New York State Dual Eligible Integrated Care Roadmap
- Roadmap is also available in Portable Document Format (PDF)
March 2022

/health_care/medicaid/redesign/duals.htm
New York State Dual Eligible Integrated Care Roadmap
Table of Contents
Introduction
Following a recommendation of the Medicaid Redesign Team (MRT) II in March 2020, the Office of Health Insurance Programs (OHIP) within the New York State Department of Health (DOH) has been diligently spearheading a number of related initiatives that are designed to promote integrated care for Medicaid members who are dually eligible for Medicare & Medicaid (dual eligible members or duals). This Dual Eligible Integrated Care Roadmap (or the Roadmap) outlines why DOH has made integrated care for dual eligible members a priority in the Medicaid program and describes the coordinated initiatives for improving integrated care.
I. Why Is Integrated Care Important for Dual Eligible Members?
Members qualifying for both Medicare and Medicaid are referred to as dual-eligibles, or as "duals." For the purposes of this paper, duals will refer to those individuals who are Medicare beneficiaries with full Medicaid benefits (i.e. Full Benefit Dual Eligibles) unless otherwise indicated.1
The healthcare coverage for duals is often fragmented and lacks coordination. Members frequently receive Medicare benefits from one health plan or from Medicare fee-for-service (FFS), while receiving their Medicaid benefits from a separate health plan or Medicaid FFS. Duals are one of the most complex populations and the bifurcation of the sources of their health benefits leads to inefficiencies, a lack of coordination and potentially diminished health outcomes.2
On the other hand, integrated care occurs when a member receives both Medicare and Medicaid services through the same health plan (Managed Care Organization or MCO). States that promote integrated care for duals have the opportunity to improve outcomes, enhance member satisfaction and reduce costs.
Integrated care brings with it a number of benefits to members, health care providers, MCOs, and the State.
- Members receive a simplified process for interacting with their MCO for care coordination, service receipt, benefit communications and maximization, and integrated appeals and grievances processes (where available). Members will also have the advantage of having one interdisciplinary care team that assists them with their medical and behavioral health needs as well as long term services and supports (LTSS), if applicable.
- Health care providers may see an increase in the ability to provide continuous care for members newly becoming dual, improved care coordination between Medicare and Medicaid benefits, and streamlined administrative procedures with MCOs, including simplified billing.
- MCOs will benefit from the ability to engage in enhanced care coordination and to achieve administrative efficiencies. MCOs will also benefit from more streamlined communication with states and Centers for Medicare and Medicaid Services (CMS) related to financial management, reporting requirements, coordination of benefits, and enrollment and disenrollment processes.
- New York will benefit from integrated care via reduced duplication of billing and more data insights into their dual eligible Medicaid population, which may lead to better care outcomes and fewer administrative expenditures.
CMS has a number of resources describing the additional benefits of integrated care3.
Despite this potential for improved outcomes, only approximately 4% of duals in New York State currently receive integrated care, as illustrated in Table 1. These factors led to the MRT II recommendation to undertake the duals initiatives outlined in this Roadmap aimed at improving duals integration for NYS's Medicaid beneficiaries. Through these initiatives, the Department is seeking to achieve a 250% increase in the number of duals receiving integrated care through an aligned contract by the end of 2023.
Table 1: Percentage of Duals by Integration as of June 2021
| Medicare Placement | Medicaid MCO 6/1/2021 | Medicaid FFS 6/1/2021 |
|---|---|---|
| Medicare D-SNP* with Medicaid Contract aligned | 4% | 0% |
| Medicare D-SNP with Medicaid Contract not aligned | 14% | 21% |
| Medicare Advantage excluding D-SNPs | 7% | 11% |
| Medicare FFS | 13% | 30% |
| Totals | 38% | 62% |
*D-SNPs are Dual Special Needs Plans
**Note that while PACE does not utilize DSNPs to create alignment, it is included as an integrated product
***Note the primary channel for plan enrollment for these duals is MLTCP; however, there are a small number of duals enrolled across other available plans that fit these criteria.
Note in Table 1, that members receiving integrated care through an aligned contract, or are ‘aligned', receive Medicaid and Medicare services via companion MCOs operated by the same organization. In other words, these members are enrolled in a Medicaid managed care plan for their Medicaid coverage, and, except for PACE, are also enrolled in a companion Medicare D- SNP product for their Medicare coverage. For a full listing of what integrated plans are available today, please see Appendix A.
II. New York State's Goals for Integrated Care
Following recommendations from the MRT II, which were enacted into state law as part of the State Fiscal Year 2020-21 budget, DOH has established four goals for moving forward with integrated care for duals. These goals are guiding DOH in creating this Duals Integration Roadmap:
- Create more opportunities to build alignment between Medicare and Medicaid through integrated MCO offerings.
- Streamline MCO offerings and promote informed member choice.
- Enable fewer member transitions and build stronger continuity of care; and
- Simplify administrative infrastructure for providers and MCOs.
These goals were formulated with lessons learned from New York State's past integration efforts and current integration challenges in mind, including consideration for the following key factors:
- Medicare Choice - under the principles of Medicare coverage choice, as codified in federal regulations, individuals may not be auto-enrolled into an integrated product. Accordingly, creating a smooth pathway for duals to elect an integrated product offering must rely on key, visible, and repeated opportunities to fully inform members regarding their options for dual coverage and the benefits associated with each option. In addition, choice principles require New York State to maintain a robust Medicaid fee-for-service or partial capitation option.
- Prior Experience - the Fully Integrated Dual Advantage (FIDA) Demonstration was the prior iteration of duals integration and experienced challenges ranging from insufficient member outreach and education, adequacy of Medicare and Medicaid MCO reimbursement rates, participation by MCOs not fully experienced in managing this complex population to poor provider engagement from the State.
- Engagement - for duals integration to be successful, DOH must work with members, providers, MCOs, and other stakeholders to educate and inform, as well as absorb and incorporate valuable feedback; and
- Integrated Grievance and Appeals - FIDA established Integrated Grievances and Appeals as the gold standard appeals process for integrated care.
Understanding these past barriers to successful implementation enables promotion of improved mechanisms for duals integration going forward.
Graphic 1: New York State Goals for Integrated Care for Dual Eligibles

III. Overview of Integrated Care Projects
To achieve its Goals for Integrated Care, DOH is implementing six related and scaffolded reform initiatives. These reforms include:
- Streamlining enrollment pathways.
- Enhancing dual eligible health plan coverage and benefits.
- Leveraging new contracting requirements.
- Developing member and provider education.
- Expanding enrollment opportunities to the federally authorized Program of All-Inclusive Care for the Elderly (PACE).
- Utilizing an integrated grievances and appeals process, where possible.
The Overview of Dual Eligible Integrated Care Projects below lists the current progress that DOH has made in implementing these integrated care initiatives and the continued ways in which DOH is growing the integrated duals infrastructure. DOH intends to supplement these initiatives as new opportunities are identified, whether through federal reforms, its experience during the COVID-19 Public Health Emergency (PHE) or proposed changes to align Medicaid eligibility tests for different groups of Medicaid members.
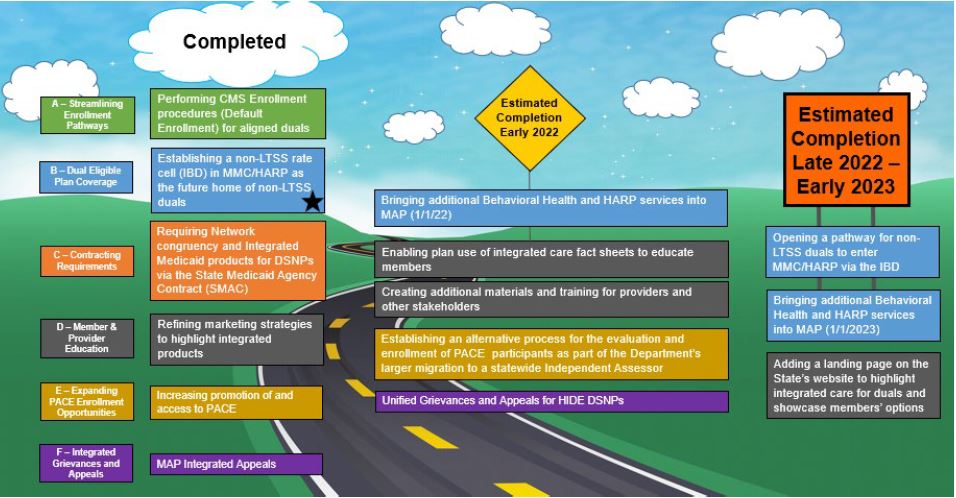
Graphic 2: Overview of Dual Eligible Integrated Care Projects
Reflecting the completion of several years of effort, DOH has created a new program to enable further growth of integrated duals, offering a distinct capitation rate in MMCP or HARP specific to this population. This program is discussed in additional detail in Section B below
DOH welcomes stakeholder feedback on additional initiatives that would promote integrated care for New York State's dual eligible population.
a. Streamlining Enrollment Pathways (Default Enrollment)
Perhaps the most high-profile initiative in this Roadmap is Default Enrollment for Medicaid members who become newly eligible for Medicare. Default Enrollment is a CMS enrollment procedure whereby Medicaid members seamlessly enroll into the aligned Medicare D-SNP of their current Mainstream Medicaid Managed Care Plan (MMCP) or Health and Recovery Plan (HARP) as they first become Medicare eligible. Under the same process, eligible MMCP/HARP members in receipt of LTSS are seamlessly transferred to the organization's MAP, where available, and default enrolled in the MAP-affiliated D-SNP. In line with federal requirements, this process preserves member choice by allowing members to "opt-out" of Default Enrollment if they would prefer another option for their Medicare and Medicaid coverage.
The Department views Default Enrollment as one of the primary drivers of increasing integrated care, as in the past, most newly dual Medicaid members would be disenrolled from their MMCP or HARP plan and exit to Medicaid FFS upon becoming Medicare eligible. In order to participate in Default Enrollment, MCOs must operate an MMCP or HARP product with an aligned D-SNP and successfully complete an application with CMS and DOH.
Graphic 3: Default Enrollment pathways
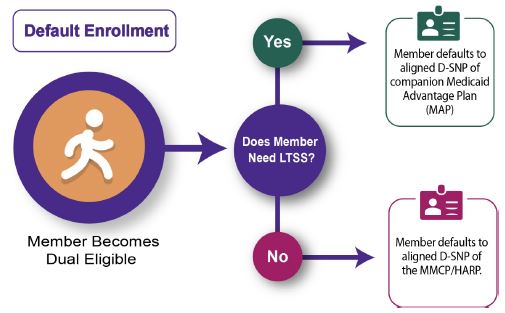
MCOs apply to become eligible for Default Enrollment and meet criteria established by DOH and CMS as described in the New York State Default Enrollment Plan Application. MCO criteria include operating an MMCP or HARP and an aligned Medicare D-SNP to establish proper alignment between programs for dual eligibles. Other requirements include having a 3.0 or higher CMS STAR rating for quality and committing in advance to meet the reporting requirements established within the application.
On April 1, 2021, Default Enrollment was launched in New York with three qualifying MMCPs. As of June 2021, four MMCPs are participating in Default Enrollment. In addition to the current MMCPs expanding the county coverage in which they are utilizing Default Enrollment, DOH expects additional MMCPs to participate beginning in 2022. In the first three months of the process, approximately 2,500 members have been successfully Default Enrolled, whereas historically these members would have been diverted to Medicaid FFS and not to integrated care. Default Enrollment is vital to DOH's integration goals as it allows the members to begin their Medicare journey in an integrated product from the earliest time they can be integrated. The program has now been in operation for ten months, and as of January 2022, there have been approximately 17,000 members successfully default enrolled.
b. Enhance Dual Eligible Plan Coverage and Benefits
These Default Enrollment efforts are buttressed by four changes in MCO coverage specific to duals that streamline MCO offerings and add benefits to make these new products comparatively attractive.
First, DOH has created a new program offering a distinct capitation rate in MMCP or HARP specific to this population, which is referred to as the Integrated Benefits for Dually Eligible Enrollees Program or "IB-Dual". As described above, the purpose for streamlining enrollment pathways for the dual eligible populations includes using Default Enrollment to enable new dually eligible members to remain in their current MMCP or HARP via that MCO's aligned IB-Duals offering, which is also aligned with the same MCO's Medicare D-SNP. This process is already underway for MCOs approved for Default Enrollment and IB-Dual. At a later point, if a member in the IB-Dual program requires LTSS, the member will be transitioned into a Managed Long-Term Care (MLTC) product. DOH is building the capacity for members to more seamlessly move from the IB-Dual program to their plan's integrated long-term care program at the time they require LTSS.
Second, with the introduction of the IB-Dual offering in MMCP and HARP, the "Medicaid Advantage" name and MCO type will be phased out because it is no longer necessary and is duplicative of the more streamlined IB-Dual/Default Enrollment option. DOH coordinated with the remaining MCOs that offered Medicaid Advantage products to close this program effective December 31, 2021. There were approximately 3,000 Medicaid Advantage members transitioned to the IB-Dual program in MMCP or HARP or disenrolled to fee-for-service as appropriate; all members retained the option to make another choice for their Medicare and Medicaid coverage.
Third, most duals not requiring LTSS (non-LTSS) today utilize Medicaid FFS. A significant portion of these non-LTSS duals are already enrolled in a Medicare D-SNP that is aligned with a MMCP. The Department is creating a pathway for these members, at their election, to transition to Medicaid managed care where the MMCP/HARP IB-Dual program alignment exists.
Fourth, consistent with promoting integration and enabling stronger member continuity of care, DOH is taking the necessary steps to incorporate Behavioral Health and Home and Community Based Services (HCBS) into the MAP benefit package, projected to begin in January 2023.
c. Leveraging New Contracting Requirements
MCOs that operate integrated Medicare and Medicaid managed care products must enter into contracts with both CMS and DOH for the delivery of benefit package services under all applicable program rules. The annual State Medicaid Agency Contract (SMAC) provides specific requirements for D-SNPs operating in New York State to improve and expand the integration and coordination of benefits, educate duals about D-SNP products, and reduce costs and administrative burden.
The 2022 SMAC instructed MCOs that offer a D-SNP in New York that they are required to submit an application to offer an integrated Medicaid product on or before March 31, 2022.
Effective January 1, 2022, MCOs operating D-SNPs will also be required to ensure that at least 50% of their Medicare and Medicaid participating provider networks are congruent. This requirement will increase to 65% beginning January 2023 and 80% beginning January 1, 2024.
The 2022 SMAC also encourages MCOs to work with New York State in good faith to ensure its Supplemental Benefits will overlap with Medicaid benefits covered by New York's Medicaid Plan during the next Medicare bid filing cycle. MCOs are encouraged to use at least 10% of their full rebate amount for covering Medicaid Benefits as Medicare Advantage Supplemental Benefits.
d. Developing Member and Provider Education Initiatives:
DOH is increasing its member and provider education strategies to highlight integrated products. In addition, DOH is creating the necessary educational materials to promote and encourage the transition to integrated care for dual eligible members enrolled in Medicare Advantage to join affiliated MMCP and HARP. These efforts include:
- Refining marketing strategies and creating materials to highlight integrated products, including updated documents with more information about the benefits of integrated care and developing professional documents for different stakeholder groups such as:
- Consumer-friendly language for beneficiaries, caregivers, families, and professionals for a dedicated duals website.
- Shareable outreach materials for both beneficiaries and professionals on New York's integrated care landscape.
- A collection of professional-facing handouts that state and county agencies, and others can use to understand New York's various integrated care products, including information on eligibility, enrollment, transitions, coverage and care coordination, benefits, and appeals and grievances.
- A collection of consumer-facing handouts on New York's various integrated care products, including information on eligibility, enrollment/transitions, coverage, and care coordination, and appeals and grievances.
- Utilizing integrated care fact sheets and MCO enrollee outreach resources to educate consumers:
- This includes performing targeted DOH mailings to consumers and allowing approved MCOs to share DOH fact sheets with consumers; and
- Working with approved MCOs on improving Default Enrollment process and outreach, including basic default noticing requirements to reduce the opt-out rate and make available detailed information on the MCO's products and benefits coverage options for a member newly becoming a dual.
- Creating additional materials and training for providers and other stakeholders, such as:
- Providing information for health care providers via the Medicaid Update, the official newsletter of the New York State Medicaid Program, on integrated care options.
- Continuing posting Frequently Asked Questions with key information for consumers and stakeholders regarding Default Enrollment and other initiatives.
- Establishing Frequently Asked Questions and other resource material for healthcare professionals on New York's integrated care landscape and how to help beneficiaries understand their options; and
- Conducting trainings on the Default Enrollment process for MCOs, Medical Directors, and Local Departments of Social Services.
- Adding a landing page on the State's website to highlight integrated care for duals and showcase members' options:
- Increasing the quality and amount of online resources, incorporating a guide-me section on the State's websites to explore Medicare and integrated care options; and
- Providing links to the New York State enrollment broker–New York Medicaid Choice–to allow consumers and caregivers to further explore how to enroll in integrated care options.
This Marketing Strategy and educational efforts will be continuously updated as new strategies are identified that might offer an informed choice by Medicaid members. DOH invites stakeholder input on ways that it may be best to reach and inform these Medicaid populations.
e. Expanding PACE Enrollment Opportunities
For over forty years, PACE Organizations have enabled thousands of New Yorkers aged 55 and older who are otherwise eligible for nursing home admission to remain safely in their communities. PACE fully integrates provision and payment for the entire array of Medicare and Medicaid covered services for duals. PACE also benefits from being federally authorized by Title VIII, Section 1894 and Title XIX, Section 1934 of the Social Security Act, and subject to detailed Federal regulations and requirements. Among these are provisions relating to marketing, enrollment, and assessment.
To ensure compliance with these unique federal requirements associated with PACE and as a means of enabling equal access to PACE, as compared to other available MLTC options, DOH is establishing an alternative process for the evaluation and enrollment of PACE participants as part of the Department's larger migration to a statewide Independent Assessor (IA).
Specifically, under regulations being issued by DOH, PACE Organizations will not be required to use the IA to complete the Community Health Assessment that informs the service authorization process. Additionally, and related to this alternative process for completion of the Community Health Assessments, DOH will work with PACE Organizations to determine a more streamlined, alternative process that is consistent with the federal requirements and expectations for determining eligibility and conducting service authorizations as part of PACE enrollment for members who are new to LTSS or already LTSS-eligible. These changes would build on other differentiations made in state law and policy that reflects the unique federally designated and regulated status of PACE, including the retained inclusion of non-emergency medical transportation services within the benefit package and different rate setting standards.
f. Unify Medicare and Medicaid Grievance and Appeals Process for D-SNPs
Dual eligibles have historically had to utilize two different, and sometimes conflicting, grievance and appeals processes for Medicaid and Medicare. The integrated appeals process allows for a single filing of an appeal or grievance with a member's plan regardless of whether the issue involves a Medicaid or Medicare benefit. This streamlined approach is administratively more efficient for MCOs and easier to navigate for members. Currently, DOH requires all exclusively aligned Fully Integrated Dual Eligible Special Needs Plan (FIDE SNPs) to participate in the integrated appeals and grievance demonstration process. Additionally, DOH is requiring that exclusively aligned Highly Integrated Dual Eligible Special Needs Plans (HIDE SNPs) comply with the unified appeals and grievances process in 2022.
IV. Conclusion
The Department is committed to working with the stakeholder community to enable the success of these integrated care initiatives. This Dual Eligible Integrated Care Roadmap presents a high- level overview of the initiatives that are planned and underway to further the goals of integration for dual eligible members in New York State.
Additional details on specific initiatives and materials for plans and stakeholders will be forthcoming. Please submit any questions to dualintegration@health.ny.gov.
V. Glossary of Terms
- Aligned: An aligned member, or a member in an aligned plan, refers to a member enrolled in a Medicaid managed care plan who is also enrolled in the organization's Medicare D- SNP designated to operate in an integrated manner with the Medicaid managed care plan.
- Default Enrollment: Default Enrollment is a Centers for Medicare & Medicaid Services (CMS) enrollment procedure whereby a Medicaid member who is prospectively identified as becoming Medicare eligible (becoming a dual), may be seamlessly enrolled into their MMCP or HARP's affiliated D-SNP at the time they become dual-eligible.
- D-SNP: Dual Special Needs Plan or D-SNP is a specialized type of Medicare Advantage plan for duals.
- Duals: Dually Eligible Beneficiary or dual is a Medicaid recipient who is also eligible for Medicare.
- FBDE: Full Benefit Dual Eligible of FBDE is a Medicare beneficiary with full Medicaid benefits (as opposed to individuals in programs that only provide partial coverage of the Medicare premium or co-insurance costs, called "partial duals").
- HARP: Health and Recovery Plan or HARP is a specialized comprehensive Medicaid managed care plan offering integrated physical health, mental health, and substance abuse services for adults with significant behavioral health needs.
- IB-Dual: The Integrated Benefits for Dually Eligible Enrollees Program or IB-Dual is a special integrated premium group within a MMCP or HARP for non-LTSS dual members who elect to enroll in the MMCP/HARP's aligned D-SNP. MMCP/HARPs must apply to the Department of Health (DOH) to operate the IB-Dual program; approval is added to the MCO's certificate of authority.
- Integrated care: Integrated care occurs when a dual is enrolled in both a Medicaid managed care plan and a Medicare D-SNP, where both MCOs are operated by the same organization, and the MCOs work together as to appear and function as one MCO for the benefit of the member.
- LTSS: Long Term Services and Supports or LTSS means health care and supportive services provided to individuals of all ages with functional limitations or chronic illnesses who require assistance with routine daily activities such as bathing, dressing, preparing meals, and administering medications. LTSS is comprised of community-based services such as home health services, private duty nursing, consumer directed personal assistance services, adult day health care program, personal care services, and institutional services including long term placement in residential health care facilities.
- MAP: Medicaid Advantage Plus or MAP is a specialized Medicaid managed care plan for duals in receipt of LTSS and meeting other eligibility requirements, which is exclusively aligned with a Medicare D-SNP (all MAP members must be enrolled in the affiliated D- SNP, all members of the affiliated DSNP must be enrolled in the MAP).
- Managed Care Organization (MCO): A managed care organization is a health care provider or a group or organization of medical service providers who offers managed care health plans. It is a health organization that contracts with insurers or self-insured employers and finances and delivers health care using a specific provider network and specific services and products.
- Medicaid Advantage: Medicaid Advantage is a specialized Medicaid Managed care plan designed to provide non-LTSS duals enrolled in a Medicare Advantage plan with a "wrap around" partial Medicaid benefit to improve coordination between Medicare and Medicaid service delivery for members. This MCO type will sunset at the end of 2021.
- Medicare Advantage: Medicare Advantage or Medicare Part C is an MCO providing coverage to a member for Medicare Part A and Medicare Part B (Inpatient and Outpatient); members often get coverage for Part D (prescription drug coverage), as well.
- MLTCP: Managed Long Term Care Plan or MLTCP is a specialized Medicaid Managed care plan offering a partial benefit (partially capitated) for coverage of LTSS for Medicaid recipients meeting certain eligibility requirements.
- MMCP: Mainstream Medicaid Managed Care Plan or MMCP is a Medicaid managed care plan that provides a comprehensive benefit package to their members. Most Medicaid recipients in New York State are enrolled in an MMCP for their Medicaid coverage.
- Non-LTSS: Non-LTSS is term used to refer to members not in receipt of long term services and supports.
- PACE: Program of All Inclusive Care for the Elderly or PACE is a special integrated MCO for dual members in receipt of LTSS; members are not in a D-SNP.
Appendix A
Integrated Plans
While integrated care only covers approximately 4% of duals in New York State, DOH has been focused on increasing the integrated offerings for both LTSS and non-LTSS members. The below table shows what plans offer integrated products today. More integrated plans are expected to come online next year.
Table 1: Percentage of Duals by Integration as of June 2021
| Medicare Placement | Medicaid MCO 6/1/2021 | Medicaid FFS 6/1/2021 |
|---|---|---|
| Medicare D-SNP with Medicaid Contract aligned | 4% See below for listing |
0% |
| Medicare D-SNP with Medicaid Contract not aligned | 21% | |
| Medicare Advantage excluding D-SNPs | 7% | 11% |
| Medicare FFS | 13% | 30% |
| Totals | 38% | 62% |
Table 2: Integrated Plan Offerings in New York State
| Integrated Offerings for LTSS Duals | Integrated Offerings for Non-LTSS Duals |
|---|---|
Medicaid Advantage Plus (MAP) (13)
|
Medicaid Advantage (3) (Being replaced by IB-Dual)
Default Enrollment Approved Plans: Integrated Benefits for Dually Eligible Enrollees Program (IB-Dual) (4)
|
Developing Member and Provider Education Initiatives
Following a recommendation of the Medicaid Redesign Team (MRT) II in March 2020, the Office of Health Insurance Programs (OHIP) within the New York State Department of Health (DOH) is spearheading a number of related initiatives that are designed to promote integrated care for Medicaid members who are dually eligible for Medicare & Medicaid (Dual Eligible Members or duals). These initiatives are discussed in detail in the Duals Integration Roadmap.

One of the integrated care initiatives being worked on by the Department is Developing Member and Provider Education Initiatives. This initiative is intended to facilitate the achievement of NYS' Goals for Integrated Care for Dual Eligibles, seen below.
Specifically, the Member and Provider Education Initiative will promote informed member choice (Goal #2) and enable fewer member transitions and build stronger continuity of care (Goal #3). New York is partnering with Medicare Rights Center (MRC) and New York Medicaid Choice (NYMC) to implement the Member and Provider Education Initiative.
The Member and Provider Education Initiative currently comprises four components:
- Refining marketing strategies and creating materials to highlight integrated products, including:
- Consumer-friendly language for beneficiaries, caregivers, families, and professionals for a website
- Shareable outreach materials for both beneficiaries and professionals on New York's integrated care landscape.
- A collection of professional-facing handouts that state and county agencies, and others can use to understand New York's various integrated care products, including information on eligibility, enrollment, transitions, coverage and care coordination, benefits, and appeals and grievances.
- A collection of consumer-facing handouts on New York's various integrated care products, including information on eligibility, enrollment/transitions, coverage, and care coordination, and appeals and grievances.
- Enabling plan use of integrated care fact sheets to educate consumers, including:
- Performing special mailings of the fact sheets to targeted populations.
- Creating additional materials and training for providers and other stakeholders, including:
- Providing information via the Medicaid Update for providers on integrated care options.
- Continuing FAQs for consumers and stakeholders regarding Default Enrollment and other initiatives.
- Establishing an FAQ for professionals on New York's integrated care landscape and how to help beneficiaries understand their options.
- Conducting trainings for plans and Local districts, such as the training DOH conducted on the default enrollment process for BH Medical Directors in April 2021.
- Adding a landing page on the State's website to highlight integrated care for duals and showcase members' options, including:
- Exploring all pathways to increase information on integrated care in the online space.
- Incorporating a guide-me section of the website to explore Medicare and integrated care options.
- Adding a link to the New York Medicaid Choice webpage to allow consumers and caregivers to further explore integrated care options and how to enroll.
____________________________________
1. QMB, SLMB, QI, and QDWI are categories of partial duals who exceed the federal income limit and therefore are ineligible for full Medicaid benefits from the State. For more details, go here 1
2. ICRC | Integrated Care Resource Center 2
3. Resources for Integrated Care Available for Health Plans and Providers | CMS 3
Follow Us