Social Care Networks (SCN)
Increasing and strengthening the delivery of social care services to Medicaid members across New York State.
The mission of New York State is to protect and promote health for all, building on a foundation of health equity. In New York and nationally, there is growing recognition that fully achieving health for all requires a focus not only on physical and behavioral health but also on health-related social needs (HRSNs).
It is now widely acknowledged that addressing social needs such as food insecurity, housing instability, and lack of transportation improves health and lowers health care costs. To ensure that these needs are consistently addressed for New York's Medicaid Members, New York needs a coordinated infrastructure and set of processes through which member's unmet social needs can be identified, Members can be connected to services to address those needs, and the organizations who provide those services can be paid.
On January 9, 2024, the Centers for Medicare and Medicaid Services (CMS) approved the New York Health Equity Reform (NYHER) 1115 Waiver Demonstration Amendment, including new funding to establish Social Care Networks (SCNs) and deliver HRSN services.
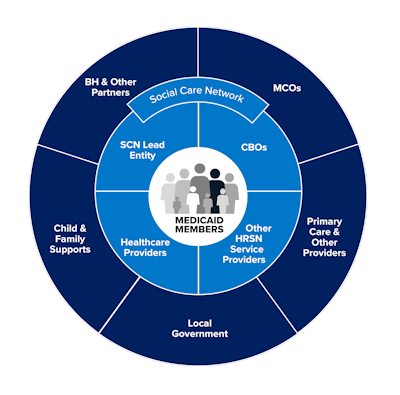
The establishment of Social Care Networks (SCNs) is a core part of the NYHER Amendment. New York State has established 9 regional Social Care Network Lead Entities who are responsible for building a robust Network of Community-Based Organizations (CBOs) and other organizations providing health-related social needs services and coordinating with health care providers (inclusive of behavioral health and primary care providers). Together, each Social Care Network is responsible for ensuring that there is a seamless, consistent, coordinated, end-to-end process in their region for Screening, Navigation, and delivery of health-related social needs services. This requires close collaboration within each Network, as well as shared data and technology provided by the State. Social Care Network Lead Entities also engage a broader ecosystem of partners to achieve their goals, including health insurance plans, local government, and child & family supports.
Social Care Networks (SCN) Program Overview (PDF)
SCN Program Updates as of September 2025 (PDF)
Social Care Networks will Achieve Four Goals for Medicaid Members:
- Expand access to high-quality HRSN services
- Enable consistent, timely screening using the Accountable Health Communities (AHC) HRSN Screening Tool and Navigation to HRSN services
- Create shared end-to-end visibility of the Member journey from HRSN Screening and Navigation through delivery of HRSN services
- Strengthen collaboration between HRSN service providers and other partners in their regional health ecosystem, including, providers, care managers, and health plans
The Role of Social Care Network Lead Entities
The Social Care Network Lead Entities are organizations chosen for their expertise in supporting New York Medicaid Members, deep understanding of their region, and ability to coordinate an ecosystem of partners. They are responsible for creating and managing networks to provide screening and navigation to Medicaid Members, and ultimately to ensure services are delivered to address health-related social needs.
The role of Lead Entities includes:
- Building a Network within the region to provide screening, navigation, and nutrition, housing, and transportation services to Medicaid Members
- Paying providers in their Network for heath-related social needs services delivered
- Facilitating secure data exchange to support navigation and service delivery
- Reporting on Network performance to support health equity goals and measure impact of the Social Care Network program
- Establishing a governing board that reflects the unique needs of the region
Awarded Social Care Networks

| Lead Entities | Map Color | Counties |
|---|---|---|
| Care Compass Collaborative | Broome, Chenango, Delaware, Otsego, Tioga, Tompkins | |
| Forward Leading IPA | Allegany, Cayuga, Chemung, Genesee, Livingston,Monroe, Ontario, Orleans, Schuyler, Seneca, Steuben, Wayne, Wyoming, Yates | |
| Health Equity Alliance of Long Island | Nassau, Suffolk | |
| Healthy Alliance Foundation Inc. | 1 |
Albany, Columbia, Greene, Rensselaer, Montgomery, Saratoga, Schenectady, Schoharie |
2 |
Cortland, Herkimer, Madison, Oneida, Onondaga, Oswego | |
3 |
Clinton, Essex, Franklin, Fulton, Hamilton, Jefferson, Lewis, St. Lawrence, Warren, Washington | |
| Hudson Valley Care Coalition, Inc. | Dutchess, Orange, Putnam, Rockland, Sullivan, Ulster, Westchester | |
| Public Health Solutions | Kings (Brooklyn), New York (Manhattan), Queens | |
| Staten Island Performing Provider System | Richmond (Staten Island) | |
| Somos Healthcare Providers, Inc. | Bronx | |
| Western New York Integrated Care Collaborative Inc. | Cattaraugus, Chautauqua, Erie, Niagara |
Recent News
- New York State Medicaid Director Amir Bassiri speaks at United Hospital Funds 2024 Medicaid Conference (YouTube) - July 31, 2024
- Governor Hochul Announces $500 Million for New Social Care Networks Program to Deliver Social Services and Improve Health Outcomes for Millions of Low-Income New Yorkers - August 7, 2024
Additional Resources
Stay in Touch
To subscribe, send an email addressed to listserv@list.ny.gov and include the following information in the body of the message:
"SUBSCRIBE MRT-L YourFirstName YourLastName"