Moving to Value-Based Care
- Presentation also available in Portable Document Format (PDF)
New York´s Medicaid Section 1115 Waiver
December 11, 2019
Agenda
- Moving to Value–Based Care
- Continuing the Transformation
- The Process to Date and Public Comments
- The Amendment Request
- Phase 1 – The Waiver Extension – April 1, 2010 through March 31, 2021
- Phase 2 – The Waiver Amendment – April 1, 2021 through March 31, 2024
- The Waiver Amendment – A Closer Look
- Timeline
- Questions
Significant Progress in Four Years and More Work to Do!
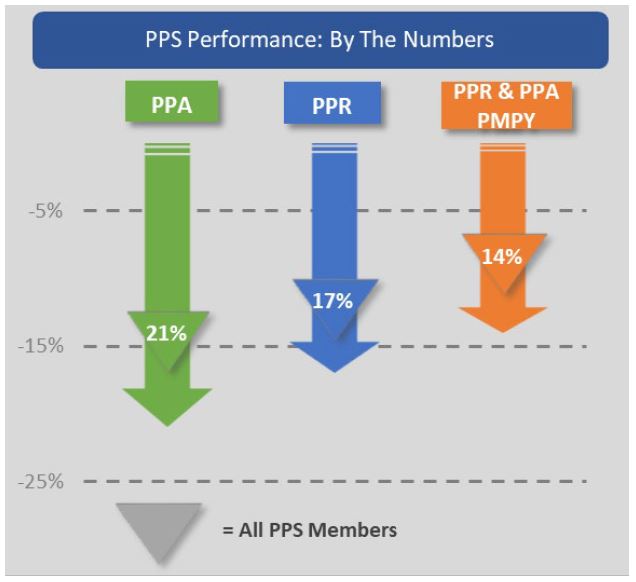
11 PPS → Exceeded a 25% or more reduction in PPAs or PPRs
5 PPS → Reduced PPAs by 38%
4PPS → PMPY Preventable Cost decreased by25% or more
3PPS → Reduced PPRs by 40% or more
PPS – Performing Provider System
PPA – Potentially Preventable Admission
PPR – Potentially Preventable Readmission
PMPY – Per Member Per Year
Moving to Value–Based Care
- Building on the successes of the current waiver through focus on Promising Practices that work
- Building networks that include non–clinical partners to further the goals of improving care
- Focusing on the needs of the whole person by addressing social determinants of health
- Increasing the number of risk–bearing, value–based contracts among Managed Care Organizations (MCOs), providers, and Community–Based Organizations (CBOs)
Continuing the Transformation: The Waiver Submission
The Process to Date
- Waiver concept paper released on September 17, 2019. Over 200 organizations submitted written comments. More than a hundred people attended public forums in NYC and Syracuse.
- Significant overall support for waiver amendment request – many ideas utilized.
- Many common themes which are incorporated in large part in waiver submission:
- Phased approach to waiver request
- Governance, leadership, regionalization approach
- Social Determinant of Health Networks – the importance of addressing social determinants of health
- Inclusion of community–based providers and social care organizations
- Importance and standardization of data access and sharing
- Added focus on new populations (children, long–term care, substance abuse)
- Need for continued support of workforce needs
- Simplification of attribution and performance measurement
Amendment Request
- New York is requesting $8 billion over a four–year timeframe:
- Waiver extension for the first year (Phase 1)
- Waiver renewal for years 2–4 (Phase 2)
- The $8 billion is to be invested as follows:
- $5 billion for targeted interventions through VMOs based on performance (approximately $625 million in Phase 1);
- $1.5 billion for Social Determinant of Health Networks;
- $1 billion on workforce development; and
- $500 million for Interim Access Assurance Fund (IAAF).
- More time is needed to sustain and scale the Delivery System Reform Incentive Payment (DSRIP) program´s Promising Practices with MCOs as part of value–based payment (VBP) arrangements, while driving more careful alignment with current federal healthcare initiatives.
Phase 1 – The Waiver Extension
- Waiver Extension (Phase 1) – April 1, 2020 – March 31, 2021:
- Continue to promote and scale the Promising Practices through existing PPS structure, and
- Streamline performance measurement to:
- the pay–for–performance (P4P) population health measures (e.g. potentially preventable readmissions and potentially preventable visits),
- clinical P4P measures, such as for asthma and diabetes, to align with Total Care VBP measures, and
- high–priority pay–for–reporting (P4R) measures related to the Promising Practices.
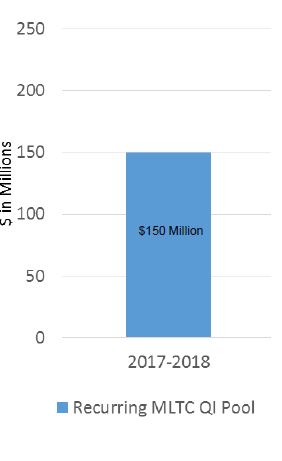
- Funded by unearned dollars from current waiver estimated at $625M.
- Continue robust stakeholder process and negotiations with Centers for Medicare and Medicaid Services (CMS) for Phase 2 implementation.
Phase 2– The Waiver Renewal
- Waiver Renewal (Phase 2) April 1, 2021 – March 31, 2024:
- Permanently sustain Promising Practices through more robust, value–based arrangements and contracting;
- Implement Value Management Organizations and Social Determinant of Health Networks;
- Expand focus to new populations including pregnant women, children, and those in long–term care, and broaden efforts to care for those with substance use disorders;
- Continue focus on improving population health measures;
- Invest in workforce programs to address needed skillsets and workforce shortages; and
- Incentivize network and regional performance, and refined VBP arrangements through Accountability Funding pools.
Phase Two– Waiver Renewal – A Closer Look
Coordinated Population Health Improvement
Value Management Organizations (VMOs): A Multi–Payer Context for Reform
- VMOs will integrate Prevention Agenda goals and consider a multi–payer lens when implementing the Promising Practices to promote 360–degree population health and to further the sustainability of these reform approaches.
Social Determinant of Health Networks (SDHN): Addressing the Whole Person
- Continuing New York´s pioneering investments, Social Determinant of Health Networks will be formed to deliver socially focused interventions linked to VBP.
Performance Measures and Payments to Facilitate Future Value–Based PaymentModels
- Align with the CMS Meaningful Measures Framework, CMS core measure sets, and other federal and state measures already in use.
Expanding to Additional High–Need Areas and Populations
Reduce Maternal Mortality – 50 percent of the State´s births are covered by Medicaid
- In April 2018, Governor Andrew M. Cuomo announced a comprehensive initiative to target maternal mortality and reduce racial disparities in health outcomes. The waiver includes working with Maternal and Infant Community Health Collaboratives and the State–led Perinatal Quality Collaboratives.
Children´s Population Health – 47 percent of the State´s children are covered by Medicaid
- Promising Practices would extend to kids for chronic care management, behavioral health integration with a 2–Generational focus, and attention to adverse childhood experiences and social determinants.
Long–Term Care Reform
- Addresses the rapidly growing senior population and the long–term care sector and workforce including chronic care needs that could be met through palliative care and hospice services.
Continued Improvements/Investments
Workforce Flexibility and Investment
- Promising Practices have relied on non–traditional, non–clinical workforce to achieve project goals and ongoing flexibility will allow for VMOs to invest earned dollars to support this workforce as MCOs and CBOs design VBP approaches to sustain these models in the long term.
Addressing the Opioid Epidemic
- Build on best practices of broad screening for Opioid Use Disorders/Substance Use Disorders (OUD/SUD) in primary care and medication–assisted treatment initiated in EDs and primary care settings. Further focus on the justice–involved population, hospital–to–community linkages, and deployment of peers in care transitions, navigation, and recovery.
Interim Access Assurance Fund
- IAAF 2.0 will be structured to ensure sufficient numbers and types of providers for Medicaid members and uninsured individuals while the State continues its transformation path of driving down avoidable hospitalizations.
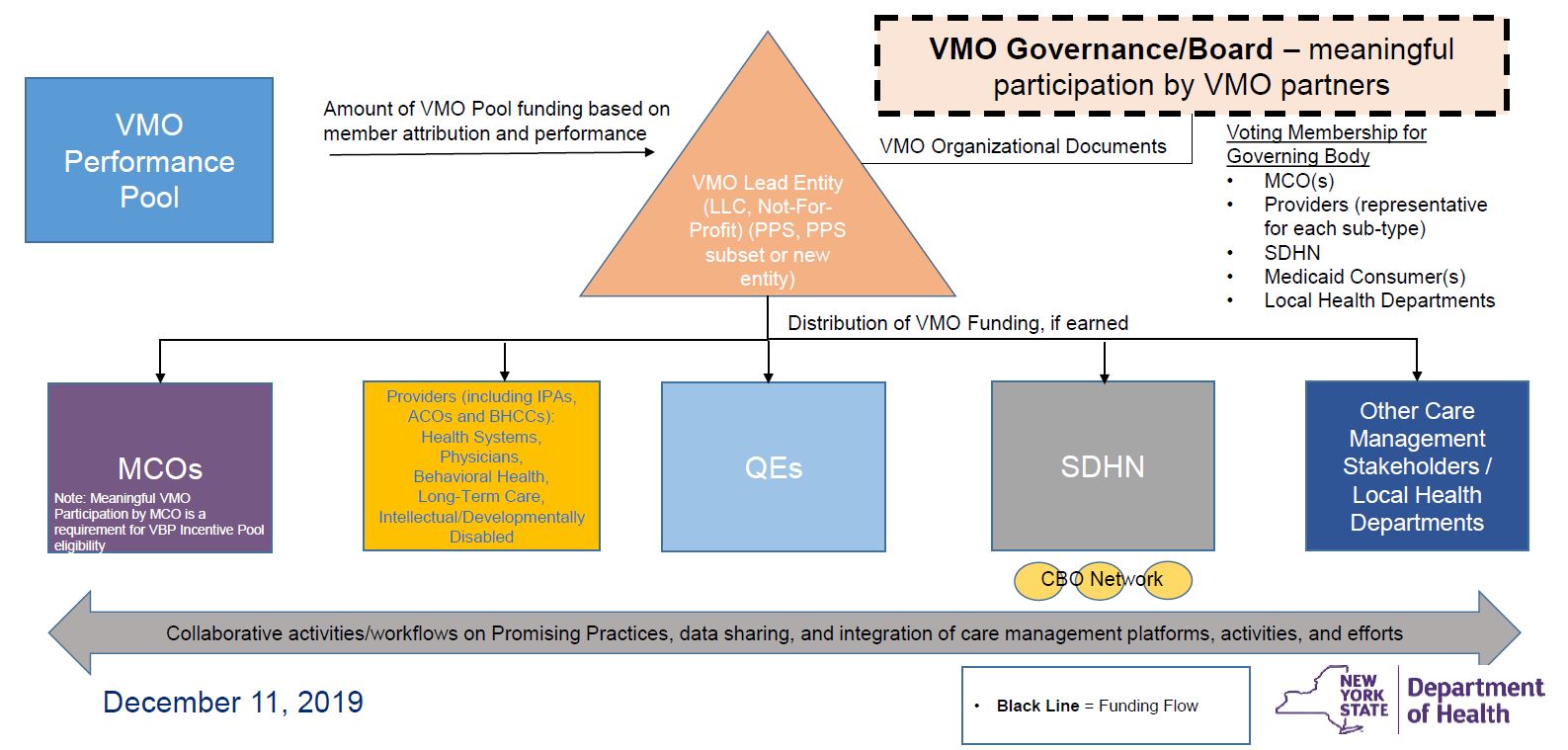
Value Management Organizations (VMOs)
- VMOs will include other sectors in governance and have the primary purpose to create and coordinate broader delivery networks to:
- Create cross–disciplinary networks to advance population health initiatives and promote/scale Promising Practices;
- Coordinate and build upon care management activities among its network participants;
- Support existing value–based payment networks including: Integrated delivery networks, accountable care organizations (ACOs), independent practice associations (IPAs), and Behavioral Health Care Collaborative (BHCCs) and other provider network configurations; and
- Serve as a support vehicle which promotes more sophisticated VBP arrangements, including those that build in CBOs and social support organizations.
- Two funding pools will provide incentive–based award opportunities for both VMOs and MCOs based on achieving performance milestones.
Bringing High–Priority Promising Practices to Scale Statewide
- VMOs will be required to select Promising Practices most appropriate for their region or subpopulation based on their community needs assessment.
- In addition, each VMO will be required to implement 5 high–priority Promising Practice focus areas:
- Transforming and Integrating Behavioral Health – specifically through Peer Outreach and expansion of crisis capacity;
- Care Coordination, Care Management and Care Transitions – specifically through hot spotting, development of care transition teams, and leveraging telehealth;
- Addressing Social Needs, Community Partnerships, and Cross–sector Collaborations – specifically, through utilizing Community Health Workers (CHWs) and linking to SDHN high– priority social care;
- Addressing the Opioid Crisis – specifically Medication–Assisted Treatment (MAT) expansion to primary and emergency department (ED) care and SUD peer bridging; and
- Addressing High Utilizers of Care through Rapid–Cycle Continuous Improvement processes.
United Hospital Fund – DSRIP Promising Practices for Meaningful Change for New York Medicaid
Social Determinant of Health Networks (SDHNs)
- SDHNs will organize a broad base of social care providers in a geographic region;
- Support CBOs and social support organizations in contracting in VBP contracts with MCOs and providers;
- Deliver social–focused interventions included in the VBP contracts:
- SDHNs are expected to convene CBOs and coordinate the CBO activities and infrastructure required to achieve the goals identified in the VBP contracts;
- Work with VMOs to integrate social care into population health work of the VMO; and
- Facilitate CBOs in identifying and receiving non–Medicaid programmatic funding in support of maximizing funding opportunities which align with both federal and state goals.
Phase Two Waiver Structure and Accountability Funding
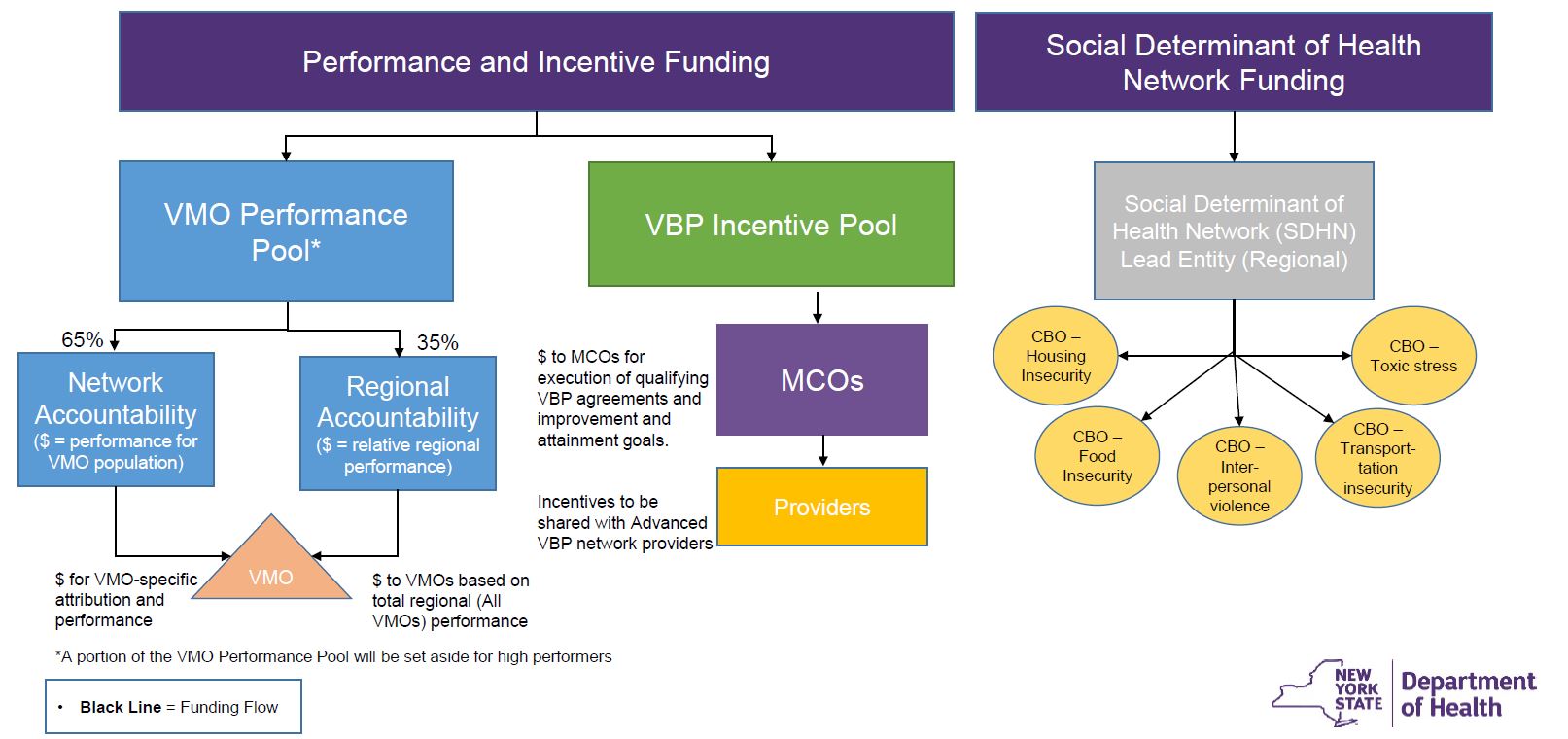
VMO Performance Pool Legal Structure
VBP Incentive Pool Legal Structure
VBP Incentive Pool: Eligibility
- VBP Incentive Pool will fund "Eligible VBP Agreements"
- Eligible VBP Agreements will be new agreements or amendments to existing agreements with the following features:
- Meaningful Participation: MCO must participate meaningfully in one or more VMOs in the region
- Risk Arrangement: Level 2 or greater risk
- Network Composition: Provider network in the arrangement is appropriately inclusive of VMO–affiliated providers to serve the needs of Medicaid members in the arrangement
- Data–Sharing: Minimum standard requirements for data sharing between MCO and providers met
- Quality Reporting: Quality measures and reporting consistent with VMO priorities
- Financial Risk Management: Strategy to address financial security deposit requirements
- VMO Support Services: VMO will furnish ongoing support or administrative services to VBP arrangement
Timeline
Timeline

Follow Us