Maternity Care
Value Based Payment Quality Measure Set
Measurement Year 2025
- Measure Set is also available in Portable Document Format (PDF)
January 2025 NYS Medicaid Value Based Payment
INTRODUCTION
The Measurement Year (MY) 2025 Maternity Care Quality Measure Set was created in collaboration with the Maternity Care, the Primary Care (Physical Health), and the Children's Health Clinical Advisory Groups (CAGs), the New York State Department of Health (the Department) CAG Strategy team, as well as subject matter experts from the the Department Division of Family Health. The goal of this measure set is to align with measures put forth in the NYS Quality Assurance Reporting Requirements (QARR), the Healthcare Effectiveness Data and Information Set® (HEDIS)1 Technical Specifications for Health Plans, the Centers for Medicare & Medicaid Services (CMS) Core measure set, the Merit-based Incentive Payment System (MIPS), where applicable, and the Department's Vital Statistics maternity care program. The Maternity measure set was designed to encourage providers to meet high standards of patient-centered clinical care and coordination across multiple care settings throughout the maternity care episode.
MEASURE SELECTION AND FEASIBILITY
Upon receiving recommendations from CAGs, the release of guidelines from national measure stewards, such as National Committee for Quality Assurance (NCQA)/HEDIS© and CMS, and in accordance with the NYS Value Based Payment (VBP) Roadmap;2 the Department defined a final list of measures to be included in the Maternity Care Measure Set for MY2025. For MY2025 there are a total of seventeen Category 1 and 2 Maternity Care Quality Measures.
VBP ARRANGEMENT REQUIREMENTS FOR MY2025 - HEALTH EQUITY
In MY2022, NCQA added race and ethnicity stratification to several HEDIS measures to help promote transparency in health plan performance. Because high-quality care requires equitable care, NCQA hopes to better identify where disparities exist so they can be addressed. They also hope to identify and learn from top performers in areas where disparities don't exist. To align with this initiative, in July 2022, NYS required payers and providers to incorporate race and ethnicity measure stratification in VBP arrangements. For MY2025, there are 26 HEDIS stratified measures. Twenty-two of these are included in various New York Medicaid VBP arrangement measure sets for payers and providers to add to their VBP contracts. Please refer to the following section for VBP contracting stratification specifications for MY2025.
Stratification Specifications:
- Payers are required to include at least one of the following measures in all level 1 or higher VBP contracts and stratify results by race and ethnicity categories as outlined in the HEDIS MY2025 specifications.3
| NQCA Measure Name | Measure Inclusion by Arrangement Type | |||||
|---|---|---|---|---|---|---|
| TCGP | HARP/BH | Maternity | HIV/AIDs | Children's | ||
| Adult Immunization Status (AIS-E) | ✓ | |||||
| Asthma Medication Ratio (AMR) | ✓ | ✓ | ✓ | ✓ | ||
| Breast Cancer Screening (BCS-E) | ✓ | ✓ | ✓ | |||
| Cervical Cancer Screening (CCS-E) | ✓ | ✓ | ✓ | |||
| Child and Adolescent Well-Care Visits (WCV) | ✓ | ✓ | ||||
| Childhood Immunization Status (CIS-E) | ✓ | ✓ | ||||
| Colorectal Cancer Screening (COL-E) | ✓ | ✓ | ✓ | |||
| Controlling High Blood Pressure (CBP) | ✓ | ✓ | ✓ | |||
| Eye Exam for Patients with Diabetes (EED) | ✓ | ✓ | ✓ | |||
| Follow-Up After Emergency Department Visit for Mental Illness (FUM) | ✓ | ✓ | ✓ | |||
| Follow-Up After Emergency Department Visit for Substance Use (FUA) | ✓ | ✓ | ||||
| Follow-Up After Hospitalization for Mental Illness (FUH) | ✓ | ✓ | ||||
| Glycemic Status Assessment for Patients with Diabetes (GSD) | ✓ | ✓ | ✓ | |||
| Immunizations for Adolescents - Combo 2 (IMA-E) | ✓ | ✓ | ||||
| Initiation and Engagement of Substance Use Disorder Treatment (IET) | ✓ | ✓ | ✓ | |||
| Kidney Health Evaluation for Patients with Diabetes (KED) | ✓ | ✓ | ✓ | |||
| Pharmacotherapy for Opioid Use Disorder (POD) | ✓ | ✓ | ||||
| Postpartum Depression Screening and Follow-Up (PDS-E) | ✓ | |||||
| Prenatal and Postpartum Care (PPC) | ✓ | ✓ | ||||
| Prenatal Depression Screening and Follow-Up (PND-E) | ✓ | |||||
| Prenatal Immunization Status (PRS-E) | ✓ | ✓ | ||||
| Well-Child Visits in the First 30 Months of Life (W30) | ✓ | ✓ | ||||
Stratification Requirements:
- Any measure(s) from the preceding table can be selected for stratification of race and ethnicity provided the two groups approve on the contracting elements around other performance of the measure.
- Payers are required to include the following details in the Provider Contract Statement and Certification form (DOH-4255)4 and Contract language:
- Indicate what measure(s) are included for race and ethnicity stratification.
- Indicate how the stratified measure results for applicable measures will be shared with the VBP contractor.
- Plans are required to include the race and ethnicity data when submitting to NYS using the following method:
- Race and ethnicity fields have been added to the annual VBP member attribution submission file specifications. This will allow the Department to stratify measure performance by race and ethnicity categories for applicable performance measures at the VBP contract and VBP Contractor levels.
All new contracts must meet this requirement to be approved by the Department. As of April 1, 2023, all other existing contracts were to be updated/amended at the end of the contract's current measurement period and before the contract's next measurement period began.
MEASURE CLASSIFICATION
Each measure has been designated by the Department as Category 1, 2, or 3 with associated recommendations for implementation and testing for future use in VBP Arrangements. The measures below are classified by category based on an assessment of reliability, validity, and feasibility, and according to suggested method of use (either Pay for Reporting (P4R) or Pay for Performance (P4P)).
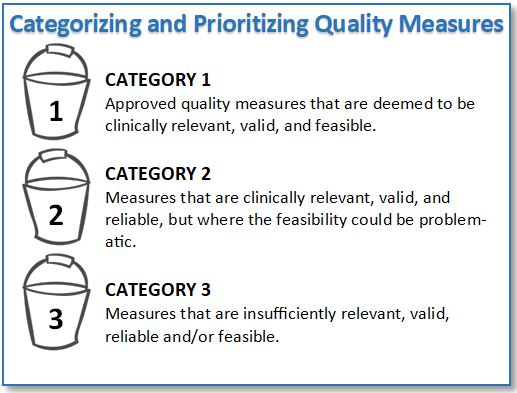
Category 1
Category 1 quality measures as identified by the CAGs and accepted and deemed reportable by the Department are to be reported by VBP Contractors to the Managed Care Organuzatuins (MCOs). These measures are also intended to be used to determine the amount of shared savings for which VBP contractors are eligible.5 At least one Category 1 P4P measure must be included in a VBP contract.
The Department classified each Category 1 measure as either P4P or P4R:
- P4P measures are intended to be used in the determination of shared savings amounts for which VBP Contractors are eligible. Measures can be included in both the determination of the target budget and in the calculation of shared savings for VBP Contractors.
- P4R measures are intended to be used by the MCOs to incentivize VBP Contractors for reporting data to monitor the quality of care delivered to members under the VBP contract. Incentives for reporting will be based on timeliness, accuracy, and completeness of data. Measures can be reclassified from P4R to P4P through annual CAG and Department review or as determined by the MCO and VBP Contractor.
Not all Category 1 measures will be reportable for the measurement year, as reporting on some of these measures will be phased in over the next few years. Please refer to the 2025 Value-Based Payment Reporting Requirements Technical Specifications Manual (MY2025) for details as to which measures must be reported for the measurement year. This manual will be updated annually, in line with the release of the final VBP measure set for the subsequent year.
Categories 2 and 3
Category 2 measures have been accepted by the Department based on the agreement of clinical importance, validity, and reliability but flagged as presenting concerns regarding implementation feasibility. The Department has discussed measure testing approaches, data collection, and reporting requirements with MCOs and VBP Contractors as part of the CAGs.
Measures designated as Category 3 were identified as unfeasible at this time or as presenting additional concerns, including accuracy or reliability when applied to the attributed member population for an arrangement.
MY 2025 MATERNITY QUALITY MEASURE SET
The measures provided on the following pages are recommendations for MY2025. Note that measure classification is a Department recommendation, and implementation is to be determined between the MCO and VBP Contractor.
Measure sets and classifications are considered dynamic and will be reviewed annually. Updates will include measure additions, deletions, recategorizations, and/or reclassifications from P4R to P4P or vice versa, based on experience with measure implementation in the prior year. Please see Appendix A for a full list of these changes.
Category 1
The table below displays the Category 1 MY2025 Maternity Care Quality Measure Set, arranged alphabetically and includes measure title, measure steward and State-recommended classification for measure use. The measure set is redlined to highlight changes made between MY2024 and MY2025; please refer to the key at the end of this tables for an explanation of redlined formatting.
| Maternity Care Measures | Measure Steward | Classification |
|---|---|---|
| Cesarean Birth (eCQM~) (PC-02) | The Joint Commission (TJC) | P4R |
| Contraceptive Care - Postpartum | United States Office of Population Affairs | P4R |
| COVID-19 Immunization Measure (CVS)^ | NYS | P4P |
| Depression Screening and Follow-Up for Adolescents and Adults (DSF-E) | NCQA | P4R |
| Exclusive Breast Milk Feeding (PC-05) | TJC | P4R |
| Hepatitis C Virus (HCV) for all Patients - one time screening* | American Gastroenterological Association | P4R |
| Incidence of Episiotomy | American Medical Association- Physician Consortium for Performance Improvement (AMA-PCPI) | P4R |
| Initiation and Engagement of Substance Use Disorder Treatment (IET) | NCQA | P4P |
| Live Births Weighing Less Than 2,500 Grams (LBW-CH) | Centers for Disease Control and Prevention (CDC) | P4R |
| Postpartum Depression Screening and Follow-up (PDS-E) | NCQA | P4R |
| Prenatal and Postpartum Care (PPC) | NCQA | P4P |
| Prenatal Depression Screening and Follow-Up (PND-E) | NCQA | P4R |
| Prenatal Immunization Status (PRS-E) | NCQA | P4P |
| Preventive Care and Screening: Tobacco Use: Screening and Cessation Intervention | NCQA | P4R |
| Social Need Screening and Intervention (SNS-E) | NCQA | P4P |
^Measure Revised for MY2025
*New Measure MY2025
~eCQM - electronic clinical quality measure
Category 2
The table below displays the Category 2 MY2025 Maternity Care Quality Measure Set and includes the measure title and measure steward. All Category 2 measures are classified as P4R in MY2025. Category 2 measures were reviewed in detail this year and streamlined to include only those with an active measure steward and/or potential for movement to Category 1 in subsequent years. The measure set is redlined to highlight changes made between MY2024 and MY2025; please refer to the key at the end of this table for an explanation of redlined formatting.
| Measure | Measure Steward |
|---|---|
| Hepatitis B Vaccine Coverage Among All Live Newborn Infants Prior to Hospital or Birthing Facility Discharge | Centers for Disease Control (CDC) |
| Postpartum Blood Pressure Monitoring | Texas Maternity Bundle |
Appendix A
The tables below identify the changes to the Category 1 measures for the MY2025 Maternity Care Quality Measure Set.
Category 1 Measure Changes from 2024 to 2025
| Measure Name | Change | Rationale for Change |
|---|---|---|
| COVID-19 Immunization Measure (CVS) | Specifications Change | Enrollment/anchor dates, measurement period, and CDC vaccine codes updated. |
| Hepatitis C Virus (HCV) for all Patients - one time screening | New Measure | Added to align with the Department's campaign to promote expanded Hepatitis C screenings. |
Category 2 Measure Changes from 2024 to 2025
| Measure Name | Change | Rationale for Change |
|---|---|---|
| No Changes for 2025 | ||
__________________________________________________________
1. HEDIS® is a registered trademark of the National Committee for Quality Assurance (NCQA). 1
2. New York State Department of Health, Medicaid Redesign Team, Value Based Payment: Update, May 2023. (Link) 2
3. HEDIS® Measurement Year 2025 Volume 2 Technical Specification for Heath Plans, General Guidelines section 31. 3
4. DOH 4255 has been updated, Section C 2e, to include a Quality Measure Race and Ethnicity Stratification section (Link) 4
Follow Us