| Updated Language |
All Other Limited Health-Related Services that a 29-I Health Facility provides must be included in on the 29-I License prior to delivery of services except for CFTSS and HCBS, and which may require a separate State designation and are indicated in the 29-I's NYS Designation letter. prior to delivery of services. |
p.8 |
| Updated Language |
Children's Waiver Home and Community-Based Services (HCBS)
- a. Caregiver Family Advocacy and Support Services
b. Community Advocacy and Support- g. Palliative Care:
Bereavement Therapy Counseling and Support Services
- m. Adaptive and Assistive
Equipment Technology
|
p.8-9 |
| Added language |
Agencies that do not obtain Article 29-I Licensure are not authorized to receive a Medicaid per diem to provide Core Limited Health-Related Services and are not permitted to bill for Other Limited Health-Related Services. |
p.12 |
| Added language |
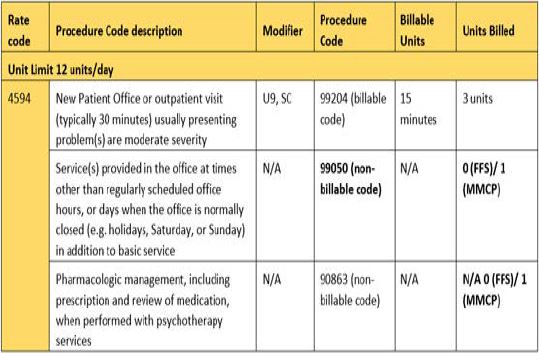
Non-billable procedure codes submitted on MMCP claims will have one unit and will be reimbursed at $0. ; Non-billable procedure codes submitted on FFS claims will have zero units and will not be reimbursed. Although these codes are not associated with a fee, they should be reported on the claim to accurately represent services delivered during the encounter. Each rate code should be billed on separate claim. |
p.19 |
| U pdated Language |
It is permissible to claim the 29-I Health Facility Medicaid residual per diem rate for all days of the following absence categories:
- Weekday and weekend visits , up to seven consecutive days per visit
|
p.20 |
| Removed Language |
Absence Categories when it is Not Permissible to Claim the Medicaid Residual Per Diem: In the following circumstances of absence, it is not permissible to claim the 29-I Core Limited Health- Related Services (Medicaid residual per diem) rate:
- Out-of-state
congregate care placement setting
|
p.21 |
| Added Language |
In addition to rate codes, procedure codes are required when submitting Medicaid Managed Care claims. If an encounter requires multiple procedure codes to detail the services that were delivered, include all procedure codes that apply (including non-billable procedure codes). |
p. 23 |
| Updated Billing Example |
|
p.25 |
| Added Language |
Non-billable procedure codes on FFS claims will have zero units and will not be reimbursed; however, they should be reported on the claim to accurately represent the services delivered during the encounter. |
p.26 |
| Updated Language |
When submitting MMCP Other Limited Health Related-Service claims for services delivered to the same child/youth, during the same day and under the same rate code, submit one claim indicating one rate code. On each claim, report the procedure codes that reflect the services delivered during the encounter related to the rate code. Non-billable procedure codes will have one unit and will be paid at $0; however, they should be reported on the claim to accurately represent services delivered during an encounter. |
p.26 |
| Updated Language |
MMCP Example: If a 29-I Health Facility provides Developmental Test Administration using rate code 4589 for one hour and thirty minutes, the claim would need to reflect rate code 4589, procedure codes 96112 and 96113 with a total of 6 units on the claim . I f more than one procedure code is billable on the claim the units must reflect what was delivered in the encounter. Non-billable procedure codes will be indicated as one unit on the managed care claim and will pay at $0. Only the billable portion of the claim will be associated with a payment amount. |
p.26-27 |
| Refreshed Hyperlinks |
All hyperlinks refreshed throughout manual. |
Throughout Manual |