must document which providers were engaged including but not limited to the Enrollee's Personal Care Agency, the Fiscal Intermediary, primary care physician and other providers that render services to the Enrollee in the community.
Note: Member education must include an explanation that the assessment is required to continue plan eligibility and enrollment and that services could be discontinued. Enrollees who are involuntarily disenrolled for this reason must meet current MLTC program enrollment criteria upon re-enrollment, which may include a new NYIAP assessment. - In the event that the member has an authorized or designated representative that assists in making decisions, the plan must include outreach to the authorized or designated representative in at least five (5) of the ten (10) outreach attempts.
Each of the attempts must have a documented outcome of the attempts to reach, schedule and complete the required assessment.- For example: Contacted the member at (123) 456-7891 and the member is ill. Advised that we will attempt to reschedule once the member is well. The case record must be updated with the current status of when a follow up outreach attempt will be made.
- For example: Contacted the member at (123) 456-7891 and the member said that they do not want an assessment and their health has not changed since the last assessment. Member wants to continue the plan of care without having to complete the required assessment. Educated the member that the assessment is a requirement for continued enrollment. The member declined to schedule the assessment.
- The outcome of each outreach attempt must be documented in the case record. As a reminder, there must be ten (10) outreach attempts to the Enrollee including five (5) outreach attempts to the authorized or designated representative, if applicable.
- The plan must submit the following documents with the Managed Long Term Care Involuntary Disenrollment Request Form:
- The Intent to Disenroll letter; and
- The required documentation outlined above including the required statements.
C. Optional Involuntary Disenrollment Reasons
- Enrollee or an Enrollee's family member or other person in the home engages in behavior that seriously impairs the Plan's ability to furnish services for reasons other than those resulting from the Enrollee's special needs.
- This reason is applicable to all MLTC plan types. The plan may initiate an involuntary disenrollment with NYMC if the Enrollee or an Enrollee's family member or other person in the home engages in conduct or behavior that seriously impairs the plan's ability to furnish services to either that particular Enrollee or other Enrollees. The plan must have made and documented reasonable efforts (as described in Section B. Reason ii.) to resolve the problems presented by the involved individual(s).
- The plan must submit the Managed Long Term Care Involuntary Disenrollment Request Form to NYMC with all of the required supporting documentation, which includes:
- The plan's written statement describing the case situation and why the plan is unable to furnish services.
- The names of different home care agencies utilized, and the results of service attempts.
- Documentation of a referral to Adult Protective Services (APS) must be included when there is a report of safety issues.
- For approved involuntary disenrollment requests for this reason, mandatory enrollees will be notified by NYMC that they may transfer to another MLTC plan. Eligible enrollees who do not choose a plan will be auto assigned to a MLTCP in their service area. Those enrollees who are not eligible for MLTC, will be disenrolled to FFS. The disenrollment confirmation notice will indicate that the Enrollee should contact NYMC to discuss enrollment options that may be available to them.
D. Enrollee Contacts the Plan or NYMC to Continue the Enrollment
After receiving an Intent to Disenroll letter or an involuntary disenrollment notice, an Enrollee may contact the plan or NYMC to request to continue an existing enrollment. The enrollment in the plan can continue in the following scenarios, provided that all requirements are met:
- Enrollee has been absent from the Plan's service area or has not received CBLTSS.
- The Enrollee must return to the service area, prior to the disenrollment effective date, or requests to reinstate their PCSP. The plan must document the continued enrollment request as an occurrence in the monthly Care Management record including any changes to the existing PCSP.
- Enrollee enters a residential program or is hospitalized for 45 consecutive days or longer.
- The enrollment in the plan can continue if the Enrollee has returned to a community setting or has an active discharge plan with an expected discharge date, prior to or near the disenrollment effective date. The plan must document the active discharge plan or the return to the community setting as an occurrence in the monthly Care Management record.
- A MAP or PACE Enrollee is not enrolled in the aligned Medicare Plan
- The enrollment in plan can continue if, prior to the disenrollment effective date, the Enrollee reenrolls in the aligned Medicare plan.
The Enrollee may contact the plan or NYMC, stating that they have met the requirements to remain in the plan. NYMC, if contacted, will initiate a three-way call to notify the plan of the Enrollee's request to continue the enrollment. The plan must verify that the Enrollee has satisfied the conditions described in Section D. according to the relevant scenario. Upon verification, the plan must immediately submit a request to withdraw the disenrollment to NYMC Health Plan Affairs team if the disenrollment has not been processed.
In the instance where NYMC has processed the disenrollment, the plan must submit a new enrollment transaction via the U-file submission for the next enrollment effective date.
The plan must provide an updated enrollment notice to the Enrollee when the enrollment is reinstated. If NYMC has sent a disenrollment notice, NYMC is responsible for noticing the Enrollee that their coverage will continue.
However, if the request to continue the enrollment is received after the disenrollment effective date, a new enrollment application must be completed. The existing CHA on file may be used if it is not valid.
- The enrollment in plan can continue if, prior to the disenrollment effective date, the Enrollee schedules and completes the required assessment.
Enrollee has refused a required assessment.
The Enrollee may contact the plan or NYMC, stating that they have met the requirements to remain in the plan. NYMC, if contacted, will initiate a three-way call to notify the plan of the Enrollee's request to continue the enrollment. The plan must verify that the required assessment was completed by the Enrollee. Upon verification, the plan must immediately submit a request to withdraw the disenrollment to NYMC Health Plan Affairs team if the disenrollment has not been processed.
In the instance where NYMC has processed the disenrollment, the plan must submit a new enrollment transaction via the U-file submission for the next enrollment effective date.
The plan must provide an updated enrollment notice to the Enrollee when the enrollment is reinstated. If NYMC has sent a disenrollment notice, NYMC is responsible for noticing the Enrollee that their coverage will continue.
However, if the request to continue the enrollment is received after the disenrollment effective date, a new enrollment application must be completed. The existing CHA on file may be used if it is valid.
E. ON HOLD. Involuntary Disenrollment Reasons
The Department is finalizing guidance on the below reasons for involuntary disenrollment; therefore, MLTC plans should not submit an involuntary disenrollment package for the below reasons until further guidance is issued:
- Enrollee knowingly provides false information, otherwise deceives the plan, or engages in fraudulent conduct with respect to any substantive aspect of their plan membership. Applicable to all MLTC plan types. This reason is on hold until further guidance from the Department.
- Enrollee fails to pay spenddown fee or Net Available Monthly Income (NAMI) within 30 days after such amount comes due. Applicable to all MLTC plan types. This reason is on hold until further guidance from the Department.
- MLTCP Enrollee is in a long term nursing home stay for more than three (3) months. For Enrollees in a Partial Capitation plan who have reached the three (3) month nursing home benefit limit, the Department will continue to initiate the involuntary disenrollments on behalf of the MLTCP via a batch disenrollment cycle until the end of 2024. Partial Capitation plans will continue to receive the communication and response due dates from the Department for each cycle to involuntarily disenroll Enrollees who have reached their nursing home limit until future guidance is from the Department.
F. Process for Involuntary Disenrollments
The involuntary disenrollment process is initiated when the plan sends the Enrollee an Intent to Disenroll letter as the first step. The plan then submits a completed Managed Long Term Care Involuntary Disenrollment Request Form to NYMC with all of the required supporting documentation for the associated involuntary disenrollment reason.
As part of the resumption of all involuntary disenrollments, the plan must send the approved Intent to Disenroll letter to all Enrollees and their authorized representatives for whom it requests disenrollment. The plan must send this letter prior to submitting a completed involuntary disenrollment request to NYMC. The plan must include a copy of the Intent to Disenroll letter, along with the required supporting documentation for each reason in the involuntary disenrollment package described below.
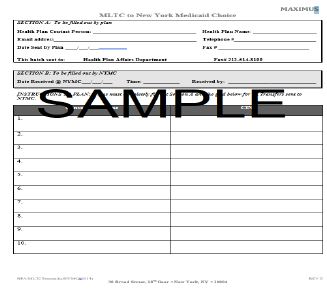
The plan must submit an involuntary disenrollment package to the NYMC Health Plan Affairs Department via the NYMC secure portal, MoveIT. The package must include the following:
A completed Managed Long Term Care Involuntary Disenrollment Request Form,
The required supporting documentation for the selected disenrollment reason,
The Intent to Disenroll letter, and
The transmittal form requested from NYMC
The involuntary disenrollment package must be submitted within the required timeframe provided in the MLTC Involuntary Disenrollment Processing Schedule for the next available effective date. To avoid processing delays, the plan is advised not hold the submission of the completed involuntary disenrollment package until the deadline.
NYMC will issue the "D File" to each MLTC plan for all submitted involuntary disenrollment requests. The "D file" is a daily file provided by NYMC and contains the status of a plan's involuntary disenrollment request including approved, disregarded, and overturned involuntary disenrollment outcomes. In the case of disregarded or overturned involuntary disenrollment, the Enrollee will remain enrolled in the plan. Plans must review the "D File" to ensure the Enrollee's continuity of care. The plan must review errors with the involuntary disenrollment package and resubmit the package as appropriate.
The plan will be notified of disenrollments via the eMedNY 834 TERM File. MLTCP plans will also be notified of auto assigned enrollments for individuals that are mandatory via the eMedNY 834 ADD File. The eMedNY 834 ADD file is sent to the receiving plan when a disenrollment results in a transfer to a MLTCP, thereby a new enrollment. More information on the Department's roster files of all enrollment changes can be found at https://www.emedny.org/HIPAA/5010/index.aspx. Please see Appendix 3 for the involuntary disenrollment reasons that result in a transfer to a MLTCP.
The involuntary disenrollment process will continue on a monthly basis. The date of the disenrollment depends on the date the disenrollment request is received by NYMC and accepted per the NYMC Disenrollment Processing Schedule.
NYMC REMAINING DISENROLLMENT PROCESSING SCHEDULE FOR 2024
| Plan Submission Window | Disenrollment Effective Date |
|---|---|
| 8/12/2024 - 9/9/2024 | 10/1/2024 |
| 9/10/24 - 10/7/2024 | 11/1/2024 |
| 10/8/2024 - 11/6/2024 | 12/1/2024 |
| 11/7/2024 - 12/9/2024 | 1/1/2025 |
Note: NYMC will provide the involuntary disenrollment schedule separately.
Individuals will be notified of their involuntary disenrollment by NYMC via an Involuntary Disenrollment Notice. Fair Hearing rights apply to this notice from NYMC including Aid to Continue. The involuntary disenrollment notice has contact information if the individual has questions regarding the disenrollment. Individuals who are disenrolled from their MLTC plan will continue the existing Medicaid coverage period through another managed care plan or FFS.
G. Transition of Care Responsibilities
Prior to the effective date of the disenrollment, plans must make any necessary referrals to another plan or the HRA/LDSS for covered and non-covered services based on the disenrollment outcome. The plan must make arrangements to transfer the PCSP to the receiving plan or HRA/LDSS. If the member is auto assigned to a MLTCP plan, the receiving plan should continue the current PCSP until a new PCSP is completed. The new PCSP must be created within fifteen (15) calendar days of the enrollment effective date. This new PCSP should be based on the existing New York Independent Assessor Program CHA, if current. If the Enrollee is due for reassessment, a new CHA should be conducted.
H. Department's Right to Recover Premiums
The resumption of these involuntary disenrollment reasons reinstates the Department's right to recover premiums in instances where the Enrollee was inappropriately enrolled. It is the plan's duty to repay the premiums inappropriately paid on or after the effective date of the involuntary disenrollment reason resumption as updated in this policy. Please be reminded that there were five (5) involuntary disenrollment reasons resumed during the public health emergency on October 1, 2021, January 1, 2022 and July 1, 2022 for which guidance was issued. Any recovery efforts for additional involuntary disenrollment reasons that were on hold during the public health emergency have resumed with the issuance of this guidance.
MANAGED LONG TERM CARE POLICY 24.02
APPENDIX 1
MANAGED LONG TERM CARE INTENT TO DISENROLL TEMPLATE LETTER
<Date>
<Member Name>
<Address>
<City, State> <Zip Code>
Intent to Disenroll Notice
<Member ID.>
<Client Identification Number>
Dear <Member Name>,
This is an important notice about your enrollment in <Plan Name>. We are writing because we have submitted an involuntary disenrollment request to New York Medicaid Choice because <Involuntary Disenrollment Reason>.
What Happens Now
New York Medicaid Choice (NYMC) must review and agree with <Plan Name>'s involuntary disenrollment request. If approved, we expect the disenrollment to be effective by <Anticipated Effective Date>.
We will notify you when your disenrollment is complete. Until that time, we will continue to provide you with the covered services you are now receiving.
What Happens Next
If your involuntary disenrollment is approved by NYMC, you will be provided a disenrollment letter from NYMC which includes fair hearing rights.
{Insert ONLY ONE (1) based on the disenrollment outcome, see Appendix 3.}
[{insert as applicable} <Disenrolled to Fee-for-Service: Once disenrolled, your Medicaid benefits will be continued under Medicaid fee-for-service using your Medicaid card. >
[{insert as applicable} <Mandatory to MLTCP: Once the disenrollment is approved by NYMC, NYMC will contact you to assist you with picking a different Managed Long Term Care plan. >
[{insert as applicable} <Voluntary to MLTCP: Once the disenrollment is approved by NYMC, to continue to receive services, you will need to speak with NYMC to pick a different Managed Long Term Care plan. NYMC will contact you to pick another plan. >
We will work with you to transfer your care to other providers prior to the disenrollment effective date. Your <Care Manager> will call to discuss your transfer plan and preferences for continued care following disenrollment from <Plan Name>.
What You Can Do Now
Share this letter with your family or someone who knows about your health care needs.
Call <Plan Name>. Please call us at <Plan Phone Number>, <Hours of Operation> if you have any questions, if you feel information in this letter is incorrect or wish to work with us to maintain enrollment. For TTY, call <TTY Number>.
insert only ONE (1) based on the involuntary disenrollment needs, see Appendix 3}
[{insert as applicable} Out of the service area: < If you have returned to community and wish to reinstate your service plan, please contact us immediately.>
[{insert as applicable} No CBLTSS: <If you wish to reinstate your service plan, please contact us immediately.>
[{insert as applicable} Hospitalized or in a residential program: <If you have a plan to return to the community or would like assistance in returning to the community, please contact us immediately.>
[{insert as applicable} Unaligned Medicare enrollment: <If you have or will reenroll in the [Insert Plan Name]'s Medicare plan, please contact us immediately.>
[{insert as applicable} Refused Assessment: < If you wish to schedule and complete your assessment, please contact us immediately.>
You can call the Independent Consumer Advocacy Network (ICAN) to get free, independent advice about your coverage, complaint, and appeal options. They can help you manage the appeal process. Contact ICAN to learn more about their services:
Phone: 1-844-614-8800 (TTY Relay Service: 711)
Web: www.icannys.org | Email: ican@cssny.org
<Salutation>
Thank you.
<Notice of Non-Discrimination>
<Multi-Language Insert>
MANAGED LONG TERM CARE POLICY 24.02
APPENDIX 2
MANAGED LONG TERM CARE INVOLUNTARY DISENROLLMENT REQUEST FORM
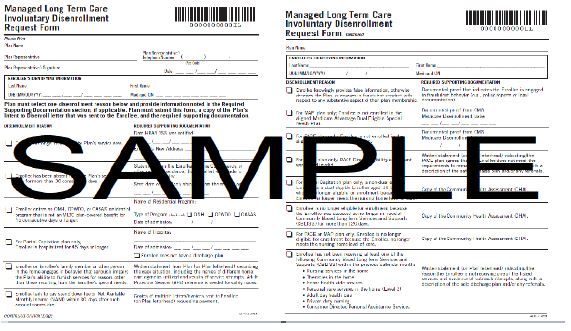
Note: MLTC plans are responsible for requesting the updated MLTC Involuntary Disenrollment Form from NYMC that includes the new reason added in this MLTC Policy 24.02, Section B xi. Enrollee refused to cooperate or was unable to be reached to complete the required assessment, to be submitted to NYMC the earliest, October 3, 2024 for November 1, 2024 effective involuntary disenrollment date or thereafter
Transmittal Form provided by NYMC
MANAGED LONG TERM CARE POLICY 24.02
APPENDIX 3
INVOLUNTARY DISENROLLMENT TABLE
The involuntary disenrollment table identifies:
- The Mandatory or Optional column provides the type of involuntary disenrollment reason.
- The Applies to column indicates the applicable plan types that may involuntarily disenroll an Enrollee for that reason.
- The Involuntary Disenrollment Reason column lists the involuntary disenrollment reason.
- The Required Supporting Documentation column lists the required information that must be provided for that reason.
- The Disenrollment Outcome column explains how the disenrollment is processed based on the enrollee's status (Mandatory, Voluntary or Excluded). More information can be found here.
The involuntary disenrollment table must be used in conjunction or as a supplement to the Involuntary Disenrollment policy.
| Involuntary Disenrollment Reason Table | |||||
|---|---|---|---|---|---|
| Mandatory or Optional | Applies to | Involuntary Disenrollment Reason | Required Supporting Documentation | Disenrollment Outcome | |
| Mandatory Enrollees | Voluntary & Exempt Enrollees | ||||
| Mandatory | All MLTC plan types | The Enrollee no longer resides in the plan's service area |
|
Enrollee must join a different MLTC plan If the Enrollee does not choose a new plan, one of the MLTC Medicaid plans will be selected for the Enrollee |
Enrollee may join a different MLTC plan If the Enrollee does not choose a new plan, the Enrollee will be disenrolled to FFS |
| Mandatory | All MLTC plan types | Enrollee has been absent from the Plan's service area for more than thirty (30) consecutive days |
|
Enrollee is disenrolled to FFS | Enrollee is disenrolled to FFS |
| Mandatory | All MLTC plan types | Enrollee enters an OMH, OPWDD, OASAS residential program or OMH state operated psychiatric center that is not a MLTC Plan covered benefit for 45 consecutive days or longer |
|
Enrollee is disenrolled to FFS | Enrollee is disenrolled to FFS |
| Mandatory | Partial Only | For Partial Capitation plan only, Enrollee is hospitalized for 45 days or longer |
|
Enrollee is disenrolled to FFS | Enrollee is disenrolled to FFS |
| Mandatory | MAP only | For MAP only, Enrollee is not enrolled in the aligned Medicare Advantage Dual Eligible Special Needs Plan |
|
Enrollee must join a different MLTC plan If the Enrollee does not choose a new plan, one of the MLTC Medicaid plans will be selected for the Enrollee |
Enrollee may join a different MLTC plan If the Enrollee does not choose a new plan, the Enrollee will be disenrolled to Medicaid fee-for service |
| Mandatory | PACE only | For PACE only, Enrollee is not enrolled in the associated PACE Medicare Health Plan, if applicable |
|
Enrollee must join a different MLTC plan If the Enrollee does not choose a new plan, one of the MLTC Medicaid plans will be selected for the Enrollee |
Enrollee may join a different MLTC plan If the Enrollee does not choose a new plan, the Enrollee will be disenrolled to FFS |
| Mandatory | MAP and PACE | For PACE or MAP, Enrollee is no longer eligible for enrollment because the Enrollee no longer meets the nursing home level of care, based on the assessment tool prescribed by the Department, and cannot be deemed eligible |
|
Enrollee must join a different MLTC plan If the Enrollee does not choose a new plan, one of the MLTC Medicaid plans will be selected for the Enrollee |
Enrollee may join a different MLTC plan If the Enrollee does not choose a new plan, the Enrollee will be disenrolled to FFS |
| Mandatory | Partial Only | For Partial Capitation plan only, a non-dual eligible Enrollee or a dual eligible Enrollee aged 18 to 20* who is no longer eligible for enrollment because the Enrollee no longer meets the nursing home level of care based on the assessment tool prescribed by the Department. * Applies to individuals under twenty-one (21) |
|
Not applicable | Enrollee is disenrolled to FFS |
| Mandatory | All MLTC plan types | Enrollee is no longer eligible for enrollment because the enrollee was assessed as no longer in need of a Community Based Long Term Services and Supports (CBLTSS) service for more than 120 days |
|
Not applicable | Enrollee is disenrolled to FFS |
| Mandatory | All MLTC plan types | Enrollee knowingly provides false information, otherwise deceives the Plan, or engages in fraudulent conduct with respect to any substantive aspect of their plan membership. Note: This reason will be on HOLD until further notice |
On Hold | On Hold | On Hold |
| Mandatory | All MLTC plan types | Enrollee does not receive at least one of the following Community Based Long Term Services and Supports (CBLTSS) within previous calendar month:
|
|
Enrollee is disenrolled to FFS | Enrollee is disenrolled to FFS |
| Mandatory | All MLTC plan types | Enrollee refused to cooperate or was unable to be reached to complete the required assessment. |
|
Enrollee is disenrolled to FFS | Enrollee is disenrolled to FFS |
| Optional | All MLTC plan types | Enrollee fails to pay spend down fee or Net Available Monthly Income (NAMI) within 30 days after such amount comes due Note: This reason will be on HOLD until further notice |
On Hold | On Hold | On Hold |
| Optional | All MLTC plan types | Enrollee or family member engages in behavior that seriously impairs the Contractor's ability to furnish services for reasons other than those resulting from the Enrollee's special needs |
|
Enrollee must join a different MLTC plan If the Enrollee does not choose a new plan, one of the MLTC Medicaid plans will be selected for the Enrollee |
Enrollee may join a different MLTC plan If the Enrollee does not choose a new plan, the Enrollee will be disenrolled to FFS |
Follow Us