Design and Implementation of Health Homes for Children and Transforming the Delivery of Health Care for Children

Overview for Care at Home I & II Providers
- Slides also available in Portable Document Format (PDF, 2MB)
August 13, 2015
Overview of Today´s Discussion with CAH I & II Providers
- Purpose of Today´s Discussion – Request from CAH Providers for Overall Briefing
- Medicaid Redesign Team (MRT) – Vision and Goal for Transforming the Delivery of Health Care for Children
- Implementation Schedule and Overview of Key Elements of Children´s Health and Behavioral Health Reform Design
- Overview Health Home Model for Children
- Health Homes Designated to Serve Children
- Today and Tomorrow: Changing Landscape and Opportunities for CAH I and II Providers
- Other Health Home for Children Design Features of Interest to CAH I & II Providers
- CANS–NY: Child and Adolescent Needs and Strengths–NY
- Health Home Per Member Per Month Rate and Legacy Rates
- Medicaid Analytics Performance Model (MAPP)
- Health Home Assignment and Referral Process for Children
- Appendix
Medicaid Redesign Team (MRT) – Vision and Goals for Transforming the Delivery of Health Care for Children
Medicaid Redesign Team (MRT)´s Vision, Goals and Principles for Transforming the Delivery of Heath Care for Children
- The Design and Implementation of Health Homes for Children is a component of the Medicaid Redesign Team´s (MRT) Plan to Transform the Delivery of Health Care for children
- MRT is a collaborative partnership among State Agencies, stakeholders, providers and advocates
- Vision and Goals for the Children´s Medicaid Redesign
- ✓ Keep children on their developmental trajectory
- ✓ Focus on recovery and building resilience
- ✓ Identify needs early and intervene
- ✓ Maintain child at home with support and services
- ✓ Maintain the child in the community in least restrictive settings
- ✓ Prevent escalation and longer term need for higher end services
- ✓ Maintain accountability for outcomes and quality
- ✓ Maintain access to services for children without Medicaid as a "Family of One"
Who?
- ✓ Children and youth younger than 21
- ✓ Children with Serious Emotional Disturbance (SED)
- ✓ Children in Foster Care
- ✓ Medically fragile/complex children, require significant medical or technological health supports
- ✓ Youth with Substance Use Disorders
How?
- Multi–faceted Children´s Redesign Plan
- ✓ Increase access to appropriate interventions by enhancing service array available in the continuum of care (Care Management, including Health Homes for Children, State Plan, Home and Community Based Services)
- ✓ Right services, at the right time, in the right amount
- ✓ Expand the number of children that can obtain community based services
(Requires Centers for Medicare and Medicaid (CMS) approvals) - Offer children Medicaid services within a Managed Care delivery system
- ✓ Integrate the delivery of physical and behavioral health services
- ✓ Integrate approaches to care planning and service provision
- ✓ Maintain levels of care (do no harm), ensure continuity of care
- ✓ Increase access to appropriate interventions by enhancing service array available in the continuum of care (Care Management, including Health Homes for Children, State Plan, Home and Community Based Services)
Principles for Serving Children in Managed Care and Health Homes
- Ensure managed care and care coordination networks provide comprehensive, integrated physical and behavioral health care that recognizes the unique needs of children and their families
- Provide care coordination and planning that is family–and–youth driven, supports a system of care that builds upon the strengths of the child and family
- Ensure managed care staff and systems care coordinators are trained in working with families and children with unique, complex health needs
- Ensure continuity of care and comprehensive transitional care from service to service (education, foster care, juvenile justice, child to adult)
- Incorporate a child/family specific assent/consent process that recognizes the legal right of a child to seek specific care without parental/guardian consent
- Track clinical and functional outcomes using standardized pediatric tools that are validated for the screening and assessing of children
- Adopt child–specific and nationally recognized measures to monitor quality and outcomes
- Ensure smooth transition from current care management models to Health Home, including transition plan for care management payments
Implementation Schedule of the Key Elements of Children´s Medicaid Redesign Plan (the "How")
| Anticipated Schedule for Implementing Children´s Medicaid Redesign Plan | |
|---|---|
Health Homes for Children
|
January 1, 2016 |
|
January 1, 2017 |
| Expanded Array of State Plan Services for All Children | Early in 2016 |
|
January 1, 2017 (NYC and Long Island) July 1, 2017 (Rest of State) |
Health Home Care Management for Children with Chronic Conditions, Serious Emotional Disturbance, HIV, Trauma – January 2016 Enrollment Begins – January 2017 Waiver/CAH I & II Care Coordination Transition to Health Home
| Current Health Home Eligibility Criteria and Proposal to Modify Health Home Eligibility Criteria (Modifications in Bold Black, Require CMS Approval) |
|---|
Person must be enrolled in Medicaid and have:
|
Chronic Conditions Include:
|
- ✓ Comprehensive Care management available to broader array of children with chronic and complex conditions –
not just waiver eligible children (12,000 to ˜ estimated 175,000) - ✓ CAH I & II and Medically Fragile Children (MFC) – meet two or more chronic conditions criteria
- ✓ Requires CMS Approval of State Plan Amendment
- ✓ Discussions with CMS are now underway
- ✓ See Appendix for proposed definition of trauma and definition of SED
Six Proposed New State Plan Services Early in 2016
|
- ✓ More tools in the tool box
- ✓ Requires CMS Approval of State Plan Amendment
- ✓ Discussions with CMS are underway
- ✓ New State Plan Services available to ALL children – Medically necessary criteria under development
- ✓ See Appendix for Descriptions of New Services
Proposed Home and Community Based Services – January 2017
|
- ✓ Reflects "alignment" of all HCBS services available under different 1915c Waiver Programs (including CAH I & II)
- ✓ Requires CMS Approval of 1115 Amendment for Managed Care
- ✓ Approach to determining eligibility for HCBS
- ✓ Level of Care (LOC)– criteria met and determined by assessment that would indicate a child is eligible for or at risk of medical institutional placement in licensed by NYS OMH, Intermediate Care Facility for the Mentally Retarded (ICF/MR), or skill nursing facility/Hospital. Current criteria for children´s 1915(c) Waivers.
- ✓ NEW Concept: Level of Need (LON)– criteria met and determined by assessment that would indicate a child has needs that cannot be met only by non–medical institutional State Plan Services, but who does not qualify for Level of Care.
- Both levels determined by CANS–NY (Child and Adolescent Needs and Strengths Assessment) and its algorithms.
- ✓ More tools in the tool box: HCBS available to larger population of children (no longer limited to waiver population)
- ✓ Broader array of HCBS available, at the same time 1915c Waiver Programs are discontinued
- ✓ See Appendix for Descriptions of Proposed HCBS
Children that Qualify for Medicaid as Family of One Preserve Access to Services
- Individuals with third party health insurance and dual coverage – excluded from managed care in NYS (lifting of exclusion under discussion)
- Children´s design includes proposal to evaluate LON/LOC eligibility to establish disability and need for HCBS benefits, then follow with determination of Medicaid eligibility without regard to parental income
- Once eligible for Medicaid through LON/LOC eligibility and Medicaid budget methodology, the door is opened to access all Medicaid services for which the child is eligible (e.g., Health Home, State Plan services, HCBS)
- HCBS benefits will be available in Medicaid Managed Care and in separate, but equal fee–for–service Medicaid system for these "family of one" children who are excluded from enrolling in a Plan in NYS
"Today and Tomorrow" – Expansion of Services for All Children
| Today – 2015 | Tomorrow – 2017 Full Implementation | |
|---|---|---|
|
→ |
|
"Today and Tomorrow" – The Future for CAH Children
| Today 2015 – CAH Children | Tomorrow CAH Children January 2017 |
|---|---|
| Children Eligible for CAH enrolled in CAH I, II Waiver | Children enrolled in CAH and other Waiver children will transition to Health Home (directly enrolled in Health Home by CAH provider that contracts with Health Home) Transition provisions will be developed and will preserve continuity of care (care manager and types of services) Parental Consent and Choice |
| Under Waiver: Receive Case Management from CAH I and II Case Manager | Will receive Care Management under Health Home Program (6 Core Services) CAH case managers will be transitioned to Health Home Care Managers – Preserve expertise of CAH case managers in Health Home Program |
Under Waiver: Receive Select Array of Four HCBS Services
|
In addition to existing 4 HCBS services, 7 new HCBS services available to those that qualify (LOC, LON criteria)
|
| Under Waiver: Children age out of CAH I and II at the age of 18 | Children that continue to qualify for Health Home Care management transition to adult Health Homes (i.e., they do not "age out") |
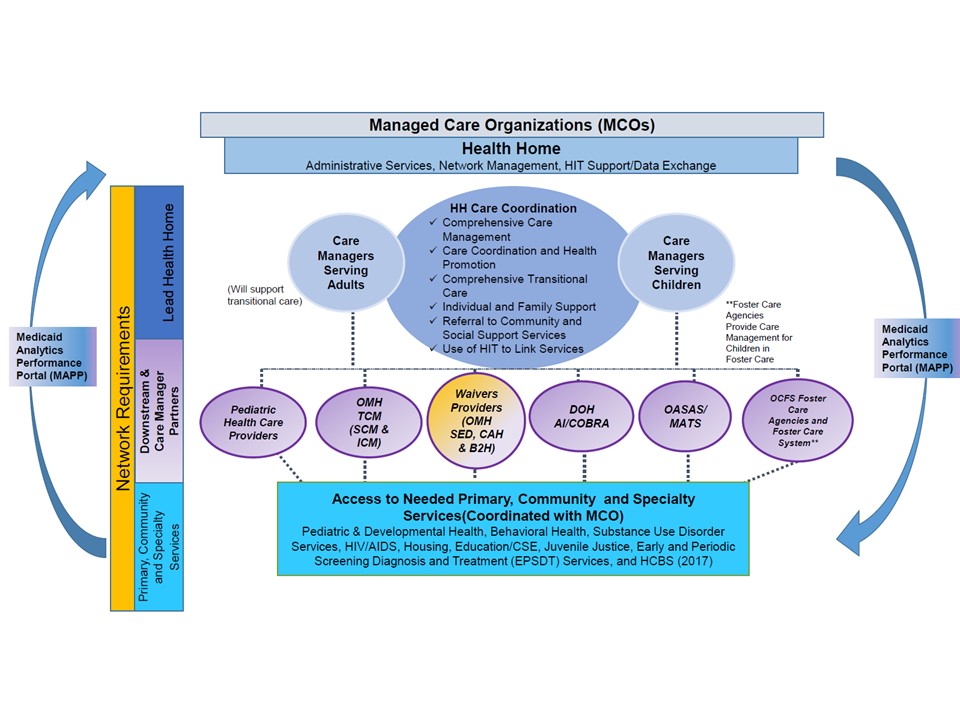
Overview
Health Home Model for Children
Health Home Optional Benefit that Provides Comprehensive Care Management
- Health Home is an optional State Plan benefit authorized under Section 2703 of the Affordable Care Act (ACA) to coordinate care for people with Medicaid who have chronic conditions – there is choice
- Health Home is a Care Management model that provides:
- Enhanced care coordination and integration of primary, acute, behavioral health (mental health and substance abuse) services, and
- Linkages to community services and supports, housing, social services, and family services for persons with chronic conditions
- In New York State, the Health Home model has been a central feature of the Medicaid Redesign Team (MRT) initiatives for adults and children, and overall efforts to integrate behavioral and physical health and social supports, transition the behavioral health benefit to managed care for children and adults, provide "Care Management for All," and reduce avoidable hospitalizations under the Delivery System Reform Incentive Payment (DSRIP) Program
New York State Health Home Model
- Health Homes are led by one provider (single point of accountability) which is required to create a comprehensive network of providers to help members connect with:
- One or more hospital systems
- Multiple ambulatory care sites (physical and behavioral health, specialty providers for children and adults)
- Community and social supports, e.g., housing and vocational services
- Health Homes provide an opportunity to establish critical linkages and help break down silos of care by linking systems and programs (education, child welfare, early intervention) to comprehensive care planning
- Managed care plans
- Existing care management providers (e.g., TCM, Waiver Providers) that have (adults) and will (children) operate under the Health Home program to provide care management and develop plan of care
- The Health Home model has been designed to incorporate the expertise of existing care managers, including CAH I & II providers
- Health Homes were implemented across the State in January 2012, adults prioritized for enrollment – work now underway to begin to enroll children
Tailoring Health Home Model to Serve Children
- Over the past year, the State Agency partners (DOH, OMH, OASAS, OCFS) have worked with stakeholders to tailor the Health Home Model for children to:
- Expand Health Home eligibility criteria to include trauma
- Incorporate modified Child and Adolescent Needs and Strengths Assessment–NY tool in the model
- Develop Health Home rates for children
- Tailor the delivery of the six core Health Home services to children to the needs of the child and family
- Develop referral and assignment process for enrolling children into Health Home (parental consent requirements)
- Develop criteria and Application for providers seeking to be a Health Home Designated to Serve Children
- Expanded network requirements – children´s specialty and other providers and care managers that currently serve children,
- Develop standards and policies for Health Homes serving children,
- Linkages to children´s systems of care (child welfare, education, juvenile justice)
New York State Health Home Model for Children
Health Home Care Managers Provide Six Core Care Management Functions
Detailed description of activities that comprise the six core services available here.
Health Homes Provide Six Core Care Management Functions
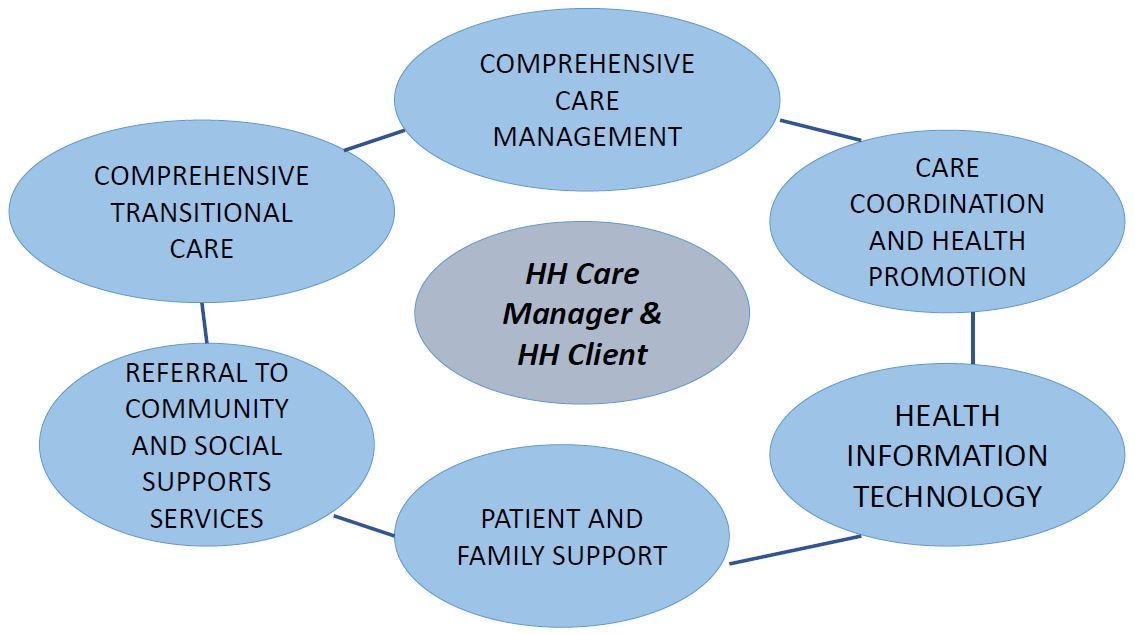
Health Home care management is "whole–person" and "person–centered" and integrates a care philosophy that includes both physical/behavioral health care with family and social supports.
Health Home Designated to Serve Children
- June 15, 2015 – Health Home Designations Announced
- ✓ 16 Health Homes Contingently Designated to Serve Children
- 12 adult Health Home expanding to serve children, 4 new children´s Health Homes
- Every county has at least two designated Children´s Health Homes
- List of Designated Health Homes Serving Children (see Appendix), and their primary contacts, can be found here.
- ✓ All 16 accepted designations and have agreed to address contingencies
- ✓ Contingency responses due back to State Team on August 17
- ✓ 16 Health Homes Contingently Designated to Serve Children
Health Home Designated to Serve Children and Opportunities for CAH I & II Providers
- All Designated Health Homes included contingencies requiring them to expand their network to include existing CAH I & II providers other providers with expertise in providing care management to children (e.g., other TCM OMH and other Waiver providers)
- Ensures continuity of care and a smooth transition for children receiving existing care management services that will transition to Health Home
- Builds capacity of knowledgeable Health Home care management providers
- Opportunity: Between January 1, 2016 – date children will begin to enroll in Health Home and January 1, 2017 when CAH Waiver I & II children and care management providers will transition to Health Home, CAH I & II providers may provide Health Home Care Management to children that are not enrolled in CAH or other waivers (medically fragile children, other children that meet Health Home eligibility requirements)
- Designated Children´s Health Homes will be contacting CAH I & II providers to become part of their networks, CAH I & II providers may also directly contact Designated Health Homes
- Request a copy of their Business Associate Agreement (BAA), complete and return it to the respective Health Home(s) in your area. This allows the designated Health Home to share data with network partners (e.g., with those that provide case management services)
"Today and Tomorrow"
The Future for CAH Providers: Changing Landscape and Opportunities for CAH I and II Providers
| Today 2015 – CAH Providers | Tomorrow CAH Providers 2017 |
|---|---|
| Under Waiver: Subject to requirements outlined in 1915c Home and Community Based Waiver Agreement | Meet requirement of Health Home care management model as defined by six core services and other standards for delivering care management for children (e.g., at least one face–to–face meeting per month for children with High or Medium acuity) |
| Under Waiver: Pediatric Patient Review Instrument (PPRI) and Level of Care form used to determine eligibility for HCBS and plan of care needs | CANS–NY will be used to determine Health Home rate tier and eligibility for HCBS services (providers may use other assessment tools to assist in development of person centered care plan) |
| Under Waiver: Paid $22.73 per 15–minute interval unit using case management rate codes 2301 or 2302, no additional fee for assessment, no concept or payment for outreach | Initially paid Legacy Payment then paid Per Member Per Month (PMPM) rate based on High, Medium, Low tier that is determined by CANS–NY algorithm and paid separate rate for assessment and outreach |
| Under Waiver: No central data register or system to record, review, and analyze individual and/or aggregate performance measures across network | MAPP a performance management system that will provide tools to the HH network to track members, assist with billing information, and provide performance data dashboards and eventually house other performance metrics |
| Under Waiver: Limited number of HCBS services available | Wider array of State Plan services (2016) and HCBS services available to those who qualify – more tools in the tool box to develop comprehensive plans of care |
| Under Waiver: Case Manager Qualifications Individual case management staff must meet the educational and experience qualifications outlined in 18 NYCRR 505.16. The individual providing case management must have two years of experience in a substantial number of activities outlined in this Directive, including the performance of assessments and development of case management plans. Voluntary or part–time experience which can be verified will be accepted on a prorated basis. The following may be substituted for this requirement: a. one year of case management experience and a degree in a health or human service field; b. one year of case management experience and an additional year of experience in other activities with the target population; c. a bachelor's or master's degree which includes a practicum encompassing a substantial number of activities outlined in this Directive, including the performance of assessments and development of case management plans; or d. meeting the regulatory case management requirements of another State agency. | Case Manager Qualifications: Care managers that serve children with acuity level of "high" as determined by the CANS–NY or in HFW when implemented have: A Bachelor of Arts or Science with two years of relevant experience, or
|
| Under Waiver: Limited number of HCBS services available | Wider array of State Plan services (2016) and HCBS services available to those that qualify – more tools in the tool box to develop comprehensive plans of care |
Opportunities for CAH providers to expand lines of business:
|
Other Health Home for Children Design Features of Interest to CAH I & II Providers
CANS–NY and Health Home
(CANS–NY: Child and Adolescent Needs and Strengths–NY)
- The CANS–NY assessment (as modified for New York) will be used:
- ✓ To assist in the development of the person–centered care plan
- ✓ Determine acuity for Health Home rate tiers
- ✓ Provide information that may help determine if children meet the Health Home eligibility functional criteria for Serious Emotional Disturbance (SED) and Trauma
- ✓ CANS–NY by itself will not determine Health Home eligibility
- CANS will also be used to determine the eligibility for Home and Community Based Services (HCBS) that will be made available with the behavioral health and health benefit transitions to Managed Care in 2017
Modifying CANS–NY for Health Homes
- The State Agency Partners, in consultation and under the guidance of Dr. John Lyons, author of the CANS have been working to:
- ✓ Modify the tool to better reflect the population of children that are expected to be eligible for Health Home, resulting in revisions made in 2014–15 which include:
- Broad array of target populations
- Separate tools for 0–5 and 6–21 age groups
- Addition of more modules for the 14 and older youth population (e.g., independent activities of daily living, transition to adulthood)
- Make enhancements to better assess medically fragile children
- Modify the tool to determine functional limitations required to meet the SED and Trauma Health Home eligibility criteria
- ✓ Develop algorithms to determine acuity for assignment to a Health Home per member per month rate tier (i.e., High, Medium, Low) and HCBS eligibility (Level of Care, Level of Need)
- ✓ Modify the tool to better reflect the population of children that are expected to be eligible for Health Home, resulting in revisions made in 2014–15 which include:
CANS–NY Testing and Refinements Underway
- The draft revised tools have been posted to the Department´s website
- The modifications to the CANS–NY have been tested
- Testing began in March 2015 and includes:
- ✓ The following providers, working with newly assessed or currently served children:
- OMH TCM
- OMH Waiver
- LGU/SPOA
- OCFS Waiver
- CAH I/II Waiver
- OASAS providers
- Providers working with medically fragile children
- ✓ Databases available to Dr. John Lyons will test the NY algorithms for Medically Fragile and Early Intervention populations in Ontario, Canada and Indiana
- ✓ Existing OCFS and OMH databases
- ✓ The following providers, working with newly assessed or currently served children:
- Chapin Hall of the University of Chicago will be collecting and assisting the State in analyzing and evaluating the test data and algorithms
Modifying CANS–NY for Medically Fragile Population
The Department of Health has been working with a small number of CAH I and II and Medically Fragile Children providers to test the tool and receive their input on how to better modify the tool for these populations.
- ✓ Meetings have occurred between CAH and MFC providers helping test the CANS–NY, DOH staff, State Agency Partners and Dr. John Lyons
- ✓ Feedback from these meetings has been incorporated into the tool
- Items have been modified (e.g. mobility, sensory)
- A "medical module" has been added to both CANS (0–5 and 6–21), and a "developmental module" has been incorporated into CANS (0–5)
- ✓ Structured vignettes were submitted by CAH and MFC providers and have been incorporated into in–person CANS training (which will also be recorded and posted to website)
- ✓ Modifications to the CANS–NY tool and algorithm can continue to be made to reflect actual experience and data collected with use – expectation is this is ongoing process
CANS–NY Training
- CANS–NY In Person Training Sessions
- ✓ July 29, 30 – Albany – Completed with representation from CAH
- ✓ August 20, 21 – Rochester–Hillside; 8:30am – 4:30pm
- ✓ August 25, 26 – NYC–OASAS; 9am–5pm
- ✓ September 22, 23 – NYC– OASAS; 9am – 5pm
Day 2 of all Trainings are for Supervisors Only
- CANS Training Albany – July 29, 30
- This session will be recorded and posted to the website
- CANS Training Rochester – August 20, 21
- CANS Training NYC 1 – 8/25, 8/26
- CANS Training NYC 2 – 9/22, 9/23
- ✓ Online CANS–NY training and certification is available to all care managers and can be accessed at www.canstraining.com
Framework for Development of Health Home Per Member Per Month Rates for Children
- ✓ Tiered rate structure would take effect January 2016 and would be the mandated government rates in effect in the first two years of Managed Care (2017 and 2018)
- ✓ Legacy care management payments are being developed for OMH TCM providers that will transition to Health Homes on January 1, 2016
- ✓ Legacy care management payments will be also be developed for children´s waiver programs (B2H, CAH I/II, OMH Waiver Programs) when they transition to Health Home in 2017
Health Home Rates for Children
(under 21)
| Per Member Per Month HH Care Management Rates for Children under 21 (non–Legacy Providers) (does not include HHDF rate add that may be applicable through November 2016) |
||
|---|---|---|
| Acuity (CANS Algorithm) |
Upstate | Downstate |
| HFW | $900 | $958 |
| High | 750 | 799 |
| Medium | 450 | 479 |
| Low | 225 | 240 |
| Outreach | 135 | 135 |
| Assessment | 185 | 185 |
Medicaid Analytics Performance Portal (MAPP) Functionality for Children´s Health Homes
- CANS–NY tool will be integrated into the Medicaid Analytics Performance Portal (MAPP)
- Billing, rate information and CANS–NY algorithms (High, Medium, Low)
- Referral Portal for Children (under 21)
- Community Referral (by LGU/SPOA and LDSS, and eventually others – discussed later) for Assignment
- Assignment and Enrollment by Health Homes, Plans and Care Managers
- Consent Management (Consent to refer, enroll, share information/ protected services)
- Access to MAPP
- MAPP will be launched shortly for adult model
- MAPP will be modified (as described above) for children
- Training specific to Health Home for Children providers (Health Homes, Plans, care managers) will be available later this Fall, prior to January 1, 2016 launch
Referral and Health Home Assignments Process for Children will be Housed in MAPP
- The consent of the parent/guardian is required to make a referral or enroll a child in Health Home (HH consent forms have been developed)
- Referrals for assignment and enrollment will be made through the MAPP Referral Portal for Children (members under 21)
- MAPP will accommodate "Community" Referrals for Assignment and Enrollment and "Direct" Referrals for Assignment and Enrollment
Direct Referrals for Health Home Assignment and Enrollment
- Direct referrals are made by Health Homes and Health Home care managers (e.g., CAH providers that have contract with Health Home to provide care management)
- Health Homes and care managers/voluntary foster care providers for foster care children, with parent/guardian and LDSS consent in the case of foster care, may make direct referrals to a Health Home
- Health Homes and care managers making direct referrals will be provided information regarding contractual relationships between the member´s Plan and Health Homes
- Assignments cannot be made to Health Homes where there is no contractual relationship with the Plan (there will be exceptions and procedures developed for foster care assignments that involve relocation of a child to an area outside of the plan´s network)
- Health Homes and care managers will make direct assignments – enter child in outreach segment (if consent to enroll has not been obtained) or care management enrollment segment (if consent has been obtained)
- Plans can also identify eligible children and make assignments to Health Homes
- Families always have ability to choose
Community and Provider Referral and Assignment Process
"Community" Referrals:
- Made by an entity or provider that is not a Health Home, Health Home care manager or a Managed Care Plan
- In the short term, State will pilot the use of the Portal by authorizing LGU/SPOAs and LDSS to access the Community Referral portion of MAPP to make referrals that will identify children for assignment and enrollment to a Health Home
- Over time, the State will expand access to the Community Referral portal by identifying and authorizing other entities that are natural points of contact in the systems of care that impact children to make referrals through the Community Referral portal (Early Intervention initial care coordinators School Districts, county probation departments, pediatricians, emergency rooms,)
- Require referee to provide information including: affirmatively indicating they have parent/guardian consent to make a referral to a Health Home, will require Medicaid CIN number, will require parent/guardian contact information, and whether a member is receiving preventive services and by which entity (if the information is provided),
- Provide "feedback" to the referring entity including: if the member is already enrolled in a Health Home and which one, confirmation the referral was made
Staying Current with Design and Implementation of Health Homes for Children
Health Homes Serving Children Website
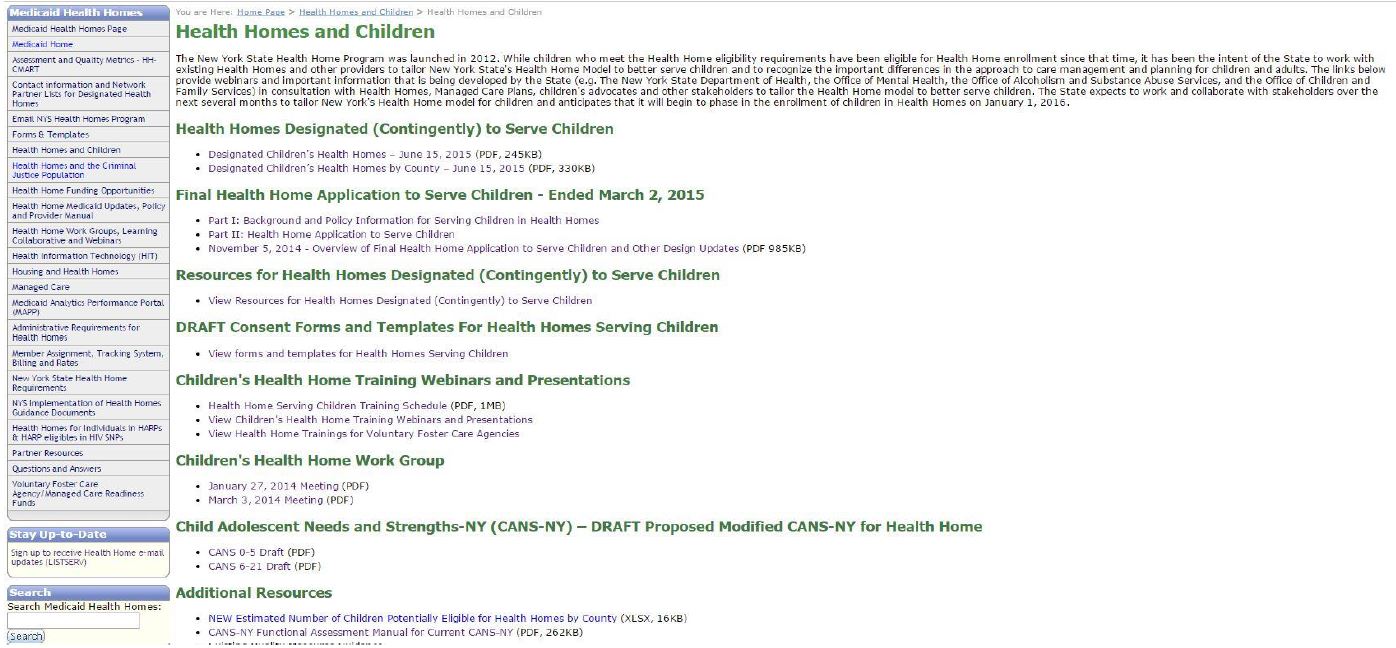
Select Trainings on Key Elements of Health Home Design
- Children´s Health Home Trainings
- http://www.health.ny.gov/health_care/medicaid/program/medicaid_health_homes/hhsc_webinars.htm
- MAPP – July 9, 2015
- Health Homes Designated to Serve Children – June 24, 2015
- Transitioning Office of Mental Health Targeted Case Management Program Serving Children to HHs– June 8, 2015
- Date Exchange Application & Agreements for Health Homes Serving Children – May 27, 2015
- Consent Policies and Procedures– May 18, 2015
- Referral and Health Home Assignment Process for Children – May 11, 2015
- Design and Implementation Updates – April 29, 2015
- Health Information Technology: Requirements for HHs– March 4, 2015
- All trainings are recorded and posted to the Website
Subscribe to the HH Listserv, Other Resources and Assistance
- Stay up–to–date by signing up to receive Health Home e–mail updates
- Health Homes for Individuals in HARPs & HARP eligibles in HIV SNPs
- Health Home Bureau Mail Log (BML)
- Contact the Health Home Program at the Department of Health at 518.473.5569
Appendix
Health Homes Designated to Serve Children*
| Health Home | Designated to Serve Children Pending the Acceptance and Implementation of Contingencies* |
|---|---|
| Catholic Charities of Broome County | Encompass Catholic Charities Children´s Health Home Albany, Allegany, Broome, Cattaraugus, Chautauqua, Cayuga, Chemung, Chenango, Clinton, Columbia, Cortland, Delaware, Erie, Essex, Franklin, Fulton, Genesee, Greene, Hamilton, Herkimer, Jefferson, Lewis, Livingston, Madison, Monroe, Montgomery, Niagara, Oneida, Onondaga, Ontario, Orleans, Oswego, Otsego, Rensselaer, Saratoga, Schenectady, Schoharie, Schuyler, Seneca, St. Lawrence, Steuben, Tioga, Tompkins, Wayne, Warren, Washington, Wyoming, Yates |
| Greater Rochester Health Home Network LLC | Cayuga, Chemung, Livingston, Monroe, Ontario, Seneca, Steuben, Wayne, Yates, Allegany, Genesee, Orleans, Wyoming |
| Central New York Health Home Network (CNYHHN Inc.) | Albany, Rensselaer, Schenectady, Cayuga, Herkimer, Jefferson, Lewis, Madison, Oneida, St. Lawrence |
| North Shore LIJ Health Home | Queens, Nassau, Suffolk |
| Coordinated Behavioral Care, Inc. dba Pathways to Wellness Health Home | Bronx, Brooklyn, Manhattan, Queens, Staten Island |
| St. Mary´s Healthcare | Fulton, Montgomery |
| Niagara Falls Memorial Medical Center | Niagara |
| Hudson River HealthCare, Inc. (HRHCare) | Nassau, Suffolk |
| St. Luke´s–Roosevelt Hospital Center dba Mount Sinai Health Home | Bronx, Brooklyn, Manhattan, Queens, Staten Island |
| VNS – Community Care Management Partners, LLC (CCMP) | Bronx, Brooklyn, Manhattan, Queens, Staten Island |
| Adirondack Health Institute, Inc. | Clinton, Essex, Franklin, Hamilton, St. Lawrence, Warren, Washington |
| VNS of Northeastern NY (Care Central) | Saratoga, Schenectady |
| New Children´s Health Home – Partnership to Be Formed Among: Montefiore Medical Center dba Bronx Accountable Healthcare Network Health Home, Open Door Family Medical Centers dba Hudson Valley Care Coalition, Hudson River Healthcare dba Community Health Care Collaborative (CCC), and Institute for Family Health |
Bronx, Columbia, Dutchess, Greene, Orange, Putnam, Rockland, Sullivan, Ulster, Westchester |
| Children´s Health Homes of Upstate New York, LLC (CHHUNY) | Albany, Allegany, Broome, Cattaraugus, Cayuga, Chautauqua, Chemung, Chenango, Clinton, Columbia, Cortland, Delaware, Dutchess, Erie, Essex, Franklin, Fulton, Genesee, Greene, Hamilton, Herkimer, Jefferson, Lewis, Livingston, Madison, Monroe, Montgomery, Niagara, Oneida, Onondaga, Ontario, Orange, Orleans, Oswego, Otsego, Putnam, Rensselaer, Rockland, Saratoga, Schenectady, Schoharie, Schuyler, Seneca, St. Lawrence, Steuben, Sullivan, Tioga, Tompkins, Ulster, Warren, Washington, Wayne, Wyoming, Yates |
| Collaborative for Children and Families | Bronx, Brooklyn, Manhattan, Nassau, Queens, Staten Island, Suffolk, Westchester |
| Kaleida Health–Women and Children´s Hospital of Buffalo | Allegany, Cattaraugus, Chautauqua, Erie, Genesee, Niagara, Orleans, Wyoming |
Children with Developmental Disabilities
- Children in Health Homes that have a developmental delay diagnosis and one other Health Home chronic condition or a single qualifying Health Home chronic condition and who are not currently receiving services from the Office for People with Developmental Disabilities (OPWDD) may be enrolled in Health Home
- Children in the Care at Home III, IV, and VI Waivers will not be included in the waivers that are transitioned to Health Home in 2017 (i.e., only OMH SED, DOH CAH I/II, OCFS B2H)
Health Home Appropriateness Criteria
| Appropriateness Criteria for Health Home Eligibility |
|---|
Appropriateness Criteria: Individuals meeting the Health Home eligibility criteria must be appropriate for Health Home care management. Assessing whether an individual is appropriate for Health Homes includes determining if the person is:
|
SED Definition for Health Home –SED is a single qualifying chronic condition for Health Home and is defined as a child or adolescent (under the age of 21) that has a designated mental illness diagnosis in the following Diagnostic and Statistical Manual (DSM) categories* as defined by the most recent version of the DSM of Mental Health Disorders AND has experienced the following functional limitations due to emotional disturbance over the past 12 months (from the date of assessment) on a continuous or intermittent basis
| SED Definition for Health Home – DSM Qualifying Mental Health Categories* |
|---|
|
| Functional Limitations Requirements for SED Definition of Health Home |
|---|
To meet definition of SED for Health Home the child must have experienced the following functional limitations due to emotional disturbance over the past 12 months (from the date of assessment) on a continuous or intermittent basis
|
*Any diagnosis in these categories can be used when evaluating a child for SED. However, any diagnosis that is secondary to another medical condition is excluded.
Health Home Eligibility Criteria
Trauma at Risk for Another Chronic Condition
Trauma is defined as exposure to a single severely distressing event, or multiple or chronic or prolonged traumatic events as a child or adolescent, which is often invasive and interpersonal in nature. Trauma includes complex trauma exposure which involves the simultaneous or sequential occurrence of child maltreatment, including psychological maltreatment, neglect, exposure to violence, and physical and sexual abuse.
A child or adolescent who has experienced trauma would be defined to be at risk for another chronic condition if they have one or more functional limitations that interfere with their ability to function in family, school, or community activities, or they have been placed outside the home.
Functional limitations are defined as difficulties that substantially interfere with or limit the child in achieving or maintaining developmentally appropriate social, behavioral, cognitive, communicative, or adaptive skills, or for a child who experienced trauma due to child maltreatment, a functional limitation is defined as a serious disruption in family relationships necessary for normal childhood growth and development.
Proposed Descriptions of Expanded State Plan Services for Children
Crisis Intervention: Crisis Intervention (CI) services are provided to a child and his/her family/caregiver who is experiencing a psychiatric or substance use crisis, are designed to interrupt and/or ameliorate a crisis experience including an assessment, immediate crisis resolution and de–escalation, and development of a safety plan.
Psychosocial Rehabilitation: Psychosocial Rehabilitation Services (PRS) are designed to work with children and their families to implement interventions outlined on a treatment plan to compensate for or eliminate functional deficits and interpersonal and/or environmental barriers associated with a child/youth´s behavioral health needs.
Community Psychiatric Support & Treatment (CPST): CPST services are goal–directed supports and solution–focused interventions intended to achieve identified goals or objectives as set forth in the child´s plan of care. CPST is designed to provide community–based services to children and families who may have difficulty engaging in site–based program or services, but can benefit from or prefer on–site rehabilitative services.
Other Licensed Practitioners: Non–physician licensed behavioral health practitioner who is licensed in the State to prescribe, diagnose and/or treat individuals with the physical or mental disability or functional limitations at issue, operating within the scope of practice defined in State law and in any setting permissible under State practice law. Activities would include: Recommending treatment, developing recovery or treatment plan, and activities within the scope of all applicable state laws and their professional license including counseling, individual or family therapy.
Family Peer Support Services: Family Peer Support Services (FPSS) are an array of formal and informal services and supports provided to families caring for/raising a child who is experiencing social, emotional, developmental, substance use and/or behavioral challenges in their home, school, placement, and/or community. FPSS provide a structured, strength–based relationship between a Family Peer Advocate and the parent/family member/caregiver for the benefit of the child/youth.
Youth Peer Support and Training: Youth support and training (YSAT) services are youth formal and informal services and supports provided to youth and families raising an adolescent who are experiencing social, emotional, developmental, substance use and/or behavioral challenges in their home, school, placement, and/or community centered services that provide the training and support necessary to ensure engagement and active participation of the youth in the treatment planning process and with the ongoing implementation and reinforcement of skills learned throughout the treatment process.
Proposed Children´s HCBS Descriptions
Care Coordination: Care coordination (for children not eligible for Health Home) eligibility under development – CMS requires care plans for children that receive HCBS services
Habilitative Skill Building: This service focuses on helping the child to be successful in the home, community and school by acquiring both social and environmental skills associated with his/her current developmental stage.
Family/Caregiver Supports & Services: Family/caregiver supports, and services enhance the child´s ability to function as part of a family/caregiver unit and enhance the family/caregiver´s ability to care for the child in the home and/or community. This service may be provided to individual children and their family/caregivers in small groups of a maximum of three HCBS–eligible children and their support networks, where the child and/or family/caregivers participate with others who are in similar situations.
Crisis Respite: Crisis Respite is a short–term care and intervention strategy for children and their families as a result of a child´s mental health/substance use crisis event, medical crisis or trauma that creates an imminent risk for an escalation of symptoms without supports and/or a loss of functioning. It may be used when acutely challenging emotional or medical crisis occur which the child is unable to manage without intensive assistance and support.
Planned Respite: Planned respite services provide planned short–term relief for family/caregivers that are needed to enhance the family/caregiver´s ability to support the child´s functional, mental health/substance use disorder and/or health care issues. The service is direct care for the child by staff trained to support the child´s needs while providing relief from caregiver activities for the family/caregiver.
Prevocational Services: Prevocational services are individually designed to prepare a youth to engage in paid work, volunteer work or career exploration. Prevocational services are not job–specific, but rather are geared toward facilitating success in any work environment for youth whose functional limitations do not permit them access to other prevocational services.
Supported Employment: Supported employment services are individually designed to assist youth to engage in paid work or volunteer work. Supported employment services provide assistance to children/youth with severe functional challenges for the purposes of engaging in work.
Community Advocacy & Support: Community advocacy and support improves the child´s ability to gain from the community and educational experience and enables the child´s environment to respond appropriately to the child´s disability and/or health care issues. Community advocacy and support is intended to assist the child, family/caregiver, and community/school staff in understanding and addressing the participant´s needs related to their disability(ies).
Non–Medical Transportation: Non–medical Transportation services are offered, in addition to any medical transportation furnished under the 42 CFR 440.17(a) in the State Plan. Non–medical Transportation services are necessary, as specified by the service plan, to enable participants to meet als outlined in their plan of care.
Day Habilitation: Day habilitation services assists children with developmental disabilities with the self–help, socialization, and adaptive skills necessary for successful functioning in the home and community when other types of skill–building services are not appropriate.
Adaptive & Assistive Equipment: This service provides technological aids and devices that can be added to the home, vehicle, or other eligible residence of the enrolled child to enable him/her to accomplish daily living tasks that are necessary to support the health, welfare, and safety of the child.
Accessibility Modifications: This service provides internal and external physical adaptations to the home or other eligible residences of the enrolled child that are necessary to support the health, welfare, and safety of the child.
Palliative Care: This is a set of services offered to help families deal with end–of–life related issues due to child´s illness. Types of services included: Family Palliative Care Education (Training); Bereavement Therapy; Pain and Symptom Management; Expressive Therapy (Art, Music and Play); and Massage Therapy.
|top of page|