Diabetes Basics
This section provides basic information about prediabetes and diabetes, including diabetes symptoms, types of diabetes, who is at risk for type 2 diabetes, and diabetes diagnosis, complications and treatment.
Click on each box, below, for more information on each topic:
What is Diabetes?
Diabetes is a disease in which blood glucose (blood sugar) levels are above normal. Much of the food we eat is turned into glucose, or sugar, for our bodies to use for energy. The pancreas, an organ that lies near the stomach, makes a hormone called insulin that helps glucose get into the cells of our bodies, where it can be used for energy.
When someone has diabetes, the body either doesn't make enough insulin or can't use its own insulin as well as it should. This causes sugar to build up in the blood. There are two major types of diabetes, type 1 and type 2. Before people develop diabetes, they almost always have prediabetes – blood sugar levels that are higher than normal but not yet high enough to be diagnosed as diabetes.
Diabetes can cause serious health problems called complications, including heart disease, blindness, kidney failure, and lower-extremity amputations. Diabetes is the 8th leading cause of death in the United States. Type 2 diabetes is also associated with obesity.
- For more information on heart disease, visit NYSDOH Cardiovascular Disease
- For more information on obesity, visit NYSDOH Obesity Prevention
Diabetes Symptoms
The symptoms of diabetes may be mild to severe. Some people may not have any symptoms at all. People who are concerned that they might have diabetes should talk to their doctor or health care provider to find out how to get tested to learn if they have diabetes.
People may have SOME or NONE of the most common symptoms of diabetes:
- Increased thirst
- Increased hunger
- Having to urinate more often – especially at night
- Feeling very tired
- Weight loss
- Blurry vision
- Sores that do not heal
- Tingling/numbness in the hands and feet
Types of Diabetes
Type 1 Diabetes
Type 1 diabetes usually appears in children, teenagers, or young adults under the age of 30, but it can also be diagnosed later in life. About 5% of people with diabetes have type 1 diabetes.
In type 1 diabetes, the body does not produce insulin. During eating, the body breaks down the sugars and starches eaten into a simple sugar called glucose, which the body uses for energy. Insulin is a hormone that the body needs to get glucose from the bloodstream into the cells of the body. When the body does not make insulin, sugars build up in the blood. This is why many people refer to diabetes as "sugar."
People with type 1 diabetes must take insulin every day to live. Insulin is usually given by a shot or a small pump that is attached to the body. For more information, visit the American Diabetes Association's (ADA) website at: Insulin and Other Injectables
Type 1 diabetes cannot be prevented, but it can be controlled by keeping the level of glucose (sugar) in the blood within a normal range. Keeping blood sugar at an ideal level helps prevent problems or complications and helps people feel better every day.
People with diabetes should talk to their doctor or health care provider to find out how to test their blood sugar and how often, and what their healthy blood sugar range should be. For most people with diabetes, a healthy range is between 80 and 130 mg/dl before meals and less than 180 mg/dl at 1 to 2 hours after a meal.
Type 2 Diabetes
About 95% of people with diabetes have type 2 diabetes, making it the most common type of diabetes. In type 2 diabetes, the body either doesn't make enough insulin or can't use its own insulin as well as it should.
While its cause is unknown, type 2 diabetes has been associated with obesity, genetic risk factors, and inactivity. Although type 2 diabetes can be prevented, there is no known way to cure it once someone has it. Type 2 diabetes can be controlled by keeping the level of sugar in the blood within a normal range.
People with type 2 diabetes should talk with their doctor or health care provider to find out what their healthy blood sugar range should be and test their blood sugar levels on a regular basis. According to the American Diabetes Association (ADA), for most people with diabetes, a healthy range is between 80 and 130 mg/dl before meals and less than 180 mg/dl at 1 to 2 hours after a meal.
Who is at Risk for Type 2 Diabetes?
Type 2 diabetes is the most common form of diabetes. In type 2 diabetes, the body either doesn't make enough insulin or can't use insulin as well as it should. The cause of type 2 diabetes is largely unknown, but several risk factors have been associated with the disease.
Risk factors for type 2 diabetes include:
- Age (greater than age 45)
- Overweight or obesity
- A family history of diabetes
- Being physically active less than three times a week
- Family background that is American Indian, African American, Hispanic/Latino, Asian American, or Pacific Islander
- Having had a baby that weighed more than 9 pounds or a history of diabetes while pregnant (gestational diabetes)
- Prediabetes
- History of polycystic ovary syndrome (PCOS)
It is important for people at risk for type 2 diabetes to discuss with their doctor or health care provider how to get tested for diabetes.
Think you or a loved one might be at risk for type 2 diabetes? Take the online risk test.
Gestational Diabetes and Pregnancy
Gestational (pronounced jess-tay-shun-ul) diabetes is a type of high blood glucose or sugar that only happens during pregnancy. If a woman has high blood sugar when she's pregnant, but she never had high blood sugar before, she has gestational diabetes. When someone has diabetes, the body cannot use the sugars and starches (carbohydrates) it takes in as food to make energy. As a result, they have extra sugar in their blood. Between 2 to 10% of U.S. pregnancies are affected by the condition every year, making it a top health concern for pregnant women.
Gestational diabetes can cause problems for mothers and babies if not treated.
For mothers, these problems include:
- High blood pressure during pregnancy
- Difficult delivery
- Risk for Cesarean Section (C-Section)
- An extra-large baby
For babies, these problems include:
- Low blood sugar levels right after birth
- Breathing problems
Gestational diabetes is easily treatable, and can be controlled. Getting treatment greatly reduces health problems for mother and baby. Most of the time, gestational diabetes goes away after the baby is born. However, women who have had gestational diabetes are more likely to develop type 2 diabetes later in life and experience gestational diabetes again in future pregnancies.
Women who have had gestational diabetes need to be tested for type 2 diabetes immediately after the baby is born, and then every one to two years thereafter.
To learn more about gestational diabetes, view the CDC Diabetes and Pregnancy brochure (PDF).
Who is at Risk for Gestational Diabetes?
Gestational diabetes is a type of diabetes that develops only during pregnancy. Diabetes means that blood glucose, also called blood sugar, is too high. The body uses glucose for energy. Too much glucose in the blood is not good for mother or baby.
A diagnosisthe determination of a disease from its signs and symptoms.X of gestational diabetes doesn't mean that someone had diabetes before they were pregnant, or that they will have diabetes after having the baby. Gestational diabetes can be dangerous for both mother and baby. A health care provider will do a blood test to diagnose gestational diabetes between weeks 24 and 28 of the pregnancy.
Risk factors associated with gestational diabetes are:
- Overweight or obesity
- Family history of diabetes
- Family background that is Hispanic Latino, African American, American Indian, Alaska Native, Asian American, or Pacific Islander
- Age (greater than 25)
- History of gestational diabetes, stillbirth or miscarriage, or giving birth to a baby weighing more than 9 pounds
- History of polycystic ovary syndrome (PCOS)
- History of insulin or blood sugar problems, including insulin resistance, glucose intolerance, or prediabetes
- High blood pressure
- High cholesterol
- Heart disease
To learn more about gestational diabetes, view the CDC Diabetes and Pregnancy brochure (PDF).
How is Diabetes Diagnosed?
Diabetes can be diagnosed in any one of three ways:
- 1. Hemoglobin A1C test (A1C)
The A1C test is a blood test that provides information about a person's average levels of blood glucose, also called blood sugar, over the past 3 months. The A1C test is sometimes called the hemoglobin A1C, HbA1c, or glycohemoglobin test and is used to diagnose diabetes. - 2. Fasting plasma glucose test (FPG)
A blood test that measures glucose after a person has not eaten for at least 8 hours. - 3. Oral glucose tolerance test (OGTT)
A blood test that measures glucose after a person has not eaten for 8 hours and 2 hours after that person has had a glucose-containing drink.
The results of any of the above tests can be used to determine whether diabetes or prediabetes is present. Positive tests should be repeated on a different day to be sure the above results are correct.
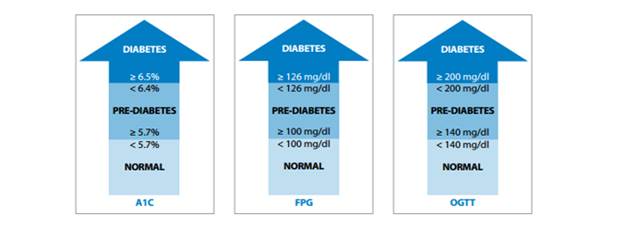
| Test | Normal | Prediabetes | Diabetes |
|---|---|---|---|
| A1C | Less than 5.7% | 5.7% to 6.4% | 6.5% or higher |
| FPG | Less than 100 mg/dl | 100 mg/dl to 125 mg/dl | 126 mg/dl or higher |
| OGTT | Less than 140 mg/dl | 140 mg/dl to 199 mg/dl | 200 mg/dl or higher |
What Complications (Health Problems) are Caused by Diabetes?
If blood sugar is regularly high, over time it can affect the heart, eyes, kidneys, nerves, and other parts of the body. These problems are called complications. Sometimes people with diabetes don't realize that they have the disease until they begin to have other health problems. A health care provider may find signs of diabetes damage even though the patient does not know that he/she has the disease.
Complications of diabetes include:
- Heart Disease– People with diabetes have a higher risk for heart attack and stroke
- Eye Complications– People with diabetes have a higher risk of blindness and other vision problems
- Kidney Disease– Diabetes can damage the kidneys and may lead to kidney failure.
- Nerve Damage (neuropathy) – Diabetes can cause damage to the nerves that run through the body
- Foot Problems– Nerve damage, infections of the feet, and problems with blood flow to the feet can be caused by diabetes
- Skin Complications– Diabetes can cause skin problems, such as infections, sores, and itching. Skin problems are sometimes a first sign that someone has diabetes
- Dental Disease– Diabetes can lead to problems with teeth and gums, called gingivitis and periodontitis
Type 1 Diabetes Treatment and Management
People with type 1 diabetes don't make insulin in their bodies. Insulin helps turn sugar, starches, and other food we eat into energy. People with type 1 diabetes must take insulin every day to live. Insulin is usually given by an injection (shot) or a small pump that is attached to the body. Insulin is not a cure, and people with type 1 diabetes must regularly monitor their blood-sugar level, inject or use insulin through a pump, and carefully balance their insulin doses with eating and daily activities throughout the day and night. For more information about how to stay healthy with type 1 diabetes, visit the American Diabetes Association's website
Some ways to stay healthy with type 1 diabetes are:
- Take insulin and medications as prescribed
- Monitor blood pressure
- Maintain a healthy diet
- Increase physical activity
- Manage blood sugar
- Get an annual (yearly) flu shot
- Get a dental checkup twice a year
- Get a dilated eye exam once a year
Type 2 Diabetes Treatment and Management
Some people with type 2 diabetes can manage their diabetes with healthy eating and living an active lifestyle. However, a health care provider may need to also prescribe oral medications (pills) and/or insulin to help meet target blood sugar levels.
Healthy eating, physical activity, and blood glucose (sugar) testing are the basic therapies for type 2 diabetes. In addition, many people with type 2 diabetes require oral medication, insulin, or both to control their blood sugar levels. Some ways to can stay healthy with type 2 diabetes are:
- Take medications as prescribed
- Monitor blood pressure
- Maintain a healthy diet
- Increase physical activity
- Manage blood sugar
- Get an annual (yearly) flu shot
- Get a dental checkup twice a year
- Get a dilated eye exam once a year
For more information about how to stay healthy with diabetes, visit CDC Stay Healthy/Manage Diabetes
Diabetes Management: Healthy Eating
Eating well to maintain a healthy weight is one of the most important things a person can do to manage diabetes. It can seem hard for people to make healthy food choices, particularly if they are on a budget and short on time. There are some simple steps to help people eat healthier:
- Use a grocery list when shopping for food to help choose more fresh vegetables, fruits, and whole grains
- Buy leaner meats (such as chicken, turkey and lean cuts of pork or beef such as sirloin or round roast) and lower fat dairy products (like low-fator skim milk and yogurt)
- Buy whole grain breads and cereals
- Eat more vegetables, beans, fruits, and whole grains
- Try smaller portions
- Eat less candy, fried foods, canned foods, processed meats, and drink less soda and fruit-flavored drinks
For more tips about how to eat healthy visit NIDDK Making Healthy Food Choices or visit CDC Tasty Recipes for People with Diabetes and their Families
Diabetes Management: Increasing Physical Activity
Being physically active for at least 150 minutes a week helps keep blood sugar in control. It can also relieve stress, strengthen heart muscles and bones, and keep the body and joints flexible. Here are some tips to stay active:
- Try to avoid being physically inactive– some exercise is better than none
- Try moderate-intensity physical activity (such as brisk walking, hiking, swimming, dancing, or gardening) for at least 150 minutes a week
- To build muscle, try doing strength exercises with hand weights, elastic bands, or weight machines
- Engage in the amount and types of physical activity recommended by a health care provider
Diabetes Management: Managing Your Blood Glucose (Sugar)
Blood glucose (sugar) testing is the main way to check diabetes control. Managing diabetes can prevent or slow the progress of manycomplicationsof diabetes, giving a person extra years of a healthy, active life.
Poor control of diabetes can cause symptoms that can affect mental and physical health. During the day, high or low blood sugar can make people feel tired or anxious. Low blood sugar levels can also lead to hunger and eating too much. Low blood sugar at night can disturb sleep. If a person has high blood sugar at night, they may get up often to urinate and then feel tired during the day.
Managing diabetes is hard work, but it's worth it! Take steps today to monitor diabetes, prevent serious complications, and feel better while living with diabetes.
For more information, visit the American Diabetes Association (ADA) website at ADA Checking Your Blood Glucose
Diabetes Self-Management Education and Support
Diabetes Self-Management Education and Support is a process through which people with diabetes can learn and develop skills to help manage their diabetes. New York State Medicaid, Medicare, and most private health insurances include diabetes self-management education (DSME) as a covered benefit.
Talk with your healthcare provider for a referral to a DSME program in your area.
Diabetes Self-Management Program (DSMP)
The Diabetes Self-Management Program (DSMP) developed at Stanford University and now run out of the Self-Management Resource Center (SMRC) is a 6-week workshop for people with type 2 diabetes.
Diabetes and Mental Health
The stress of daily diabetes management can build, so that a person may feel alone or set apart from friends and family because of the extra effort it takes to manage diabetes. Mental health issues, including depression, are common among those with diabetes.
- Many people with diabetes experience mental health issues
- Individuals with type 1 or 2 diabetes are 2 times as likely to be diagnosed with major depressive disorder over their lifespan than those without diabetes
- Depression is treatable even when other illnesses are present
- When people have the support of their family and friends, they can better manage their diabetes
Visit American Diabetes Association: Diabetes and Mental Health or for more information, the National Institute of Mental Health
If someone has diabetes complications such as nerve damage, or has having trouble keeping blood sugar levels normal, they may feel like they're losing control of their diabetes. If a person feels overwhelmed, they should talk to their health care provider to help develop a plan to better manage the stress of living with diabetes.
Diabetes and Disability
People with diabetes of all types are protected as people with qualifying disabilities and have rights and protections. Under most laws, both type 1 and type 2 diabetes are protected as disabilities. For more information on how people with diabetes have rights and protections, visit ADA Is Diabetes a Disability? website
For more information on staying active with a disability, visit Physical Activity and People with Disabilities
Can Type 2 Diabetes Be Prevented?
The good news is that people can prevent or delay type 2 diabetes by:
- Participating in a CDC-recognized diabetes prevention lifestyle change program (NDPP) to learn skills and get resources to help make healthy changes
- Losing small amounts of weight (5 to 7 percent of total body weight)
- Making healthy food choices
- Being more physically active for 150 minutes per week
There are many resources available to help people find out if they are at risk for prediabetes, and to help people with prediabetes prevent or delay diabetes:
- To find out if you or a loved one are at risk for prediabetes, take the online risk test
- Are you a health care provider who wants more information on how to diagnose patients with prediabetes? Visit the American Medical Association and the Centers for Disease Control Prevent Diabetes STAT Toolkit
- CDC Diabetes Prevention Programs
How Can I Find Out if I Have Prediabetes?
Diabetes and prediabetes can only be diagnosed by a health care provider. Diabetes and prediabetes can be diagnosed in any one of these three ways.
- Hemoglobin A1C test (A1C)
A non-fasting blood test that measures the amount of glucose attached to hemoglobin. This test is used to assess blood glucose control over the previous 2-3 months, and has recently been added to the list of tests that may be used to diagnose diabetes. - Fasting plasma glucose test (FPG)
A blood test that measures glucose after a person has not eaten for at least 8 hours. - Oral glucose tolerance test (OGTT)
A blood test that measures glucose after a person has not eaten for 8 hours and 2 hours after that person has consumed a glucose-containing drink.
The results of any of the above tests can be used to determine whether diabetes or prediabetes is present. Positive tests should be repeated on a different day to be sure the above results are correct.
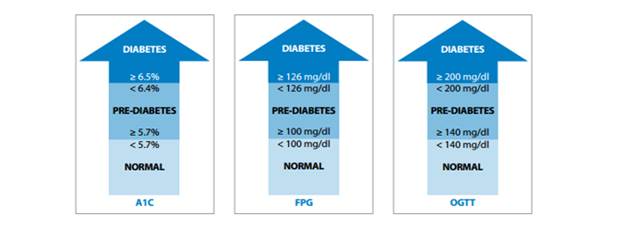
| Test | Normal | Prediabetes | Diabetes |
|---|---|---|---|
| A1C | Less than 5.7% | 5.7% to 6.4% | 6.5% or higher |
| FPG | Less than 100 mg/dl | 100 mg/dl to 125 mg/dl | 126 mg/dl or higher |
| OGTT | Less than 140 mg/dl | 140 mg/dl to 199 mg/dl | 200 mg/dl or higher |