Information for Health Care Providers
Health care providers are a key partner in the Social Care Network program, which aims to increase integration of physical health, behavioral health, and services that address health-related social needs. Coordinating these aspects of a Member's care is foundational to New York State's health equity goals. Please review the SCN: Introduction for Health Care Providers Guide (PDF) here.
Watch this short video to learn more about how health and behavioral health providers can help Medicaid members access the right services to meet their social care needs.
Health care providers, including physical and behavioral health, can participate in the Social Care Network program in many ways:
- Talk to Medicaid patients about Social Care Networks and the services that may be available to them across nutrition, housing, transportation, and navigation supports; Lead Entities may share factsheets and other informational material that can be distributed via your offices
- Share contact information for a regional Lead Entity
- Conduct screening for health-related social needs in Medicaid patients using the required data elements of the Accountable Health Communities Health-Related Social Needs Assessment in the domains of housing, utilities, nutrition, transportation, employment, education, and interpersonal safety.
Have questions about how to exchange data with the Social Care Network? Please review our SCN Data and IT factsheet for providers.
Providers who join a Social Care Network may receive reimbursement for screening and navigation of Medicaid Members if using twelve questions from the Accountable Health Communities Health-Related Social Needs Assessment. (please see section b. Screening in the Social Care Network: Program, Billing, and Data Governance Operations Manual). To receive reimbursement, health care providers must:
- Be in contract with a Lead Entity (providers working across multiple regions may contract with multiple Lead Entities)
- Be able to submit the HRSN screening through the regional Qualified Entity to the Statewide Health Information Network OR use the Social Care Network IT platform.
- Remain in good standing with New York Medicaid
Reach out to the Lead Entity in your region(s) to learn more.
Health care providers - including health systems, behavioral health providers, federally qualified health centers, primary care providers, and others - all play important roles in the care of Medicaid Members. Social Care Networks (SCNs) are new, Member-centric partners that closely coordinate with the provider community to increase integration of physical health, behavioral health, and social care. The ultimate goal of the SCN program is to address health-related social needs (HRSNs) in the Medicaid population and to improve health equity in New York State. Click here for an introductory guide on providers’ roles in the SCN program, which contains a more extensive FAQ beyond the answers below.
Frequently asked questions
What is a social care network?
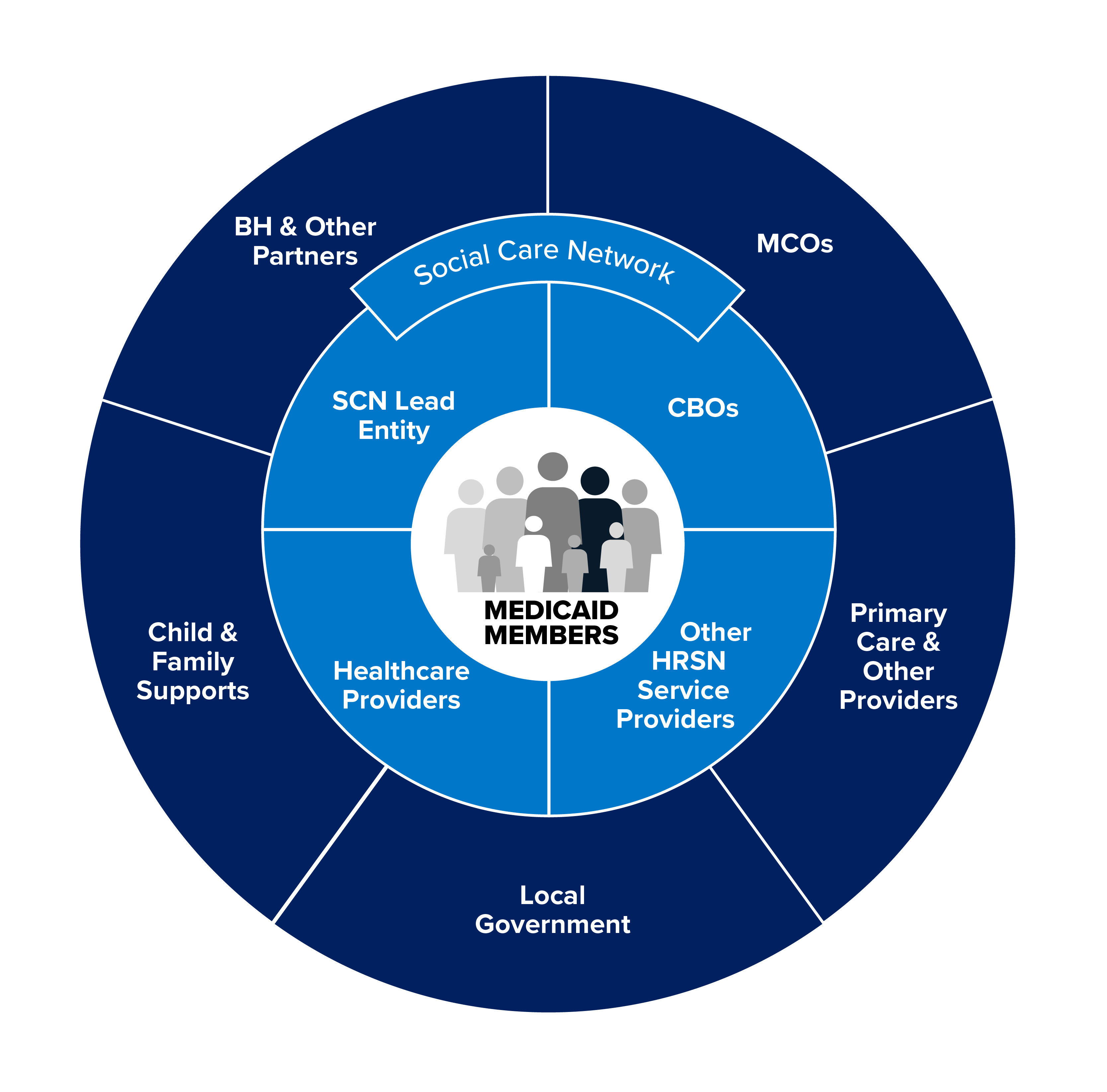
A Social Care Network (SCN) is a network comprised of health-related social needs (HRSN) service providers including community-based organizations, Medicaid managed care organizations (MCOs), health care providers, and other partners. Network participants contract with and are reimbursed by an SCN Lead Entity for activities including screening Medicaid Members for unmet HRSNs, navigating Members to HRSN services, and delivering HRSN services to Members.
Social Care Network ecosystem partners
What is the Member experience?
The Member experience when accessing SCN services consists of three key steps:
- Screening: The SCN program aims to screen all Medicaid Members for HRSNs. Providers can contract with an SCN to deliver HRSN screenings using a State-standardized version of the Accountable Health Communities (AHC) tool, a questionnaire which enables quick assessment of HRSNs from five domains determined to be “core needs” by CMS and eight supplemental domains. Providers may be reimbursed for HRSN screenings of Medicaid Members if they are contracted with an SCN to perform this activity, use the AHC tool, and enter screening data into a regional SCN IT platform or send it to that platform via a regional Qualified Entity (QE) that is connected to the Statewide Health Information Network for New York (SHIN-NY). SCN Lead Entities will provide more information on how to connect with their IT platform when partners reach out about joining the Network, and will offer training and technical assistance to contracted providers.
- Navigation: Medicaid Members with HRSN(s) identified through screening can receive navigation services, which include an eligibility assessment and connection to social care services (e.g., housing supports, nutrition assistance, transportation, education, employment) for which they qualify. These services may be existing federal, state, or local programs, or may be enhanced HRSN services offered through the SCN program (see next step). Providers can contract with an SCN to deliver navigation services and be reimbursed; social care navigators may be non-clinical including care managers, social workers, or community health workers.
- HRSN service delivery: All Medicaid Members may be navigated to existing federal, state, or local services, and Medicaid Managed Care Members who qualify may be navigated to enhanced HRSN services. These enhanced services are temporary and can range from short-term (e.g., 1-2 weeks) to longer-term (up to 6 months) depending on Member health and social needs. Categories of enhanced HRSN services include housing supports, food and nutrition assistance, transportation, and social care management (including connection to these and other social care services). Details on enhanced HRSN services by category can be found in the introductory guide (figure 4).
Who qualifies for enhanced HRSN services?
Medicaid Members in both fee for service (FFS) and Medicaid Managed Care (MMC) can be screened for HRSN and receive navigation to existing local, state, and federal supports (e.g., Supplemental Nutrition Assistance Program, supportive housing). MMC beneficiaries may qualify for additional, enhanced HRSN services.
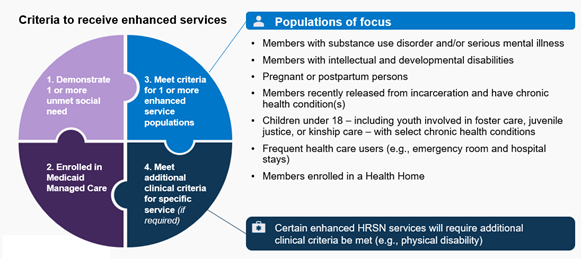
For a Member to qualify for enhanced HRSN services, there are four criteria:
- Member has one or more unmet HRSNs (demonstrated through AHC screening)
- Member is enrolled in Medicaid Managed Care
- Member meets criteria for one or more enhanced services populations (see image below)
- Member meets additional clinical criteria as required for specific HRSN services (e.g., physical disability that requires a home modification for accessibility, such as a ramp)
Medicaid Member eligibility overview
How can a provider participate in a Social Care Network and be paid for screening?
The only way for a provider to participate in an SCN and get paid is to contract directly with the SCN lead entity of the region where the member lives. Any data exchange will need to fit in and be in close coordination with the technical workflow of the contracted SCN lead entity and the QEs/SHIN-NY.
What role do health care providers play in confirming Member eligibility?
Health care providers will support Members in accessing enhanced HRSN services by completing a State-standardized provider attestation form at the request of a Social Care Navigator or Member. Provider attestation may be needed to confirm certain clinical or population criteria required for a Member to be eligible for enhanced HRSN services. The State-standardized form includes a list of criteria providers can review and attest to, as well as definitions of those criteria.
Completed provider attestation forms should be shared back with the Member or the SCN through a HIPAA-compliant transmission method. Any provider who sees Medicaid Members may complete the form - providers do not need to be contracted into the SCN. Providers may embed the attestation form within their existing process flows, for example, integrating the form within their EHR.
How can you join a Social Care Network?
To learn more about becoming a provider in an SCN, reach out to the SCN Lead Entity in your service delivery region. If you provide services in more than one region, you may collaborate and/or contract with multiple SCNs. SCN Lead Entities will also be able to share more detailed operational guidance as you get started, including specific processes for your region and the services you provide to Medicaid Members.

| Lead Entities | Map Color | Counties |
|---|---|---|
| Care Compass Collaborative | Broome, Chenango, Delaware, Otsego, Tioga, Tompkins | |
| Forward Leading IPA | Allegany, Cayuga, Chemung, Genesee, Livingston,Monroe, Ontario, Orleans, Schuyler, Seneca, Steuben, Wayne, Wyoming, Yates | |
| Health Equity Alliance of Long Island | Nassau, Suffolk | |
| Healthy Alliance Foundation Inc. | 1 |
Albany, Columbia, Greene, Rensselaer, Montgomery, Saratoga, Schenectady, Schoharie |
2 |
Cortland, Herkimer, Madison, Oneida, Onondaga, Oswego | |
3 |
Clinton, Essex, Franklin, Fulton, Hamilton, Jefferson, Lewis, St. Lawrence, Warren, Washington | |
| Hudson Valley Care Coalition, Inc. | Dutchess, Orange, Putnam, Rockland, Sullivan, Ulster, Westchester | |
| Public Health Solutions | Kings (Brooklyn), New York (Manhattan), Queens | |
| Staten Island Performing Provider System | Richmond (Staten Island) | |
| Somos Healthcare Providers, Inc. | Bronx | |
| Western New York Integrated Care Collaborative Inc. | Cattaraugus, Chautauqua, Erie, Niagara |
Additional resources for Health Care Providers
- SCN program overview - (PDF)
- SCN Introductory Guide for Health Care Providers - (PDF)
- Webinar: Provider Introduction to Social Care Networks - (YouTube) - (PDF)
- Social Care Network Webinar: Opportunities for Provider Participation and Impact - (YouTube) - (PDF)
- Provider attestation form - (PDF)
- SCN Program, Billing, and Data Governance Operations Manual - (PDF) - Updated January 2026