Community First Choice Option (CFCO)
Role of LDSS in Implementing Community First Choice Option (CFCO) Services
February 20, 2019
What is the Community First Choice Option (CFCO)?
- CFCO is not a program – CFCO is a set of personal attendant services (e.g., home– and community–based services and supports) authorized under the Affordable Care Act (Affordable Care Act, PL 111–148, Sec. 2401)
- CFCO provides additional federal money to expand home– and community–based services and supports to individuals in need of long term care help with everyday activities and health–related tasks that can be performed by an aide or direct care worker (for example, Activities of Daily Living [ADLs] and Instrumental Activities of Daily Living [IADLs])
- CFCO allows long term services and supports that were previously only available through 1915 waivers (e.g., vehicle modifications) to be Medicaid State Plan Services
- Those services will be included in the Mainstream, MLTC Partial Plan, PACE, and MAP benefit packages
- CFCO is available to all Medicaid members that meet the CFCO eligibility criteria
- CFCO is designed to be person centered and consumer driven, and intended to maximize independence and participation in the community
CFCO Services
- Current CFCO Services:
- Consumer Directed Personal Assistance Services (CDPAS)
- Home Health Aide
- Homemaker/Housekeeper (Personal Care Level 1)
- Personal Care Level 2
- Personal Emergency Response System (PERS)
- Non–Emergency Medical Transportation (NEMT)
- Implementation for July 1, 2019: o Community Transitional Services (CTS)
- Assistive Technology (AT) o Skill Acquisition Maintenance and Enhancement (SAME)
- Environmental Modification (E–Mod)
- Vehicle Modification (V–Mod)
- Moving Assistance
- Home–Delivered/Congregate Meals
Points of Clarification
- The LDSS is not responsible for setting any rates for CFCO services
- The rate range provided for congregate and home–delivered meals is based on the contract
- Any LDSS contract with a meal provider that is set at a rate within the posted rate range can be billed
- Rate range is posted here.
- There are no changes for the LDSS with respect to how they authorize non– emergency medical transportation (NEMT)
Role of LDSS in 7/1/19 CFCO Service Provision Limited to Certain Fee–for–Service Recipients
- The role of the LDSS in CFCO service provision outlined in this webinar applies to the seven CFCO services authorized on July 1, 2019
- The role of the LDSS in CFCO service provision (i.e., oversight, assessment, reassessment and service planning) is limited to certain Medicaid members in Fee–for–Service (FFS) that have an assessed need for CFCO and are currently the responsibility of the LDSS
- Not all of the recipients will meet CFCO eligibility requirements and need one or more of the specific CFCO services that will be implemented on July 1, 2019
- For individuals enrolled in the Traumatic Brain Injury (TBI) or Nursing Home Transition and Diversion (NHTD) 1915(c) Waivers, CFCO service provision will be the responsibility of the Regional Resource Development Center (RRDC)
- For most individuals eligible for Office for People with Developmental Disabilities (OPWDD) services (RE 95), authorization for certain CFCO service will be the responsibility of the Developmental Disabilities Regional Office (DDRO) or its delegate
| CFCO Service Authorization for Fee-for-Service individuals – July 1, 2019 (Individuals NOT Enrolled in Managed Care Plan) | |||||||
|---|---|---|---|---|---|---|---|
| FFS Population | AT | E–MOD | V–MOD | SAME/CH | Home/ Congregate Meals | CTS | Moving Assistance |
| OPWDD Comprehensive Waiver | DDRO | DDRO | DDRO | DDRO | LDSS | DDRO | DDRO |
| OPWDD Individuals with RE 95 not in the OPWDD Waiver (applies to adults and children), and not in the Consolidated Children's Waiver*** | DDRO* | DDRO | DDRO | DDRO | LDSS | DDRO | DDRO |
| Nursing Home Transition and Diversion (NHTD) Waiver | RRDC** | RRDC | RRDC | LDSS | RRDC | RRDC | RRDC |
| Traumatic Brain Injury (TBI) Waiver | RRDC | RRDC | RRDC | LDSS | LDSS | RRDC | LDSS |
| All other FFS individuals not in OPWDD Comp Waiver, NHTD, TBI, or in Managed Care Plan * | LDSS | LDSS | LDSS | LDSS | LDSS | LDSS | LDSS |
| * Developmental Disabilities Regional Office **Regional Resource Development Center ***The Department will provide separate guidance, including an ADM and Webinar, on the role of the LDSS in providing AT, V-Mods, E-Mods, and SAME to children enrolled in the 1915(c) Children's Consolidated Waiver for the period April 1, 2019 through June 30, 2019, and for any child in the 1915(c) Consolidated Waiver that may be eligible for AT, V–Mods, E–Mods, and SAME on and after July 1, 2019 when CFCO services are launched |
|||||||
1915(c) Consolidated Children’s Waiver
- The Care at Home I/II 1915 (c) Waiver is amended to become the Consolidated Children’s Waiver
- This amendment is pending CMS approval with an effective date of April 1, 2019
- The Waiver will now combine all existing 1915 (c) children’s service target groups into one population, combining children who are medically fragile, Seriously Emotionally Disturbed (SED), developmentally disabled, medically fragile and developmentally disabled and in foster care into one 1915 (c) Waiver
- The Consolidated Children’s Waiver authorizes an array of HCBS that include AT, V– Mods, E–Mods and SAME (Community Habilitation)
- The service definitions under the Consolidated Children's Waiver for AT, V–Mods, E– Mods and SAME (Community Habilitation) are aligned with the CFCO services
- Pending CMS approval, effective July 1, 2019, most children in the Consolidated Children’s Waiver will be enrolled in Managed Care, and service authorization for these services will be the responsibility of the Managed Care plans
- The Department will provide separate guidance, including an ADM and webinar, on the role of the LDSS in providing AT, V–Mods, E–Mods, and SAME to children enrolled in the 1915(c) Children's Consolidated Waiver for the period April 1, 2019 through June 30, 2019, and for any child in the 1915(c) Consolidated Waiver that may be eligible for AT, V–Mods, E–Mods, and SAME on and after July 1, 2019 when CFCO services are launched
LDSS Will Not Provide 7/1/19 CFCO Service Provision for Members Enrolled in Plans
- Effective July 1, 2019, all CFCO services will be included in the Mainstream, MLTC Partial Plan, MAP, and PACE benefit packages
- For individuals enrolled in Mainstream, MLTC Partial Plan, MAP or PACE Plans, their respective Managed Care Plan (not the LDSS), will be responsible for CFCO service provision (i.e., oversight, assessment, reassessment, service planning, and authorization)
LDSS Role for FFS Recipients
- As described in more detail in the following slides, for the LDSS CFCO FFS recipients (i.e., those identified in the previous slides) LDSS will assist with CFCO service provision including:
- CFCO eligibility determination
- Authorization
- Service planning
- See 19–OHIP/ADM–01, Community First Choice Option for additional details, go here.
LDSS Role: CFCO Eligibility Determination
- An individual eligible to receive CFCO services must fulfill all of the following criteria:
- Be Medicaid eligible for community coverage with community–based long term care (with or without a spend down), or be Medicaid eligible for coverage of all care and services
- Reside in his/her own home, or the home of a family member
- Have an assessed institutional level of care
- The operationalization of CFCO has no impact on the current Medicaid eligibility determination process
- Individual’s Medicaid eligibility may not be dependent on:
- Spousal impoverishment post–eligibility rules
- The Special Income Standard for Housing Expenses
- Family of one budgeting for a child participating in a HCBS Waiver (The State is seeking CMS approval to allow family of one children under the proposed consolidated Children’s 1915(c) Waiver to be eligible for CFCO services)
Level of Care
- An initial determination must be made that the individual seeking CFCO services requires the level of care (LOC) provided in a hospital, a nursing facility, an Intermediate Care Facility for Individuals with Intellectual Disabilities (ICF/IID), an institution providing psychiatric services for individuals under age 21, or an institution for mental diseases for individuals age 65 or over
- LOC for individuals between ages 21 and 65 needing psychiatric services is determined using hospital, ICF/IDD or nursing facility LOC criteria
- Please note that once initial LOC eligibility is determined for these individuals, a LOC determination must be made at least annually thereafter by utilizing the various State– approved assessment tools in use across disability populations in the State
- For example, State–approved assessments include the Community Assessment and the Pediatric Assessment in the Uniform Assessment System (UAS)
- A score of five or more on each of these tools would indicate a member meets LOC criteria
Residential Determination
- After it is determined that the individual meets the CFCO Medicaid eligibility requirement, a residential status determination must be made
- Only an individual living in his/her own home or the home of a family member is eligible for CFCO services
- Individuals who live in congregate settings, institutional settings, or provider owned and/or controlled properties are not eligible to receive CFCO services
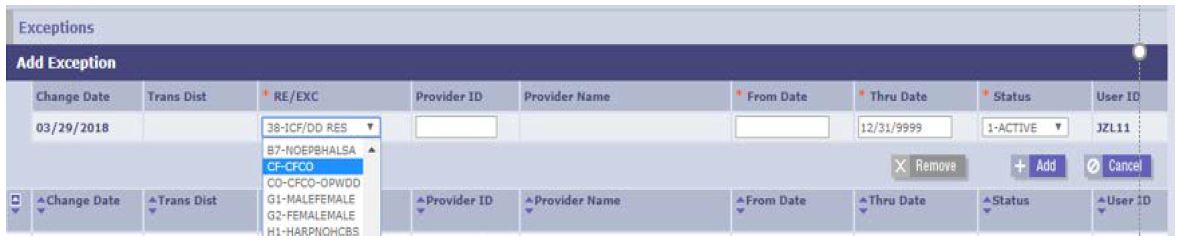
LDSS Role: RR/E Code Placement and Maintenance
- The placement of the CFCO RR/E code on a consumer eligibility file is completed after a consumer has been determined eligible for CFCO
- LDSS is responsible for the placement and maintenance of the ‘CF’ RR/E code, which will be completed through eMedNY Thin Client
- OPWDD will be responsible for the placement and maintenance of the ‘CO’ RR/E code for Medicaid FFS individuals identified as OPWDD
- Step–by–step instructions can be found in Attachment IV: Placement and Maintenance of CFCO RRE Code – LDSS of the recently released.
LDSS Role: Functional Needs Assessment
- The functional needs assessment (FNA) must be completed face–to–face and where the individual currently resides
- The individual can request the participation of anyone that s/he wants involved in the FNA
- A registered nurse, either employed by the LDSS or an approved provider agency or directly contracted by the LDSS or the State, will conduct the FNA
- Various State–approved assessment tools are in use across the State to assess an individual across the critical domains of functional status, health condition, and cognition
- Currently, the Community Assessment located in the Uniform Assessment System (UAS) is the most widely used
- The UAS provides the nurse with an FNA tool that will record the individual’s needs, strengths, preferences and goals for maximizing independence and community integration, as well as an assessment of risk that identifies potential risks and vulnerabilities
- The results of the FNA will inform the development of the Person–Centered Plan of Care (POC) and authorization for CFCO Services
CFCO Service Parameters
- Assistive Technology
- Environmental Modification
- Vehicle Modification
- Home Delivered/Congregate Meals
- These services must increase an individual’s independence or substitute for human assistance, where human assistance would otherwise have been provided
- All CFCO services must be specifically identified in the individual’s Person– Centered Plan of Care (POC)
- Community Transitional Services (CTS)
- Moving Assistance (MA)
- CTS and MA are only available to individual’s transitioning from institutional setting (e.g., nursing home, immediate care facility) to community–based settings
- CTS and MA may not be used to fund transitions from one community–based setting to another
- All services must be specifically identified in the individual’s Person–Centered Plan of Care (POC)
LDSS Role: Person–Centered Service Planning
- A Person–Centered Plan of Care (POC) will be developed with the individual following completion of the FNA and will identify the individual’s needs and goals related to living independently in the community
- The individual can request the participation of anyone that s/he wants involved in the person–centered planning process
- The Person–Centered POC will be informed by the FNA, which identifies the individual’s needs related to ADLS, IADLS and health–related tasks, and must specifically identify all services to be provided to address these needs
- Please see the Person–Centered Service Planning Guidelines for Medicaid Managed Care Plans and Local Departments of Social Services
- The Person–Centered Planning Guidelines are intended to provide information regarding the requirements for the Person–Centered Service Planning (PCSP) process for individuals receiving services through FFS from the LDSS
- The Department has provided a PC POC template for the LDSS to utilize.
- The use of this template is not mandatory – you may use a current POC or another template, as long as it meets the PCSP requirements
LDSS Role: Service Authorization
- Following the assessment and service planning process, which aligns needed services with identified functional need for assistance with ADLS, IADLS and/or health–related tasks:
- The LDSS must provide written notification of initial authorization, reauthorization or denial of the requested CFCO services
- This notification must be completed in its entirety and provide the required information regarding fair hearings
- For the CFCO services already authorized by the LDSSs, including personal care services and consumer–directed personal assistant services, the LDSS must use the existing service notices for these CFCO services
- For the July 1, 2019 services, including AT, E–Mods and V–Mods, the Department will be issuing new notices for the LDSS to use for these services
- As required, the Notice of Decision (NOD) must be provided to the individual and, if applicable, the individual’s designated representative
- A copy of the NOD must be maintained in the individual’s case record
Payment Models for Certain CFCO Services
- LDSS have expressed concern over the use and reliance upon Schedule E (which requires LDSS to upfront payments and later receive reimbursement) to process payments for E–Mods, V–Mods, and AT (i.e., the providers are not typically Medicaid providers that can directly bill the State)
- The State has made progress in its efforts to explore alternative options including a Special Payment Vouchering process that will avoid the need for the LDSS to make upfront payments and will provide additional information and guidance as soon as possible
- In the meantime, options to reduce or eliminate timeframe for reimbursement include:
- LDSS Seeking MMIS provider number
- Provides a pathway to accelerate the time period for reimbursement
- MMIS application fee will be waived for LDSS
- Training was provided on the MMIS application process on February 2, 2019
- Most counties just need an updated category of service
- LDSS may contract with other Medicaid–enrolled providers that have the capacity to arrange and pay for the new CFCO services
- LDSS Seeking MMIS provider number
CFCO Contracting Process
- Service Authorization Guidelines for AT, E–Mods, and V–Modsinclude information on obtaining bids and circumstances where that might not be necessary
- The Department is in the process of developing an example contract, which the LDSS may find helpful to use as a model during the contracting process with providers for AT, E–Mods and V–Mods
- This will be finalized shortly and posted on the CFCO homepage
Home and Vehicle Modification Usage – Some Context
- Home and Vehicle Modification now available under CAH I/II Waivers
- Statewide usage in calendar year 2018 – a total of 202 home and vehicle projects requested – Statewide average of 16 projects per month
- Home Modifications:
- 164 project requests
- Types of requests: Bathroom modifications, wheelchair ramps, platform–lifts, widen doors, stair lifts, ceiling track systems, generators, railings
- Vehicle Modifications:
- 38 vehicle modification requests
- Types of requests: Van ramps and BraunAbility rotating seat lift
- Home Modifications:
Money Follows the Person (MFP)
- If a CFCO–eligible individual is currently in an institutional setting (nursing home, Intermediate Care Facility, etc.) and would like to reside in a home in the community (i.e., qualified community–based setting), s/he may be access Community Transition and Moving Assistance CFCO services
- CTS and Moving Assistance can be accessed by MFP participants through the Olmstead Housing Subsidy or one of the 1915(c) Waiver housing subsidies
- MFP is designed to streamline the process of deinstitutionalization for vulnerable populations, including older adults, individuals with physical, intellectual, and/or developmental disabilities, and individuals with a TBI
- Open Doors is the MFP program that funds transition specialists and peer support to assist these individuals to transition out of institutions, such as nursing homes and intermediate care facilities, and into qualifying community settings
- In order to identify whether a CFCO–eligible individual is currently identified as an MFP–qualified participant
- The LDSS will need to review the individual’s eligibility file
- A RR/E code of 89 on an individual’s file indicates that the individual is/was an MFP–qualified participant for a period of time
- The RR/E 89 code is placed after the transition to the community. LDSS should ask the individual if they are participant in MFP
- LDSS may also reach out to the Department if it has concerns about member’s participation in MFP
Guidelines and Reference: Administrative Guidance
- April 1, 2018 ADM was recently published and introduces the process for determining eligibility for individuals seeking CFCO services
- April 1, 2019 ADM will provide the LDSS with information on how to assess and authorize for E–Mods, V–Mods, AT and SAME for children in the Consolidated Children’s 1915c Waiver during the April 1, 2019 to June 30, 2019 period
- Beginning July 1, 2019, most children will transition to Managed Care and the MCO will authorize and manage CFCO services that will be part of the plan benefit package on that date
- July 1, 2019 ADM will describe operationalization of the new services that will be available to eligible individuals in Fee for Service, Managed Care, Managed Long Term Care or enrolled in waiver programs
Personal Emergency Response Systems (PERS)
- PERS serves as one option for the required backup mechanism under CFCO to ensure continuity of service and safety of the participant
- PERS may not be authorized separately from personal care services
- Other backup mechanisms under CFCO include informal supports, such as a neighbor, relative or friend who is committed to be available when the personal assistant is unavailable
- A telephone (mobile or land line) may also be a back–up mechanism
- Any backup mechanism selected must be noted in the Person–Centered POC
CFCO Service Authorization Complements Existing LDSS Service Authorization Process
- The process for authorizing CFCO services will complement the processes that the LDSS now have in place
- For example, if you have a Person–Centered POC in place for a consumer receiving personal care services, a new, separate POC is not necessary if the consumer now qualifies for a CFCO service – you can simply amend the current Person–Centered POC
- Please note that all services authorized by the LDSS must:
- Be documented as an assessed need in the functional needs assessment
- Be included in the Person–Centered POC
Bi–Weekly Calls, Guidelines and Reference
- Please visit the Department’s CFCO website for guidance and helpful information
- Information including Model Contracts, listing of CFCO Service Providers, and the 4/1/18 CFCO ADMcan be found on this website
- Bi–Weekly calls with LDSS – Open Forum to Ask Questions
- Next call February 27, 2019 at 11 am
Contact Information
Questions / Comments – CFCO@health.ny.gov
https://www.health.ny.gov/health_care/medicaid/redesign/community_first_choice_option.htm
Follow Us