Integrated Care Plans for Dual Eligible New Yorkers

What does "Dual Eligible" mean?
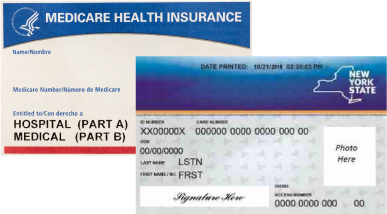
Dual-eligible beneficiaries (Medicare "dual-eligibles" or "duals") refers to those who qualify for both Medicare and Medicaid benefits. As a dual eligible beneficiary, you receive health coverage from both the Federal (Medicare) and State (Medicaid) government. You will have health insurance cards that may look like the following:
If you join a managed care plan for your coverage, you may have a health plan card with the company or plan name on it. In the United States, approximately 9.2 million people are considered to be qualified for "dual-eligible" status. (wikipedia.org)
New York State Dual Eligible Integrated Care Roadmap
On March 3, 2022, the New York State Department of Health (NYSDOH) released for public comment a draft of the New York State Dual Eligible Integrated Care Roadmap (the Roadmap) which outlines the State's priority to promote integrated care for Medicaid members who are dually eligible for Medicare and Medicaid, and describes the coordinated initiatives for improving integrated care options across the State.
Following a recommendation of the Medicaid Redesign Team (MRT) II in March 2020, the Office of Health Insurance Programs (OHIP) within the NYSDOH has been diligently spearheading a number of related initiatives that are designed to promote integrated care for dual eligible members. NYSDOH welcomed input from all stakeholders interested in providing feedback on the Roadmap.
For Consumers
Integrated Care Plans
An Integrated Care Plan is one that provides you with both your Medicaid and Medicare services from the same health plan. Integrated Care Plans are designed to help dual-eligible beneficiaries meet their health care needs within their own community, instead of going to a nursing home or other facility for care. There are three types of Integrated Care Plans in New York. Depending upon your care needs and whether you qualify as a dual-eligible, you may be eligible for an Integrated Care Plan.
Integrated Plans for dual-eligibles who are in need of LTSS (Long Term Services and Supports)
Both Medicaid Advantage Plus (MAP) and the Program of All Inclusive Care for the Elderly (PACE) are also known as Managed Long Term Care (MLTC) plans. These plans will pay for all your Medicare health services at little to no additional cost to you and include benefits such as home care and other long term services and supports (LTSS) you may need. As a member of an Integrated Care Plan, you must use the plan's network of doctors, although your existing doctor(s) may agree to participate with the plan.
- MAP - Medicaid Advantage Plus
- MAP provides Medicaid benefits including LTSS and Medicare benefits. Plans may also provide additional benefits such as transportation, home-delivered meals and over-the-counter (OTC) benefits such as vitamins, bandages, cold medicine, etc.
- More information about MAP can be found in the dedicated section below.
- PACE provides all Medicaid LTSS and Medicare covered services through a team of health care professionals. This team helps decide what services are necessary to improve and maintain your health.
- PACE offers you the option of receiving some services in your home or in its day center and on-site health clinic
- Additional information about PACE can be found in the dedicated section below.
For additional enrollment information about the above plans visit New York Medicaid Choice.
Integrated Care Plans for dual-eligibles who are not in need of LTSS (Long Term Services and Supports)
- IB-Dual - Integrated Benefits for Dually-Eligible Enrollees Program
- This new program replaces the former Medicaid Advantage product. It provides a more complete set of benefits and services for those dual-eligible beneficiaries who do not require long term services and supports.
- IB-Dual provides you with Medicaid and Medicare covered services through the same health plan.
- IB-Dual allows members who are Medicare eligible to remain in their Mainstream Medicaid Managed Care health plan. You will receive both your Medicaid services and Medicare benefits through your current health plan as a dual-eligible beneficiary.
- Upon becoming Medicare eligible, you must enroll in the Medicare D-SNP (Dual Eligible Special Needs Plan) through the same health plan that is providing your Medicaid services to join the IB-Dual program.
- Additional information about IB-Dual can be found in the dedicated section below.
For Providers
Providing Integrated Care for Dual-Eligible New Yorkers
How to Join an Integrated Care Plan Network
Providers wishing to join a health plan´s network may contact the health plan directly to request application procedures and the minimum qualification requirements a provider must meet in order to be considered by the health plan. There is no requirement in New York State law that health plans accept any provider who wishes to join their network. However, health plans must maintain a network that is sufficient to deliver comprehensive services to their enrolled population. The Division of Health Plan Contracting and Oversight (DHPCO) reviews provider networks routinely to ensure enrollee access to health care. Contact DHPCO for problems encountered in obtaining application procedures.
Contracting with a Health Plan
The Division of Health Plan Contracting and Oversight (DHPCO) reviews HMO and IPA provider contracts to ensure that applicable laws and regulations are adhered to. However, the specific terms, services, compensation, risk arrangements, claims procedures, quality assurance requirements, etc. of the contracts are the purview of the contracting parties. Assistance with general contracting issues may be found by contacting professional associations or provider trade organizations.
Medicaid Managed Care Program
Medicaid managed care plans provide comprehensive health care services to enrollees. More specific information on enrollee eligibility and conditions of Medicaid coverage should be obtained by contacting the health plan and/or eMEDNY.
Frequently Asked Questions (FAQ)
- Contact your SHIP (State Health Insurance Assistance Program) at 1-800-701-0501. Representatives provide free, personalized health insurance counseling. SHIP counselors are not affiliated with any health plan.
- Visit Medicare.gov Medicare's web site has tools that can help you compare plans and answer your questions. Click "Find health & drug plans" to compare plans in your area.
- Call 1-800-MEDICARE (1-800-633-4227). Tell them you got a letter saying you have Medicaid now and are going to be eligible for Medicare. Say that you want help with your Medicare choices. This toll-free helpline is available 24 hours a day, 7 days a week. TTY users should call 1-877-486-2048.
- Refer to your Medicare & You Handbook for a list of all Medicare health and prescription drug plans in your area. This handbook is mailed out annually to those eligible for Medicare. If you want to join one of these plans, you can call the plan to get information about their costs, rules, and coverage.
General Information on Integrated Care for Dual Eligible New Yorkers
What is Medicare?
Medicare is a health insurance program that provides healthcare coverage to most people at age 65 and older and to disabled persons under age 65 regardless of income. The program has two parts, Medicare Part A (hospital insurance) and Part B (medical insurance).
What is Medicare Advantage
Medicare Advantage is a managed care program also known as Part C. This is a voluntary program that provides healthcare coverage to people eligible for Medicare Part A and Part B. Eligible individuals may join this program if they choose to, and if available in the area where they live. The program offers coverage of Medicare services and may offer additional benefits such as vision, dental, hearing aids, gym memberships etc. Enrollees must use the plan's doctors to receive their care, except in an emergency or urgent situation.
What is Medicaid?
Medicaid provides health care to people with low or limited incomes to help them with health care costs not covered by Medicare. This may include coverage for long term care services and supports provided in your home or nursing care services provided in a facility.
What is a Health and Recovery Plan (HARP)?
HARP is for individuals with mental health conditions and substance abuse disorders. This plan combines your medical care and behavioral health needs into one plan with additional services.
What is a D-SNP?
A D-SNP (Dual Eligible Special Needs Plan) is a type of Medicare Advantage health plan that is designed to meet the specific needs of dual-eligible beneficiaries. The health plan includes doctor, hospital, and prescription drug coverage and some health plans may also offer extra benefits. These extra benefits may include transportation, home delivered meals, over-the-counter (OTC) drugs, etc. Enrolling in a D-SNP will allow your health plan to coordinate all of your Medicare and Medicaid benefits, including your hospital, medical, prescription drug, and long term services and supports (LTSS). You will be eligible for enrollment into a D-SNP as long as you have both Medicare and Medicaid coverage and continue to live within the D-SNP's service area.
Do I need to join a DSNP?
If you wish to enroll in the MAP or IB-Dual Integrated Care Plans, you must join your health plan's D-SNP. If you choose not to join these Integrated Care Plans, joining a D-SNP is not required, but still an option. Other options include other Medicare Advantage plans or Medicare Fee For Service (also known as Original Medicare). See below for how you can compare your choices.
How can I get help comparing my Medicare plan choices?
It's important to find a plan that covers your doctor visits and prescription drugs. You can get help comparing your plan choices if you:
How to Renew Your Medicaid Eligibility
Now that the public health emergency (PHE) has ended, DOH has begun conducting Medicaid eligibility renewals that were paused during the COVID-19 emergency. Consumers enrolled in the Integrated Benefits for Dually Eligible Enrollees (IB-Dual) Program may continue to be enrolled in MMC/HARP and the aligned Medicare Advantage D-SNP. IB-Dual enrollees must be receiving their Medicare and Medicaid coverage from the same health insurance company. It is important that you follow Medicaid renewal notice instructions to ensure your Medicaid eligibility stays current. Please refer to the following website for more details on eligibility renewal guidance: Important Changes to New York Medicaid, Child Health Plus and the Essential Plan.
We know this unwind period has raised many questions for consumers, caregivers, providers and other stakeholders. To help address some of these concerns, please find the Q&A below for questions about default enrollment and the IB-Dual Program.
Q. Will my health plan remain the same?
A. If you are currently enrolled in the IB-Dual program, you will remain in your MMC/HARP plan with your aligned Medicare Advantage Dual Special Needs Plan (D-SNP). If you are determined no longer Medicaid eligible at your renewal date or you move to a county that does not offer the IB-Dual program, you will be disenrolled to Fee-for-Service Medicaid.
Q. What if I opted out of the Medicare D-SNP and IB-Dual?
A. If you chose not to enroll in the Medicare D-SNP when it was first offered, you may still have an opportunity to enroll in order to remain enrolled in your MMC/HARP plan. Otherwise, you will be disenrolled to Fee-for-Service Medicaid.
Q. What if I am receiving long term care services?
A. If you are receiving long term care services and also enrolled in the IB-Dual program, DOH will take steps to transition you to Managed Long Term Care (MLTC) if you are determined mandatory for that program. DOH or your plan will contact you with more details regarding your coverage options if you are in receipt of long term care services.
Q. Can I still get HARP services?
A. Yes, you will still receive HARP services if you are enrolled in the IB-Dual program. If you have additional questions about HARP services or changing plans, please contact the New York State Office of Mental Health (OMH) at (800) 597-8481.
Q. How can I join or change an IB-Dual plan?
A. If you would like more information about joining or changing to another IB-Dual program, please contact New York Medicaid Choice (NYMC) or reach out to the plan that you would like to join from the chart located in the IB-Dual section. . If you choose to change IB-Dual plans, you will be required to join the new plan's Medicare DSNP. Please be sure to check the service area to make sure the plan is available in your county.
Q. Are there any new plans offering IB-Dual?
A. The chart found on this webpage lists all of the currently available IB-Dual offerings. This chart will be updated as new plans become available.
Information on Default Enrollment
Q. What is Default Enrollment?
A. Default Enrollment is a process to allow a Mainstream Medicaid Managed Care Plan (MMC) or Health and Recovery Plan (HARP) member to be enrolled into their health plan's Medicare Dual Eligible Special Needs Plan (D-SNP) at the time they become eligible for Medicare.
Q. How does Default Enrollment work?
A. Your health plan will send you a notice at least 60 days before you become eligible for Medicare. This notice will let you know that you will be enrolled automatically into your health plan's Medicare D-SNP while remaining in your current Mainstream Medicaid Managed Care Plan (MMC) or Health and Recovery Plan (HARP). You do not have to take any action. The D-SNP coverage will take effect when your Medicare eligibility begins.
Q. What if I do not want to be in the D-SNP? Can I opt-out of Default Enrollment?
A. You do not have to enroll in your plan's D-SNP. You have other options for how to get your Medicare coverage. You may opt-out of Default Enrollment by calling your health plan or by sending a written opt-out request to your health plan. New York Medicaid Choice can connect you with your health plan to opt-out of the D-SNP. Also, New York Medicaid Choice can help answer questions about your Medicaid managed care enrollment, since your Medicaid managed care options change when you become eligible for Medicare.
Q. Why does Anthem/HealthPlus remain suspended on the chart?
A. Anthem/HealthPlus remains suspended for default enrollment until further notice. If you are an existing member of this plan, you will remain enrolled in Anthem/HealthPlus unless you chose to disenroll. The plan will not be accepting any individuals through default enrollment who become newly Medicare eligible and are enrolled in Medicaid managed care. However, a dual consumer can choose to voluntarily enroll in the Anthem/Health Plus IB-Dual Program.
Q. Can I change health plans after being enrolled through default enrollment process?
A. Yes. You should contact your Medicare health plan for more information about disenrollment from the Medicare Advantage D-SNP. If you choose to disenroll, you will no longer have your Medicare and Medicaid coverage through the same health plan. If you have questions about your Medicaid plan options, you can contact New York Medicaid Choice for more information.
Medicaid Advantage Plus (MAP)
Consider MAP
The Medicaid Advantage Plus (MAP) plan is an integrated managed long term care plan that combines Medicaid and Medicare coverage offered through the same health care organization. When you join Medicaid Advantage Plus, you must also enroll in the plan's Medicare Advantage Dual Special Needs Plan (D-SNP) product. The plan will take care of all your long term services and supports needs and other health services. You must choose one of the doctors from the plan to be your Primary Care Provider (PCP).
The plan will cover all Medicaid home care and long term services and supports. You will also get your Medicare services from the plan.
Who qualifies for MAP?
To enroll in the MAP plan, you must be 18 years or older, have full Medicaid and be eligible for Medicare Parts A and B. In addition, you must need at least 120 days or more of long term care services and supports. The MAP plan allows you to remain in the community in your own home while receiving your Medicaid and Medicare services.
What services can I get through MAP?
Services covered in the MAP plan include the following Medicaid and Medicare benefits:
- Health Services at Your Home
- Nurses
- Home Health Aides
- Physical Therapists
- Personal Care
- Help with bathing, dressing, and grocery shopping
- Adult Day Health Care
- Social Day Care
- Nursing Home Care
- Specialty Health
- Audiology
- Dental
- Optometry
- Podiatry
- Physical Therapy
- Mental Health Services
- Other Services
- Home-delivered meals
- Personal emergency response
- Transportation to medical appointments
- Medicare Services
- Doctor office visits
- Specialty care
- Clinic visits, hospital stays
- Mental health services
- X-ray and other Radiology services
- Chiropractic care
- Medicare Part D drug benefits
- Ambulance services
Note: MAP plans also offer over-the-counter (OTC) drug cards and may offer other benefits.
What service areas are MAP plans available in?
To join you must live in an area covered by a MAP plan. Not all areas of New York State have a MAP plan available, so you need to check with New York Medicaid Choice at (888) 401-6582 (TTY users: 1-888-329-1541) to find out if you live in a MAP service area.
Can you disenroll from MAP if it does not work for you?
If you enroll in MAP and then decide it is not the right program for you, you have the option to disenroll.
How can I get more information about MAP?
If you and your loved ones are considering MAP, the next step is to contact New York Medicaid Choice to discuss your interest and start the enrollment process. Remember, when you join the MAP plan, you must also enroll in a Medicare Advantage Dual Special Needs Plan (D-SNP). You can contact the following for more information on your Medicare enrollment choices:
- 1-800-MEDICARE (1-800-633-4227)
- Medicare Rights Center
Additional useful information may also be found in the Medicaid Managed Long Term Care (MLTC) Brochure (PDF).
PACE
Consider PACE
The Program of All-inclusive Care for the Elderly (PACE) is, as its name indicates, a comprehensive managed long term care model designed to cover almost all an eligible individual's health care needs in a single package. Serving individuals age 55 or older, PACE covers your Medicare, Medicaid and Part D prescription drug services, based at a social day center that can provide a full health care clinic, meals, social activities and transportation. Fundamental to the PACE philosophy is keeping individuals independent and living in the community and includes a strong home health care component.
All your care and services are coordinated through a team of professionals focused on your needs and preferences.
Who qualifies for PACE?
As noted, you must be at least 55 years old. PACE services are completely covered for individuals with both Medicare and Medicaid, or who have Medicaid only. In addition, a community health assessment is needed to determine that you meet a certain level of care and that you will continue to need long term care supports and services (LTSS) for more than 120 days.
What services can you count on in PACE?
PACE services include the following:
- A day center and clinic that offer social activities; nursing; physical, occupational, speech and recreational therapies; meals; nutritional counseling; social work and personal care.
- Home health nursing and aide services
- Medical care provided by a team led by your PACE physician working with you and your loved ones to design a complete care package.
- Home health care and personal care.
- Medicare Part D prescription drugs and over the counter supplies.
- Social services.
- Medical specialties, such as audiology, dentistry, optometry, podiatry and speech therapy.
- Respite care for your loved ones.
- End of life care for and pain management.
- Emergency room and 24-hour phone coverage.
- Telehealth.
- Transportation to and from medical appointments.
- Hospital and nursing home care when necessary.
What if I need different services?
Keeping you home and independent may require more than the usual medical services. Unique to the PACE model, the team can authorize many of the supplemental supports you may need, including:
- Over-the-counter supplies and medications
- Home modifications necessary to keep you safe and independent.
- Pastoral and spiritual supports
Do PACE participants qualify for CDPAP?
As a PACE participant you are also eligible to participate in the Consumer Directed Personal Assistant Program (CDPAP) which may allow you to personally direct the hiring of a personal care aide.
CDPAP is a Medicaid option where the consumer has more control over who provides their care and how it is provided. Rather than an agency that manages the hiring and assigning of personal care aides, the consumer and his/her family directly manage these services.
Who decides what care and services I receive?
Ultimately, it's you and your loved ones. To support you in making your health care decisions you will have a team of health care providers, led by your PACE primary care doctor. This team meets on a regular basis with you to develop a plan of care and evaluate your progress. It may also be possible for your current community physician to continue to follow your care at PACE.
What service areas are PACE plans available in?
To join you must live in an area covered by a PACE center. Not all areas of New York State have PACE, so you need to check with New York Medicaid Choice at (888) 401-6582 (TTY users: 1-888-329-1541) to find out if you live in a PACE service area.
What is a PACE Center?
Choosing PACE gives you the resources of both the PACE center and full service health clinic.
- At the center, you can choose to come and benefit from maintenance therapy, social and recreational activities, meals, transportation, and personal care.
- At the clinic, you can benefit from a complete, fully staffed health facility with doctors, nurses and therapists.
How did PACE start?
In considering if PACE is right for you, a little bit of history may help understanding the PACE model. PACE isn't new, but the concept may be new to a lot of folks. The program was started in the 1970s on the West Coast by ethnic communities that were seeking an alternative to nursing home care for their loved ones. So, they designed a model that provides all the services of a nursing home but does so while keeping seniors at home in their communities. The popularity of the model is such that it soon spread across the country.
Can you disenroll from PACE if it doesn't work for you?
PACE may not be for everyone. If you enroll in PACE and then decide it isn't the right program for you, you can disenroll at any time, with no lock-in period.
How can I get more information about PACE?
If you and your loved ones are considering PACE, the next step is to contact New York Medicaid Choice to discuss your interest and start the process. A PACE representative will also want to meet with you and describe their program in detail, perhaps arrange a center visit and further help you make your decision.
Additional useful information may also be found in the Medicaid Managed Long Term Care (MLTC) Brochure (PDF).
IB-Dual - (Integrated Benefits for Dually Eligible Enrollees)
Consider IB-Dual
The Integrated Benefits for Dually Eligible Enrollees (IB-Dual) is the newest integrated care plan option available for individuals who have both Medicare and Medicaid coverage. The IB-Dual program is for individuals who do not require long term care services and supports. The program allows an individual who is becoming newly Medicare eligible to remain in their Mainstream Medicaid Managed Care Plan or Health and Recovery Plan (MMC/HARP) and enroll in the aligned Medicare D-SNP.
How Can I Join the IB-Dual Program?
Enrollment in the IB-Dual program occurs when an individual in MMC/HARP is also enrolled in the Medicare D-SNP of the same healthcare organization that provides one's Medicaid services. When a MMC/HARP member becomes newly eligible for Medicare, the individual will be enrolled into the aligned Medicare D-SNP through a Centers for Medicare and Medicaid Services (CMS) procedure called "default enrollment". The following describes the default enrollment process for newly dual eligibles.
What is Default Enrollment?
Default Enrollment is a process that allows a Mainstream Medicaid Managed Care Plan (MMC) or Health and Recovery Plan (HARP) member to be enrolled into their health plan's Medicare Dual Eligible Special Needs Plan (D-SNP) at the time they become Medicare eligible. To learn more about Medicare D-SNPs, please see the FAQ section.
Once you are enrolled in the aligned Medicare D-SNP of your MMC/HARP, you become a member of the IB-Dual program. This integrated care plan allows you to receive your Medicaid and Medicare benefits through one health plan that will coordinate all of your services.
Do All MMC/HARP plans offer the IB-Dual Program?
No. Not all MMC/HARP plans offer the IB-Dual Program. To find out which plans offer IB-Dual, you can review the list of approved health plans on this webpage or contact your MMC/HARP plan directly for more information.
Do I have to Join an IB-Dual Program?
No. You do not have to join the IB-Dual Program. You may opt-out of the default enrollment process if you do not want to be enrolled into the aligned Medicare D-SNP. However, you will not be able to remain in your MMC/HARP if you opt out, and instead, you will be disenrolled to Medicaid fee-for-service.
Can I Join IB-Dual at another time?
As a dual eligible enrollee, there are other options available for joining the IB-Dual program outside of the default enrollment process. The next section will tell you more about other options for joining the IB-Dual program.
Additional Enrollment Options into IB-Dual:
In addition to Default Enrollment, and even if a plan's Default Enrollment is paused, dual eligibles who are not newly Medicare eligible, have options for enrollment into IB-Dual. This includes voluntary enrollment into the MMC/HARP from Medicaid Fee-for-Service (FFS) after they have joined the aligned D-SNP or joining the aligned D-SNP if they are still in MMC/HARP.
For more information about health plans who have been approved to use the Default Enrollment process please see the table below.
- Members in need of LTSS will be enrolled into MAP through the Default Enrollment process.
- LTSS Default Enrollment Notice: Long Term Care Services and Supports Member Notice for Default Enrollment into Medicare D-SNP and Medicaid Integrated Care Plan.
- Members who do not need LTSS will be enrolled into the IB-Dual program through the Default Enrollment process.
- Non-LTSS Default Enrollment Notice: Non-Long Term Care Services and Supports Member Notice for Default Enrollment into Medicare D-SNP and Medicaid Integrated Care Plan.

Integrated Plan Offerings - 2026
Integrated Benefits for Dually Eligible Program (IB-Dual) Offerings - 2026
| Plan Name | H# / PBP# | Product Type | Service Area | IB-Dual Status | Default Status | Medicaid FFS Transition to IB-Dual |
|---|---|---|---|---|---|---|
| Anthem/HealthPlus* | H8432 (041) |
MAP | Bronx, Kings, Nassau, New York, Orange, Queens, Richmond, Rockland, Suffolk, and Westchester (10) | Suspended | ||
| Anthem/HealthPlus* | H8432 (042) |
MMC/HARP | Bronx, Kings, Nassau, New York, Orange, Queens, Richmond, Rockland, Suffolk, and Westchester (10) | Active | Suspended | Yes |
| Excellus Health Plan | H7524 (001/003) | MMC/HARP | Broome, Erie, Herkimer, Livingston, Monroe, Oneida, Onondaga, Ontario, Orleans, Otsego, Seneca, Wayne, Yates (13) | Active | Active (as of 2/1/2024) |
Yes |
| Fidelis | H5599 (013-001) | MMC/HARP | Albany, Allegany, Bronx, Broome, Cattaraugus, Cayuga, Chemung, Chenango, Clinton, Columbia, Cortland, Delaware, Dutchess, Erie, Essex, Franklin, Fulton, Greene, Hamilton, Herkimer, Kings, Lewis, Montgomery, Nassau, New York, Niagara, Oneida, Onondaga, Orange, Orleans, Oswego, Otsego, Putnam, Queens, Rensselaer, Richmond, Rockland, Saratoga, Schenectady, Schoharie, Schuyler, Seneca, St. Lawrence, Steuben, Suffolk, Sullivan, Tioga, Ulster, Warren, Washington, Westchester, Wyoming, Yates Genesee, Jefferson, Livingston, Madison, Monroe, Ontario, and Wayne (60) |
Active | Active | Available in all counties except for: Genesse, Jefferson, Madison, Monroe, Ontario and Wayne |
| Fidelis | H5599 (013-002) | MMC/HARP | Bronx, Kings, Nassau, New York, Queens, Richmond, Rockland, Suffolk, Westchester | Active | Active | Yes |
| Fidelis | H5599 (003) | MAP | Albany, Allegany, Bronx, Broome, Cattaraugus, Cayuga, Chemung, Chenango, Clinton, Columbia, Cortland, Delaware, Dutchess, Erie, Essex, Franklin, Fulton, Greene, Hamilton, Kings, Lewis, Montgomery, New York, Niagara, Oneida, Onondaga, Orange, Orleans, Oswego, Otsego, Putnam, Queens, Rensselaer, Richmond, Rockland, Saratoga, Schenectady, Schoharie, Schuyler, Seneca, St. Lawrence, Steuben, Sullivan, Tioga, Ulster, Warren, Washington, Wyoming, Yates Genesee, Jefferson, Livingston, Madison, Monroe, Ontario and Wayne (56) |
Active | ||
| Healthfirst | H3359 (034) | MAP | Bronx, Kings, New York, Queens, Richmond, Nassau, Westchester, Orange, Rockland, Sullivan (10) | Active | ||
| Healthfirst | H3359 (021) | MMC/HARP | Bronx, Kings, Nassau, New York, Orange, Queens, Richmond, Rockland, Suffolk, Sullivan, Westchester (11) | Active | Active | Yes |
| Health Insurance Plan of Greater New York (dba EmblemHealth) | H5991 (013) | MMC/HARP Only | Bronx, Kings, New York, Queens, Richmond, Nassau, Suffolk, Westchester (8) | Active | Active | |
| MetroPlus | H0423 (001) | MMC/HARP | Bronx, Kings, New York, Queens, Richmond (5) | Active | Active | Yes |
| MetroPlus | H0423 (007) | MAP | Bronx, Kings, New York, Queens, Richmond (5) | Active | ||
| Molina Healthcare of New York | H5992 (010) | MMC/HARP | Bronx, Kings, Nassau, New York, Orange, Queens, Richmond, Rockland, Westchester (9) | Active | Active | |
| Molina Healthcare of New York | H5992 (007) | MAP | Bronx, Kings, Nassau, New York, Orange, Queens, Richmond, Rockland, Westchester (9) | Active | ||
| MVP Health Plan | H3305 (034) | MMC/HARP | Albany, Columbia, Dutchess, Greene, Monroe, Orange, Putnam, Rensselaer, Rockland, Saratoga, Schenectady, Sullivan, Ulster, Westchester (14) | Active | Active | |
| United Health Care | H3387 (013) | MAP | Erie, Genesee, Monroe, Niagara, Orleans, Wyoming | Active | ||
| United Healthcare | H3387 (014) | MMC/HARP Only | Albany, Bronx, Broome, Cayuga, Chautaugua, Chemung, Chenango, Clinton, Columbia, Dutchess, Erie, Essex, Franklin, Fulton, Genesee, Greene, Herkimer, Jefferson, Kings, Lewis, Livingston, Madison, Monroe, Nassau, New York, Niagara, Oneida, Onondaga, Ontario, Orange, Orleans, Oswego, Queens, Rensselaer, Richmond, Rockland, Schenectady, Seneca, St. Lawrence, Suffolk, Tioga, Ulster, Warren, Wayne, Westchester, Wyoming, Yates (47) | Active | Active | Yes |
* Members already enrollend in this plan will remain enrolled and do not need to make any changes.
Integrated Duals Policy
Guidance for Health Plans
Instructions for Completing the Notice of Denial of Medical Coverage (or Payment) CMS-10003-NDMCP for the Integrated Benefits for Dually Eligible Enrollees (IB-Dual) Program - (Web) - (PDF)
Duals Dental Policy
As of January 1st, 2025, the New York State Department of Health will require D-SNP plans to provide dental benefits as a Medicare supplemental benefit. Please see the Frequently Asked Questions document linked below for more informaiton.
Follow Us