Information for Medicaid Members
New York Medicaid Members with social and health needs may qualify for support to access services like food, housing, and transportation. Local groups called Social Care Networks (SCNs) are available to connect Medicaid Members to services in their community.
Watch this short video to learn more about how SCNs can help Medicaid members access the right services to meet their social care needs.
Explore the member factsheets to learn what navigation and other services are available through the SCN program, including help with food, housing, transportation, and more.
Member Factsheets
Frequently Asked Questions
- Social Care Networks are groups of local, primarily non-profit organizations that support the health and wellbeing of communities across New York State.
- Social Care Networks can help New York Medicaid Members find services that could help address their social needs, such as housing, food and nutrition, transportation, and other social needs.
- Screening: Social Care Networks may help Medicaid Members identify social needs impacting their health, such as living situation, access to healthy food, access to transportation, employment, education, and personal safety
- Navigation: Social Care Networks may help Medicaid Members find services in the community to meet their social needs. Navigation involves working with a Social Care Navigator to get connected to services and may take place in-person or over the phone
- Social care services: Depending on individual needs, there may be additional one-time or temporary services (up to 6 months) available for Medicaid Members who qualify, beyond Medicaid services and benefits available today
- Screening: Medicaid Members in New York may connect with a Social Care Network to identify social needs impacting their health (for example, living situation, access to healthy food or transportation, etc.)
- Navigation: Help finding services in the community may be available to Medicaid Members who have a social need impacting their health.
- Social care services: Those with a Medicaid Managed Care Plan may be connected to additional one-time or temporary services available in their community if they qualify by having a specific health condition. All Medicaid Members may be connected to existing community, state, and federal programs if they qualify (e.g., Supplemental Nutrition Assistance Program).
- Social Care Networks may offer one-time or temporary services to Medicaid Managed Care Members for a short period (1-2 weeks) or longer (up to 6 months) depending on Members clinical needs.
- Temporary social care services help Medicaid Managed Care Members who qualify better manage and/or maintain their health. Examples include:
- Food and nutrition assistance such as home delivered meals, food prescription boxes, or cooking supplies
- Housing support such as housing navigation for someone who is unhoused, home safety modifications for those with a physical disability, or mold/pest removal for those with uncontrolled asthma
- Transportation to appointments like enrolling in supportive housing
- Social care management, or connections to social care services after the temporary service
- Availability of these temporary services may vary by region.
- Medicaid Managed Care Members with certain health conditions and social needs may be eligible for one-time or temporary services as part of the Social Care Network program, in addition to existing benefits and services already available in the community.
- Medicaid Managed Care Members with the following needs may be able to receive additional one-time or temporary services in addition to help finding services outside of this program.
- Living with a mental health condition or substance use challenge
- Living with an intellectual or developmental disability
- Pregnant or recently had a baby
- Recently released from jail or prison with a chronic health condition (such as diabetes, cancer, kidney or bone diseases, substance use challenges, hepatitis C, or others)
- Kids and young people with health needs (e.g., asthma, diabetes)
- Having frequent visits to the emergency room or hospital
- Enrollment in a New York State Health Home
- Some services have specific health conditions required to qualify in addition to those listed above (e.g. home modifications and home remediation have additional criteria).
- Your local Social Care Network can help find programs and services that you or your family may qualify for.
- To help connect to services, Members may be asked about health and daily needs, like living situation, access to healthy food, access to transportation, education, employment, and personal safety.
- If you are enrolled in Medicaid Managed Care and have certain qualifying health conditions, you may be eligible for temporary services based on individual, household, or family needs.
- Reach out to your Social Care Network to find out more about programs and services available by region.
- There is no cost for Medicaid Members to receive assistance determining any social needs impacting their overall health.
- For Medicaid Members with a social need impacting their overall health, there is no cost for navigation, or help finding services in the community that could help address those needs.
- Finally, Medicaid Managed Care Members with qualifying health conditions can receive temporary services at no cost through the Social Care Network program.
- Medical benefits for Medicaid Members are not affected by the Social Care Network program.
- This program gives qualifying Medicaid Members access to assistance finding programs and services related to food, nutrition, housing, transportation, education, employment, and safety. For those enrolled in Medicaid Managed Care with certain qualifying health conditions, there may also be one-time or temporary social care services available.
- The one-time or temporary social care services are complementary to existing Medicaid benefits.
- Getting help finding programs and services and receiving temporary social care services through the Social Care Network program does not affect eligibility for state or federal services, such as the Supplemental Nutrition Assistance Program (SNAP) or Special Supplemental Nutrition Program for Women, Infants, and Children (WIC).
What is a Social Care Network?
What services do Social Care Networks provide?
Who is eligible for Social Care Network services?
What are examples of one-time or temporary social care services?
What conditions may qualify a Medicaid Managed Care Member for additional one-time or temporary services?
How do I get help through this program?
Do I have to pay for Social Care Network services?
Are my Medicaid benefits changing?
Find a local Social Care Network
By SCN
SCN Counties Phone number
for MembersCare Compass Collaborative Broome, Chenango, Delaware, Otsego, Tioga, Tompkins 607-352-5264 Forward Leading IPA Allegany, Cayuga, Chemung, Genesee, Livingston, Monroe, Ontario, Orleans, Schuyler, Seneca, Steuben, Wayne, Wyoming, Yates 315-264-9991 Health Equity Alliance of Long Island Nassau, Suffolk 516-505-4434 Healthy Alliance Foundation Inc. Albany, Columbia, Greene, Rensselaer, Montgomery, Saratoga, Schenectady, Schoharie 518-520-3211 Cortland, Herkimer, Madison, Oneida, Onondaga, Oswego 315-505-2290 Clinton, Essex, Franklin, Fulton, Hamilton, Jefferson, Lewis, St. Lawrence, Warren, Washington 518-656-8312 Hudson Valley Care Coalition, Inc. Dutchess, Orange, Putnam, Rockland, Sullivan, Ulster, Westchester 914-215-5292 Public Health Solutions Manhattan, Queens, Brooklyn 888-755-5045 Staten Island Performing Provider System Richmond 917-830-1140 Somos Healthcare Providers, Inc. Bronx 833-SOMOSNY
(833-766-6769)Western New York Integrated Care Collaborative Inc. Cattaraugus, Chautauqua, Erie, Niagara 716-431-5100 By County
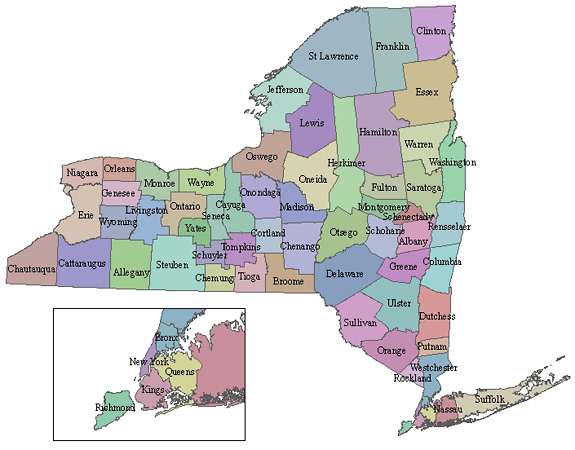
To find information about SCN by county, select a county from the map below. For information about a specific SCN, select from the list below.
SCN by County Phone number
for MembersAlbany Back to Map 518-520-3211 Allegany Back to Map 315-264-9991 Bronx Back to Map 833-SOMOSNY
(833-766-6769)Broome Back to Map 607-352-5264 Cattaraugus Back to Map 716-431-5100 Cayuga Back to Map 315-264-9991 Chautauqua Back to Map 716-431-5100 Chemung Back to Map 315-264-9991 Chenango Back to Map 607-352-5264 Clinton Back to Map 518-656-8312 Columbia Back to Map 518-520-3211 Cortland Back to Map 315-505-2290 Delaware Back to Map 607-352-5264 Dutchess Back to Map 800-768-5080 Erie Back to Map 716-431-5100 Essex Back to Map 518-656-8312 Franklin Back to Map 518-656-8312 Fulton Back to Map 518-656-8312 Genesee Back to Map 315-264-9991 Greene Back to Map 518-520-3211 Hamilton Back to Map 518-656-8312 Herkimer Back to Map 315-505-2290 Jefferson Back to Map 518-656-8312 Kings (Brooklyn) Back to Map 888-755-5045 Lewis Back to Map 518-656-8312 Livingston Back to Map 315-264-9991 Madison Back to Map 315-505-2290 Monroe Back to Map 315-264-9991 Montgomery Back to Map 518-520-3211 Nassau Back to Map 516-505-4434 New York (Manhattan) Back to Map 888-755-5045 Niagara Back to Map 716-431-5100 Oneida Back to Map 315-505-2290 Onondaga Back to Map 315-505-2290 Ontario Back to Map 315-264-9991 Orange Back to Map 800-768-5080 Orleans Back to Map 315-264-9991 Oswego Back to Map 315-505-2290 Otsego Back to Map 607-352-5264 Putnam Back to Map 800-768-5080 Queens Back to Map 888-755-5045 Rensselaer Back to Map 518-520-3211 Richmond (Staten Island) Back to Map 917-830-1140 Rockland Back to Map 800-768-5080 Saint Lawrence Back to Map 518-656-8312 Saratoga Back to Map 518-520-3211 Schenectady Back to Map 518-520-3211 Schoharie Back to Map 518-520-3211 Schuyler Back to Map 315-264-9991 Seneca Back to Map 315-264-9991 Steuben Back to Map 315-264-9991 Suffolk Back to Map 516-505-4434 Sullivan Back to Map 800-768-5080 Tioga Back to Map 607-352-5264 Tompkins Back to Map 607-352-5264 Ulster Back to Map 800-768-5080 Warren Back to Map 518-656-8312 Washington Back to Map 518-656-8312 Wayne Back to Map 315-264-9991 Westchester Back to Map 800-768-5080 Wyoming Back to Map 315-264-9991 Yates Back to Map 315-264-9991