Community First Choice Option (CFCO)
LOCAL DISTRICT SOCIAL SERVICE OFFICES
MMIS APPLICATION TRAINING
February 1, 2019
Agenda
- Community First Choice Option Overview
- ADM´s – 4/1/18, 4/1/19 and 7/1/19
- The Services Available for Eligible Individuals – 4/1/18 and 7/1/19
- Local Districts Responsible for Following Populations
- The Consolidated Children´s 1915c Waiver
- The Service Delivery and Payment Methodology
- Selection of District Contacts for Application processing, eMedNY Claiming
- Questions and Concerns
Overview
- Community First Choice Option (CFCO) became available to all states under the Affordable Care Act of 2010
- This option provides a 6 percent increase in federal matching payments to states to expand and enhance Medicaid State Plan (State Plan) home– and community–based attendant services to individuals in need of long–term care for Activities of Daily Living (ADLs), Instrumental Activities of Daily Living (IADLs) and health–related tasks
- The LDSS will now be required to administer the CFCO through adherence to the State Plan, 42 CFR Part 441, and State–issued guidance, which will ensure statewide consistency when authorizing or reauthorizing CFCO services
- All services must be provided statewide in a manner that provides such services in the most integrated setting appropriate to the individual´s needs, and without regard to the individual´s age, type or nature of disability, severity of disability, or the form of home and community–based attendant services and supports that the individual requires to lead an independent life
ADM´s: 4/1/18; 4/1/19 and 7/1/19
- The initial CFCO ADM, dated 4/1/18, has just completing a second period of review and comments from the Local Districts
- It will be ready for Statewide distribution as soon all comments are addressed and it completes the internal process necessary for all ADMs
- This initial ADM is meant to introduce the process for identifying eligibility for individuals seeking CFCO services and the work instructions for adding and closing Recipient/Restriction Exceptions codes attached to CFCO eligibility
- A draft copy of the 4/1/18 ADM is available here
- This draft copy does not contain the current comments
- The next phase in changes for the LDSS is the pending approval of the Children´s Consolidated 1915c Waiver, scheduled for 4/1/19
- An ADM will be released shortly
- Pending CMS approval, under the 4/1/19 Consolidated Children´s 1915c Waiver, CFCO State Plan Services will be uniformly available to eligible individuals in the Consolidated Children´s 1915c Waiver
- These services, Assistive Technology (AT), Environmental Modifications (E– Mods) and Vehicle Modifications (V–Mods), are currently not available in all of the individual waivers
- E–Mods, V–Mods and AT will become available on 4/1/19 and will be the responsibility of the Local Districts to authorize and provide these services for any eligible individual enrolled in the Consolidated Children´s 1915c
- Reimbursement methodology is currently being reviewed and will be shared as soon as it is finalized
- The focus is to change as little as possible to the current process during this three–month interim period
- For individuals who are enrolled in both the new 1915c Children´s Consolidated Waiver and in a Managed Care plan, the Local Districts will be responsible for providing these services until these services are implemented into the Managed Care benefit package on 7/1/19
- The 7/1/19 ADM is in production and every effort is being made to have this out the Local Districts as soon as possible
- This ADM will contain the new permissible services that will be available to any eligible individual in Fee for Service, Managed Care, Managed Long Term Care or enrolled in waiver programs that must utilize State services before waiver services
Current CFCO Services
- Consumer Directed Personal Assistance Services (CDPAS)
- Home Health Aide
- Homemaker/Housekeeper (Personal Care Level 1)
- Personal Care Level 2
- Personal Emergency Response System (PERS)
- Non–Emergency Medical Transportation (NEMT)
Implementation of Additional CFCO Services
- Implementation for July 1, 2019:
- Assistive Technology (At)
- Environmental Modification (E–Mod)
- Vehicle Modification (V–Mod)
- Moving Assistance
- Community Transitional Services (CTS)
- Skill Acquisition Maintenance and Enhancement (SAME)
- Home–Delivered/Congregate Meals
- For the 7/1/19 services, only Skill Acquisition Maintenance and Enhancement (SAME)/Community Habilitation currently has an established Provider Network who can bill services directly to eMedNY
- On 7/1/19, it will be the responsibility of the Local Districts to provide the remaining services on the list
- Guidance documents for these services are being finalized and are posted to the CFCO website
- The CFCO SPA identifies the fiscal cap for five of the seven services
- AT, E–Mods and V–Mods has an annual limit of $15,000
- Community Transition and Moving Services have a one–time allowance of $5,000
Local Districts Responsible for Following Populations
- The following two slides outline populations that will seek services from the Local Districts
- The following slide shows current waivers that include some/all of the new CFCO services
- These waivers include DOH Care at Home (CAH 1/11); OPWDD (CAH); OCFS Bridges to Health SED (B2H SED); OCFS Bridges to Health Medically Fragile (B2H MF); OCFS Bridges to Health DD (B2H DD) and OMH SED
- Pending CMS approval, on 4/1/19, these six individual waivers will be consolidated under DOH into the Consolidated Children´s 1915c Waiver:
- AT, E–Mods and V–Mods are included in the 4/1/19 waiver
- Children will be seeking these services from the LDSS effective 4/1/19
| CFCO Services Available in 1915(c) Waiver Services Today | ||||||||
|---|---|---|---|---|---|---|---|---|
| Current Services that will Remain in Effect Under 1915(c) with Implementation of CFCO Services | Current Children´s 1915(c) Waivers Effective Now Thru 3/31/19* | *Effective 4/1/19 with CMS Approval | ||||||
| CFCO Services | MLTC | TBI Waiver |
NHTD Waiver |
OPWDD Comprehensive Waiver |
OPWDD CAH |
DOH Care at Home (CAH) I/II |
OCFS B2H (MF, DD, SED) |
Consolidated Children´s Waiver |
| Assistive Technology (AT) | X | X | X | X | X | X | ||
| Vehicle Modifications | X | X | X | (Part of AT) | X | X | X | |
| Environmental Modifications | X | X | X | X | X | X | X | X |
| Moving Assistance | X | |||||||
| Community Transitional Services | X | X | X | |||||
| Home–Delivered/ Congregate Meals | X | X | ||||||
| Skill Acquisition Maintenance and Enhancement (SAME)/ Community Habilitation(CH) | X | X | ||||||
- The following slide provides a breakdown of the 7/1/19 CFCO services and where waiver individuals will go to request those services
- With the exception of the current OPWDD Care at Home children, OPWDD eligible individuals will continue to go through their regional DDRO´s
- Care at Home children will now be part of the Consolidated Children´s 1915c Waiver and will seek services through the LDSS
- Also, because home–delivered and congregate meals are not included in the comprehensive OPWDD Waivers, individuals seeking those services will apply through the LDSS
- Individuals enrolled in Traumatic Brain Injury (TBI) and the Nursing Home Transition and Diversion (NHTD) Waivers will continue to utilize their RRDC Centers.
- Please note that the limits outlined in the SPA for the services being implemented on 7/1/19 may be overridden with a documented medical necessity and a separate authorization from DOH. There will be more information available shortly.
| CFCO Service Authorization for Fee–for–Service individuals – July 1, 2019 (individuals NOT Enrolled in Managed Care Plan) |
|||||||
|---|---|---|---|---|---|---|---|
| FFS Population | AT | E–MOD | V–MOD | SAME/CH | Home/ Congregate Meals |
CTS | Moving Assistance |
| OPWDD Comprehensive Waiver | DDRO | DDRO | DDRO | DDRO | LDSS | DDRO | LDSS |
| OPWDD Individuals with RE 95 not in the OPWWD Waiver, (applies to adults and children) | DDRO** | DDRO | DDRO | DDRO | LDSS | DDRO | DDRO |
| 1915(c) Consolidated Children´s Waiver * | LDSS | LDSS | LDSS | LDSS | LDSS | LDSS | LDSS |
| Nursing Home Transition and Diversion Waiver | RRDC*** | RRDC | RRDC | LDSS | RRDC | RRDC | RRDC |
| Traumatic Brain Injury Waiver | RRDC | RRDC | RRDC | LDSS | LDSS | RRDC | LDSS |
| All other FFS individuals | LDSS | LDSS | LDSS | LDSS | LDSS | LDSS | LDSS |
* Upon CMS approval will take effective April 1, 2019 – Service authorization will be the same as CFCO service authorization
** Developmental Disabilities Regional Office
***Regional Resource Development Center
The Service Delivery and Payment Methodology
- After careful review of available reimbursement methodologies currently available to the Local Districts, the decision was made to facilitate the enrollment of Local Districts into eMedNY
- This will provide the fastest and most direct pathway for reimbursements to the Local Districts
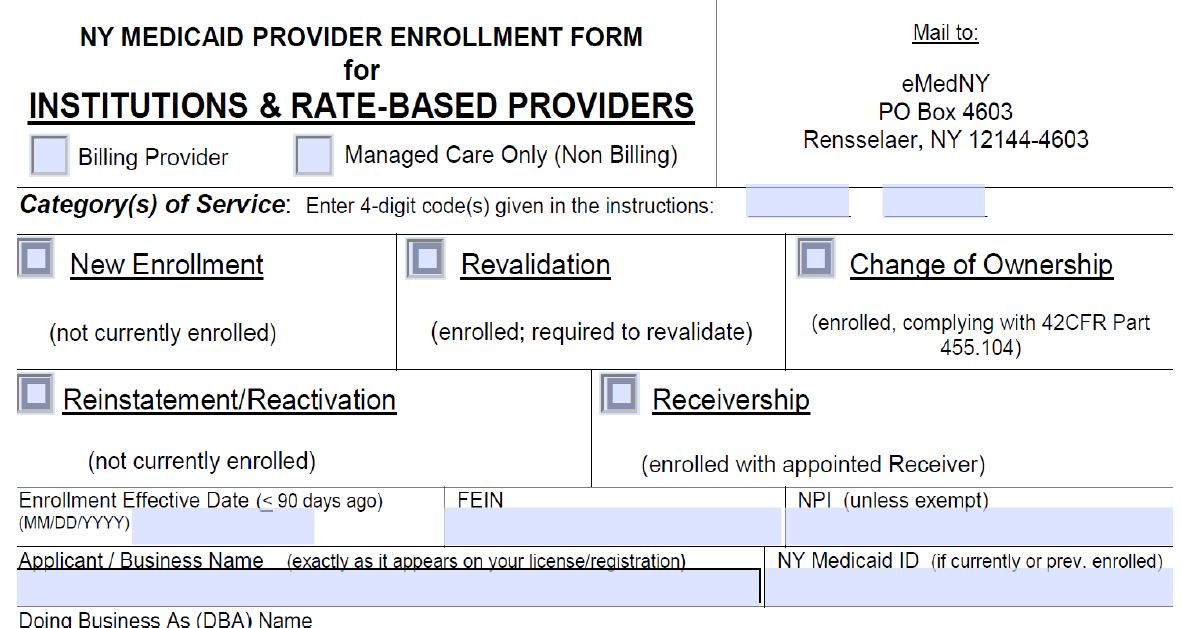
- Local Districts will be asked to complete a new eMedNY Provider Enrollment form to obtain a new MMIS provider identification number, specific to CFCO
- Local Districts currently have MMIS numbers associated with County Health Departments, County Nursing Homes, Special Projects, etc.
- The process for issuing a MMIS number associated only with CFCO services will be done through collaboration with MLTC and Provider Enrollment

MMIS Process
- Provider Enrollment will be adding a new provider type– LDSS–CFCO. Once this provider type has been added to the current list, applications will be available for completion
- We will be providing upcoming webinars to review completion of the application and all of the fields that need to be completed
- In a modified process, completed applications will be sent to an MLTC BML rather than submitting them directly to eMedNY
- Staff at MLTC will be reviewing the applications for missing or incorrect data and contacting the Local District directly to obtain the necessary information
- Completed applications will be submitted to eMedNY from MLTC
- This process is to assist in a faster turnaround time for the applications
- We have requested that the standard application fee of $500.00 for new applications be waived for all Local District submissions
- Please do not contact Provider Enrollment or start the application process until you are directed to do so by Managed Long Term Care.
- It is very important that the application process be done through MLTC. We are collaborating with Provider Enrollment and eMedNY to make this process as smooth and efficient as possible. PLEASE do not contact Provider Enrollment independently as this is a special project and not everyone at Provider Enrollment will be able to assist you.
Selection of Local District Contacts for Application Processing, eMedNY Claiming
- Today´s webinar was directed to the Local District Commissioners to provide an overview of the roles and responsibilities that the Local Districts are being asked to assume
- Please provide contact staff in the Local District that will assist in both the MMIS application process and also for claim submissions to eMedNY
- We are asking that you provide any and all names, e–mails and direct telephone numbers for your contact staff
- Please send the contact information for your County and direct all inquires pertaining to the MMIS application process to: LDSS.MMIS.Applications@health.ny.gov
Contact information
- Please be sure to forward the contact information from your district to: LDSS.MMIS.Applications@health.ny.gov
- We are requesting that this information be returned to us by Friday, February 15th
- We are requesting that the contact information include:
- Contact´s name
- Contact´s e–mail
- Contact´s Telephone
- Contact´s Fax number
Questions and Concerns
- As this is a new process for both the Districts and for DOH, we ask your patience in establishing the guidelines for implementation of these services and the reimbursement methodology.
- We ask that you utilize today´s information to begin a discussion of questions and answers for this process. We will request assistance from all areas of DOH for support and responses to questions that you will most certainly have.
Follow Us